Abstract
Non-Hodgkin’s lymphoma of mucosa-associated lymphoid tissue (MALT) type arises from a wide variety of extranodal sites, most frequently from the gastrointestinal tract. Recently, it has been demonstrated that karyotypic alterations involving the PIK3CA and FOXP1 genes of chromosome 3 occur in MALT lymphoma. However, their associated protein expression has not been extensively studied. Tumor tissues from 27 gastric and 23 intestinal MALT lymphomas were analyzed for PIK3CA and FOXP1 protein expression using immunohistochemistry and correlated with histological features and treatment outcomes. Expression of PIK3CA, a novel indicator, was found in 40% of gastrointestinal cases and indicated an inferior progression-free survival in both gastric and intestinal MALT lymphomas (P = 0.001 and P = 0.015). Tumor staining of nuclear FOXP1 (46.0%) was more common in gastric than intestinal MALT lymphomas (P = 0.042) and was significantly associated with polymorphic histology (P = 0.007). FOXP1 expression was identified as an adverse prognostic factor for overall survival in gastric MALT lymphomas (P = 0.035). We further combined these two markers and observed that patients that are positive for both PIK3CA and FOXP1 had a worse overall and progression-free survival. Considering the small sample size of this study, these results should be confirmed in a large prospective study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-Hodgkin’s lymphoma (NHL) of mucosa-associated lymphoid tissue (MALT) type was first described by Isaacson and Wright in 1983 [1]. MALT lymphoma occurs in a number of anatomic sites, with the gastrointestinal tract being the most frequently involved organ [2]. This kind of lymphoma is relatively uncommon, accounting for approximately 7.6% of NHL [1]. Although MALT lymphoma is an indolent disease and responds well to frontline treatments, the relapse rate is still high with a life-long follow-up [3].
Cytogenetic data accumulated in recent years have enriched our knowledge about this disease. Aberrations of chromosome 3 have been recently described in MALT lymphoma, including allelic imbalance of the 3q26.2-27, t(3;14)(p14.1;q32) and trisomy of chromosome 3. High levels of amplification in the 3q26.2-27 region, which harbors the phosphoinositide-3-kinase, catalytic, α polypeptide (PIK3CA) gene, were observed in 21% of gastric MALT lymphomas [4]. The forkhead box protein P1 (FOXP1) gene at 3p14.1 is under the control of the IGH gene enhancer and deregulates FOXP1 expression in MALT lymphoma due to a t(3;14)(p14.1;q32) translocation [5]. In other reports, trisomy of chromosome 3 was found in MALT lymphoma, suggesting that an increased gene copy number may be another mechanism of deregulated gene expression [6–8]. Several studies indicated that the expression of FOXP1 was associated with tumor progression in diffuse large B cell lymphoma (DLBCL) [9, 10], and PIK3CA overexpression was correlated with a poor outcome in esophageal squamous cell carcinoma and ovarian cancer [11, 12]. Whether these observations are found in MALT lymphoma is unknown.
Histologically, the concurrent presence of large-cell (LC) and small-cell components are well-known features of indolent lymphoma and indicative of tumor transformation and progression [13–15]. However, the prognostic value of histological features has not been well described in MALT lymphoma. Prior to the WHO classification system of hematopoietic and lymphoid tissues in 2001 [16], “low-grade MALT” or “high-grade MALT” is still extensively used in many previous studies, and it remains difficult to identify and differentiate between MALT lymphoma and DLBCL with MALT components [17–19].
In the current study, we investigated the expressions of PIK3CA and FOXP1 and the histological features in 50 gastrointestinal MALT lymphomas. Considering the inherent differences in lymphoid tissue throughout the gastrointestinal tract, including native collections of lymphocytes such as Peyer’s patches in the intestine and acquired lymphoid tissues such as in gastritis [2], we further compared the distribution of PIK3CA and FOXP1 expression and histological features in gastric and intestinal MALT lymphomas and correlated them with treatment outcomes.
