Abstract
Background
The TFAP2 family of transcription factors, regulating gene expression related to vertebrate evolution, have been studied extensively in human cancer. However, the distinct roles of each TFAP2 in the expression and prognostic significance of lung carcinoma have not been elucidated yet.
Objective
This study is aimed to identify the mRNA expression and prognostic value of TFAP2 family in human lung cancer.
Methods
The transcriptional and survival data of TFAP2s in patients with lung cancer were obtained via ONCOMINE, LinkedOmics, GEPIA, cBioPortal, Kaplan–Meier Plotter and Human Protein Atlas databases.
Results
The results showed that expression levels of TFAP2A and TFAP2C were higher in lung adenocarcinoma and squamous cell carcinoma tissues than in normal lung tissues, whereas no difference was found in the TFAP2B expression level. TFAP2A was related to an unfavorable overall survival in lung cancer and its upregulation was significantly related to the overall survival in patients with smoking, non-chemotherapy and non-radiotherapy.
Conclusion
This study implied that TFAP2A was a reliable prognostic factor, which could be a potential marker for improving survival and prognostic accuracy of lung cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer (LC), as one of the most common cancers, is the leading cause of cancer-related mortality in the world, and approximately 85% of lung cancers are non–small cell lung cancers (NSCLC), which is much more aggressive than other types (Bray et al. 2018; Ettinger et al. 2010; McAleese et al. 2019). In spite of a declining global incidence (Chen et al. 2016), lung cancer remains poor prognosis with its 5-year overall survival rate no higher than 15%. Therefore, to fully evaluate and identify its prognostic factors become crucially important to gain a better understanding of this cancer.
Transcriptional factor plays a critical role in cellular process, biological behaviors and functions, which has an effect on the prognosis of patients. TFAP2 (AP-2), a family of basic helix-span-helix, have been identified to participate in vertebrate evolution (Eckert et al. 2005).The family consists of five paralogs in mammals: TFAP2A to TFAP2E, encoding the proteins AP-2α to AP-2ε, respectively. AP-2α knockout animals damage neural-crest-derived facial structures while AP-2β is essential for kidney development (Eckert et al. 2005). In addition to their effects on development, AP-2 family have also been studied in cancer. Previous studies showed that KRT16 was found to be an oncogene induced by TFAP2A in lung adenocarcinoma (Yuanhua et al. 2019) and TFAP2C plays a role in tumorigenesis and aggressiveness in lung cancer (Kang et al. 2017). Yet, little is known regarding their dysregulated expression level and prognostic values in clinic.
An increasingly large number of bio-information involved in lung cancer has been accessible from the public database so far, including genomics and transcriptomes as well as the corresponding clinical information. Therefore, the present study is conducted to evaluate the prognostic values of AP-2 in patients with lung cancer through bioinformatics methods which may serve as a reference to further confirm their important roles in lung cancer.
Materials and methods
Oncomine database
The gene expression levels of TFAP2 in different types of cancer were evaluated through Oncomine (https://www.oncomine.org/) which is a cancer microarray platform from genome-wide expression (Rhodes et al. 2004, 2007). To compare transcriptional level between clinical neoplastic and normal tissues, the cutoff of p value and fold change were defined as 1E−4 and 2 respectively by using the Student’s t test.
GEPIA analysis
Gene Expression Profiling Interactive Analysis (GEPIA) (https://gepia.cancer-pku.cn), as an online tool for in-depth analysis of gene functions based on the TCGA and the GTEx datasets featuring 198,619 isoforms and 84 cancer subtypes, can perform multiple interactive functions such as differential expression analysis, correlation analysis, patient survival analysis as well as similar gene detection analysis (Tang et al. 2017, 2019). We compared the mRNA level as well as the clinical tumor stage of TFAP2 factors between lung carcinoma tissue and normal tissue.
