Abstract
Mucus forms a protective layer across a variety of epithelial surfaces. In the gastrointestinal (GI) tract, the barrier has to permit the uptake of nutrients, while excluding potential hazards, such as pathogenic bacteria. In this short review article, we look at recent literature on the structure, location, and properties of the mammalian intestinal secreted mucins and the mucus layer they form over a wide range of length scales. In particular, we look at the structure of the gel-forming glycoprotein MUC2, the primary intestinal secreted mucin, and the influence this has on the properties of the mucus layer. We show that, even at the level of the protein backbone, MUC2 is highly heterogeneous and that this is reflected in the networks it forms. It is evident that a combination of charge and pore size determines what can diffuse through the layer to the underlying gut epithelium. This information is important for the targeted delivery of bioactive molecules, including nutrients and pharmaceuticals, and for understanding how GI health is maintained.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mucus is a highly complex viscous system of glycoproteins that provide a defensive barrier across many epithelial surfaces including the respiratory, reproductive, and gastrointestinal (GI) tracts. It serves many functions in those locations, among which are lubrication of the passage of objects; maintenance of a hydrated layer over the epithelium; a barrier to pathogens, destructive enzymes, and toxic substances; and as a permeable gel layer for the exchange of gases and nutrients with the underlying epithelium [7]. The GI tract mucus is made up of two very different groups of mucins, secreted and membrane-bound [9]. Membrane-bound mucins such as MUC1 are transmembrane glycoproteins expressed at the apical surface of enterocytes, forming what is known as the glycocalyx [29]. The extracellular domain of these mucins forms an extremely large thread-like structure covered by a dense array of complex O-linked oligosaccharides and can be shed from the cell surface. The cytoplasmic domains of cell surface mucins are highly conserved across species and undergo both serine and tyrosine phosphorylation, consistent with a role in signal transduction. However, the primary function of these mucins is not well understood [29]. Secreted mucins, such as MUC2, are continuously produced by goblet cells and are highly specialized glycoproteins characterized by their very high molecular weight (5–40 MDa) and size (600–900 nm) [40] and high proportion of O-linked carbohydrate (usually 50–80 %) [34] and their ability to form viscoelastic gels [6, 39]. These gels are thought to be formed through disulfide links rather than entanglement [35]. The gel strength is determined by the strength of interaction, the level of entanglement, and the size of the holes or “cages” in the network and, hence, by the mucin concentration. It has been shown that the small intestinal mucus layer is highly heterogeneous in density and structure [15], with microviscosities varying by more than four orders of magnitude [24]. Despite this heterogeneity, mucus covers virtually the whole mucosal surface and provides a barrier to invading pathogenic bacteria and certain other particulates while remaining permeable to nutrients. The barrier relies on a combination of porosity and charge. Large particles or those with insufficient charge are unable to diffuse into the mucus.
Digestion is a complex process, and despite significant research in this area, the way to provide optimum delivery of nutrients and GI-protective compounds in realistic meal scenarios is still unclear. As part of the digestion process, a range of physiological surfactants are secreted into the gut lumen. These include phospholipids such as phosphatidylcholine (PC), which is a significant component of the bile secreted into the proximal small intestine [4]. In addition to PC, bile also contains a range of charged bile salts (BS) [32]. BS are surface active and have the ability to solubilize lipids during intestinal digestion, an essential prerequisite for the effective absorption of dietary lipids by the intestinal epithelium. Particles in the GI tract lumen, including emulsified fat, cellular material, and bacteria, are exposed to this range of physiological surfactants that can adsorb to the particle surface and change the surface properties and thus mucus interactions. This is one reason why the selective nature of the GI tract mucus barrier in not well understood.
In an attempt to improve our understanding of the interactions between food structures and GI mucus, we will describe what mucins are present in the different regions of the GI tract. We will then go on to show the structure of the primary secreted intestinal mucin MUC2 and then describe its properties in more detail with a view to elucidating its barrier function.