Materials and methods
Clinical data
Analyses of tumor tissues were performed of 50 patients with MALT lymphoma in the gastrointestinal tract treated during the period January 1999 through September 2007 at two affiliated hospitals of Sun Yat-sen Medical College, Guangzhou, China. Anatomical organs and other clinical information were collected for all patients: age, sex, stage, presence of systemic symptoms, LDH level, nodal or multifocal involvement, bulky disease, efficacy of initial treatment, and outcomes. Patients were staged according to the Lugano system [20]. Staging workup included physical examination, gastroscopy, enteroscopy, whole-body computed tomography scan and bilateral bone marrow aspiration or biopsy. After treatments, patients were followed up until death or May 2010.
Immunohistochemical analysis
A panel of antibodies against LCA, CD3, CD5, CD10, CD20, CD23, CD45RO, and cyclin D1, was performed to confirm the diagnosis of MALT lymphoma and exclude other small lymphocytic neoplasms. Sections with colonized follicles were stained by the Bcl-2 antibody to differentiate the infiltrated tumor cells and other cells in the germinal center. The antibody against CD3 was used to exclude the nonneoplastic T cells in the marginal zone. Only the staining of the interfollicular marginal zone neoplastic cells was scored. The presence of solid clusters (>20 cells), sheet-like proliferation of LC components outside colonized follicles, or >20% scattered LC components was considered as DLBCL and was an exclusion criteria [19, 21].
All cases were histologically stratified according to LC components (polymorphic histology with >5% LC versus monomorphic histology with <5% LC). Sections for an immunohistochemical analysis were stained using the DAKO EnVision+ System (DAKO, Carpinteria, CA, USA). As a control, four cases of reactive lymph node proliferation were included. Deparaffinized sections for PIK3CA staining were microwaved in 10 mmol/L of citrate buffer at pH 6.0, and sections for FOXP1 staining were treated with tris-ethylenediamine tetraacetic acid (Tris–EDTA) at pH 9.0. The slides were treated with 0.03% hydrogen peroxide for 5 min to block endogenous peroxidase before incubation with monoclonal antibodies to PIK3CA (catalog no. AP8016b; dilution, 1:80; ABGENT, San Diego, CA, USA) or FOXP1 (catalog no. NB 200–554; dilution, 1:80; Novus Biologicals, Littleton, CO, USA) for 30 min at room temperature (PIK3CA) or overnight at 4°C (FOXP1). Sections were incubated with peroxidase-labeled polymer conjugated to goat anti-mouse IgG for 20 min. Finally, the sections were stained for 20 min with diaminobenzidene chromogen and counterstained with Gill’s hematoxylin.
For negative controls, the appropriate primary antibody was omitted, and phosphate-buffered solution was applied. Sections from ovarian cancer specimens with known PIK3CA expression and from DLBCL specimens with known FOXP1 expression were used as positive control samples. The results of the immunohistochemical analysis were interpreted by two pathologists (QLW and HLL) without knowledge of the clinical information. After the assessments were finished, these two pathologists met to resolve contradictory results and reach final conclusions. The mean percentage of positive tumor cells in at least five areas at ×400 magnification was determined and assigned to one of five categories: (1) <10%, (2) 10% to 25%, (3) 25% to 50%, (4) 50% to 75%, and (5) >75%. Protein levels were defined as negative when 10% or fewer of the tumor cells was stained and positive when more than 10% of tumor cells was stained in the cytoplasm for PIK3CA [12]. Protein levels of FOXP1 were defined as positive when more than 25% of the tumor cells was stained [22, 23].
Statistical methods
The associations among clinical variables, histological subgroups, and expressed proteins were evaluated using the chi-square test. Overall survival (OS) was measured from the date of treatment to death (from any cause) or the date of the last contact. The progression-free survival (PFS) for all patients was taken from the time of treatment until disease progression or death or the date of the last follow-up. Survival curves were constructed according to the Kaplan–Meier method and compared using the log-rank test. A two-tailed P value of less than 0.05 was considered significant. The analysis was carried out using the SPSS 13.0 software (SPSS Inc., Chicago, IL, USA).