Kaplan‐Meier plotter
Kaplan–Meier Plotter (www.kmplot.com) could implement survival analysis of different cancer subtypes and is supervised and extended regularly (Nagy et al. 2018). We assessed TFAP2 mRNA for their prognostic power, and the risk ratios with 95% confidence intervals and logarithmic rank p values were calculated. Median expression was used as a cut-off point for dividing patients into high and low expression groups as mentioned previously (Mihaly et al. 2013). The JetSet best probe set of each TFAP2 was selected in order to carry out the overall survival analysis, and the numbers at risk are shown below the main plot.
LinkedOmics portal
The LinkedOmics database (https://www.linkedomics.orglogin.php) can access, analyze and compare cancer multi-omics data within and across all 32 TCGA cancer types (Tomczak et al. 2015). LinkedOmics three analytical modules could be applied to explore attributes that are associated with a query attribute, perform enrichment analysis and compare integrated association results (Vasaikar et al. 2018). The association of TFAP2 mRNA expression with clinical features and overall survival in this study was accessed by the LinkedOmics portal.
c-BioPortal databases
The cBioPortal for Cancer Genomics is a web-based interactive tool for analysis of RNA sequencing expression data of cancer and normal samples from TCGA (Gao et al. 2013). In the present study, c-BioPortal was applied to evaluate lung adenocarcinoma (TCGA, Provisional) dataset including data from 586 samples with clinicopathologic reports for interactive analysis of TFAP2 factors. The targeted genes include mutation information from GISTIC and mRNA expression Z-scores (RNASeq V2 RSEM). TFAP2 genes were accessed by Z-score ± 2.0. Co-expression and network were also performed.
Results
The comparison of TFAP2 expression levels between lung cancer and normal tissue
From the mRNA level, the expression of TFAP2 family (including TFAP2A, B, C) in 18 different types of cancer were compared with adjacent normal tissues as shown in Fig. 1a. An obvious up-regulation of TFAP2A mRNA level in patients with LC was found in eleven datasets while TFAP2C mRNA expression was moderately upregulated in five datasets. Particularly, Bhattacharjee’s dataset demonstrated that TFAP2A in squamous cell lung carcinoma was 98 times higher than the paired normal tissue as shown in Table 1. In other databases, TFAP2A mRNA expressions were 3–15 times more expressed in squamous cell lung carcinoma tissues than in normal lung tissues. In the dataset of Garber, Hou, Su and Selamat, 3 times higher expressions of TFAP2A mRNA were found in lung adenocarcinoma tissues compared with that in normal tissues. Meanwhile, expressions of TFAP2C mRNA were, on average, approximately twice as common in lung adenocarcinoma tissues as in normal lung tissues as shown in three datasets. And Bhattacharjee’s database reported a ten-fold increasing in squamous cell lung carcinoma compared with normal lung tissue.
The comparison of TFAP2 expression levels between lung cancer and normal tissue. a The transcriptonal levels of TFAP2 in different types of cancers (ONCOMINE). b The elevated expressions of TFAP2A and TFAP2C in lung carcinoma compared with that in normal tissue (GEPIA). c Immunohistochemistry staining for TFAP2 in normal and tumor lung tissue from a Human Protein Atlas Portal
Furthermore, we verified the mRNA expressions of TFAP2 between LC and normal lung tissues via GEPIA database. We found that TFAP2A and TFAP2C in LC were both higher than that in normal lung tissues for adenocarcinoma and squamous cell carcinoma, but a larger difference was found in lung squamous cell carcinoma. However, no difference was found in the TFAP2B mRNA expression (Fig. 1b).
Additionally, we identified the expression of TFAP2 at the protein level using Human Protein Atlas database. Immunohistochemistry staining showed a higher expression in cytoplasmic and membranous parts of lung cancer cells for TFAP2A, while no marked difference was found for TFAP2C between lung cancer and normal lung samples. Interestingly, TFAP2B was found to be higher expressed in LC compared with normal lung tissue (Fig. 1c).
