Abstract
Transforming growth factor-β1 (TGFβ1) plays a significant role in regulating cellular proliferation and apoptosis. A large number of studies related to the association between TGFβ1 Leu10Pro polymorphism and prostate cancer (PC) risk, but get conflicting results. We performed a meta-analysis based on six studies, assessing the strength of the association using odds ratios (OR) with 95 % confidence intervals (CI). Overall, our evidence has indicated that TGFβ1 Leu10Pro polymorphism had significantly increased PC risk in the allele comparison model (OR = 1.081, 95 % CI = 1.003–1.165, P heterogeneity = 0.141, P = 0.041). In the stratified analysis by ethnicity, the same results were found among Caucasians (for heterozygote model, OR = 1.741, 95 % CI = 1.004–3.020, P heterogeneity = 0.000, P = 0.049; recessive model, OR = 1.339, 95 % CI = 1.045–1.717, P heterogeneity = 0.020, P = 0.021; allele comparison model, OR = 1.091, 95 % CI = 1.005–1.184, P heterogeneity = 0.048, P = 0.037). In conclusion, this meta-analysis suggested that TGFβ1 Leu10Pro polymorphism contributed to the development of PC. A well-designed and larger study is still required to evaluate this polymorphism and PC risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PC) is one of the most common malignancies among men in the Western world and a major health problem in many industrialized countries [1]. PC, like other tumors, is a complex event and is caused by multiple mechanisms. Recent advances in research on the TGF-β1 signaling pathway have revealed that it is regulated by several mechanisms, and many oncogenic and anti-oncogenic proteins play important roles in the tumor development under the control of the TGF-β1 [2]. TGF-β1 is a multifunctional cytokine involved in inducing cell differentiation, embryogenesis, vascularization, migration, and cell cycle regulation. It is part of a family consisting of at least three members (TGF-β1-3) [3, 4]. Among them, TGF-β1 is the most abundant and commonly expressed [5]. It is reported that the TGF-β1 gene product has a biphasic nature: in normal cells, it is associated with tumor suppression by promoting differentiation and inhibiting growth by arresting the cell cycle at the G1 phase [6, 7]. In transformed cells, defects in the TGF-β1 signaling pathway lead to resistance to TGF-β1-mediated growth-inhibiting effects and to an overexpression of TGF-β1 [8]. When the anti-proliferative effect of the TGF-β1 signaling pathway is disrupted, increased expression of TGF-β1 aids in the promotion of tumorigenesis.
There are different polymorphism sites in the TGF-β1 gene, which is located at 19q13.1 [9]. One of these polymorphisms, a T to C transition at nucleotide 29 of amino acid number 10, changes leucine to proline and is termed Leu10Pro (L10P, formerly also known as 869 T > C). This is one of the most widely studied mutations. This change is associated with increased serum level of TGF-β1 because of increased secretion [5, 10]. Several case–control studies investigated the role of the TGF-β1 Leu10Pro polymorphism on the risk of prostate cancer [11–15]. One study proposed that codon10 polymorphism in TGF-β1 may have a significant influence on the development of PC, whereas two other studies could not confirm this association [11, 13, 14]. In order to investigate the association between TGF-β1 Leu10Pro polymorphism and the risk of PC, we conducted this meta-analysis.
Materials and methods
Publication search strategy
A comprehensive and systematic search through the PubMed and Embase databases was performed using these terms as follows: “transforming growth factor β1” or “TGFβ1,” “polymorphism,” and “glioma” “brain tumor” (the last search was updated July 25, 2013). There were no language and sample size limitation in the included studies. All relevant publications were reviewed. Articles in reference lists were also hand-searched for potentially relevant publications. When more than one of the same or overlapping populations was included in several studies, only the most recent or complete study was used for this meta-analysis.