Gastrointestinal Mucin Geography
A wide range of mucins are found in the GI tract and these can be divided into two groups, secreted and membrane-bound. In this article, we will limit the discussion to secreted mucins, although it is acknowledged that membrane-bound mucins play an important role in the mucosal barrier [29]. There are a number of citations in the literature describing where in the GI tract the various mucins are expressed [8, 30, 41] and these are summarized in Table 1. In the gel-forming mucins, MUC2, MUC5AC, MUC5b, and MUC6, amino acid sequences of the regions upstream and downstream of the central domain (see below) are highly conserved across the four genes. The central domains of MUC5B and MUC5AC show little length variation in contrast to the second repetitive domain of MUC2, which is highly variable in length [45]. In all the mucins, the central domains are heavily glycated and the terminal sialic acid or sulfates provide a high density of negative charge [22]. In the oral cavity and the esophagus, the primary secreted mucin is MUC5B and, to a lesser extent, MUC7. In the gastric compartment, the primary secreted mucin is MUC5AC, with smaller amounts of MUC6 also present. A good example of mucin from this source is the porcine gastric mucin supplied by Sigma-Aldrich, which is widely used in research. This source is rather degraded in terms of molecular weight but is readily soluble in water/buffer and contains approximately 1 % bound sialic acid. The mucus is primarily composed of MUC5AC, with much lower amounts of other mucins and approximately 3–4 % DNA. The thickness of the mucus layer in the gastric compartment is thought to be about 200–300 μm and consists of an inner tightly adherent layer and an outer loosely adherent layer [47]. A more detailed description of the layer structure is given below where the validity of specifying a layer thickness is questioned.
A comparatively impermeable gel layer can be maintained in the gastric compartment because of the limited amount of adsorption that takes place there [20]. However, this is not true of the small intestine, which is the main site of absorption. By far, the most abundant secreted mucin in the intestine of all mammals is MUC2, although MUC6 and MUC11 are also reported as minor components [30]. In this, the main part of the GI tract, the mucus layer is at its thinnest and most heterogeneous [3, 15]. It is the mucus layer in this region that will be the subject of the discussion below. The final region of the GI tract is the colon, where the environment and the architecture are rather different from that in the small intestine, although the primary secreted mucin is still MUC2 and additional minor mucins are MUC5B and MUC11 [15]. The thickness of the mucus layer in the colon is much greater than in the small intestine, being many hundreds of microns and, as in the gastric compartment, comprising tightly and loosely adherent layers [3, 13].
Gastrointestinal Mucus Layer Structure
In the previous section, the mucin expression geography was described and some mention was made of the thickness of the mucus layer. While the general structure of the mucus layer can be defined in the various parts of the GI tract, determining the layer thickness is more equivocal. For example, in the gastric compartment, distension and contraction are part of the normal meal consumption and digestion cycle. This in turn has an effect on the surface area of the stomach and, consequently, on the thickness of the mucus layer on that surface. Figure 1 shows two MRI images of the human stomach (outlined in yellow) immediately before (left) and after (right) consuming a milk-type drink. The fasted (empty) image shows the thick layer of secretion that has built up on the walls of the stomach and shows up as the gray “figure of eight” region, whereas in the fed (full) image, the layer is hardly visible at all. The problem is underlined in the schematic in Fig. 1 where the green region has the same area in both the collapsed and distended shapes. These images highlight the problem of trying to assign thicknesses to the mucus layer in the stomach, but similar problems arise in the small intestine.
