Abstract
The prognosis for ovarian metastasis of gastric cancer is poor. There is no currently available treatment for this disease. The purpose of this study was to evaluate the efficacy and safety of hyperthermic intraperitoneal chemotherapy (HIPEC) after cytoreductive surgery (CRS) in female gastric cancer patients with metachronous ovarian metastasis. From January 2000 to December 2010, 62 patients developed ovarian metastasis after undergoing gastrectomy with D2 lymphadenectomy. Thirty-two patients underwent CRS plus HIPEC, and 30 patients underwent CRS alone. The median age of all 62 patients was 44 years (range 19–71 years). Metastatic carcinoma involving bilateral ovaries was observed in 50 patients (80.6 %). The median survival time in the CRS + HIPEC group was 15.5 months (95 % confidence interval [CI] 12.1–18.9 months) but was only 10.4 months (95 % CI 8.5–12.2 months) in the CRS group (P = 0.018). Among the 32 patients with pelvic peritoneal metastasis, a stratified analysis revealed that the median survival period for the 15 patients treated with CRS + HIPEC was significantly higher than that for the patients treated with CRS alone (P = 0.046). Among the 30 patients who suffered from ovarian metastasis alone, the median survival times were similar in both groups (P = 0.141). A multivariate analysis revealed that CRS + HIPEC and a low Peritoneal Cancer Index (PCI) were independent predictors for improved survival. In conclusion, our study indicates that employing the HIPEC procedure after CRS could improve the survival time of patients with ovarian metastasis with few complications; however, we do not recommend HIPEC treatment for ovarian metastasis alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the fourth most common cancer in the world and is the leading cause of cancer-related deaths in China [1]. In China, gastric cancer is usually diagnosed at an advanced stage. The quality of treatment for patients with gastric cancer has improved dramatically in the past decade to include techniques such as gastrectomy with D2 lymphadenectomy, neoadjuvant chemotherapy regimens, and new targeted drugs. However, many patients are diagnosed at advanced stages with synchronous or metachronous metastases in the peritoneum, ovary, and liver [2, 3]. The prognosis of these patients is extremely poor even after surgery and chemotherapy.
Particularly among women, cancers of the gastrointestinal tract are most likely to give rise to ovarian metastases (Krukenberg's tumors); ovarian metastasis is common and is one of the most important causes of treatment failure. It was originally thought that the cancer cells drifted across the abdomen to the ovaries, but there is now evidence that these cells can also be transported in the blood or lymph [4]. It has been reported in previous studies that only surgery could improve the prognosis of these patients [5–7]. Other scholars have suggested that young female patients with gastric cancer who have multiple regional lymph node metastases should be treated with prophylactic oophorectomy [8, 9]. However, this opinion has not been widely accepted because no large, prospective, randomized clinical studies have been conducted.
In our hospital, we performed cytoreductive surgery (CRS) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) in patients with metachronous ovarian metastasis. The goal of this study was to evaluate the safety and the survival benefit of CRS plus HIPEC for gastric cancer patients with metachronous ovarian metastasis.
Patients and methods
Patients
From January 2000 to December 2010, 62 patients developed ovarian metastasis after undergoing gastrectomy with D2 lymphadenectomy at the Department of Gastrointestinal Surgery at Beijing Cancer Hospital in Beijing, China. All cases were retrospectively reviewed. All the patients with gastric cancer had a pathological diagnosis before surgery and no clinical or radiological evidence of distant metastasis. Among this group, 32 suffered simultaneously from pelvic peritoneal dissemination. Of these 62 patients, 32 were treated with CRS and HIPEC, whereas the other 30 were treated with CRS alone. Because HIPEC is an exploratory therapy with uncertain consequences, the patients either accepted or refused treatment with CRS plus HIPEC, based on patients individual situations after consultation.
