Abstract
The aim of this study was to examine the negative predictive value for a panel of serum markers in women at high risk for developing ovarian cancer. A total of 201 serum samples were collected and analyzed from 102 women at “high risk” for ovarian cancer: 26 with primary ovarian cancer, 31 with recurrent ovarian cancer, 28 with benign gynecologic diseases, and 14 with other cancers. Samples were tested for cancer antigen (CA) 125 II, CA19-9, CA72-4, CA15-3, and macrophage colony-stimulating factor, OVX1, and the marker values were further used as input to be evaluated by a previously trained artificial neural network (ANN). CA125 alone identified 72% of the primary ovarian cancers at a specificity of 95%. If either CA125 or CA72-4 were elevated, sensitivity rose to 80%. Adding macrophage colony-stimulating factor–improved sensitivity to 84% and when CA15-3 was included, a sensitivity of 88% was achieved. Specificity of the four marker panel was, however, reduced to 82.5%. By contrast, at the same sensitivity of 88%, the ANN exhibited a much higher specificity at 92.5% (p = 0.0105). Our data suggest that the combined use of multiple biomarkers improve sensitivity in women at high risk for ovarian cancer. In contrast to the simple “or” combination rule, the ANN was able to achieve a higher sensitivity without significant loss in specificity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumor markers are important in clinical oncology, but their role must be better understood to permit their correct use. Recently, by antibody microarrays, enzyme-linked immunosorbent assay, and other approaches including proteomics, a number of potential markers were identified and used either individually or in combination in an attempt to increase specificity and sensitivity, especially in early stages of the disease.
In the case of ovarian cancer, immunoassay studies indicated that elevated cancer antigen (CA) 125 levels (>35 U/ml) are found in 1.4% of healthy women but in 82% of patients with epithelial ovarian cancer, and yet only 50% of ovarian cancer patients with stage I disease have CA125 levels higher than normal [1–4]. The ability of CA125 levels to distinguish benign from malignant disease is greater for postmenopausal women than for premenopausal (sensitivity 81% vs. 60%, specificity 91% vs. 73%) [5–8].
The prognosis of ovarian cancer remains poor mostly due to late detection: in fact, 70% to 75% of cases are diagnosed with advanced stage disease and have 5-year survival rates between 10% and 30%. In contrast, early-stage disease (stage I/IIa) has a 5-year survival rate of nearly 95% [9]. Attempts have been made to identify the disease at an earlier stage through the use of various serum proteins in an effort to increase survival rates; however, studies show that while known markers can identify disease, specificity and sensitivity are not yet adequate for screening.
Many other serum markers are presently being investigated both for early detection/screening and as a means of distinguishing benign from malignant disease [10] (Table 1). Combination of multiple serum markers using an artificial neural network (ANN) could improve specificity in discriminating malignant from benign pelvic masses [11].
In contrast, first diagnosis of breast cancer is often possible at initial stages through the usual monitoring examinations, which include periodic mammography (MX), ultrasound tomography, CA15-3, and macrophage colony-stimulating factor (M-CSF) serum levels [12]. However, these markers are observed prevalently in advanced disease.
The patients with high genetic risk are the special population that needs to be followed; this group includes women with BRCA1 or BRCA2 germline mutations or who are at high familial risk. This population has an elevated risk of developing breast and/or ovarian cancer. Because of the early onset of the disease, screening of this group of women should start at an earlier age than in the general population. Breast magnetic resonance imaging (BMRI), ultrasonography (US) with MX, and clinical breast examination (CBE) have been suggested for screening [13], but there are fewer reports of serum tests [14].
The aim of this study is to verify whether a panel of serum markers can be used to predict or monitor ovarian cancer in high-risk women and whether their combined use improves sensitivity in detection ovarian cancer without significant loss in specificity.
