Abstract
Intrafraction prostate motion degrades the accuracy of radiation therapy (RT) delivery. Whilst a number of metrics in the literature have been used to quantify intrafraction prostate motion, it has not been established whether these metrics reflect the effect of motion on the RT dose delivered to the patients. In this study, prostate motion during volumetric modulated arc therapy (VMAT) treatment of 18 patients and a total of 294 fractions was quantified through novel metrics as well as those available in the literature. The impact of the motion on VMAT dosimetry was evaluated using these metrics and dose reconstructions based on a previously validated and published method. The dosimetric impact of the motion on planning target volume (PTV) and clinical target volume (CTV) coverage and organs at risk (OARs) was correlated with the motion metrics, using the coefficient of determination (R 2), to evaluate their utility. Action level threshold for the prostate motion metric that best described the dosimetric impact on the PTV D95% was investigated through iterative regression analysis. The average (range) of the mean motion for the patient cohort was 1.5 mm (0.3–9.9 mm). A number of motion metrics were found to be strongly correlated with PTV D95%, the range of R 2 was 0.43–0.81. For all the motion measures, correlations with CTV D99% (range of R 2 was 0.12–0.62), rectum V65% (range of R 2 was 0.33–0.58) and bladder V65% (range of R 2 was 0.51–0.69) were not as strong as for PTV D95%. The mean of the highest 50% of motion metric was one of the best indicator of dosimetric impact on PTV D95%. Action level threshold value for this metric was found to be 3.0 mm. For an individual fraction, when the metric value was greater than 3.0 mm then the PTV D95% was reduced on average by 6.2%. This study demonstrated that several motion metrics are well correlated with the dosimetric impact (PTV D95%) of individual fraction prostate motion on VMAT delivery and could be used for treatment course adaptation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intrafraction motion during prostate radiation therapy could lead to inaccurate dose delivery through geometric miss of the target and excessive irradiation of organs at risk including rectum [1–14]. In context of prostate stereotactic ablative radiation therapy and intra-prostatic nodal boost, the dose delivered in individual fractions becomes critical. However, the effect of the intrafraction motion on the delivered treatment is not well understood, which is vital for assessing the requirements of intrafraction motion management methods. Few studies [4–7] have attempted to correlate the 3D prostate motion with the corresponding dosimetric impact. Li et al. [6] calculated the motion inclusive dose for patients’ treatment courses by convolving static treatment doses with corresponding motion probability functions. They acknowledged that the convolution approaches do not account for dose-per-fraction effects and inter-play effects. Therefore, correlation of individual fraction motions and their dosimetric impact was not investigated. In another study, Langen et al. [4, 5] investigated the dosimetric effect of the motion for each fraction, for helical Tomotherapy, finding no strong relationship between the motion and dosimetric impact on the target. However, the applicability of their result is also limited to helical Tomotherapy systems; whereas other delivery techniques such as intensity modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT) are more widely available and utilised, and may show correlation. Colvill et al. [7] in their study assessed the dosimetric impact of multi-leaf collimator (MLC) tracking and gating as intrafraction motion correction strategies and compared these with no motion correction using 20 fractions from five patients. They showed strong correlation between the motion and its dosimetric impact on the target. The authors acknowledged that their study had selection bias as most of the studied fractions were in the upper range of the motion percentiles. It should be noted that none of the existing studies investigated the use of various motion metrics on the correlation between the motion and their dosimetric impact on target coverage and OARs. This is important because quantification of prostate motion itself is likely to have a major effect on the correlation. In case of IMRT and VMAT the dosimetric effect of the motion has so far not been investigated in a study without any selection bias. In addition, the correlation between the motion and organs at risk (OARs) doses has also not been assessed to date.
The objective of this study was to quantify 3D prostate motion using novel motion metrics along with other metrics available from the literature and to correlate these motion measures with the dosimetric effect of the motion on targets and OARs. The aim was to investigate whether such metrics can be used to indicate action thresholds for prostate motion, i.e., when effects will be significant or not and hence when treatment parameters and decisions may need to take this into account.