Mucin Synthesis
The issues of thickness of the mucus layer are especially important in the small intestine where the layer is at its thinnest and absorption is greatest. Because the layer in the small intestine is highly heterogeneous, it makes sense to look at mucin structure at a range of length scales. With this in mind, this section will look in detail at how MUC2 is formed and secreted and what implications this has for the formation and turnover of the mucus layer and its barrier properties. MUC2 is initially formed in the endoplasmic reticulum of goblet cells lining the crypts and villi of the intestine. The protein backbone comprises a number of different regions as outlined in Fig. 2 and detailed in a number of reviews [12, 15, 35]. The largest and most ill-defined part of the molecule is the variable number tandem repeat region, which is also known as the proline, threonine, and serine (PTS) region. Both the C-terminal and N-terminal ends are very similar to those in von Willebrand factor (vWF) and both terminal ends of the molecule contain a number of disulfide-rich D domains. Indeed, it has been suggested that vWF evolved from mucins [21]. Once assembled, the monomers form disulfide-linked dimers through their C-terminal CK domains [2, 23]. These dimers are then transported to the Golgi complex where the PTS regions are O-glycosylated. Once the glycosylated dimers reach the trans-Golgi compartments, they are assembled into disulfide-linked multimers through their N-terminal D domains. It is important to note that the initial oligomerization is the formation of dimers through the one to one interactions between C termini and that the second step is the formation of higher oligomeric forms through the dimeric or more commonly trimeric interactions between N termini [1, 10]. The final stage in the cell is the packing of the multimeric forms into granules. The packing appears to be dependent on local pH and calcium concentrations. At reduced pH (6.2) and in the presence of elevated levels of Ca2+, mucin aggregates and can be packed into the granule, but upon secretion, the higher extracellular pH and lower calcium concentrations allow the mucin to unpack [1, 11].
The cellular assembly of mucin MUC2, showing the main domains in the primary sequence. The monomer shows the highly variable main tandem repeat region also known as the proline, threonine, and serine (PTS)-rich region in yellow. Also shown in various colors are the terminal domains that are so similar to vWF, all of which are disulfide-rich. In the Golgi and granule, the heavy glycation of the PTS regions are shown in green. This also highlights the formation of dimers, trimers, and higher oligomers
We have recently shown in porcine mucin that the behavior of the multimeric forms as they are packed into the granule is key to their subsequent behavior [37]. In particular, the trimeric links lead to a strictly two-dimensional network that can be packed into the granule and will then unpack once the granule has been secreted. Examples of the trimeric form of the partially degraded network from porcine jejunum mucin can be seen in Fig. 3. This two-dimensional network formation is also thought to be the reason that a stratified tightly adherent layer can be formed while allowing it to break down to a more loosely adherent form [14]. In such a network, the coherence of the network layers defines the difference between the tightly and loosely adherent regions. In addition, lubrication through the formation of a slip plane is favored by slippage between the layers in much the same way as in graphite. This is a key feature of the mucus structure that prevents buildup of a very thick layer.
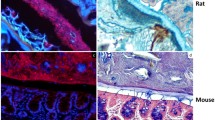
The high degree of heterogeneity of the small intestinal mucus layer has already been shown [3, 15, 24]. While the reason that MUC2 is able to form a homogenous adherent layer in the colon but not in the small intestine is not understood, the differences in architecture and water flux may play a significant role, as highlighted in Fig. 4. In particular, the villi in the small intestine represent a significant barrier to the formation of extended laminar structures. Conversely, in the gastric compartment and the colon, the surface architecture is largely flat and permeated only by the gastric pits or colonic crypts, respectively. In addition, there can be a high water flux through the mucosa of the small intestine, depending upon the meal type [28]. This is in contrast to the water flux in the colon which always acts to remove water so that the luminal contents of the rectum under normal healthy conditions is relatively dry [31].
Properties of the Mucus Layer
In the sections above, the structure and thickness of the GI mucus layer have been discussed. However, the essential thing from the perspective of understanding digestion and transport is how the barrier properties of the mucus are affected by the structure. Thus, it is important to determine the microrheological properties and understand the influence of endogenous components on the transport of nutrients to the intestinal brush border.