Materials and methods
Patients and clinical samples
From 1999 through 2005, 201 serum samples were collected and analyzed from subjects in five different categories (Table 2): (1) 26 patients with initial diagnosis of ovarian cancer (6 stage I-II, 6 borderline tumor, 13 with late-stage III-IV, 1 unknown stage); (2) 31 patients with metastatic, relapsed ovarian cancer; (3) 28 patients with benign gynecologic lesions; (4) 14 samples from metastatic breast cancer (6 samples) and other cancers; and (5) 102 healthy women at “high risk” for epithelial ovarian or breast cancer who had BRCA1/BRCA2 mutations (33 samples), or a known mutation in BRCA1/BRCA2 in a first-degree relative (26 samples), or a family history of breast/ovarian cancer (43 samples). The median age of women in this study was 48 years (range, 18-91 years).
Blood was drawn at the Oncology Clinic at Padua Hospital (now the Veneto Oncology Institute). Blood collection in this study was approved by the ethical committee of the Oncology Clinic at Padua Hospital, and all patients gave an informed consent before initiation of the study. Blood was collected from cancer patients prior to surgery or during follow-up. Blood from healthy women with high risk was collected during the clinic visit. We followed previous protocols of specimen collection [11]; in briefly, samples were allowed to coagulate for 1 hour at room temperature and were centrifuged at 4000 rpm for 10 minutes. Serum was then collected and aliquoted. Separated serum specimens were stored at -80°C or below, and then frozen shipped to M. D. Anderson Cancer Center, where they were stored at -80°C until analysis. Samples were thawed only once or twice.
Biomarker tests
We have selected six known biomarkers to analyze 201 serum specimens; these assays are CA125II, CA72-4, CA15-3, CA19-9, OVX1, and M-CSF [1, 15–17]. Radioimmunoassay kits (Fujirebio Diagnostics Inc., Malvern, PA) were used to evaluate levels of CA125II, CA72-4, CA15-3, and CA19-9. OVX1 and M-CSF radioimmunoassays were developed as previously described [16, 17].
Cutoff values for the markers examined in this study were: CA125 <35 U/mL, CA72-4 <3.8 U/mL, CA15-3 <32, M-CSF <3.1 U/mL, OVX1 <12.1 U/mL, and CA19-9 <39 U/mL. The cutoff levels of OVX1 and MCSF were from Woolas et al. [15] and Skates et al. [18]; the cut off levels of CA125 II, CA19-9, CA72-4, and CA15-3 were from the manufacturer.
Artificial neural network analysis and statistical analysis
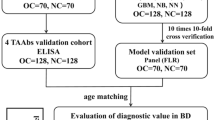
To evaluate the performance of the tumor markers in a multivariate algorithm, four of the tested tumor markers were further used as inputs to be analyzed by a previously reported ANN. The ANN was previously derived using a training set from 100 apparently healthy women, 45 women with benign conditions arising from the ovary, and 55 invasive epithelial ovarian cancer patients (including 27 stage I/II cases). Details of the ANN and its validation on early stage epithelial ovarian cancer have already been published [19]. In the current article, the new data should be considered as an independent validation since none of the current samples were ever involved in the derivation of the ANN. Receiver operating characteristic (ROC) curve analysis was performed using Analyse-It 2.0 (Analyse-it Software, Ltd., Leeds, UK).
Results
Serum biomarker test results in different groups
Two hundred one samples were analyzed for the six markers. Table 3 describes the mean, median, and ranges of individual markers for each of the clinical groups.
Initial diagnosis ovarian cancer
Of the 26 women with first diagnosis of ovarian cancer, 23 samples (88.5%) had elevated levels of at least one of the markers examined. Among these patients, the number of cases (%) with an elevated level of the individual markers, CA125, CA72-4, CA15-3, CA19-9, OVX1, and MCSF were 18 (69.2%), 15 (57.7%), 12 (46.2%), 11 (42.3%), 6 (23.1%), and 14 (53.8%), respectively. When CA125 or CA72-4 is above normal, they identified 21 of 26 cases and improved the sensitivity to 80.8%. By adding M-CSF, 22 of 26 tumors were detected with a sensitivity of 84.6%. Finally, by adding CA15-3, 23 of 26 tumors were identified with a sensitivity of 88.5%.