Correlation between TFAP2 and clinicopathological features in LC patients
Next, we evaluated the relationship of TFAP2 family with other clinicopathological features. All the TFAP2 family members including TFAP2A (p = 0.451), TFAP2B (p = 0.140) and TFAP2C (p = 0.050) in Fig. 2a were found to be not correlated to the age in lung cancer patients. No significant difference was found between histology and three TFAP2A (p = 0.322) and TFAP2C (p = 0.477) in Fig. 2b, but we found that mucinous subtype of lung carcinoma was more likely to be enriched with higher expression of TFAP2B (p = 0.028). Meanwhile, no significant difference was found between TAFAP2 family members and stage TFAP2A (p = 0.223), TFAP2B (p = 0.479) and TFAP2C (p = 0.197) in Fig. 2c.
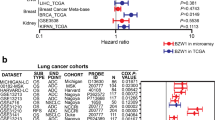
The prognostic significances of TFAP2 in patients with LC
We further evaluated the prognostic significances of TFAP2 in LC patients using Kaplan–Meier Plotter. As illustrated in Fig. 3a, the results showed that only TFAP2A was significantly associated with patient prognosis. In particular, a higher level of TFAP2A mRNA expression predicted a poor overall survival (OS) in lung cancer. However, there were no statistical differences for TFAP2B and TFAP2C in Kaplan–Meier analysis (Fig. 3b, c).
Kaplan–Meier survival curves for overall survival in patients with LC (Kaplan–Meier plotter). a The high expression of TFAP2A correlates with poor prognosis. b, c No prognosis significance was found for the expression of TFAP2B and TFAP2C. The high expression of TFAP2A correlates with poor prognosis in smoking patients (d) compared with that in non-smoking patients (g). The high expression of TFAP2A correlates with poor prognosis in non-chemotherapy patients h compared with that in chemotherapy patients (e). The high expression of TFAP2A correlates with poor prognosis in non-radiotherapy patients i compared with that in radiotherapy patients f
In the subgroup analysis, the upregulated TFAP2A showed significant relation to the overall survival in patients with smoking, non-chemotherapy and non-radiotherapy, whereas no significant survival difference was found in patients with non-smoking, chemotherapy and radiotherapy (Fig. 3d–i).
Sequence alterations and correlations of TFAP2 in lung cancer
To further explore TFAP2 sequence alterations and their correlations, we used the cBioPortal for lung adenocarcinoma (TCGA, Provisional). As shown in Fig. 4a, TFAP2 genes were altered in 20.7% of 517 cases with lung adenocarcinoma and mRNA high expression accounted for 12.96%. Compaerd with 3% mutation rate of TFAP2B, higher rate of sequence alterations was found for the genes, TFAP2A and TFAP2C, with 10% and 12% mutation rate, respectively (Fig. 4b). Genes co-expressed with TFAP2 families were detected in lung adenocarcinoma, and the result showed that TFAP2A was positively correlated with MUC16, KRT16, PCDH7 and RHOV. Besides, TFAP2C was positively correlated with GRHL1, DUSP9, SERTAD4 and NECTIN4 (Fig. 4c).
TFAP2 genes alteration and correlation analysis in lung adenocarcinoma (cBioPortal). a, b The genetic alteration of TFAP2 in lung adenocarcinoma. c MUC16,EPHA7 and GRHL1 are the most correlated genes with TFAP2A, TFAP2B and TFAP2C in mRNA expression level, respectively. d Correlation between TFAP2 transcription factors
We also evaluated the association among TFAP2A, TFAP2B and TFAP2C by Spearman analysis via the GEPIA dataset and found that they were all positively correlated with each other (Fig. 4d). In particular, TFAP2A was moderately correlated with TFAP2C (R = 0.53, p < 0.01) but was low correlated with TFAP2B (R = 0.3, p < 0.01). And TFAP2B was also low correlated with TFAP2C (R = 0.26, p < 0.01).
Network analysis of functions and pathways affected by TFAP2 in patients with LC
To investigate the biological functions and molecular interaction networks of TFAP2 factors and their associated genes, Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) analysis were utilized by DAVID database.