Materials and methods
Patient cohort
Prostate intrafraction motion data for 294 fractions from a cohort of 18 patients were retrospectively investigated. Of these, 8 patients had intrafraction motion determined using a novel kV fluoroscopic imaging system, called kilovoltage intrafraction monitoring (KIM) [15]. Another 10 patients were monitored using the Calypso® system [8, 16]. Both of these trials had the necessary ethics, governance, legal, and regulatory processes completed prior to the initiation. Informed consent was obtained from all individual participants included in the study. Patients from these two trials were pooled together to increase the sample size for the analysis and differences between the measured motion from them were not significant (p < 0.05). All the fractions with dose reconstruction available from the trials, at the time of the initiation of this study, were used without any selection (or exclusion) bias. Patient treatments were delivered using VMAT and a standard departmental protocol [17] with all patients simulated with an empty rectum and a comfortably full bladder. The patient cohort comprised of two main treatment fractionation schedules, 13 patients received the conventional fractionation schedule of 80 Gy in 40 fractions and 5 patients received the second fractionation schedule involving radiation therapy boost fractions. A detailed distribution of patient cohort and treatment types and times is presented in Table 1. Patients were aligned daily with imaging before treatment and negligible inter-fraction variations were assumed.
Motion monitoring
KIM real-time target position was used to monitor the intrafraction prostate motion in the KIM trial. The KIM technology uses kV fluoroscopy to monitor, in real-time, the 3D position of three radio-opaque markers implanted into the prostate target [9, 15]. It uses 2D X-ray images to accurately estimate the 3D target position at 5–10 Hz during the treatment delivery [18]. The Calypso® system uses implanted electromagnetic transponder-based markers [19] to report the position at 10 Hz. Each patient had three implanted markers. Both the KIM [9, 15] and Calypso® [19] systems have been reported to have sub-millimetre accuracy. In both trials, the motion of the centroid of the implanted markers, with no corrections, was used as a surrogate for intrafraction prostate motion. The planning target volume (PTV) margins were 5 mm posteriorly and 7 mm elsewhere on the clinical target volume (CTV). In this study PTV was modelled with the same motion as the target to represents a CTV with zero margins and therefore is a representation of the most extreme case.
Measure of prostate motion
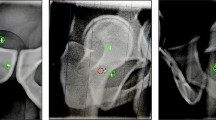
The mean prostate motions across patient fractions were visualised using the probability of 3D displacement (see Fig. 1). This was defined as the percentage of time the 3D displacement was over a certain value, ‘x’, during an individual fraction. It provides a descriptive representation of the motion and has previously been used to present prostate motion [11]. The prostate motion from individual fractions was quantified to a single figure-of-merit through various motion metrics. These metrics comprised of 9 newly defined measures. For each prostate motion trajectory, motion was quantified by the mean of the highest x% (H x% ) of the 3D displacements (motion); x was investigated for 10, 20, 30, 40, 50, 60, 70, 80, 90 and 100%, where H100% represents the mean of all 3D displacements at a fraction while lower percentages represent the more outlying motion. Previously in the literature, Langen et al. [12] have defined and used the fraction of time the prostate displacements are: >3, >5 and > 7 mm; and Li et al. [6] have defined and investigated R95, R90, and R80, which represent that the 3D displacement is less than Rx (magnitude) during x percentage of the monitoring time. Metrics from both these studies were also evaluated here.
Motion inclusive dose reconstruction
Previously, motion inclusive dose reconstruction for the trial data used in this study has been reported [7–9, 16]. Dose delivered in the presence of prostate motion, with and without motion compensation, during each fraction was estimated using a motion-synchronized isocenter shift dose reconstruction method developed and validated by Poulsen et al. [20]. In this study, the estimated dose delivered without any motion compensation after the initial pre-treatment beam-prostate alignment (i.e. first intrafractional shift is always zero) was used to investigate the effect of motion on the dosimetry. It should be noted that the motion inclusive dose reconstruction system assumes that prostate and surrounding OARs move together rigidly and ignores any differential motion between the prostate and OARs.