There is a body of published work looking at the microrheological properties of a range of different types of mucus using multiple particle tracking [5, 17–19]. Such experiments use fluorescence microscopy to track the motion of fluorescent particles with a well-defined size. From the tracks of the particles, the two-dimensional projection of the volume swept out by the particles as a function of time can be calculated. This value is known as the mean square displacement (MSD) and is defined as \( < \Delta {r^2}\left( {\Delta {t^2}} \right) > = < \Delta {x^2} + \Delta {y^2} > \), where ∆x and ∆y are the particle displacements in x and y, respectively, in time ∆t. The particle diffusion coefficient D can then be calculated from the MSD as D = MSD/4∆t. By taking ensemble values for many hundreds of particles, the local viscosity η can be calculated from the Stokes–Einstein equation (η = kT/6πrD), where k is Boltzmann’s constant, T is the temperature, and r is the particle radius. We have previously used multiple particle tracking of 500 nm carboxylated polystyrene latex to determine the microviscosity of porcine intestinal mucin [24]. In that paper, we provided the first data showing that BS present in the small intestine and an important factor in lipid digestion also play an important role in transport. We showed for the first time that colloidal structures formed during digestion are only able to penetrate the mucus barrier in the small intestine as a result of the adsorption of BS. In the absence of BS adsorption, partially digested lipid droplets formed an adherent layer on the surface of the mucus. When the negatively charged BS adsorb to the surface of oil droplets, they impart significant negative charge to the droplets and this allows them to diffuse through the mucus. This highlights the importance of luminal compounds in determining mucus interactions that allow particulate components of digesta (chyme) to penetrate or adhere to the GI tract mucus. Thus, although it may be possible to modulate the gastric phase behavior of an emulsion by structuring of the interfacial layer, it is not likely to affect the transport of fat droplets through duodenal mucus towards the epithelium where detection of the nutrients can trigger secretion of appetite-suppressing hormones [25].
While mucus needs to allow the passage of nutrients including those in a particulate form such as mixed micelles, it also acts as a barrier to bacteria. A number of recent studies have shown that, in the colon, the mucin layer is able to maintain an adherent region that is free of bacteria. However, it is unclear whether this is simply a function of the mucin structure [13, 15] or of other components such as the antibacterial lectin RegIIIγ [46]. Thus, with this in mind, we have looked at the interactions between motile and nonmotile bacteria and MUC2 mucin as a function of the mucin concentration. Escherichia coli are the most prevalent gram-negative bacteria in the intestine and have dimensions that are very similar to emulsion droplets (i.e., 1–2 μm). Initial experiments showed that, regardless of the presence of BS, nonflagellated E. coli JH3513 that was fluorescently tagged by introduction of a constitutively expressed green fluorescent protein was unable to penetrate into the small intestine mucus, as shown in Fig. 5. Measurements of the surface charge on the bacteria showed values around −18 mV in the presence or absence of BS [24].
Interaction of nonflagellated E. coli (the nonflagellated E. coli JH3513 strain was fluorescently tagged by introduction of a constitutively expressed multicopy plasmid-borne fusion rpsM′-gfp+ into DH5α, a known nonmotile strain) with ex vivo porcine intestinal mucus. All images are 184 μm2 with the mucus labeled with a red fluorescent lectin
This lack of diffusion into the mucus led us to investigate the ability of flagellated bacteria to swim through partially purified mucus of different concentrations using approaches developed at the University of Edinburgh [38, 48]. In short, high-speed video from low-resolution microscopy was analyzed to yield accurate values for velocity, tumbling frequency, and diffusivity of E. coli. A typical example of swimming velocity as a function of mucin concentration is shown in Fig. 6. In dilute solutions, the swimming velocity was the same as in water, but as the concentration increased, so did the velocity. This continued up to a certain value when the local viscosity became too great and the velocity started to decrease. In reality, it is difficult to compare the swimming velocities in these well-controlled experiments, with those that might occur in the heterogeneous mucus of the small intestine, where the local viscosity can vary significantly and is on average much higher than the values because of variations in concentration. The reason for the initial increase is due to the ability of the bacteria to metabolize the mucin and utilize it as an energy source. Where other carbon sources are not readily available, this is likely to have an impact on the local concentrations of bacteria in the mucus layer.