Results
Clinical findings
The primary sites included the stomach (n = 27), small intestine (n = 9), and large intestine (n = 14). Table 1 lists the patients’ features. Gastric and intestinal lymphoma occurrences were well balanced in terms of age, stage, multifocal or nodal involvement, and bulky disease. As initial treatments, 24 patients (48.0%), including 13 cases of the stomach, underwent surgery. Chemotherapy was given to 41 patients (82.0%, 23 in the stomach). The chemotherapy strategies included CHOP-like regimen (cyclophosphamide, vincristine, doxorubicin, and prednisone) in 30 cases, COP regimen (cyclophosphamide, vincristine, and prednisone) in five cases, R-CHOP regimen (rituximab followed by CHOP regimen) in three cases, and FND-like (fludarabine, mitoxantrone, and dexamethasone) in three cases. The median number of chemotherapy cycles given was four. Only three patients (6.0%, one gastric lymphoma) received radiation to the primary tumors and draining lymph nodes. A Helicobacter pylori infection was found in seven cases of the stomach. Of these, three patients with local lesions received H. pylori eradication treatment, and the other four cases with advanced lesions received chemotherapy as the initial treatment.
Follow-up data were available for all patients (median, 68.4 months; range, 6.8–167.0 months). Of the 50 patients, 36 (72.0%, 18 in the stomach) achieved a complete remission (CR) after initial treatment. At the time when the last survey was conducted, 11 patients (22.0%, nine gastric lymphomas) died of lymphoma dissemination (ten) and of tumor-unrelated disease (one). Relapses occurred in 19 cases (38.0%, 12 gastric lymphomas). The PFS and OS rates for all cases at 5 years were 65.9% and 81.5%, respectively.
Histological and immunohistochemical features
The main pathologic and immunohistochemical features of the 50 MALT lymphomas are summarized in Table 1. The diagnosis of MALT lymphoma was accounted for by 26 biopsies (52.0%) and 24 surgical samples (48.0%). Eleven cases (22.0%) were of polymorphic histology (Fig. 1), including eight gastric lymphomas and three intestinal lymphomas. Polymorphic histology was discovered in seven biopsies and four surgical tumors. No significant correlation was observed between the specimens (biopsy or surgery) examined and polymorphic histology (P = 0.382). In total, a positive cytoplasmic expression of PIK3CA was detected in 20 cases (40.0%), and a positive nuclear expression of FOXP1 was detected in 23 (46.0%) cases. It should be noted that FOXP1 nuclear expression was significantly different between gastric and intestinal lymphomas (59.3% vs. 30.4%; P = 0.042). Representative positive expressions of each protein are shown in Fig. 1.
Protein levels in relation to clinical variables and histological features
The relationship of 50 gastrointestinal MALT lymphomas associated with clinical variables and protein levels or histological features are shown in Table 2. Overall, nine of 11 polymorphic lymphomas (81.8%) were FOXP1-positive, whereas 14 of 39 tumors (35.9%) in the monomorphic histology group were FOXP1-positive. The difference was significant (χ 2 = 7.284; P = 0.007). FOXP1 positivity also had a trend to correlate with nodal involvement (χ 2 = 3.632; P = 0.057). No other significant relationships were found.
Histological features and protein levels in relation to treatment outcomes
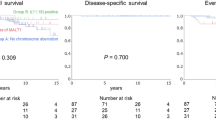
Among the 27 gastric lymphomas, patients in the FOXP1-positive group had a lower CR rate than those in the FOXP1-negative group (50.0% vs. 90.9%; P = 0.042, Fisher’s exact test). Histological features and PIK3CA expression were not associated with the CR rate. A univariate analysis indicated a significantly shorter 5-year OS (48.6%) in patients with high FOXP1 expression compared to those with negative expression (90.9%; χ 2 = 4.437, P = 0.035, Fig. 2). Other variables associated with a poor OS rate included polymorphic histology (χ 2 = 6.041; P = 0.014) and the Lugano stage IIE-IV (χ 2 = 5.733; P = 0.017). Patients with negative PIK3CA expression had a significantly longer 5-year PFS than those with positive PIK3CA expression (81.3% vs. 18.2%; χ 2 = 11.616, P = 0.001, Fig. 2). For 23 intestinal lymphomas, polymorphic histology was identified as a prognostic factor for OS (χ 2 = 6.67; P = 0.010). A significantly longer 5-year PFS (80.8%) was found in patients with negative PIK3CA expression compared to those with a positive expression (44.4%; χ 2 = 5.912, P = 0.015, Fig. 2). No other significant correlations were found between protein levels and treatment outcomes.
