Abstracts
Objective
To develop a predictive model for late stillbirth among women with hypertensive disorders of pregnancy (HDP) in low- and middle-income countries.
Materials and Methods
Study was part of the WHO newborn birth defect (NBBD) project and included all stillbirths occurring in the facility from November 2015 to December 2020. The age and parity matched subjects with HDP having live birth were taken as controls. All significant predictors were analyzed and a predictive model was developed.
Results
Out of 69,007 deliveries, 1691(24.5/1000) were stillborn. HDP was seen in (390/1691, 23.0%), in 265/390 (67.4%) cases it occurred at or after 28 weeks of gestation and were included as cases. On comparing the cases with controls, the significant factors were estimated fetal weight less than 2000 gms (P < 0.001, OR 10.3), poor antenatal care (p < 0.001, OR–5.9), family history of hypertension (p < 0.018, OR-4.4) and the presence of gestational hypertension (p = 0.001, OR 2.2). The predictive model had sensitivity and specificity of 80.3% and 70.03%, respectively, the receiver operating curve showed the area under the curve(AUC) in the range of good prediction (0.846).
Conclusion
The predictive model could play a potential role in stillbirth prevention in women with HDP in low- and middle-income countries.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The hypertensive disorders of pregnancy (HDP) is observed in 5–10% of antenatal population [1]. Hypertension in pregnancy has been associated with perinatal mortality and morbidity and is a major contributor to stillbirth, particularly in low- and middle-income countries(LMIC) [2]. World Health Organization South-East Asian Region (WHO SEAR) started a newborn-birth defects (SEAR-NBBD) database in 2014. Simultaneously the project involved keeping a database of stillbirth as well. The analysis of the data generated from the study showed that HDP was the most common maternal condition associated with stillbirth [3]. Most of the morbidity could be prevented by recognizing the early warning signs associated with the disease, leading to adequate monitoring and early delivery in HDP cases and thus preventing stillbirth. Previous studies have examined the associations between stillbirths and clinical and non-clinical characteristics such as late or no antenatal care, inadequate management of anemia, infection, diabetes, and fetal growth restriction [3,4,5]. The knowledge generated upon various studies on the subject would have a positive impact on the prevention of stillbirths if these were applied in promoting targeted interventions and closer monitoring by the health care providers. Hence a user-friendly clinical decision-making tool for the identification of such patients might be beneficial in prioritization of care which is particularly relevant in low resource settings.
Previous studies have used the clinical and biochemical parameters which involved biomarkers and Doppler for the prediction of stillbirth among low-risk population [6,7,8]. The biomarkers like PAPP-A, PlGF are costly and Doppler is often not available in areas where the stillbirths mostly happen, therefore, they are not suitable for LMICs, thus, using clinical and socioeconomic parameters would be more pragmatic in our environment [9]. Therefore the study aimed to develop an easy-to-use tool using clinical and biophysical parameters for the prediction of risk of late stillbirth in women with hypertensive disorders of pregnancy.
Materials and Methods
The study was an observational, analytical case–control study performed from November 2015 to December 2020 at a single tertiary care center after ethical clearance, it was as a part of the WHO SEARO, NBBD stillbirth project. All babies delivered after 20 weeks of gestation showing no sign of life after birth were considered stillborn [10]. All women with HDP having a stillborn baby at 28 weeks or more were considered late stillbirths and were included in the study. The age and parity matched women with hypertensive disorders of pregnancy having live birth were taken as controls.
A detailed maternal history with special reference to high risk factors for stillbirths in the present and previous pregnancies was elicited. The period of gestation was calculated according to the last menstrual period (LMP) or first-trimester ultrasound if the LMP was not known. General physical and systemic examination of the mother, time of admission to the hospital was noted. Antenatal records were reviewed to rule out any abnormal clinical findings. All routine investigations along with an ultrasound for confirmation of intrauterine death were done. The expected fetal weight of the babies was estimated by ultrasound using biparietal diameter, abdominal circumference and femur length using Hadlock formula (Aloka, prosound alpha, Hitachi, Japan). The women with HDP having congenital anomaly in fetus were excluded from the study. Hypertensive disorder of pregnancy (HDP) was taken as any rise of blood pressure 140/90 mm Hg on two occasions four hours apart. Preeclampsia was defined according to ACOG 2013 guidelines [1]. Early-onset hypertension was termed as those which occurred before 34 weeks of gestation. Fetal growth restriction was considered when the birth weight was less than the tenth centile for the gestational age according to the Intergrowth 21 chart [11].