Surgery and HIPEC
Each patient underwent CRS, which included the resection of the ovarian metastasis, peritonectomy for simultaneous pelvic peritoneal metastasis (n = 32), and unilateral salpingo-oophorectomy (n = 12) or bilateral salpingo-oophorectomy (n = 50), based on their clinical diagnosis and according to the procedure developed by Sugarbaker. After peritonectomy, the resection status of the patients was scored using the Peritoneal Cancer Index (PCI), as described by Jacquet and Sugarbaker [10]. The PCI quantitatively determines the distribution and implant size of the cancer throughout 13 abdominopelvic regions, of which four refer to the small bowel (regions 9 and 10 define the upper and lower portions of the jejunum, and regions 11 and 12 define the upper and lower portions of the ileum). Each of these regions was assigned a score from 0 to 3 based on the size and extent of the tumor implants. The sum of each region's numerical score yielded the PCI total score, which varied from 1 to 39. After surgery, 32 patients underwent HIPEC.
HIPEC was performed after resection using three drainage tubes that were placed in the abdominal cavity. Approximately 3–4 L of heated 5 % glucose containing oxaliplatin was circulated for 60 min (460 mg/m2). The abdomen was gently rocked to distribute the drug evenly throughout the abdominal cavity. One outflow tube for perfusion was placed in Douglas's pouch, and the other tube was placed in the pelvis. The inflow tube was placed subphrenically. The heated perfusion solution was infused into the peritoneal cavity at a rate of 500–800 mL/min through the inflow tube, which was introduced by an automatic hyperthermia perfusion device (RHL-2000B, Madain Medical Devices Co., Ltd., Jilin, China). The temperature of the perfusate in the inflow tube and outflow tube was monitored in real time. The temperature of the perfusion solution in the peritoneal space was maintained at 43.0 ± 0.5 °C. The inflow and outflow temperature curves were stored in the device. After the HIPEC procedures were completed, as much fluid as possible was removed from the abdominal cavity.
Statistical analysis
Clinical follow-up was performed by calling the patients and by accessing outpatient records. The median follow-up period was 11 months (2.8–28.2 months). The overall survival was defined as the period between the date of surgery and either the date of the last follow-up or the date of death. A death due to ovarian metastasis was considered to be an endpoint event. Patients who were still alive at the time of the last follow-up, who died of other causes, or with whom we lost contact were excluded from the study.
All the statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) software (version 18.0; SPSS Inc., Chicago, IL, USA). The demographic and clinical characteristics of the patients in both groups were compared using a two-tailed Student's t test for the continuous variables and a chi-square test for the discrete variables. Overall survival curves were estimated using the Kaplan–Meier method. The differences in survival between the two groups were assessed using a log-rank test. Additionally, the Cox proportional hazards regression model was used in a stepwise fashion to perform a multivariate analysis of the clinical factors to determine an overall model of independent predictors of OS. For all the analyses, the significance level was specified as P < 0.05.
Results
Patient characteristics
All the patients underwent CRS treatment, and HIPEC procedures were performed on 32 patients (51.6 %). The median age of all 62 patients at the time of treatment was 44 years (range 19–71 years). Metastasis involving both ovaries was observed in 50 patients (80.6 %). The operation revealed metastatic deposits on the pelvic peritoneum in 32 patients; subsequently, 15 patients underwent HIPEC (Table 1). The clinicopathological characteristics of primary gastric cancer are listed in Table 2. The tumor location, differentiation, depth of invasion, status of lymph node metastases, and TNM (tumor, lymph node, and metastasis) stage were similar between the two groups.
Surgical results
All the cases of ovarian metastasis and pelvic peritoneal metastasis of gastric cancer were confirmed by pathology. In the present study, we found pelvic peritoneal metastases that simultaneously occurred in 32 patients. Of these 32 patients, we defined PCI < 16 (n = 14) as a low PCI and PCI ≥ 16 (n = 18) as a high PCI after CRS for the quantitative evaluation of the cytoreductive status.
Adverse effects of HIPEC
No patients died from surgery-related complications. Furthermore, there were no significant differences between the HIPEC and non-HIPEC groups in the incidence of grades III and IV toxicities (P = 0.56). No hepatic or renal dysfunction or hematological toxicities were found in the HIPEC group; three patients exhibited severe vomiting but recovered following antiemetic treatment within 3 days after HIPEC. All the patients suffered from varying degrees of abdominal pain, but their pain was adequately controlled by medication.