Analysis
For all patients, intrafraction motion was visualised through the probability of 3D displacements. The dosimetric impact of motion was investigated through correlation between the motion metrics and variations in PTV D95% (minimum dose to 95% of the PTV), CTV D99% (minimum dose to 99% of the CTV), rectum V65% (volume of rectum receiving at least 65% of the prescribed dose) and bladder V65% (volume of bladder receiving at least 65% of the prescribed dose) from the planned values in the presence of motion. The analysis performed in this study is schematically presented in Fig. 2. PTV D95% was evaluated as it is representative of the CTV coverage without margin. Rectum and bladder were investigated as these are OAR for prostate radiation therapy. We specifically investigated V65% as this is a critical dose-volume criteria used to infer plan quality within our local planning protocol [17]. The correlations were evaluated using the Pearson’s correlation coefficient and the coefficient of determination (R 2) was reported. An action level threshold value of motion metric was estimated by segmenting the results (motion metric and measure of the dosimetric effect) into two groups using an iterative linear regression model fitting procedure. The slopes of the two segmented groups were compared and also the differences in the dosimetric effect in these two groups were statistically compared using the F test (ANOVA). The Wilcoxon rank sum test was used to evaluate the differences between variations in PTV D95% and CTV D99%.
Schematic of methods used in this study. Correlation of prostate motion of individual fractions and corresponding dosimetric impact: the dose delivered in the presence of intrafraction motion was estimated using motion inclusive dose reconstruction which utilises the original treatment plan and motion from individual fractions. This estimated dose was compared with the original planned dose and the differences (dosimetric impact metrics) were correlated with motion metrics used to quantify intrafraction motion. Note Fx. stands for fraction
Results
Prostate motion
The prostate motion for the patients is presented, through probability of 3D displacement, in Fig. 1. The quantification of this motion using various metrics was performed and mean values (across all the fractions) and 5th and 95th percentiles values are presented in Fig. 3. In the calculation of the percentage of time that 3D motion is greater than a certain value, only the >3 mm metric had considerable sample size (>30) with non-zero values. The other two metrics >5 and >7 mm with small sample size (<30) were not considered further in this study. There is large variability across fractions in all the motion metrics as seen in Fig. 3. For example, averages (ranges) of some of the metrics are: mean of all motion is 1.5 mm (0.3–9.9 mm); mean of highest 50% of motion is 1.9 mm (0.4–15.4 mm); the percentage of the time motion > 3 mm is 9.4% (0–100%); and R80 is 1.9 mm (0.4–16.0 mm). Moreover, values of the three R80, R90 and R95 metrics are similar and this is also true for means of highest and means of lowest. This might be due to small motion in the majority of fractions analysed in this study as seen in Fig. 1.
Results: Measure of various motion metrics. Comparison of 3D displacement metrics: a mean measures, Hm% represent means of highest m% and 100% represents the mean of all the values; b the percentage of the time motion is greater than a certain value measures, n values gives number of data points in individual categories with non-zero values; c Measures of displacement such that 3D displacement is less than Rx (magnitude) during × percentage time. The marker represents mean value (across all the fractions) and error bar represents 5th and 95th percentile values
Dosimetric impact of the intrafraction motion
Correlation between the dosimetric impact of motion, differences in PTV D95% (CTV + 0 mm margin) and CTV D99%, rectum V65% and bladder V65% from the planned values, and the motion metrics of all the fractions are presented in Table 2. The PTV D95% had substantially stronger correlation with the measured motion metrics than CTV D99%, rectum V65% and bladder V65%, for all the metrics. Mean of highest 50 and 60% of motion had the strongest correlations with the differences in PTV D95% with R 2 value of 0.81. Mean of highest 20 and 30% motion and R90 had highest correlations with CTV D99% with R 2 value of 0.62. The distribution of differences in the target coverage with respect to the mean of highest 50% of motion is presented in Fig. 4. The PTV D95% and CTV D99% had some correlation (R 2 = 0.58) with each other and the differences between these two values were significant (p < 0.05). In the case of OARs, for rectum V65% correlation was highest with the percentage of the time motion >3 mm with R 2 value of 0.58, whilst for bladder V65% correlation was highest with mean of highest 90% of motion and overall means of the motion with R 2 values of 0.69. As noted earlier dose reconstruction system has a limitation in terms of estimation of OAR doses because it assumes the same rigid motion as for the prostate. However, at present the dose reconstruction method is one of few methods that allow for potential estimation of OARs doses.