Inclusion and exclusion criteria
Studies included in this meta-analysis should meet the following criteria: (1) only case–control studies; (2) evaluation of TGFβ1 Leu10Pro polymorphism and glioma risk; and (3) sufficient data for examining an odds ratio (OR) with 95 % confidence interval (95 % CI). Major reasons for exclusion of studies were as follows: (1) not for prostate cancer research; (2) only case population; (3) duplicate of previous publication; and (4) the distribution of genotypes among controls is not in Hardy–Weinberg equilibrium (P < 0.01).
Data extraction
The eligible data were extracted by two investigators, and consensus was reached by discussion. Some important information was extracted from each study: first author’s name, year of publication, ethnicity, sample size of cases and controls, numbers of cases and controls with the Leu/Leu, Leu/Pro, and Pro/Pro genotypes, and genotyping methods. The different ethnic descents were categorized as African, Asian, and Caucasian.
Statistical analysis
OR with 95 % CI was used to measure the strength of association of the TGFβ1 Leu10Pro polymorphism with glioma risk. The significance of the pooled OR was determined by the z test (P < 0.05). Hardy–Weinberg equilibrium in the control group was tested using the Pearson chi-square test for goodness of fit; P < 0.05 was considered significant. We evaluated the risk using the homozygote model (Pro/Pro vs. Leu/Leu), heterozygote model (Leu/Pro vs. Leu/Leu), dominant model [(Pro/Pro + Leu/Pro) vs. Leu/Leu], recessive model [Pro/Pro vs. (Leu/Pro + Leu/Leu)], and allele comparison model (Pro-allele vs. Leu-allele). We also carried out the stratified analysis by ethnicity. Heterogeneity was evaluated with a chi-square-based Q test among the studies (P < 0.10 was considered significant) [16, 17]. When the heterogeneity was present, the random effects model was used to calculate the pooled OR [18], whereas the fixed effects model was used in its absence [19]. Heterogeneity was also explored using subgroup analysis with ethnic groups (African, Asian, and Caucasian). Sensitivity analysis was performed to assess the stability of results. Funnel plots were drawn to estimate the potential publication bias, in which the standard error of log (OR) of each study was plotted against its log (OR). The funnel plot asymmetry was assessed with Egger’s test [20]. Publication bias was assessed with Egger test; P < 0.05 was considered statistically significant. All statistical tests for this meta-analysis were performed with STATA version 12.0 (Stata Corporation, College Station, TX).
Results
Characteristics of included studies
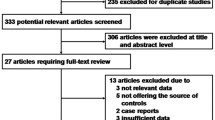
A total of 13 potentially relevant papers were identified based on the search strategy. However, only six studies from five papers with 2,604 cases and 3,129 controls were finally included into this meta-analysis [11–15]. The characteristics of the included studies are listed in Table 1. Among those total six studies, four studied the Caucasian population [11, 13–15], and the other two studied the Asian and African populations, respectively [12, 14]. There were two different studies with different ethnic population research in one paper [14]. The patients with PC were confirmed histologically or pathologically in most studies. Genotyping methods all were polymerase chain reaction-restriction fragment length polymorphism.
Quantitative synthesis
We conducted this present meta-analysis on the association between TGFβ1 Leu10Pro polymorphism and PC risk. Overall, the TGFβ1 Leu10Pro polymorphism was found to be significantly associated with increased risk of PC under allele comparison model (OR = 1.081, 95 % CI = 1.003–1.165, P heterogeneity = 0.141, P = 0.041, Fig. 1). To avoid the influence of heterogeneity among the included studies, subgroup analyses were distinctively carried out according to the ethnicity. In the stratified analysis by ethnicity, significantly increased risks were found among Caucasians (for heterozygote model, OR = 1.741, 95 % CI = 1.004–3.020, P heterogeneity = 0.000, P = 0.049, Fig. 2; recessive model, OR = 1.339, 95 % CI = 1.045–1.717, P heterogeneity = 0.020, P = 0.021, Fig. 3; allele comparison model, OR = 1.091, 95 % CI = 1.005–1.184, P heterogeneity = 0.048, P = 0.037, Fig. 4), while there was no significant association was found under the other genetic models.