Survival and follow-up
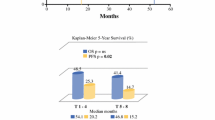
As displayed in Fig. 1, the CRS + HIPEC group experienced a significantly longer survival time than did the CRS-alone group. The median survival time in the CRS + HIPEC group was 15.5 months (95 % CI 12.1–18.9 months), compared with 10.4 months (95 % CI 8.5–12.2 months) in the group that was treated with CRS alone (P = 0.018). A further stratified analysis revealed that the median survival period of the 15 patients with pelvic peritoneal dissemination who underwent CRS + HIPEC was significantly higher than that of the patients who were treated with CRS only (10.1 vs. 7.4 months, P = 0.046, Fig. 2). Among the 30 patients who suffered from ovarian metastasis alone, the median survival time was similar between those patients treated with CRS + HIPEC and those patients treated with CRS alone (21.9 months with 95 % CI 18.9–24.9 months vs. 18.8 months with 95 % CI 14.1–23.4 months, respectively) (P = 0.141). The prognostic value of PCI after CRS on survival was also demonstrated; the median survival times of the patients with low PCIs and high PCIs after CRS were 10.4 months (95 % CI 9–11.9 months) and 7.4 months (95 % CI 5.2–9.6 months), respectively (P = 0.002, Fig. 3).
Multivariate analysis using the Cox regression model identified HIPEC and a low PCI as the major independent predictors for improved survival, whereas the menstrual status, chemotherapy cycles, and tumor size were not independent survival factors (Table 3). Compared with CRS alone, CRS + HIPEC was approximately three times more likely to improve survival (hazard ratio = 2.996; 95 % CI 1.245–7.208).
Discussion
Krukenberg's tumor was first reported in 1896 by Freidrich Ernst Krukenberg [11]. The World Health Organization (WHO) established the diagnostic standard in 1973 as follows: (1) the presence of a tumor in the ovary, (2) evidence of intracellular mucin secretions in the form of signet cells, and (3) diffuse infiltration of stroma yielding a sarcomalike appearance, which is the diagnostic standard that has been applied until recently [12]. According to this definition, Krukenberg's tumor can originate in various organs, such as the breast, esophagus, stomach, colorectal tissue, gallbladder, pancreas, small intestine, appendix, and lung. Notably, the stomach is the most common primary source [13]. Previous studies revealed that the frequency of ovarian metastasis varies from 2.7 % to 6.7 % among female patients who have undergone gastrectomy [5, 9, 14]. The present study indicates that retrograde lymphatic spread is the most likely route of metastasis of gastric carcinoma to the ovaries; other theories include implantation and hematogenous metastasis [4].
The prognosis of patients with ovarian metastasis is uniformly poor. Cheong et al. [5] reported the median survival time as 17 months among 33 patients with ovarian metastasis who underwent resection, which was significantly longer than the median survival time in the nonresection group (P < 0.001). Jiang et al. [6] reviewed a series of 54 patients with cancers that metastasized to the ovary. The estimated 5-year survival rate was 12.1 %; the median survival time among patients with microscopic residual disease after metastasectomy was 29.6 months, compared with 10 months among those patients with visible residual disease (P < 0.01). The treatment of ovarian metastasis of gastric cancer remains frustrating. Many physicians have considered surgery to be the main treatment of ovarian metastases from gastric cancer [5–7].
In the present study, we retrospectively analyzed the outcomes of 62 patients with ovarian metastasis. Our results demonstrated that the patients treated with CRS + HIPEC exhibited significantly longer survival times than did those patients who were treated with CRS alone. The median survival time of the patients treated with CRS + HIPEC was 15.5 months (95 % CI 12.1–18.9 months), compared with 10.4 months (95 % CI 8.5–12.2 months) for the patients treated with CRS alone (P = 0.018). These findings indicate that HIPEC could improve the survival of patients with ovarian metastasis.