As illustrated in Fig. 5, the results of GO analysis showed that GO:0006915 (apoptotic process), GO:0045944 (positive regulation of transcription from RNA polymerase II promoter), and GO:0000122 (negative regulation of transcription from RNA polymerase II promoter) were markedly regulated by TFAP2 alterations in LC in the aspect of biological process (Fig. 5a). As for the cellular components, GO:0005634 (nucleus), and GO:0005654 (nucleoplasm) were mostly associated with TFAP2 alterations (Figs. 5b). Furthermore, the alterations also prominently regulated molecular functions including GO:0001077 (transcriptional activator activity, RNA polymerase II core promoter proximal region sequence-specific binding) and GO:0042802 (identical protein binding) (Figs. 5c).
Meanwhile, eight most associated pathways in view of TFAP2 alterations were found through KEGG analysis. In particular, two pathways were of significant correlation with TFAP2 alterations including hsa04210: (Apoptosis) and hsa04064: (NF-kappa B signaling pathway). NF-kappa B signaling pathway and apoptosis pathway were shown in Fig. 6.
Discussion
As an important transcriptional factors family, TFAP2 in this study was demonstrated to be a prognostic factor impacting the overall survival for lung cancer patients. We investigated three family members, including TFAP2A, TFAP2B and TFAP2C, and found that they played different roles regarding the biological function and clinical course.
Specifically, TFAP2A is the most frequently studied AP-2 family, which is expressed at the early stage of embryogenesis and is involved in determining the cell fate during neural crest and epidermis formation (Zhang et al. 1996). Reduced, or overexpressed TFAP2A expression has been reported in several cancers including of ovarian, nasopharyngeal, breast, melanoma, glioma, gastric and colon (Anttila et al. 2000; Bar-Eli 1999; Douglas et al. 2004; Heimberger et al. 2005; Schwartz et al. 2007; Shi et al. 2014; Sumigama et al. 2004; Wang et al. 2011), indicating that regulation of TFAP2A gene expression may play a key role in tumorigenesis and development. This study showed that an up-regulation level of TFAP2A in LC compared with normal lung tissue, which is consistent with a previous study in which TFAP2A was illustrated to upregulate the expression of KRT16, an independent prognosis predictor for LC (Yuanhua et al. 2019).
Besides, no significant correlation between TFAP2A expression and the other clinicopathological features, e.g. age, pathological stage and histology type existed in the patients with LC. However, a high TFAP2A expression was markedly related to a poor OS in patients with LC, demonstrating the oncogenic potential of TFAP2A in LC, due to the consideration that it might play a key role in promoting tumorigenesis via epithelial- mesenchymal transition (Yuanhua et al. 2019). We found that TFAP2A was positively correlated with MUC16, KRT16, PCDH7 and RHOV, which are all related to bad survival for cancers.
Of note, the upregulation of TFAP2A was found to be significantly related to the overall survival for the patients with smoking in the subgroup analysis, not for the nonsmokers, indicating that TFAP2A played much more important role for smokers than nonsmokers. Moreover, for patients with chemotherapy or radiotherapy, no survival discriminatory difference was found, but for patients without chemotherapy or radiotherapy, the different expression of TFAP2A showed distinct significant survival, which verified that chemotherapy or radiotherapy could mitigate the effect of TFAP2A in LC.
How the cancer-related gene expressions are impacted by the TFAP2B remains largely under debate. TFAP2B was initially known for its association with the Char syndrome, a human autosomal dominant disorder (Satoda et al. 2000), and later reported to be related to type 2 diabetes mellitus (Comasco et al. 2013; Maeda et al. 2005). TFAP2B was reported previously to be correlated with endometrial cancer, lobular breast cancer, neuroblastoma and thyroid cancer (Cui et al. 2015; Ikram et al. 2016; Raap et al. 2018; Wu and Zhang 2018). Fu et al. found that TFAP2B was upregulated in lung adenocarcinomas and correlated with poor prognosis of the patients (Fu et al. 2014). However, the present study indicated that there was no difference in the expression of TFAP2B between lung cancer and normal tissues, and no significant survival discrimination was found between the patients with high and low expression level. In our view, the reasons for the difference may be due to the sample size, clinical stage and demographic characteristics. Fu et al., studied 147 patients while our prognosis results contain 1145 patients. As the relative much smaller number of patients were found in Fu’s study, we cannot deny that selection bias might have been existed between these two studies. Hence, if we want to gain a better understanding about the potential role of TFAP2B in lung cancer, further studies with much larger sample involved the biological function and the prognostic evaluation were needed.