Metastatic ovarian cancer
Among the 31 women with metastatic, relapsed ovarian cancer, 20 (64.5%) women had levels of CA125 above 35 U/ml, 18 (8.1%) had elevated levels of CA72-4, 16 (51.6%) had raised levels of CA15-3, 12 (38.7%) presented M-CSF above cutoff values, and finally only 2 (6.5%) samples had CA19-9 or OVX1 above normal. Overall, 23 women (74.2%) in this group had at least one marker elevated above its corresponding cutoff value.
Benign pelvic disease
In this group, CA19-9, CA15-3, and M-CSF may be higher than the cutoff values without any pathologic implication. However, CA72-4 results were always negative. Overall, 12 samples contained at least one marker level above normal. Only 1 (3.7%) of the 28 patients with a benign pelvic mass had an elevated CA125-II level (>35 U/ml, but <65 U/ml). Markers CA15-3 and OVX1 were elevated in one sample each (3.7%), while five women (17.9%) had elevated levels of M-CSF. CA19-9 was raised in six samples (21.4%). Only two women (7.1%) in this category presented more than one marker above cutoff values; CA19-9 was elevated in both these. No sample in this group was positive for both CA125 and CA72-4.
High-risk healthy women
Of the 102 healthy women at high risk for ovarian cancer, 6 (5.9%) had elevated CA125 levels (between 36 and 248 U/ml). Three of the six women repeated CA125 tests; for two women, CA125 returned to the normal range, while one remained elevated (<65 U/ml). Nine samples (8.8%) had high levels of CA72-4. Only 1 patient (1%) presented elevated CA15-3, while 5 (4.9%) samples had elevated CA19-9, 11 (10.8%) had raised OVX1, and 5 (4.9%) presented M-CSF above cutoff values. Thirty-two (31.4%) women had at least one elevated marker: 27 (26.5%) had only one marker above cutoff, while 5 (4.9%) had two raised markers. Nineteen of these 37 elevated markers were repeatedly tested after 3 months or 1 year, six (32%) were back to normal range, and the other 13 (68%) remained elevated.
Within the high-risk group, 33 were BRCA+. Among them, 11 (33.3%) had at least one elevated marker including 2 samples (6.0%) who had two elevated markers. These two samples were from two separate women who were sampled repeatedly during follow-up; in one woman, CA19-9 normalized, while OVX-1 remained elevated; and in another woman, CA72-4 temporarily returned to normal levels but rose again, while MCSF levels back to normal. All samples provided during the course of 2 to 6 years, respectively.
ANN analysis results
To assess the performance of the tumor markers in a multivariate algorithm, we applied a previously trained ANN, which combined the results of CA125 II, CA72-4, CA15-3, and M-CSF into a single-value index and compared the ANN index's performance with that of the four individual markers. Figure 1 shows the distributions of the ANN index values among the four clinical groups (initial diagnosis ovarian cancer, metastatic ovarian cancer, benign pelvic disease, and high-risk healthy women). Significant differences were observed between ovarian cancer (initial diagnosis plus metastatic) and noncancer (benign plus high-risk healthy women) and between ovarian cancer and high-risk healthy women alone (p < 0.0001 in both comparisons using Mann-Whitney U test).