Currently, there is no standard treatment for ovarian metastasis when it presents with peritoneal metastases from gastric cancer. Although the prognosis is very poor, the use of CRS in combination with HIPEC is gaining popularity [15–17]. Dr. Fujimoto first reported this method in 1988 [18] after the technique was applied in 15 patients with peritoneal seeding, five of whom also presented with ovarian metastasis. These patients were treated surgically followed by an intraperitoneal hyperthermic perfusion with mitomycin C and misonidazole. The mean survival time was 7.2 ± 4.6 months, with an acceptable rate of adverse events.
Li et al. [19] reported that gastric cancer patients with single peritoneal disseminations who underwent CRS plus HIPEC had significantly longer survival times than did their counterparts who were treated with resection alone. A multivariate analysis revealed that HIPEC was an independent prognostic factor. The multivariate survival analysis in the present study also suggested that HIPEC and a low PCI could improve survival times. Yang et al. [20] reported on 68 peritoneal carcinomatosis (PC) patients who were randomized to treatment with CRS alone (n = 34) or CRS + HIPEC (n = 34) as well as cisplatin and mitomycin C. The median survival times were 6.5 months and 11.0 months, respectively (P = 0.046). In the present study, we identified 32 patients who were diagnosed with Krukenberg's tumor in combination with pelvic peritoneal dissemination. The median survival time of these 32 patients was 9.4 months. We attempted to use the HIPEC with oxaliplatin method to improve the survival times of these patients. Oxaliplatin is a third-generation platinum anticancer drug that has demonstrated a wide spectrum of antitumor activities. At present, several phase II or III trials have confirmed the activity of oxaliplatin in various combinations with 5-FU/S-1/capecitabine and/or leucovorin in advanced or metastatic gastric cancer [21–24]. Fifteen patients underwent CRS plus HIPEC; among these patients, the median survival time was 10.1 months, which was significantly higher than the rates observed among those treated with CRS alone (7.4 months, P = 0.046). These results were similar to the data reported by Glehen et al. [25, 26] (OS 9.2 months).
There is a synergistic effect between hyperthermia and chemotherapeutic drugs [27]. First, heat is more toxic to cancerous tissue than to normal tissue. Second, hyperthermia increases the penetration of chemotherapeutic drugs into tissues. Finally, and perhaps most importantly, heat increases the cytotoxicity of certain chemotherapeutic agents. The most interesting finding from the present study suggests that the survival difference between the patients treated with CRS alone and the patients treated with CRS plus HIPEC was significant among the patients with synchronous peritoneal dissemination (P = 0.046). Furthermore, in our research, we found that 30 patients had ovarian metastasis without evidence of other distant metastases; of these, 13 patients who underwent surgery in combination with HIPEC exhibited survival times that were not significantly different than the survival times yielded from surgery alone (median OS 21.9 months vs. 18.8 months, P = 0.141). This result may be related to the method of spread of the gastric cancer to the ovary. Recently, retrograde lymphatic spread has been reported to be a likely route for metastasis. Cancer cells block the lymphatic uplink path and are transferred to the paraaortic and pelvic lymph nodes along the lymphatic reflux. The ovary is an organ with a rich network of lymphatic vessels. Kakushima [28] reported that eight patients with early-stage gastric cancer developed ovarian metastasis. Because the height of the gastric mucosa is significantly reduced in patients with early-stage gastric cancer and because the gastric mucosa and submucosa contain a rich lymphatic plexus, the lymphatic capillaries may be located near the surface epithelium. Consequently, cancer cells in the mucosa could easily infiltrate the lymphatic vessels and thus lead to ovarian metastasis. Therefore, HIPEC may not be an effective treatment for active ovarian metastases from gastric cancer.
In agreement with other studies [29], our results confirmed that the patients with PCI < 16 after CRS could achieve better prognoses. Therefore, according to the principles of individual treatment, patients with complete or nearly complete CRS can be considered for treatment with HIPEC.
A previous study has revealed potential complications of HIPEC in combination with CRS. These adverse effects include anastomotic leakage, hepatic or renal dysfunction, hematological toxicity, fever, intestinal obstruction, bleeding, deep vein thrombosis, chemical peritonitis, vomiting, and abdominal abscess [30]. There were no significant differences in severe surgical complications between the HIPEC and non-HIPEC groups (P = 0.56). In the HIPEC group, there were no grades III and IV hematological, hepatic, and renal toxicities. Our results suggest that HIPEC with oxaliplatin is safe for patients undergoing CRS.