It has been reported that TFAP2C participated in the regulation of tumorigenesis and was relevant to poor prognosis in some cancers (Ailan et al. 2009; Aqeilan et al. 2004; Woodfield et al. 2010). Previous studies have shown that TFAP2C overexpression led to oncogenic activity and promoted lung tumorigenesis (Kang et al. 2017; Kim et al. 2016). In the present study, a significantly increased expression of TFAP2C was detected in lung cancer compared with normal lung tissue. However, there was no correlation between TFAP2C expression and age, tumor histology types and tumor stage as well as overall survival for patients with LC.
Furthermore, we also evaluated the mutual interaction among the TFAP2 family members and found that they were all positively correlated with each other. TFAP2A was moderately correlated with TFAP2C but was low correlated with TFAP2B (R = 0.3, p < 0.01). And TFAP2B was also low correlated with TFAP2C (R = 0.26, p < 0.01). To investigate the biological functions and molecular interaction networks of TFAP2, we found it was related to the three cellular biological process and function, apoptosis, NF-kappa B signaling pathway and amyotrophic lateral sclerosis, which means TFAP2 could exert an impact for the LC patients via these three pathways.
Several limitations in the present study should be acknowledged. Firstly, the present study was based on in silico predictions, follow-up validation and extension in vivo as well as in vitro experiments are needed to clarify the biological functions of TFAP family in lung cancer. Secondly, the sample selection bias may be existed in the study, as the relatively small sample size may generate insufficient power to detect the majority of associations (Zhao et al. 2018), thus the prediction role of TFAP2 family should be combined with large-scale clinical samples to verify its value for clinical prognosis and treatment.
In all, the expression, mutation, and prognostic values of TFAP2 in LC patients were systematically analyzed in the present study. Our results demonstrated that up-regulated expression of TFAP2A was related to an unfavorable overall survival in lung cancer. Therefore, TFAP2A could be a potential marker for the improvement of survival and prognostic accuracy in patients with lung cancer.
References
Ailan H, Xiangwen X, Daolong R, Lu G, Xiaofeng D, Xi Q, Xingwang H, Rushi L, Jian Z, Shuanglin X (2009) Identification of target genes of transcription factor activator protein 2 gamma in breast cancer cells. BMC Cancer 9:279
Anttila MA, Kellokoski JK, Moisio KI, Mitchell PJ, Saarikoski S, Syrjanen K, Kosma VM (2000) Expression of transcription factor AP-2alpha predicts survival in epithelial ovarian cancer. Br J Cancer 82:1974–1983
Aqeilan RI, Palamarchuk A, Weigel RJ, Herrero JJ, Pekarsky Y, Croce CM (2004) Physical and functional interactions between the Wwox tumor suppressor protein and the AP-2gamma transcription factor. Cancer Res 64:8256–8261
Bar-Eli M (1999) Role of AP-2 in tumor growth and metastasis of human melanoma. Cancer Metastasis Rev 18:377–385
Bhattacharjee A, Richards WG, Staunton J, Li C, Monti S, Vasa P, Ladd C, Beheshti J, Bueno R, Gillette M et al (2001) Classification of human lungcarcinomas by mRNA expression profiling reveals distinct adenocarcinoma subclasses. Proc Natl Acad Sci U S A 98:13790–13795