Action threshold for the intrafraction motion
The motion measure, mean of highest 50% of motion, which had one of the strongest correlations with the differences in PTV D95%, was investigated for action threshold for prostate motion. An iterative linear regression model estimated 3.0 mm (95% confidence interval: 2.7–3.2 mm) as a value of mean of highest 50% as a threshold for PTV D95% in the data-set of this study. For the values smaller than or equal to 3.0 mm, the slope of regression was 1.0%/mm (R 2 value of 0.40) and for the values greater than 3.0 mm, the slope was 2.9%/mm (R 2 value of 0.92). Therefore, the dosimetric impact (per unit increase in motion) and correlation of prostate motion is substantially more when the mean of highest 50% of motion is greater than 3.0 mm. Additionally, 95% confidence intervals for the slopes of the two groups were non-overlapping and this strengthens the use of the threshold value of 3.0 mm. The ANOVA found dosimetric impact to be significantly higher (p < 0.05) when the mean of highest 50% of motion is greater than 3.0 mm in comparison to when the value is less than or equal to 3.0 mm. Summaries of these two groups and results are presented in Table 3.
Discussion
The dosimetric impact of intrafraction 3D prostate motion on the target coverages’ (CTV and PTV) and organs at risk doses (rectum and bladder) of the corresponding fraction during VMAT treatments, has been investigated for the first time. The present study established strong correlation (R 2 > 0.75) between a number of motion metrics (mean of highest 20, 30, 40, 50, 60, 70, 80 and 90% of motion, R90 and R80) and the dosimetric coverage (PTV D95%). These results are particularly useful because clinically an understanding of the dosimetric consequences of the motion is of interest, rather than the motion itself, for evaluating motion management needs. Amongst these metrics, the mean of highest 50% of motion was one of the best indicator of the dosimetric impact of intrafraction prostate motion. Use of this metric for our data shows the action level threshold of 3.0 mm and if the mean of highest 50% was greater than 3.0 mm then the PTV D95% was compromised on an average by 6.2% for the individual fraction. The under-dose will typically be present near the periphery of the PTV. This knowledge, where clinically justified, could be used for treatment in the remaining fractions.
The motion and dose metrics were investigated per fraction and this study did not present the cumulative affect over a number of fractions. Clearly, reducing the number of treatment fractions will increase the impact of individual fractions on the cumulative dose. These metrics will be useful to guide intervention when multiple days are shown to express large motion; towards, for example, reviewing daily CBCT for variable organ at risk volume change to potentially modify patient immobilisation or diet, or modifying (adaptively replanning) the treatment plan to respond to areas of deviated dose delivery from intended.
Only a few studies [4–7] have attempted to correlate motion measures to its dosimetric impact. For helical tomotherapy, Langen et al. [4, 5] investigated the dosimetric effect of the motion on each treatment fraction, using a 4D dose calculation engine, similar to the one used in this study. Their study did not find a strong relationship between motion and its dosimetric impact on the target (R 2 were less than 0.50). A common motion metric, the percentage of the time motion >3 mm could also not be correlated well with the dosimetric impact in this study. The observed motion was similar in both studies with the average (range) percentage of time with >3 mm motion of 9.4% (0–100%) in this study and 13.2% (0–99%) in the study by Langen et al. Similar to Langen et al. [4], this study also found that dose to the CTV, which has added margins, is affected less by motion than the PTV dose, and that variations in the PTV and CTV dose were correlated. One of the purposes of margins to the CTV is to ensure CTV coverage in the presence of intrafraction motion.