The present study demonstrated that the HIPEC procedure, when performed after CRS, could potentially improve the survival times of patients with ovarian metastasis, yielding only minor complications, especially among patients with synchronous peritoneal dissemination. This study had certain limitations because it was a retrospective analysis involving relatively few cases. Nonetheless, the results of this research were encouraging although no definitive conclusion was reached regarding the therapeutic activity of this locoregional treatment. In the absence of effective systemic agents, the therapeutic potential of CRS plus HIPEC should be further explored using a large number of prospective, randomized clinical trials.
References
Chen WQ, Zhang SW, Zou XN, et al. Cancer incidence and mortality in China, 2006. Chin J Cancer Res. 2011;23(1):3–9.
Kim HK, Heo DS, Bang YJ, Kim NK. Prognostic factors of Krukenberg's tumor. Gynecol Oncol. 2001;82(1):105–9.
Kiyokawa T, Young RH, Scully RE. Krukenberg tumors of the ovary: a clinicopathologic analysis of 120 cases with emphasis on their variable pathologic manifestations. Am J Surg Pathol. 2006;30(3):277–99.
Deslauriers N, Olney H, Younan R. Splenectomy revisited in 2011: impact on hematologic toxicities while performing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Gastrointest Oncol. 2011;2(2):61–3.
Cheong JH, Hyung WJ, Chen J, Kim J, Choi SH, Noh SH. Survival benefit of metastasectomy for Krukenberg tumors from gastric cancer. Gynecol Oncol. 2004;94(2):477–82.
Jiang R, Tang J, Cheng X, Zang RY. Surgical treatment for patients with different origins of Krukenberg tumors: outcomes and prognostic factors. Eur J Surg Oncol. 2009;35(1):92–7.
Jun SY, Park JK. Metachronous ovarian metastases following resection of the primary gastric cancer. J Gastric Cancer. 2011;11(1):31–7.
Yook JH, Oh ST, Kim BS. Clinical prognostic factors for ovarian metastasis in women with gastric cancer. Hepatogastroenterology. 2007;54(75):955–9.
Kim NK, Kim HK, Park BJ, Kim MS, Kim YI, Heo DS, et al. Risk factors for ovarian metastasis following curative resection of gastric adenocarcinoma. Cancer. 1999;85(7):1490–9.
Lu TP, Tsai MH, Hsiao CK, Lai LC, Chuang EY. Expression and functions of semaphorins in cancer. Transl Cancer Res. 2012;1(2):74–87.
Krukenberg F. Uber das fibrosarcoma ovarii mucocellulase (carcinomatoses). Arch Gynecol Obstet. 1896;50:287–321.
Serov SF, Scully RE, Sobin LH. International histological classification of tumors. No 9. Histological Typing of Ovarian Tumors. Geneva: WHO; 1973. p. 17–54.
Yada-Hashimoto N, Yamamoto T, Kamiura S, Seino H, Ohira H, Sawai K, et al. Metastatic ovarian tumors: a review of 64 cases. Gynecol Oncol. 2003;89(2):314–7.
Kobayashi O, Sugiyama Y, Cho H, Tsuburaya A, Sairenji M, Motohashi H, et al. Clinical and pathological study of gastric cancer with ovarian metastasis. Int J Clin Oncol. 2003;8(2):67–71.
Glehen O, Mohamed F, Gilly FN. Peritoneal carcinomatosis from digestive tract cancer: new management by cytoreductive surgery and intraperitoneal chemohyperthermia. Lancet Oncol. 2004;5(4):219–28.
Sugarbaker PH, Stuart OA, Bijelic L. Intraperitoneal gemcitabine chemotherapy as an adjuvant treatment for patients with resected pancreatic cancer: phase II and pharmacologic studies. Transl Gastrointest Cancer. 2012;1(2):161–8.
Yan TD, Black D, Sugarbaker PH, Zhu J, Yonemura Y, Petrou G, et al. A systematic review and meta-analysis of the randomized controlled trials on adjuvant intraperitoneal chemotherapy for resectable gastric cancer. Ann Surg Oncol. 2007;14(10):2702–13.