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66:115–132
Comasco E, Iliadis SI, Larsson A, Olovsson M, Oreland L, Sundstrom-Poromaa I, Skalkidou A (2013) Adipocytokines levels at delivery, functional variation of TFAP2beta, and maternal and neonatal anthropometric parameters. Obesity (Silver Spring) 21:2130–2137
Cui P, Shi K, Cui HX, Hao LY, Su Y, Li PL (2015) Correlation between transcription factor activator protein-2beta (TFAP-2beta) and endometrial carcinoma. Eur J Gynaecol Oncol 36:268–273
Douglas DB, Akiyama Y, Carraway H, Belinsky SA, Esteller M, Gabrielson E, Weitzman S, Williams T, Herman JG, Baylin SB (2004) Hypermethylation of a small CpGuanine-rich region correlates with loss of activator protein-2alpha expression during progression of breast cancer. Cancer Res 64:1611–1620
Eckert D, Buhl S, Weber S, Jager R, Schorle H (2005) The AP-2 family of transcription factors. Genome Biol 6:246
Ettinger DS, Akerley W, Bepler G, Blum MG, Chang A, Cheney RT, Chirieac LR, D'Amico TA, Demmy TL, Ganti AK et al (2010) Non-small cell lung cancer. J Natl Compr Canc Netw 8:740–801
Fu L, Shi K, Wang J, Chen W, Shi D, Tian Y, Guo W, Yu W, Xiao X, Kang T et al (2014) TFAP2B overexpression contributes to tumor growth and a poor prognosis of human lung adenocarcinoma through modulation of ERK and VEGF/PEDF signaling. Mol Cancer 13:89
Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, Sun Y, Jacobsen A, Sinha R, Larsson E et al (2013) Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal 6:pl1
Garber ME, Troyanskaya OG, Schluens K, Petersen S, Thaesler Z, Pacyna-Gengelbach M, van de Rijn M, Rosen GD, Perou CM, Whyte RI et al (2001) Diversity of gene expression in adenocarcinoma of the lung. Proc Natl Acad Sci U S A 98:13784–13789
Heimberger AB, McGary EC, Suki D, Ruiz M, Wang H, Fuller GN, Bar-Eli M (2005) Loss of the AP-2alpha transcription factor is associated with the grade of human gliomas. Clin Cancer Res 11:267–272
Hou J, Aerts J, den Hamer B, van Ijcken W, den Bakker M, Riegman P, van der Leest C, van der Spek P, Foekens JA, Hoogsteden HC et al (2010) Gene expression-based classification of non-small cell lung carcinomas and survival prediction. PLoS One 5:e10312
Ikram F, Ackermann S, Kahlert Y, Volland R, Roels F, Engesser A, Hertwig F, Kocak H, Hero B, Dreidax D et al (2016) Transcription factor activating protein 2 beta (TFAP2B) mediates noradrenergic neuronal differentiation in neuroblastoma. Mol Oncol 10:344–359
Kang J, Kim W, Lee S, Kwon D, Chun J, Son B, Kim E, Lee JM, Youn H, Youn B (2017) TFAP2C promotes lung tumorigenesis and aggressiveness through miR-183- and miR-33a-mediated cell cycle regulation. Oncogene 36:1585–1596
Kim W, Kim E, Lee S, Kim D, Chun J, Park KH, Youn H, Youn B (2016) TFAP2C-mediated upregulation of TGFBR1 promotes lung tumorigenesis and epithelial-mesenchymal transition. Exp Mol Med 48:e273
Landi MT, Dracheva T, Rotunno M, Figueroa JD, Liu H, Dasgupta A, Mann FE, Fukuoka J, Hames M, Bergen AW et al (2008) Geneexpression signature of cigarette smoking and its role in lung adenocarcinoma development and survival. PLoS One 3:e1651
Maeda S, Tsukada S, Kanazawa A, Sekine A, Tsunoda T, Koya D, Maegawa H, Kashiwagi A, Babazono T, Matsuda M et al (2005) Genetic variations in the gene encoding TFAP2B are associated with type 2 diabetes mellitus. J Hum Genet 50:283–292