Colvill et al. [7] in their study with a selective set of data showed that the mean intrafraction motion and variation in PTV D95% and CTV D99% from the planned values dose reduction are highly correlated (R 2 values were 0.94 and 0.72 respectively). Similarly our study found that for the fractions with large intrafraction motion (H50% > 3.0 mm), the motion and the dosimetric impact PTV D95% was highly correlated (R 2 values was 0.92). In terms of intra-prostatic lesion (IPL) boosted treatments, Pommer et al. [21] found that in the IPL boosted approach, intrafraction motion had a significantly larger (p < 0.001) impact on the dosimetry than for the conventional approach. The majority of the fractions in this study were from standard fractionation and therefore the impact of motion in nodal boost fractions was not investigated.
Previously, studies have investigated various factors that can affect the intrafraction prostate motion. The status of the rectum (such as filling, gas) has been shown to be the most significant predictor for intrafraction prostate motion [2, 13, 14]. Bladder filling has been found to have correlation with a slight posterior drift of the prostate when little or no gas is present [14]. Other studies have found strong correlation between prostate motion and observation time (>5 min) [2, 3, 11, 12]. In standard fractionation, fraction number has been found to have no effect on the intrafraction prostate motion [3, 12, 22]. The primary objective of this study was to investigate various motion measures and their correlation with dosimetric impact of the motion. Therefore the effect of these various factors on the motion was not evaluated in this study.
One of the limitations of this study is that the dose reconstruction performed utilised translational motion only. Also, for all the treatment fractions, patient anatomy has been assumed to be the same as at treatment planning. Rotational as well as deformation components of the motion can substantially affect the dose delivery during the treatments, this also needs to be investigated [23, 24]. Additionally, as noted earlier, another limitation is that the dose reconstruction system assumes that the prostate and surrounding OARs move together rigidly. Moreover, there are factors other than motion magnitude that are likely to have dosimetric impact such as the timing and the direction of the target motion and treatment plan parameters. These require a comprehensive investigation, which is out of the scope of the current study. In addition, the delivery and planning techniques were identical across the patients in this study. Though the patients from the MLC tracking trial had real-time adaptation in their actual treatment delivery but for the purpose of current study that adaptation is not considered for the estimation of the dosimetric deviation in the presence of motion.
Conclusions
This study established that motion metrics can be used as a surrogate to represent the dosimetric impact of prostate motion on target dose. These metrics could be used in studies to report intrafraction prostate motion and thereby indirectly present dosimetric consequences of the reported motion. The mean of highest 50% of motion was the best indicator of the dosimetric impact of intrafraction prostate motion. The results also confirm that the PTV coverage is significantly (p < 0.05) more compromised by the motion than the CTV which has margins to ensure adequate coverage. Finally, it should be noted that the findings from this study are based on a small number of patients (18) and ought to be independently validated in a study involving a larger cohort of patients.