Sensitivity analysis
To test the stability of the pooled results, one-way sensitivity analyses were performed. In the sensitivity analysis, a single study involved in the meta-analysis was deleted each time to reflect the influence of the individual data set to the pooled ORs, no other single study influenced the pooled OR qualitatively, suggesting that the results of this meta-analysis were stable (Fig. 5).
Publication bias
Begger’s funnel plot and Egger’s test were performed to assess the publication bias. The shape of funnel plots did not reveal any evidence of funnel plot asymmetry. The statistical results still did not show publication bias (P = 0.573 for allele comparison model, Fig. 6). Egger’s test was also performed to further assess the publication bias (P = 0.521 for allele comparison model, Fig. 7).
Discussion
The cytokine TGFβ1, which induces cell proliferation and apoptosis, plays a key role in various types of cancers, including PC. Genetic susceptibility to cancers has led to growing attention to the studies of polymorphism genes involved in carcinogenesis. Among different polymorphisms of TGFβ1, the Leu10Pro polymorphism is one of the most widely studied. However, there has been a continuing debate over the association between the TGFβ1 Leu10Pro polymorphism and PC susceptibility. Simultaneously, most of these studies have generally been underpowered to draw a convincing conclusion. Compared with a single study, a meta-analysis is a very useful tool by pooling data from all eligible studies. It can get a more precise estimate of gene–disease associations by improving the statistical power through the data combination. There are many studies investigating the association between TGFβ1 Leu10Pro polymorphism and PC risk, but studies from Asian countries report inconsistent findings. Therefore, we performed this meta-analysis to investigate this association.
Previous study indicated that TGFβ critically regulates androgen dependence in the prostate and contributes to the progression of prostate cancer by promoting the resistance of prostate cancer cells to inhibitory hormonal growth signals [21]. TGFβ1 itself may promote changes in the cellular environment to the advantage of the tumor, including suppression of the immune system, promotion of angiogenesis and extracellular matrix formation, and increased tumor cell plasticity that enhances invasion and metastasis [11]. The present meta-analysis, based on six studies from five publications with 2,604 cases and 3,129 controls included, explored the association between TGFβ1 Leu10Pro polymorphism and PC risk. We found that the TGFβ1 Leu10Pro polymorphism was significantly associated with PC risk. Simultaneously, the same results presented in stratified analysis by ethnicity.
Some limitations of this meta-analysis should be acknowledged. Firstly, the number of cases and controls in the included studies was not enough. Secondly, our result was based on unadjusted estimates, while a more precise analysis should be conducted adjusted by other factors like diet habit, smoking, drinking status, environmental factors, and so on. Thirdly, in the subgroup analyses by ethnicity, relatively limited study number made it impossible to perform ethnic subgroup analysis of Asians and African populations. Fourth, additional studies are warranted to evaluate the effect of this functional polymorphism on PC risk in different ethnicities, especially in Asians and Africans. In addition, our analysis did not consider the interactions among gene–gene, gene–environment, and even different polymorphism loci of the same gene may regulate the gene expression, affect the function of gene product, and lead to the different OR values. Because the original information was inadequate, assessment of potential interactions is limited. A more precise analysis should be conducted if special information listed above is provided for further evaluation.
In conclusion, this meta-analysis suggests that the TGFβ1 Leu10Pro polymorphism increased the risk of PC. However, larger and well-designed trials, which use standardized, unbiased-matched homogeneous patients and well-matched controls, with the assessors blinded to the data, should be conducted to re-evaluate the relationship. Gene–gene and gene–environment interactions should also be considered in future analyses, which could lead to better understanding of the association between the TGFβ1 Leu10Pro polymorphism and PC risk.
References
Hsing AW, Chokkalingam AP. Prostate cancer epidemiology. Front Biosci. 2006;11:1388–413.