Boxplot showing medians, quartiles, and ranges of ANN values of the four groups. Asterisk (*) indicates outliers. Differences in median ANN values were statistically significant between ovarian cancer (initial diagnosis + metastatic) and noncancer (benign + high risk) and between ovarian cancer and high risk alone (p < 0.0001; Mann-Whitney U test)
In receiver operating characteristic (ROC) analysis to separate ovarian cancer (initial diagnosis and metastatic) from noncancer (benign and high-risk healthy women), the area under curve (AUC) by ANN was 0.89 (95% confidence interval [CI], 82%–95%), CA125 II alone was 0.86 (95% CI, 79%–93%), CA72-4 alone was 0.80 (95% CI, 72%–87%), CA15-3 alone was 0.81 (95% CI, 74%–89%), and M-CSF alone was 0.77 (95% CI, 69%–86%). Compared with the ANN, CA125 alone identified 72% of the primary ovarian cancers at a specificity of 95%. If either CA125 or CA72-4 were elevated, sensitivity rose to 80%. Adding M-CSF improved sensitivity to 84%, and when CA15-3 was included, a sensitivity of 88% was achieved. Specificity of the four marker panel was, however, reduced to 82.5%. By contrast, at the same sensitivity of 88%, the ANN exhibited a much higher specificity at 92.5% (p = 0.0105).
The overall improvement of the ANN in AUC over that of CA125 is small and statistically insignificant. However, at relatively high sensitivities (>80%), the improvement in specificities at different sensitivity levels was quite noticeable; for example, at a sensitivity of 82.1%, CA125 had a specificity of 76.2% (95% CI, 67.9%–83.2%), while the ANN had a specificity of 92.6% (95% CI, 85.9%–96.7%). In fact, the difference in partial AUCs corresponding to areas where sensitivity >80% was statistically significant (p = 0.0086; Fig. 2).
ROC curve of ANN analysis (black) and CA125 tests (gray). The overall difference in AUCs between ANN and CA125 were not statistically significant (p = 0.1424). However, the difference in paired comparison of partial AUCs corresponding to areas where sensitivity >80% was statistically significant (two-tailed: p = 0.0086)
Among the 102 sera from women at high risk, elevation of CA125 II was found in 6, CA72-4 in 9, CA15-3 in 1, CA19-9 in 10, OVX1 in 11, and M-CSF in 5. Thirty-two women (31%) had at least one elevated marker level. Among the 28 sera from benign pelvic diseases, elevated CA125 II was found in 1, CA15-3 in 1, CA19-9 in 6, OVX1 in 1, and M-CSF in 5. Twelve samples (43%) contained at least one marker level above normal. The ANN was elevated (at ANN cutoff = 0.0 with corresponding sensitivity at 71.4%) in only 3 (3%) of 102 women at high risk, and 1 (4%) of 28 women with benign pelvic disease.
Patient follow-up
All patients are followed up from 2 to 7 years. Among the high-risk patients, two developed breast cancer in situ (one is BRCA2+, one has family history of breast cancer) and one (BRCA2+) developed in situ serous carcinoma of the fallopian tube. These three patients had no elevated serum markers. They were treated and are still disease-free.
Discussion
The first diagnosis of breast cancer is often possible at initial stages through the usual monitoring examinations, which include periodic MX, ultrasound tomography, CA15-3, and M-CSF serum detection. Routine use of carcinoembryonic antigen for monitoring response of metastatic breast disease to treatment is not recommended. However, in the absence of readily measurable disease, or an elevated CA15-3, a rising carcinoembryonic antigen may be used to suggest treatment failure [20]. In our study of metastatic breast disease, CA15-3 is confirmed to be an important marker, as in the literature.
On the contrary, the prognosis of ovarian cancer remains poor mostly due to late detection; more than 70% of patients are diagnosed with advanced-stage disease with 5-year survival rates between 30% and 40%. Currently, there is no standard or routine screening test for ovarian cancer. Tests that may detect ovarian cancer are being studied: pelvic examination, transvaginal ultrasound, and CA-125 assay. Screening for ovarian cancer is under study, and there are screening clinical trials taking place in many parts of the world [21].