References
Adamson J, Wu Q, Yan D (2011) Dosimetric effect of intrafraction motion and residual setup error for hypofractionated prostate intensity-modulated radiotherapy with online cone beam computed tomography image guidance. Int J Radiat Oncol Biol Phys 80(2):453–461. doi:10.1016/j.ijrobp.2010.02.033
Ghilezan MJ, Jaffray DA, Siewerdsen JH, Van Herk M, Shetty A, Sharpe MB, Zafar Jafri S, Vicini FA, Matter RC, Brabbins DS, Martinez AA (2005) Prostate gland motion assessed with cine-magnetic resonance imaging (cine-MRI). Int J Radiat Oncol Biol Phys 62(2):406–417. doi:10.1016/j.ijrobp.2003.10.017
Kotte ANTJ, Hofman P, Lagendijk JJW, van Vulpen M, van der Heide UA (2007) Intrafraction motion of the prostate during external-beam radiation therapy: analysis of 427 patients with implanted fiducial markers. Int J Radiat Oncol Biol Phys 69(2):419–425. doi:10.1016/j.ijrobp.2007.03.029
Langen KM, Lu W, Ngwa W, Willoughby TR, Chauhan B, Meeks SL, Kupelian PA, Olivera G (2008) Correlation between dosimetric effect and intrafraction motion during prostate treatments delivered with helical tomotherapy. Phys Med Biol 53(24):7073. doi:10.1088/0031-9155/53/24/005
Langen KM, Lu W, Willoughby TR, Chauhan B, Meeks SL, Kupelian PA, Olivera G (2009) Dosimetric effect of prostate motion during helical tomotherapy. Int J Radiat Oncol Biol Phys 74(4):1134–1142. doi:10.1016/j.ijrobp.2008.09.035
Li HS, Chetty IJ, Enke CA, Foster RD, Willoughby TR, Kupellian PA, Solberg TD (2008) Dosimetric consequences of intrafraction prostate motion. Int J Radiat Oncol Biol Phys 71(3):801–812. doi:10.1016/j.ijrobp.2007.10.049
Colvill E, Poulsen PR, Booth J, O’Brien R, Ng J, Keall P (2014) DMLC tracking and gating can improve dose coverage for prostate VMAT. Med Phys 41(9):091705. doi:10.1118/1.4892605
Keall PJ, Colvill E, O’Brien R, Ng JA, Poulsen PR, Eade T, Kneebone A, Booth JT (2014) The first clinical implementation of electromagnetic transponder-guided MLC tracking. Med Phys 41(2):020702. doi:10.1118/1.4862509
Keall PJ, Aun Ng J, O’Brien R, Colvill E, Huang C-Y, Rugaard Poulsen P, Fledelius W, Juneja P, Simpson E, Bell L, Alfieri F, Eade T, Kneebone A, Booth JT (2015) The first clinical treatment with kilovoltage intrafraction monitoring (KIM): a real-time image guidance method. Med Phys 42(1):354–358. doi:10.1118/1.4904023
Nederveen AJ, van der Heide UA, Dehnad H, van Moorselaar RJA, Hofman P, Lagendijk JJ (2002) Measurements and clinical consequences of prostate motion during a radiotherapy fraction. Int J Radiat Oncol Biol Phys 53(1):206–214. doi:10.1016/S0360-3016(01)02823-1
Adamson J, Wu Q (2010) Prostate intrafraction motion assessed by simultaneous kilovoltage fluoroscopy at megavoltage delivery I: clinical observations and pattern analysis. Int J Radiat Oncol Biol Phys 78(5):1563–1570. doi:10.1016/j.ijrobp.2009.09.027
Langen KM, Willoughby TR, Meeks SL, Santhanam A, Cunningham A, Levine L, Kupelian PA (2008) Observations on real-time prostate gland motion using electromagnetic tracking. Int J Radiat Oncol Biol Phys 71(4):1084–1090. doi:10.1016/j.ijrobp.2007.11.054
Padhani AR, Khoo VS, Suckling J, Husband JE, Leach MO, Dearnaley DP (1999) Evaluating the effect of rectal distension and rectal movement on prostate gland position using cine MRI. Int J Radiat Oncol Biol Phys 44(3):525–533. doi:10.1016/S0360-3016(99)00040-1
Adamson J, Wu Q (2009) Inferences about prostate intrafraction motion from pre-and posttreatment volumetric imaging. Int J Radiat Oncol Biol Phys 75(1):260–267. doi:10.1016/j.ijrobp.2009.03.007