a Overall survival curves: positive vs. negative expression of FOXP1 in gastric MALT lymphoma. b Progression-free survival curves: positive vs. negative expression of PIK3CA in gastric MALT lymphoma. c Progression-free survival curves: positive vs. negative expression of PIK3CA in intestinal MALT lymphoma
In this study, PIK3CA and FOXP1 expression were associated with patients’ exhibiting poor prognosis. As a result, we grouped the patients into two categories: PIK3CA and FOXP1 positive, and all others. The 5-year OS and PFS of gastric lymphoma patients with double negative PIK3CA and FOXP1 expression was 88.9% and 71.8%, respectively, while it was 41.7% and 22.2% for the other patients (P = 0.007 and P = 0.005). Patients with intestinal lymphomas exhibiting double positive PIK3CA and FOXP1 expression had a poorer OS and PFS (66.7% vs. 90.9% and 33.3% vs. 71.7%, P = 0.010 and P = 0.085).
Discussion
The phosphatidylinositol 3-kinase (PI3K)/AKT pathway mediates key cellular functions, including growth, proliferation, survival, angiogenesis, and motility [24]. Studies have showed that the PI3K/AKT pathway is activated in DLBCL and contributed to the pathogenesis of mantle cell lymphoma [25, 26]. For MALT lymphoma, deletion of two downstream targets of the PI3K/AKT pathway, PTEN and SHIP, resulted in spontaneous marginal zone lymphoma [27]. Overexpression of pAKT was also observed in gastric DLBCL with histological evidence of MALT lymphoma [28]. Somatic mutations have been reported in the PIK3CA gene that encodes the catalytic subunit p110a of PI3Ks in several types of human cancer [29]. However, the mutation of the PIK3CA gene was rarely seen in hematopoietic tumors. As described by Bousquet et al., none of the 80 NHLs, including seven MALT lymphomas possessed somatic mutations of the PIK3CA gene [30]. High level amplification of the 3q26.2-27 region in MALT lymphoma, which harbors the PIK3CA gene, may be partially responsible for its activation. In the present study, PIK3CA expression was evaluated in MALT lymphoma for the first time. The expression of PIK3CA (40.0%) in MALT lymphoma was lower than that of nasopharyngeal cancer (81.8%) and ovarian cancer (about 70%) [12, 31]. We have recently identified the prognostic impact of PIK3CA expression in 40 gastrointestinal MALT lymphomas with a limited follow-up [32]. In the current study, the difference in PIK3CA was significant in a cohort of gastrointestinal lymphomas over a longer period. These observations support the investigation of PIK3CA gene amplification in MALT lymphoma and the involvement of PTEN and pAKT expression in the activation of the PI3K/AKT pathway.
FOXP1 is a member of the FOXP1 subfamily of forkhead transcription factors, which plays diverse roles in cellular proliferation, differentiation, chromatin remodeling, mitotic program, and neoplastic transformation [33]. The translocation t(3;14)(p14.1;q32) that contributes to FOXP1 gene amplification and overexpression has been associated with extranodal diseases including MALT lymphomas of the thyroid, ocular adnexa and skin, but seldom of the gastrointestinal tract [5]. In a Japanese study, t(3;14)/FOXP1-IGH was only detected in one of 59 (1.7%) gastric MALT cases, but additional copies of FOXP1 were detected in ten of 59 (17%) cases [34]. Trisomy of chromosome 3, involved in MALT lymphoma, may contribute to extra copies and FOXP1 protein overexpression [6–8]. In addition, FOXP1 expression was found in 28.6% to 44.2% of MALT lymphomas of various sites [35, 36] consistent to what we observed in our study (46.0% overall). We also observed differences in FOXP1 nuclear staining between gastric and intestinal lymphomas (59.3% vs. 30.4%). The difference was not due to bias from various pathological samples because the categorization of specimens (biopsy or surgery) between gastric and intestinal lymphomas was similar (P = 0.982). This distribution may indicate phenotypic differences in gastric and intestinal lymphoid tissue, which can be divided into acquired and native MALT types. The native type consists of lymphoid tissue present in the gut (e.g., Peyer’s patches), whereas acquired MALT develops in sites of inflammation in response to infection such as H. pylori gastritis [2, 37]. The initial stage of gastric MALT, involving continuous antigen-dependent growth of B lymphocytes, may include more aberrations related to the FOXP1 gene than that of intestinal MALT. This hypothesis may be partially supported by a study in which 22% of gastric MALT lymphomas in comparison with 17% of nongastric MALT lymphomas had t(3;14)/FOXP1-IGH translocation and three copies of FOXP1 [38].