The mucus layer has been shown to provide protection not just against bacterial invasion but also against potentially toxic food compounds [3, 15, 24]. In addition, the osmotic pressure induced by nonabsorbable species can cause a high water flux through the mucosa of the small intestine, depending upon the meal type [28]. This is in contrast to the water flux in the colon which always acts to remove water from the luminal contents. Thus, there tends to be a gradient of water content from the ascending colon to the rectum, which under normal healthy conditions is relatively dry [31].
Given that the mucus layer in the small intestine is highly heterogeneous and that particulates including bacteria may be able to penetrate it, there is a need to ensure that the correct barrier properties are maintained. Thus, the question arises as to whether there are food components that could fulfill this role. The environment of the upper GI tract is generally very effective at digesting protein and lipid, although with the exception of starch, polysaccharide polymers are not significantly digested in this region of the gut. As a result, polymers can persist and change the viscosity of the GI luminal contents, affecting GI behavior [27], and interact with the surrounding mucus layer even further down the GI tract in the colon, as is the case for dextran sodium sulphate when used to induce colitis in mice [36]. Biopolymers can also interact with the degraded mucin that is released into the GI lumen as a result of the constant turnover of mucins from the gastric mucosa. It has been known for some time that mixtures of mucin and biopolymers such as alginate have an increased viscosity. Indeed, as far back as 2005, Taylor et al. showed that mixtures of mucin and alginate formed weak viscoelastic gels [44]. More recently, Nordgard and Draget [33] have shown data confirming the theory that guluronic acid oligomers extracted from alginate are able to disrupt interactions in complex mucus systems through electrostatic competitive inhibition, leading to a reduction in network cross-links and a resultant weakening of the gel matrix. As a result of this work, patents are in place for the use of G-block alginates to reduce the viscosity of mucin in cystic fibrosis sufferers. Thus, it has been shown that, depending on the conditions, biopolymers, especially alginates, can be used to modulate mucus properties, making it either more or less viscous. Even cheese whey proteins have been shown to play a role in protecting the mucus layer from degradation [43]. Indeed, the presence of dietary fiber has been shown to be important in reducing bacterial translocation [42] and has also been implicated in the amelioration of intestinal disorders such as inflammatory bowel disease and colitis, in which the mucus layer becomes degraded [16, 26]. However, it has yet to be shown that these types of interactions and food components can be used to improve the GI mucus barrier directly.
Conclusions and Future Perspectives
In this article, we have looked at the structure of the mucus layer and, in particular, the main intestinal secreted mucin, MUC2. We have shown that the primary structure of MUC2 comprises a variable length highly glycosylated central region. This is secreted to form a series of layers of an essentially two-dimensional network. The coherence of this network depends on the local environment, and in the small intestine, the mucus layer is highly heterogeneous in terms of density and porosity. We have also looked at the properties of the mucus layer and shown that a high negative charge allows the mucus layer to be penetrated by polymers and micron-scale particulates. Conversely, a lack of negative charge leads to an inability to penetrate the mucus layer as diffusion through the mucus layer is controlled by a combination of size and charge. We have also looked at other factors that affect the properties of the layer such as its thickness. The adsorption of BS to particulates was shown to increase the negative charge they carried and facilitated their diffusion through the mucus. This was not the case for nonflagellated E. coli, which could not penetrate to any significant extent. Finally, we have shown a limited number of studies assessing whether food ingredients and/or structures can be used to modulate barrier function for improved health. We believe this is likely to be the case, but the lack of data means more work is needed in order to demonstrate an effect in the complex environment of the GI tract in vivo.