Ng JA, Booth JT, Poulsen PR, Fledelius W, Worm ES, Eade T, Hegi F, Kneebone A, Kuncic Z, Keall PJ (2012) Kilovoltage intrafraction monitoring for prostate intensity modulated arc therapy: first clinical results. Int J Radiat Oncol Biol Phys 84(5):e655–e661. doi:10.1016/j.ijrobp.2012.07.2367
Colvill E, Booth JT, O’Brien R, Eade TN, Kneebone AB, Poulsen PR, Keall PJ (2015) MLC tracking improves dose delivery for prostate cancer radiotherapy: results of the first clinical trial. Int J Radiat Oncol Biol Phys. doi:10.1016/j.ijrobp.2015.04.024
Eade TN, Guo L, Forde E, Vaux K, Vass J, Hunt P, Kneebone A (2012) Image-guided dose-escalated intensity-modulated radiation therapy for prostate cancer: treating to doses beyond 78 Gy. BJU Int 109(11):1655–1660. doi:10.1111/j.1464-410X.2011.10668.x
Poulsen PR, Cho B, Langen K, Kupelian P, Keall PJ (2008) Three-dimensional prostate position estimation with a single X-ray imager utilizing the spatial probability density. Phys Med Biol 53(16):4331. doi:10.1088/0031-9155/53/16/008
Santanam L, Malinowski K, Hubenshmidt J, Dimmer S, Mayse ML, Bradley J, Chaudhari A, Lechleiter K, Goddu SKM, Esthappan J (2008) Fiducial-based translational localization accuracy of electromagnetic tracking system and on-board kilovoltage imaging system. Int J Radiat Oncol Biol Phys 70(3):892–899. doi:10.1016/j.ijrobp.2007.10.005
Poulsen PR, Schmidt ML, Keall P, Worm ES, Fledelius W, Hoffmann L (2012) A method of dose reconstruction for moving targets compatible with dynamic treatments. Med Phys 39(10):6237–6246. doi:10.1118/1.4754297
Pommer T, Falk M, Poulsen PR, Keall PJ, T O’Brien R, Petersen PM, af Rosenschöld PM (2013) Dosimetric benefit of DMLC tracking for conventional and sub-volume boosted prostate intensity-modulated arc radiotherapy. Phys Med Biol 58(7):2349. doi:10.1088/0031-9155/58/7/2349
Juneja P, Kneebone A, Booth JT, Thwaites DI, Kaur R, Colvill E, Ng JA, Keall PJ, Eade T (2015) Prostate motion during radiotherapy of prostate cancer patients with and without application of a hydrogel spacer: a comparative study. Radiat Oncol 10(1):1–6. doi:10.11862/s13014-015-0526-1
Huang C-Y, Tehrani JN, Ng JA, Booth J, Keall P (2015) Six degrees-of-freedom prostate and lung tumor motion measurements using kilovoltage intrafraction monitoring. Int J Radiat Oncol Biol Phys 91(2):368–375. doi:10.1016/j.ijrobp.2014.09.040
Nichol AM, Brock KK, Lockwood GA, Moseley DJ, Rosewall T, Warde PR, Catton CN, Jaffray DA (2007) A magnetic resonance imaging study of prostate deformation relative to implanted gold fiducial markers. Int J Radiat Oncol Biol Phys 67(1):48–56. doi:10.1016/j.ijrobp.2006.08.021
Acknowledgements
The authors thank the many contributing staff from the Northern Sydney Cancer Centre, the patients enrolled in the studies, and biostatistician Dr. Rachel O’Connell from the NHMRC Clinical Trials Centre. PJ acknowledges funding from the BARO (Better Access to Radiation Oncology) initiative of the Australian Department of Health, DIT from the NSW Ministry of Health. PJ in addition was supported by Northern Sydney Cancer Centre and the University of Sydney, School of Physics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Royal North Shore Hospital has a collaborative research agreement with Varian Medical Systems to support Calypso® and Kilovoltage intrafraction monitoring (KIM) clinical trials. PK holds part ownership of the patent, between Stanford University and Varian Medical Systems, on KIM technology.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Juneja, P., Colvill, E., Kneebone, A. et al. Quantification of intrafraction prostate motion and its dosimetric effect on VMAT. Australas Phys Eng Sci Med 40, 317–324 (2017). https://doi.org/10.1007/s13246-017-0536-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-017-0536-4