Recent data have showed that FOXP1 protein overexpression was associated with a poorer survival in MALT lymphoma at various sites [36]. In the current study, the prognostic value of the FOXP1 expression was evaluated individually from gastric and intestinal cases because of different clinical behaviors at different anatomic sites. The 5-year survival in patients with high FOXP1 expression was significantly lower in gastric MALT lymphomas, consistent with observations made by Han et al. [35]. An interesting finding was the relationship between the FOXP1 expression and polymorphic histology. The dynamics of phenotypic evolution associated with FOXP1 were also observed by Han et al. and Sagaert et al. which elucidated the role of FOXP1 during the transition of a MALT lymphoma to a more aggressive lymphoma [35, 36]. Therefore, FOXP1 expression may be a prognostic and predictive marker for patient survival and histological transition, respectively.
In the current study, both PIK3CA and FOXP1 expression were associated with patients’ displaying poor survival. Because the expression of PIK3CA and FOXP1 can be assessed by immunohistochemistry, we combined these two markers and found that patients that are positive for both PIK3CA and FOXP1 in gastrointestinal MALT lymphomas had a poorer OS and PFS. To the best of our knowledge, this is the first study to determine the prognostic value of combined PIK3CA and FOXP1 in MALT lymphoma. Additional studies involving a prospective analysis of patients is needed to determine whether this could be used as a prognostic criterion for MALT lymphoma.
In this study, the cutoff to differentiate the monomorphic and polymorphic histologies was consistent with the previous findings in which the monomorphic histology (<5% LC components) represented pure low-grade disease [18]. Although polymorphic histology was identified as a prognostic factor for OS in the present study, a comparison was difficult between various studies of MALT lymphoma and DLBCL due to categorizing by “low-grade MALT” and “high-grade MALT” [17–19]. A recent study using the WHO criteria found a poor 5-year disease-free survival with polymorphic histology, but the cutoff was not clear [36]. To our current knowledge, histological grading of follicular lymphoma, another common indolent lymphoma, has been recommended in the WHO classification. However, no data is readily available to address whether MALT lymphomas with polymorphic histology should be separated and further treated with more intensive treatment. Prospective trials may focus on this group of patients with a new treatment strategy.
Taken together, our results showed that FOXP1 staining is more common in gastric than in intestinal MALT lymphomas and associated with polymorphic histology. A univariate analysis indicated that PIK3CA and/or FOXP1 expression positively correlated with a poorer survival in gastrointestinal MALT lymphomas. However, a multivariate analysis was not conducted due to the relatively small sample size in the present study. Further studies focusing on the cytogenetic and histological features of gastrointestinal MALT lymphomas are needed.
References
The Non-Hodgkin's Lymphoma Classification Project. A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin's lymphoma. Blood. 1997;89(11):3909–18.
Cavalli F, Isaacson PG, Gascoyne RD, Zucca E. MALT lymphomas. Hematology Am Soc Hematol Educ Program 2004;241–258
Raderer M, Streubel B, Woehrer S, Puespoek A, Jaeger U, Formanek M, et al. High relapse rate in patients with MALT lymphoma warrants lifelong follow-up. Clin Cancer Res. 2005;11(9):3349–52.
Starostik P, Patzner J, Greiner A, Schwarz S, Kalla J, Ott G, et al. Gastric marginal zone B-cell lymphomas of MALT type develop along 2 distinct pathogenetic pathways. Blood. 2002;99(1):3–9.
Streubel B, Vinatzer U, Lamprecht A, Raderer M, Chott A. T(3;14)(p14.1;q32) involving IGH and FOXP1 is a novel recurrent chromosomal aberration in MALT lymphoma. Leukemia. 2005;19(4):652–8.
Wotherspoon AC, Finn TM, Isaacson PG. Trisomy 3 in low-grade B-cell lymphomas of mucosa-associated lymphoid tissue. Blood. 1995;85(8):2000–4.