References
Ambort D, Johansson MEV, Gustafsson JK, Nilsson HE, Ermund A, Johansson BR, Koeck PJB, Hebert H, Hansson GC (2012) Calcium and pH-dependent packing and release of the gel-forming MUC2 mucin. Proc Natl Acad Sci U S A 109(15):5645–5650. doi:10.1073/pnas.1120269109
Asker N, Axelsson MAB, Olofsson SO, Hansson GC (1998) Dimerization of the human MUC2 mucin in the endoplasmic reticulum is followed by a N-glycosylation-dependent transfer of the mono- and dimers to the Golgi apparatus. J Biol Chem 273(30):18857–18863. doi:10.1074/jbc.273.30.18857
Atuma C, Strugala V, Allen A, Holm L (2001) The adherent gastrointestinal mucus gel layer: thickness and physical state in vivo. Am J Physiol Gastrointest Liver Physiol 280(5):G922–G929
Barrios JM, Lichtenberger LM (2000) Role of biliary phosphatidylcholine in bile acid protection and NSAID injury of the ileal mucosa in rats. Gastroenterology 118(6):1179–1186
Besseris GJ, Yeates DB (2007) Rotating magnetic particle microrheometry in biopolymer fluid dynamics: mucus microrheology. J Chem Phys 127(10):105106
Celli J, Gregor B, Turner B, Afdhal NH, Bansil R, Erramilli S (2005) Viscoelastic properties and dynamics of porcine gastric mucin. Biomacromolecules 6(3):1329–1333
Cone RA (2009) Barrier properties of mucus. Adv Drug Deliv Rev 61(2):75–85
Corfield AP, Myerscough N, Longman R, Sylvester P, Arul S, Pignatelli M (2000) Mucins and mucosal protection in the gastrointestinal tract: new prospects for mucins in the pathology of gastrointestinal disease. Gut 47(4):589–594
Dekker J, Rossen JWA, Buller HA, Einerhand AWC (2002) The MUC family: an obituary. Trends Biochem Sci 27(3):126–131
Godl K, Johansson MEV, Lidell ME, Morgelin M, Karlsson H, Olson FJ, Gum JR, Kim YS, Hansson GC (2002) The N terminus of the MUC2 mucin forms trimers that are held together within a trypsin-resistant core fragment. J Biol Chem 277(49):47248–47256. doi:10.1074/jbc.M208483200
Hansson GC (2012) Role of mucus layers in gut infection and inflammation. Curr Opin Microbiol 15(1):57–62. doi:10.1016/j.mib.2011.11.002
Hansson GC, Johansson MEV, Lidell ME (2005) Biosynthesis and secretion of mucins, especially the MUC2 mucin, in relation to cystic fibrosis. In: Schultz C (ed) Defects of secretion in cystic fibrosis, vol. 558. Advances in experimental medicine and biology. Springer, New York pp 169–178
Johansson ME, Phillipson M, Petersson J, Velcich A, Holm L, Hansson GC (2008) The inner of the two Muc2 mucin-dependent mucus layers in colon is devoid of bacteria. Proc Natl Acad Sci USA 105(39):15064–15069
Johansson MEV, Ambort D, Pelaseyed T, Schutte A, Gustafsson JK, Ermund A, Subramani DB, Holmen-Larsson JM, Thomsson KA, Bergstrom JH, van der Post S, Rodriguez-Pineiro AM, Sjovall H, Backstrom M, Hansson GC (2011) Composition and functional role of the mucus layers in the intestine. Cell Mol Life Sci 68(22):3635–3641. doi:10.1007/s00018-011-0822-3
Johansson MEV, Larsson JMH, Hansson GC (2011) The two mucus layers of colon are organized by the MUC2 mucin, whereas the outer layer is a legislator of host–microbial interactions. Proc Natl Acad Sci U S A 108:4659–4665. doi:10.1073/pnas.1006451107
Komiyama Y, Mitsuyama K, Masuda J, Yamasaki H, Takedatsu H, Andoh A, Tsuruta O, Fukuda M, Kanauchi O (2011) Prebiotic treatment in experimental colitis reduces the risk of colitic cancer. J Gastroenterol Hepatol 26(8):1298–1308. doi:10.1111/j.1440-1746.2011.06690.x