The cases and controls were compared using the chi-square test. The univariate odds ratio was calculated along with 95% confidence limits. Further, Multivariate logistic regression was used to identify the impact of all significant risk factors on the outcome. The best model was attained using the Forward LR model selection criteria. The threshold of predicted probabilities for distinguishing stillbirth and live birth was obtained using the ROC curve. A formula was created using the threshold value of 50% obtained under the ROC curve to predict the outcome variable. A p-value < 0.05 was considered statistically significant. IBM SPSS version 20.0 software is used for statistical analysis.
Results
In the study period of five years and one month, there were 69,007 deliveries at the institution, out of which 1691 (24.5/1000) were stillborn. HDP was observed as the most common maternal cause (390/1691, 23.0%), it occurred at or after 28 weeks of gestation in 265/390 (67.4%) cases and hence included as cases in the study. For comparison 288, age and parity matched women with HDP having live birth were selected as controls.
The epidemiological profile of cases and controls are given in Table 1. The maternal age ranged from 19 to 40 years, the mean age was 27.14 ± 4.61 in cases. As the cases and controls were age and parity matched, there was no significant difference between the two groups (P > 0.05). There were significantly more women with previous two or more abortions among cases (31/265, 11.7%) compared to controls (19/288, 6.6%) (p = 0.038). There were considerably more subjects with poor prenatal care among cases (128/265, 48.3%) compared to controls (43/288, 14.9%) (p < 0.001). Although there was no significant difference in the family income between cases and controls (p = 0.849), there were significantly more women among cases who were either illiterate or studied only till the primary level (58.5% Vs 36.5%)). There was no significant difference in maternal weight and height between cases and controls. The mean systolic and diastolic blood pressure among cases was significantly higher than controls (p < 0.001). The delivery occurred significantly early in gestation among cases (mean 34.6 ± 3.3 weeks) compared to the controls (36.9 ± 3.4 weeks) (p < 0.001).
Table 2 shows the details pertaining to history and clinical examination of the cases and controls. The women with a family history of hypertension had significantly increased chances of stillbirth (p = 0.007). The stillbirths were considerably more in chronic or gestational hypertensive mothers compared to those having preeclampsia (p = 0.013), and the antihypertensives were given prior to stillbirth in 123/265 (46.4%) cases compared to 156/288 (54.2%) controls, however the difference did not reach statistical significance (P = 0.074). Other associated co-morbidities such as deranged blood sugar and anemia were more common among cases, but the difference was not statistically significant (p > 0.05). Known case of antiphospholipid syndrome was two each case and controls. Almost half of the cases of preeclampsia had associated complications. Abruption was the most common complication (19.6%), followed by eclampsia (3.8%), these complications were considerably more in cases compared to controls (p = 0.042), there was no significant difference in deranged renal function test among cases and controls.
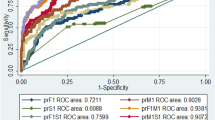
To find out about the degree to which each factor contributed to the stillbirth, the multivariate regression analysis was done and the odds ratio was calculated using binary logistic regression with forward-LR model selection criteria. The best model was obtained in 6 steps wherein explanatory power increased from 27.5 to 45.8% (p < 0.001) (Table 3). Also, the concordance between observed and model's stillbirth outcomes increased from 74.5 to 80%. With the fetal weight less than 2000gms, the odds in favor of the stillbirth were 10.3 times that of live birth (p < 0.001). Due to poor antenatal care, the odds in favor of stillbirth were 5.9 times that of live birth (p < 0.001). If there was a family history of hypertension, the odds in favor of stillbirth were 4.4 times that of live birth (p = 0.018). In the presence of abruption, the odds in favor of stillbirth were 3.4 times that of live birth (p = 0.002). Due to gestational hypertension, the odds in favor of stillbirth were 2.2 times that of live birth (p = 0.001). If the woman was illiterate or had education up to primary level only, the odds in favor of the stillbirth were 1.7 times that of live birth (p = 0.024). The ROC which was constructed showed the composite AUC of all factors to be 0.846 ( 95% CI 0.755–0.835) which was in the region of good prediction(Fig. 1). The fitted equation is given by:
Using the above equation a software using Microsoft excel sheet was created. It was modeled to work as software where the six variables could be clicked as 'yes' or 'no' options. The result would flash as chances of live birth or stillbirth along with the probability in percentage (Fig. 2, excel sheet). The prediction of stillbirth using the software had a sensitivity of 80.3% and specificity of 70.0%.