Krugmann J, Tzankov A, Dirnhofer S, Fend F, Wolf D, Siebert R, et al. Complete or partial trisomy 3 in gastro-intestinal MALT lymphomas co-occurs with aberrations at 18q21 and correlates with advanced disease stage: a study on 25 cases. World J Gastroenterol. 2005;11(46):7384–5.
Dierlamm J, Pittaluga S, Wlodarska I, Stul M, Thomas J, Boogaerts M, et al. Marginal zone B-cell lymphomas of different sites share similar cytogenetic and morphologic features. Blood. 1996;87(1):299–307.
Barrans SL, Fenton JA, Banham A, Owen RG, Jack AS. Strong expression of FOXP1 identifies a distinct subset of diffuse large B-cell lymphoma (DLBCL) patients with poor outcome. Blood. 2004;104(9):2933–5.
Banham AH, Connors JM, Brown PJ, Cordell JL, Ott G, Sreenivasan G, et al. Expression of the FOXP1 transcription factor is strongly associated with inferior survival in patients with diffuse large B-cell lymphoma. Clin Cancer Res. 2005;11(3):1065–72.
Akagi I, Miyashita M, Makino H, Nomura T, Hagiwara N, Takahashi K, et al. Overexpression of PIK3CA is associated with lymph node metastasis in esophageal squamous cell carcinoma. Int J Oncol. 2009;34(3):767–75.
Wang Y, Kristensen GB, Helland A, Nesland JM, Borresen-Dale AL, Holm R. Protein expression and prognostic value of genes in the erb-b signaling pathway in advanced ovarian carcinomas. Am J Clin Pathol. 2005;124(3):392–401.
Zelenetz AD, Chen TT, Levy R. Histologic transformation of follicular lymphoma to diffuse lymphoma represents tumor progression by a single malignant B cell. J Exp Med. 1991;173(1):197–207.
Kluin PM, van Krieken JH, Kleiverda K, Kluin-Nelemans HC. Discordant morphologic characteristics of B-cell lymphomas in bone marrow and lymph node biopsies. Am J Clin Pathol. 1990;94(1):59–66.
McCormick C, Philp E, Mansi J, Livni N, McCarthy K. Clonal analysis of three morphologically distinct lymphomas occurring in the same patient. J Clin Pathol. 1994;47(11):1038–42.
Chan JK. The new World Health Organization classification of lymphomas: the past, the present and the future. Hematol Oncol. 2001;19(4):129–50.
Ferreri AJ, Freschi M, Dell'Oro S, Viale E, Villa E, Ponzoni M. Prognostic significance of the histopathologic recognition of low- and high-grade components in stage I-II B-cell gastric lymphomas. Am J Surg Pathol. 2001;25(1):95–102.
de Jong D, Boot H, van Heerde P, Hart GA, Taal BG. Histological grading in gastric lymphoma: pretreatment criteria and clinical relevance. Gastroenterology. 1997;112(5):1466–74.
Hsi ED, Eisbruch A, Greenson JK, Singleton TP, Ross CW, Schnitzer B. Classification of primary gastric lymphomas according to histologic features. Am J Surg Pathol. 1998;22(1):17–27.
Rohatiner A, d'Amore F, Coiffier B, Crowther D, Gospodarowicz M, Isaacson P, et al. Report on a workshop convened to discuss the pathological and staging classifications of gastrointestinal tract lymphoma. Ann Oncol. 1994;5((5):397–400.
Zucca E, Conconi A, Pedrinis E, Cortelazzo S, Motta T, Gospodarowicz MK, et al. Nongastric marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue. Blood. 2003;101(7):2489–95.
Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103(1):275–82.
Hoefnagel JJ, Mulder MM, Dreef E, Jansen PM, Pals ST, Meijer CJ, et al. Expression of B-cell transcription factors in primary cutaneous B-cell lymphoma. Mod Pathol. 2006;19(9):1270–6.
Kang S, Bader AG, Vogt PK. Phosphatidylinositol 3-kinase mutations identified in human cancer are oncogenic. Proc Natl Acad Sci USA. 2005;102(3):802–7.