McAleese J, Taylor A, Walls GM, Hanna GG (2019) Differential relapse patterns for non-small cell lung cancer subtypes adenocarcinoma and squamous cell carcinoma: implications for radiation oncology. Clin Oncol (R Coll Radiol) 31:711–719
Mihaly Z, Kormos M, Lanczky A, Dank M, Budczies J, Szasz MA, Gyorffy B (2013) A meta-analysis of gene expression-based biomarkers predicting outcome after tamoxifen treatment in breast cancer. Breast Cancer Res Treat 140:219–232
Nagy A, Lanczky A, Menyhart O, Gyorffy B (2018) Validation of miRNA prognostic power in hepatocellular carcinoma using expression data of independent datasets. Sci Rep 8:9227
Okayama H, Kohno T, Ishii Y, Shimada Y, Shiraishi K, Iwakawa R, Furuta K, Tsuta K, Shibata T, Yamamoto S et al (2012) Identification ofgenes upregulated in ALK-positive and EGFR/KRAS/ALK-negative lung adenocarcinomas. Cancer Res 72:100–111
Raap M, Gronewold M, Christgen H, Glage S, Bentires-Alj M, Koren S, Derksen PW, Boelens M, Jonkers J, Lehmann U et al (2018) Lobular carcinoma in situ and invasive lobular breast cancer are characterized by enhanced expression of transcription factor AP-2beta. Lab Invest 98:117–129
Rhodes DR, Yu J, Shanker K, Deshpande N, Varambally R, Ghosh D, Barrette T, Pandey A, Chinnaiyan AM (2004) ONCOMINE: a cancer microarray database and integrated data-mining platform. Neoplasia 6:1–6
Rhodes DR, Kalyana-Sundaram S, Mahavisno V, Varambally R, Yu J, Briggs BB, Barrette TR, Anstet MJ, Kincead-Beal C, Kulkarni P et al (2007) Oncomine 3.0: genes, pathways, and networks in a collection of 18,000 cancer gene expression profiles. Neoplasia 9:166–180
Satoda M, Zhao F, Diaz GA, Burn J, Goodship J, Davidson HR, Pierpont ME, Gelb BD (2000) Mutations in TFAP2B cause Char syndrome, a familial form of patent ductus arteriosus. Nat Genet 25:42–46
Schwartz B, Melnikova VO, Tellez C, Mourad-Zeidan A, Blehm K, Zhao YJ, McCarty M, Adam L, Bar-Eli M (2007) Loss of AP-2alpha results in deregulation of E-cadherin and MMP-9 and an increase in tumorigenicity of colon cancer cells in vivo. Oncogene 26:4049–4058
Selamat SA, Chung BS, Girard L, Zhang W, Zhang Y, Campan M, Siegmund KD, Koss MN, Hagen JA, Lam WL et al (2012) Genome-scaleanalysis of DNA methylation in lung adenocarcinoma and integration with mRNA expression. Genome Res 22:1197–1211
Shi D, Xie F, Zhang Y, Tian Y, Chen W, Fu L, Wang J, Guo W, Kang T, Huang W et al (2014) TFAP2A regulates nasopharyngeal carcinoma growth and survival by targeting HIF-1alpha signaling pathway. Cancer Prev Res (Phila) 7:266–277
Stearman RS, Dwyer-Nield L, Zerbe L, Blaine SA, Chan Z, Bunn PA Jr, Johnson GL, Hirsch FR, Merrick DT, Franklin WA et al (2005) Analysisof orthologous gene expression between human pulmonary adenocarcinoma and a carcinogen-induced murine model. Am J Pathol 167:1763–1775
Su LJ, Chang CW, Wu YC, Chen KC, Lin CJ, Liang SC, Lin CH, Whang-Peng J, Hsu SL, Chen CH et al (2007) Selection of DDX5 as a novelinternal control for Q-RT-PCR from microarray data using a block bootstrap re-sampling scheme. BMC Genomics 8:140
Sumigama S, Ito T, Kajiyama H, Shibata K, Tamakoshi K, Kikkawa F, Williams T, Tainsky MA, Nomura S, Mizutani S (2004) Suppression of invasion and peritoneal carcinomatosis of ovarian cancer cells by overexpression of AP-2alpha. Oncogene 23:5496–5504