Miyazono K, Suzuki H, Imamura T. Regulation of TGF-beta signaling and its roles in progression of tumors. Cancer Sci. 2003;94(3):230–4.
Blobe GC, Schiemann WP, Lodish HF. Role of transforming growth factor beta in human disease. N Engl J Med. 2000;342:1350–8.
Boesen CC, Radaev S, Motyka SA, Patamawenu A, Sun PD. The 1.1 A crystal structure of human TGF-beta type II receptor ligand binding domain. Structure. 2002;10:913–9.
Grainger DJ, Heathcote K, Chiano M, Snieder H, Kemp PR, Metcalfe JC, et al. Genetic control of the circulating concentration of transforming growth factor type beta1. Hum Mol Genet. 1999;8:93–7.
Ravitz MJ, Wenner CE. Cyclin-dependent kinase regulation during G1 phase and cell cycle regulation by TGF-beta. Adv Cancer Res. 1997;71:165–207.
Wikstrom P, Damber J, Bergh A. Role of transforming growth factor-beta1 in prostate cancer. Microsc Res Tech. 2001;52:411–9.
Barrack ER. TGF beta in prostate cancer: a growth inhibitor that can enhance tumorigenicity. Prostate. 1997;31:61–70.
Fujii D, Brissenden JE, Derynck R, Francke U. Transforming growth factor beta gene maps to human chromosome 19 long arm and to mouse chromosome 7. Somat Cell Mol Genet. 1986;12:281–8.
Yokota M, Ichihara S, Lin TL, Nakashima N, Yamada Y. Association of a T29/C polymorphism of the transforming growth factor-beta1 gene with genetic susceptibility to myocardial infarction in Japanese. Circulation. 2000;101:2783–7.
Ewart-Toland A, Chan JM, Yuan J, Balmain A, Ma J. A gain of function TGF-B1 polymorphism may be associated with late stage prostate cancer. Cancer Epidemiol Biomarkers Prev. 2004;13:759–64.
Faria PC, Saba K, Neves AF, Cordeiro ER, Marangoni K, Freitas DG, et al. Transforming growth factor-beta 1 gene polymorphisms and expression in the blood of prostate cancer patients. Cancer Investig. 2007;25:726–32.
Kang D, Lee KM, Park SK, Berndt SI, Peters U, Reding D, et al. Functional variant of manganese superoxide dismutase (SOD2 V16A) polymorphism is associated with prostate cancer risk in the prostate, lung, colorectal, and ovarian cancer study. Cancer Epidemiol Biomarkers Prev. 2007;16:1581–6.
Li Z, Habuchi T, Tsuchiya N, Mitsumori K, Wang L, Ohyama C, et al. Increased risk of prostate cancer and benign prostatic hyperplasia associated with transforming growth factor-beta 1 gene polymorphism at codon10. Carcinogenesis. 2004;25:237–40.
Meyer A, Dork T, Bogdanova N, Brinkhaus MJ, Wiese B, Hagemann J, et al. TGF-b1 gene polymorphism Leu10Pro (c.29T/C), prostate cancer incidence and quality of life in patients treated with brachytherapy. World J Urol. 2008. doi:10.1007/s00345-008-0354-0.
Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med. 1997;127:820–6.
Berman NG, Parker RA. Meta-analysis: neither quick nor easy. BMC Med Res Methodol. 2002;2:10.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–48.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Danielpour D. Functions and regulation of transforming growth factor-beta (TGF-beta) in the prostate. Eur J Cancer. 2005;41:846–57.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Qiliang Cai and Yang Tang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Cai, Q., Tang, Y., Zhang, M. et al. TGFβ1 Leu10Pro polymorphism contributes to the development of prostate cancer: evidence from a meta-analysis. Tumor Biol. 35, 667–673 (2014). https://doi.org/10.1007/s13277-013-1092-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-013-1092-5