Attempts have therefore been made to identify the disease at an earlier stage through the use of various serum proteins. With respect to markers for early detection of ovarian cancer, CA125, CA72-4, CA15-3, CA19-9, OVX1, and M-CSF have been described [15, 22].
Follow-up of high-risk women usually includes longitudinal marker measurements (either CA125 alone or a panel of markers) and transvaginal ultrasound. At present, a multimodal approach seems to be the best strategy. In fact, current screening guidelines recommend the use of rectovaginal examination, pelvic/transvaginal ultrasound, and CA125 serum levels in women at high risk. In the present study, we used six markers to test 102 high-risk women who had BRCA1/BRCA2 mutations, or a known mutation in BRCA1/BRCA2 in a first-degree relative, or a family history of breast/ovarian cancer.
We evaluated the performance of several tumor markers and used the data to test a previously reported ANN for their potential use in high-risk populations. While serum markers can detect ovarian and breast cancer in women, sensitivity of individual markers is often poor for early-stage diseases. Combining biomarkers in a consensus panel using the “OR” logic relationship could improve sensitivity, yet, as shown in the current data, at the cost of a significantly elevated false-positive values. ANN allows us to combine multiple tumor markers nonlinearly to improve the overall diagnostic accuracy. The ANN tested in the current study was developed previously for detecting early-stage epithelial ovarian cancer from apparent healthy women and was found to perform better than CA125 alone with statistical significance [19]. In the current study, the ovarian cancer cases were mostly late-stage or metastatic disease. However, compared with using the markers in a consensus panel, the ANN was able to achieve the same improvement in sensitivity (equivalently, negative predictive value) without a significant loss in specificity among noncancer high-risk women. Women at high risk for ovarian cancer are more likely to be under active surveillance for early signs of cancer. A noninvasive serum test with a high negative predictive value would be clinically useful for such a purpose. It would be therefore of interest in future studies to validate the ANN's ability to detect early-stage ovarian cancer among high-risk women. Due to the elevated cancer prevalence in such high-risk populations, the use of a multivariate predictive index such as this ANN might be a viable approach before it can be established in more general populations.
References
Bast Jr RC, Klug TL, St John E, Jenison E, Niloff JM, Lazarus H, et al. A radioimmunoassay using a monoclonal antibody to monitor the course of epithelial ovarian cancer. N Engl J Med. 1983;309:883–7.
Zanaboni F, Vergadoro F, Presti M, Gallotti P, Lombardi F, Bolis G. Tumor antigen CA 125 as a marker of ovarian epithelial carcinoma. Gynecol Oncol. 1987;28:61–7.
Zurawski Jr VR, Orjaseter H, Andersen A, Jellum E. Elevated serum CA 125 levels prior to diagnosis of ovarian neoplasia: relevance for early detection of ovarian cancer. Int J Cancer. 1988;42:677–80.
Zurawski Jr VR, Knapp RC, Einhorn N, Kenemans P, Mortel R, Ohmi K, et al. An initial analysis of preoperative serum CA 125 levels in patients with early stage ovarian carcinoma. Gynecol Oncol. 1988;30:7–14.
Malkasian Jr GD, Knapp RC, Lavin PT, Zurawski Jr VR, Podratz KC, Stanhope CR, et al. Preoperative evaluation of serum CA 125 levels in premenopausal and postmenopausal patients with pelvic masses: discrimination of benign from malignant disease. Am J Obstet Gynecol. 1988;159:341–6.
Patsner B, Mann WJ. The value of preoperative serum CA 125 levels in patients with a pelvic mass. Am J Obstet Gynecol. 1988;159:873–6.
Vasilev SA, Schlaerth JB, Campeau J, Morrow CP. Serum CA 125 levels in preoperative evaluation of pelvic masses. Obstet Gynecol. 1988;71:751–6.
Gadducci A, Ferdeghini M, Prontera C, Moretti L, Mariani G, Bianchi R, et al. The concomitant determination of different tumor markers in patients with epithelial ovarian cancer and benign ovarian masses: relevance for differential diagnosis. Gynecol Oncol. 1992;44:147–54.