Fujimoto S, Shrestha RD, Kokubun M, Ohta M, Takahashi M, Kobayashi K, et al. Intraperitoneal hyperthermic perfusion combined with surgery effective for gastric cancer patients with peritoneal seeding. Ann Surg. 1988;208(1):36–41.
Li C, Yan M, Chen J, Xiang M, Zhu ZG, Yin HR, et al. Surgical resection with hyperthermic intraperitoneal chemotherapy for gastric cancer patients with peritoneal dissemination. J Surg Oncol. 2010;102(5):361–5.
Yang XJ, Huang CQ, Suo T, Mei LJ, Yang GL, Cheng FL, et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy improves survival of patients with peritoneal carcinomatosis from gastric cancer: final results of a phase III randomized clinical trial. Ann Surg Oncol. 2011;18(6):1575–81.
Bang YJ, Kim YW, Yang HK, Chung HC, Park YK, Lee KH, et al. Adjuvant capecitabine and oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): a phase 3 open-label, randomised controlled trial. Lancet. 2012;379(9813):315–21.
Bouchereau M, Gervais M, Sideris L, Loriot M, Ahern S, Dubé P. Hepatic necrosis and hemorrhage following hyperthermic intraperitoneal chemotherapy with oxaliplatin: a review of two cases. J Gastrointest Oncol. 2011;2(2):113–6.
Park SR, Kong SY, Rhee J, Park YI, Ryu KW, Lee JH, et al. Phase II study of a triplet regimen of S-1 combined with irinotecan and oxaliplatin in patients with metastatic gastric cancer: clinical and pharmacogenetic results. Ann Oncol. 2011;22(4):890–6.
Al-Batran SE, Hartmann JT, Probst S, Schmalenberg H, Hollerbach S, Hofheinz R, et al. Phase III trial in metastatic gastroesophageal adenocarcinoma with fluorouracil, leucovorin plus either oxaliplatin or cisplatin: a study of the Arbeitsgemeinschaft Internistische Onkologie. J Clin Oncol. 2008;26(9):1435–42.
Glehen O, Gilly FN, Arvieux C, Cotte E, Boutitie F, Mansvelt B, et al. Peritoneal carcinomatosis from gastric cancer: a multi-institutional study of 159 patients treated by cytoreductive surgery combined with perioperative intraperitoneal chemotherapy. Ann Surg Oncol. 2010;17(9):2370–7.
Glehen O, Gilly FN, Boutitie F, Bereder JM, Quenet F, Sideris L, et al. Toward curative treatment of peritoneal carcinomatosis from nonovarian origin by cytoreductive surgery combined with perioperative intraperitoneal chemotherapy: a multi-institutional study of 1,290 patients. Cancer. 2010;116(24):5608–18.
Esquivel J. Technology of hyperthermic intraperitoneal chemotherapy in the United States, Europe, China, Japan, and Korea. Cancer J. 2009;15(3):249–54.
Kakushima N, Kamoshida T, Hirai S, Hotta S, Hirayama T, Yamada J, et al. Early gastric cancer with Krukenberg tumor and review of cases of intramucosal gastric cancers with Krukenberg tumor. J Gastroenterol. 2003;38(12):1176–80.
Elias D, Blot F, Otmany A El, Antoun S, Lasser P, Boige V, et al. Curative treatment of peritoneal carcinomatosis arising from colorectal cancer by complete resection and intraperitoneal chemotherapy. Cancer. 2001;92(1):71–6.
Piso P, Slowik P, Popp F, Dahlke MH, Glockzin G, Schlitt HJ. Safety of gastric resections during cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis. Ann Surg Oncol. 2009;16(8):2188–94.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Xiao-Jiang Wu and Peng Yuan contributed equally to this study.
Rights and permissions
About this article
Cite this article
Wu, XJ., Yuan, P., Li, ZY. et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy improves the survival of gastric cancer patients with ovarian metastasis and peritoneal dissemination. Tumor Biol. 34, 463–469 (2013). https://doi.org/10.1007/s13277-012-0571-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-012-0571-4