Tang Z, Li C, Kang B, Gao G, Li C, Zhang Z (2017) GEPIA: a web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res 45:W98–w102
Tang Z, Kang B, Li C, Chen T, Zhang Z (2019) GEPIA2: an enhanced web server for large-scale expression profiling and interactive analysis. Nucleic Acids Res 47:W556–w560
Tomczak K, Czerwinska P, Wiznerowicz M (2015) The Cancer Genome Atlas (TCGA): an immeasurable source of knowledge. Contemp Oncol (Pozn) 19:A68–77
Vasaikar SV, Straub P, Wang J, Zhang B (2018) LinkedOmics: analyzing multi-omics data within and across 32 cancer types. Nucleic Acids Res 46:D956–D963
Wachi S, Yoneda K, Wu R (2005) Interactome-transcriptome analysis reveals the high centrality of genes differentially expressed in lungcancer tissues. Bioinformatics 21:4205–4208
Wang W, Lv L, Pan K, Zhang Y, Zhao JJ, Chen JG, Chen YB, Li YQ, Wang QJ, He J et al (2011) Reduced expression of transcription factor AP-2alpha is associated with gastric adenocarcinoma prognosis. PLoS ONE 6:e24897
Woodfield GW, Chen Y, Bair TB, Domann FE, Weigel RJ (2010) Identification of primary gene targets of TFAP2C in hormone responsive breast carcinoma cells. Genes Chromosomes Cancer 49:948–962
Wu H, Zhang J (2018) Decreased expression of TFAP2B in endometrial cancer predicts poor prognosis: a study based on TCGA data. Gynecol Oncol 149:592–597
Yuanhua L, Pudong Q, Wei Z, Yuan W, Delin L, Yan Z, Geyu L, Bo S (2019) TFAP2A Induced KRT16 as an Oncogene in Lung Adenocarcinoma via EMT. Int J Biol Sci 15:1419–1428
Zhang J, Hagopian-Donaldson S, Serbedzija G, Elsemore J, Plehn-Dujowich D, McMahon AP, Flavell RA, Williams T (1996) Neural tube, skeletal and body wall defects in mice lacking transcription factor AP-2. Nature 381:238–241
Zhao LY, Wang JJ, Zhao YL, Chen XZ, Yang K, Chen XL, Zhang WH, Liu K, Song XH, Zheng JB et al (2018) Superiority of tumor location-modified lauren classification system for gastric cancer: a multi-institutional validation analysis. Ann Surg Oncol 25:3257–3263
Acknowledgements
This study was supported by grants from post-doctor research project, West China Hospital, Sichuan University (Grant no. 18HXBH013). The authors appreciated Pro. Xue Zhao form Sichuan University, for her kind help in grammar revision and suggestion regarding this manuscript. All the listed authors made substantial contributions as follows: study concept and design and obtained funding: Cai-Qi Cheng, Lin-Yong Zhao; draft manuscript: Cai-Qi Cheng, Lin-Yong Zhao; analysis and interpretation of data: Cai-Qi Cheng, Zhisen Ai.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors, Caiqi Cheng, Zhisen Ai and Linyong Zhao declare that they have no conflict of interest.
Ethical approval
The study was approved by the Ethics Committee of West China College of Stomatology, Sichuan University. Informed consent was waived because all data involving the individual participants included in the study were from the public database and their private information was concealed prior to evaluation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheng, C., Ai, Z. & Zhao, L. Comprehensive analysis of the expression and prognosis for TFAP2 in human lung carcinoma. Genes Genom 42, 779–789 (2020). https://doi.org/10.1007/s13258-020-00948-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13258-020-00948-2