Lai SK, Wang YY, Cone R, Wirtz D, Hanes J (2009) Altering mucus rheology to “solidify” human mucus at the nanoscale. PLoS ONE 4(1):e4294
Lai SK, Wang YY, Hanes J (2009) Mucus-penetrating nanoparticles for drug and gene delivery to mucosal tissues. Adv Drug Deliv Rev 61(2):158–171
Lai SK, Wang YY, Wirtz D, Hanes J (2009) Micro- and macrorheology of mucus. Adv Drug Deliv Rev 61(2):86–100
Laine L, Takeuchi K, Tarnawski A (2008) Gastric mucosal defense and cytoprotection: bench to bedside. Gastroenterology 135(1):41–60
Lang TA, Hansson GC, Samuelsson T (2007) Gel-forming mucins appeared early in metazoan evolution. Proc Natl Acad Sci U S A 104(41):16209–16214. doi:10.1073/pnas.0705984104
Larsson JMH, Karlsson H, Sjovall H, Hansson GC (2009) A complex, but uniform O-glycosylation of the human MUC2 mucin from colonic biopsies analyzed by nanoLC/MSn. Glycobiology 19(7):756–766. doi:10.1093/glycob/cwp090
Lidell ME, Johansson MEV, Morgelin M, Asker N, Gum JR, Kim YS, Hansson GC (2003) The recombinant C-terminus of the human MUC2 mucin forms dimers in Chinese-hamster ovary cells and heterodimers with full-length MUC2 in LS 174T cells. Biochem J 372:335–345. doi:10.1042/bj20030003
Macierzanka A, Rigby NM, Corfield AP, Wellner N, Böttger F, Mills ENC, Mackie AR (2011) Adsorption of bile salts to particles allows penetration of intestinal mucus. Soft Matter 7:8077–8084. doi:10.1039/C1SM05888F
Macierzanka A, Böttger F, Rigby NM, Lille M, Poutanen K, Mills ENC, Mackie AR (2012) Enzymatically structured emulsions in simulated gastrointestinal environment: impact on interfacial proteolysis and diffusion in intestinal mucus. Langmuir (in press)
Maconi G, Ardizzone S, Cucino C, Bezzio C, Russo AG, Porro GB (2010) Pre-illness changes in dietary habits and diet as a risk factor for inflammatory bowel disease: a case–control study. World J Gastroenterol 16(34):4297–4304. doi:10.3748/wjg.v16.i34.4297
Marciani L, Gowland PA, Spiller RC, Manoj P, Moore RJ, Young P, Fillery-Travis AJ (2001) Effect of meal viscosity and nutrients on satiety, intragastric dilution, and emptying assessed by MRI. Am J Physiol Gastrointest Liver Physiol 280(6):G1227–G1233
Marciani L, Cox EF, Hoad CL, Pritchard S, Totman JJ, Foley S, Mistry A, Evans S, Gowland PA, Spiller RC (2010) Postprandial changes in small bowel water content in healthy subjects and patients with irritable bowel syndrome. Gastroenterology 138(2):469–477
McAuley JL, Linden SK, Png CW, King RM, Pennington HL, Gendler SJ, Florin TH, Hill GR, Korolik V, McGuckin MA (2007) MUC1 cell surface mucin is a critical element of the mucosal barrier to infection. J Clin Invest 117(8):2313–2324
McGuckin MA, Linden SK, Sutton P, Florin TH (2011) Mucin dynamics and enteric pathogens. Nat Rev Microbiol 9(4):265–278. doi:10.1038/nrmicro2538
McRorie J, Brown S, Cooper R, Givaruangsawat S, Scruggs D, Boring G (2000) Effects of dietary fibre and olestra on regional apparent viscosity and water content of digesta residue in porcine large intestine. Aliment Pharmacol Ther 14(4):471–477
Mukhopadhyay S, Maitra U (2004) Chemistry and biology of bile acids. Curr Sci 87(12):1666–1683
Nordgard CT, Draget KI (2011) Oligosaccharides as modulators of rheology in complex mucous systems. Biomacromolecules 12(8):3084–3090. doi:10.1021/bm200727c
Patsos G, Corfield A (2009) Management of the human mucosal defensive barrier: evidence for glycan legislation. Biol Chem 390(7):581–590