Baohua Y, Xiaoyan Z, Tiecheng Z, Tao Q, Daren S. Mutations of the PIK3CA gene in diffuse large B cell lymphoma. Diagn Mol Pathol. 2008;17(3):159–65.
Rudelius M, Pittaluga S, Nishizuka S, Pham TH, Fend F, Jaffe ES, et al. Constitutive activation of Akt contributes to the pathogenesis and survival of mantle cell lymphoma. Blood. 2006;108(5):1668–76.
Miletic AV, Anzelon-Mills AN, Mills DM, Omori SA, Pedersen IM, Shin DM, et al. Coordinate suppression of B cell lymphoma by PTEN and SHIP phosphatases. J Exp Med. 2010;207(11):2407–20.
Kuo SH, Yeh PY, Chen LT, Wu MS, Lin CW, Yeh KH, et al. Overexpression of B cell-activating factor of TNF family (BAFF) is associated with Helicobacter pylori-independent growth of gastric diffuse large B-cell lymphoma with histologic evidence of MALT lymphoma. Blood. 2008;112(7):2927–34.
Karakas B, Bachman KE, Park BH. Mutation of the PIK3CA oncogene in human cancers. Br J Cancer. 2006;94(4):455–9.
Bousquet M, Recher C, Queleen C, Demur C, Payrastre B, Brousset P. Assessment of somatic mutations in phosphatidylinositol 3-kinase gene in human lymphoma and acute leukaemia. Br J Haematol. 2005;131(3):411–3.
Woenckhaus J, Steger K, Werner E, Fenic I, Gamerdinger U, Dreyer T, et al. Genomic gain of PIK3CA and increased expression of p110alpha are associated with progression of dysplasia into invasive squamous cell carcinoma. J Pathol. 2002;198(3):335–42.
Zhai LZ, Huang Y, Wang SS, Cao YB, Xiao J, Fu X, et al. PIK3CA, BCL-6, MLL and FOXP1 in the transformation and prognosis of MALT lymphoma [abstract]. J Clin Oncol. 2008;26(May 20 suppl):abstr 8577.
Carlsson P, Mahlapuu M. Forkhead transcription factors: key players in development and metabolism. Dev Biol. 2002;250(1):1–23.
Nakamura S, Ye H, Bacon CM, Goatly A, Liu H, Banham AH, et al. Clinical impact of genetic aberrations in gastric MALT lymphoma: a comprehensive analysis using interphase fluorescence in situ hybridisation. Gut. 2007;56(10):1358–63.
Han SL, Wu XL, Wan L, Zeng QQ, Li JL, Liu Z. FOXP1 expression predicts polymorphic histology and poor prognosis in gastric mucosa-associated lymphoid tissue lymphomas. Dig Surg. 2009;26(2):156–62.
Sagaert X, de Paepe P, Libbrecht L, Vanhentenrijk V, Verhoef G, Thomas J, et al. Forkhead box protein P1 expression in mucosa-associated lymphoid tissue lymphomas predicts poor prognosis and transformation to diffuse large B-cell lymphoma. J Clin Oncol. 2006;24(16):2490–7.
Farinha P, Gascoyne RD. Molecular pathogenesis of mucosa-associated lymphoid tissue lymphoma. J Clin Oncol. 2005;23(26):6370–8.
Goatly A, Bacon CM, Nakamura S, Ye H, Kim I, Brown PJ, et al. FOXP1 abnormalities in lymphoma: translocation breakpoint mapping reveals insights into deregulated transcriptional control. Mod Pathol. 2008;21(7):902–11.
Acknowledgments
We thank all the pathologists and oncologists who contributed.
This study was funded by Guangdong National Science grant 05200178, Guangdong Science and Technology program 2003C30314, and Guangzhou Science grant 2006Z3-E0021.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Linzhu Zhai and Yuanyuan Zhao contributed equally to the manuscript.
Rights and permissions
About this article
Cite this article
Zhai, L., Zhao, Y., Ye, S. et al. Expression of PIK3CA and FOXP1 in gastric and intestinal non-Hodgkin’s lymphoma of mucosa-associated lymphoid tissue type. Tumor Biol. 32, 913–920 (2011). https://doi.org/10.1007/s13277-011-0192-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-011-0192-3