Cannistra SA. Cancer of the ovary. N Engl J Med. 2004;351:2519–29.
Bast Jr RC, Badgwell D, Lu Z, Marquez R, Rosen D, Liu J, et al. New tumor markers: CA125 and beyond. Int J Gynecol Cancer. 2005;3:274–81.
Zhang Z, Barnhill SD, Zhang H, Xu F, Yu Y, Jacobs I, et al. Combination of multiple serum markers using an artificial neural network to improve specificity in discriminating malignant from benign pelvic masses. Gynecol Oncol. 1999;73:56–61.
Lawicki S, Szmitkowski M, Wojtukiewicz M. The pretreatment plasma level and diagnostic utility of M-CSF in benign breast tumor and breast cancer patients. Clin Chim Acta. 2006;371:112–6.
Trecate G, Vergnaghi D, Manoukian S, Bergonzi S, Scaperrotta G, Marchesini M, et al. MRI in the early detection of breast cancer in women with high genetic risk. Tumori. 2006;92:517–23.
Olivier RI, Lubsen-Brandsma MA, Verhoef S, van Beurden M. CA125 and transvaginal ultrasound monitoring in high-risk women cannot prevent the diagnosis of advanced ovarian cancer. Gynecol Oncol. 2006;100:20–6.
Woolas RP, Xu FJ, Jacobs IJ, Yu YH, Daly L, Berchuck A, et al. Elevation of multiple serum markers in patients with stage I ovarian cancer. J Natl Cancer Inst. 1993;85:1748–51.
Xu FJ, Yu YH, Li BY, Moradi M, Elg S, Lane C, et al. Development of two new monoclonal antibodies reactive to a surface antigen present on human ovarian epithelial cancer cells. Cancer Res. 1991;51:4012–9.
Xu FJ, Ramakrishnan S, Daly L, Soper JT, Berchuck A, Clarke-Pearson D, et al. Increased serum levels of macrophage colony-stimulating factor in ovarian cancer. Am J Obstet Gynecol. 1991;165:1356–62.
Skates SJ, Horick N, Yu Y, Xu FJ, Berchuck A, Havrilesky LJ, et al. Preoperative sensitivity and specificity for early-stage ovarian cancer when combining cancer antigen CA-125II, CA 15-3, CA 72-4, and macrophage colony-stimulating factor using mixtures of multivariate normal distributions. J Clin Oncol. 2004;22:4059–66.
Zhang Z, Yu Y, Xu F, Berchuck A, van Haaften-Day C, Havrilesky LJ, et al. Combining multiple serum tumor markers improves detection of stage I epithelial ovarian cancer. Gynecol Oncol. 2007;107:526–31.
Park BW, Oh JW, Kim JH, Park SH, Kim KS, Kim JH, et al. Preoperative CA 15-3 and CEA serum levels as predictor for breast cancer outcomes. Ann Oncol. 2008;19:675–81.
Joyner AB, Runowicz CD. Ovarian cancer screening and early detection. Womens Health (Lond Engl). 2009;5:693–9. Review.
van Haaften-Day C, Shen Y, Xu F, Yu Y, Berchuck A, Havrilesky LJ, et al. OVX1, macrophage-colony stimulating factor, and CA-125-II as tumor markers for epithelial ovarian carcinoma: a critical appraisal. Cancer. 2001;92:2837–44.
Acknowledgements
Thanks to Fujirebio Diagnostics Inc for providing Radioimmunoassay kits of CA125II, CA72-4, CA15-3, and CA19-9.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Donach, M., Yu, Y., Artioli, G. et al. Combined use of biomarkers for detection of ovarian cancer in high-risk women. Tumor Biol. 31, 209–215 (2010). https://doi.org/10.1007/s13277-010-0032-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-010-0032-x