Perez-Vilar J, Hill RL (1999) The structure and assembly of secreted mucins. J Biol Chem 274:31751–31754
Petersson J, Schreiber O, Hansson GC, Gendler SJ, Velcich A, Lundberg JO, Roos S, Holm L, Phillipson M (2011) Importance and regulation of the colonic mucus barrier in a mouse model of colitis. Am J Physiol Gastrointest Liver Physiol 300(2):G327–G333. doi:10.1152/ajpgi.00422.2010
Round AN, Rigby NM, Garcia de la Torre A, Macierzanka A, Mills ENC, Mackie AR (2012) Ex-vivo MUC2 mucin trimerises in two dimensions to form weakly interacting porous lamellae, which govern the barrier role of intestinal mucus. Biomacromolecules (in press)
Schwarz-Linek J, Valeriani C, Cacciuto A, Cates ME, Marenduzzo D, Morozov AN, Poon WCK (2012) Phase separation and rotor self-assembly in active particle suspensions. Proc Natl Acad Sci U S A 109(11):4052–4057. doi:10.1073/pnas.1116334109
Sellers LA, Allen A, Morris ER, Rossmurphy SB (1991) The rheology of pig small intestinal and colonic mucus—weakening of gel structure by non-mucin components. Biochim Biophys Acta 1115(2):174–179
Sheehan JK, Thornton DJ, Howard M, Carlstedt I, Corfield AP, Paraskeva C (1996) Biosynthesis of the MUC2 mucin: evidence for a slow assembly of fully glycosylated units. Biochem J 315:1055–1060
Sheng YH, Hasnain SZ, Florin THJ, McGuckin MA (2012) Mucins in inflammatory bowel diseases and colorectal cancer. J Gastroenterol Hepatol 27(1):28–38. doi:10.1111/j.1440-1746.2011.06909.x
Spaeth G, Berg RD, Specian RD, Deitch EA (1990) Food without fiber promotes bacterial translocation from the gut. Surgery 108(2):240–247
Sprong RC, Schonewille AJ, van der Meer R (2010) Dietary cheese whey protein protects rats against mild dextran sulfate sodium-induced colitis: role of mucin and microbiota. J Dairy Sci 93(4):1364–1371. doi:10.3168/jds.2009-2397
Taylor C, Pearson JP, Draget KI, Dettmar PW, Smidsrod O (2005) Rheological characterisation of mixed gels of mucin and alginate. Carbohydr Polym 59(2):189–195. doi:10.1016/j.carbpol.2004.09.009
Thornton DJ, Rousseau K, McGuckin MA (2008) Structure and function of the polymeric mucins in airways mucus. Annu Rev Physiol 70:459–486
Vaishnava S, Yamamoto M, Severson KM, Ruhn KA, Yu XF, Koren O, Ley R, Wakeland EK, Hooper LV (2011) The antibacterial lectin RegIII gamma promotes the spatial segregation of microbiota and host in the intestine. Science 334(6053):255–258. doi:10.1126/science.1209791
Varum FJO, Veiga F, Sousa JS, Basit AW (2010) An investigation into the role of mucus thickness on mucoadhesion in the gastrointestinal tract of pig. Eur J Pharm Sci 40(4):335–341. doi:10.1016/j.ejps.2010.04.007
Wilson LG, Martinez VA, Schwarz-Linek J, Tailleur J, Bryant G, Pusey PN, Poon WCK (2011) Differential dynamic microscopy of bacterial motility. Phys Rev Lett 106(1):018101. doi:10.1103/PhysRevLett.106.018101
Acknowledgments
The authors at IFR would like to acknowledge the BBSRC for their support of this work through the Food and Health Strategic Programme grant to the institute. We would also like to acknowledge Jana Schwarz-Linek and Vincent Martinez at the Institute for Condensed Matter and Complex Systems, University of Edinburgh for the bacterial motility data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mackie, A.R., Round, A.N., Rigby, N.M. et al. The Role of the Mucus Barrier in Digestion. Food Dig. 3, 8–15 (2012). https://doi.org/10.1007/s13228-012-0021-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13228-012-0021-1