Discussion
To the best of our knowledge, for the first time, a model for the prediction of the risk of stillbirth in women with HDP has been created. The model is simple, low cost, user-friendly, and can be used in clinical settings, using the parameters involving history, clinical features, and ultrasound biometry for fetal weight estimation. The model allows for early detection of pregnancies at high risk of stillbirth due to hypertension in pregnant women, by a physician or even a health worker and allocation of targeted interventions such as closer monitoring throughout the pregnancy or early delivery. This prioritization of care allocation based on the prediction by the model is particularly relevant in low resource settings.
The data from the last five years of research on the analysis of factors associated with stillbirth under the WHO SEARO project have shown that hypertension in pregnancy was associated with nearly one-quarter of the stillbirths [12], making it the most common maternal cause of stillbirths according to ICD -10 PM coding. In our previous study on the factors associated with stillbirth in hypertensive women, it was noted that 80.6% of them occurred after 28 weeks of gestation, thus, the babies were salvageable and could be saved by timely intervention [13]. Therefore, it was pertinent that the factors associated with salvageable babies be pondered upon to find out ways to prevent them.
In the present prediction model six variables which contributed most to stillbirth on regression model, namely, less than four antenatal visits, gestational/ chronic hypertension, abruption, fetal weight less than 2000gms, education only to primary/ no education, and family history of hypertension were used in a modified excel sheet with options as "yes" and "no" against each. Although, abruption occurs as a late event, it was included with all other significant prenatal factors as its presence would alert the health care personnel regarding a very high risk of impending stillbirth if "yes" was clicked. If abruption would not be present "no" could be clicked.
To date, there have been very few studies regarding the development of a decision-making tool for prediction of the risk of stillbirth. Moreover, these models involved estimation of biomarkers and doppler studies which are difficult to apply in the low-resource settings [6, 7]. In the model developed by Akolekar et al., the prediction stillbirth was studied in low risk women by the maternal factors along with the estimation of biomarker PlGF levels and doppler in the first and second trimester of pregnancy, with the use of the maternal factors alone, 16% of all stillbirths could be predicted at a 5% false-positive rate (FPR), and with the addition of biomarkers, the prediction rate increased to one-third of all stillbirths at the end of the first trimester and nearly half at the end of second trimester [6,7,8]. The model developed in the present study is for women with hypertensive disorder of pregnancy in late second or third trimester.
In our study we found that the area under the receiver operating curve (AUROC) was in good prediction range (0.846). The sensitivity was as high as 80.3% at the specificity of 70.0%. In a study by Koivu et al., a model was developed using clinical parameters with the help of artificial intelligence, in the study the best-performing machine learning models achieved 0.76 AUC for early stillbirth, 0.63 for late stillbirth [14], in another study by Kayode et al., done in a low resource setting, using clinical parameters the discriminative performance of the final basic model was very good with a C-statistic of 0.80 (95% CI 0.78–0.83) [15]. Therefore, in the present study, the sensitivity specificity and the AUC were better than previous studies.
The major strengths of the study were its large sample size and a novel attempt to create a practically feasible model for predicting stillbirth in hypertensive pregnant women for a population that is the most vulnerable to this risk. The major limitation of the study could be the possibility of an overestimation of the performance of screening as it was derived and tested using the same dataset, therefore, consequently, the model needs validation from prospective studies.
The study demonstrates that nearly four fifths of deaths occurring in the study population could have been predicted using a simple, user friendly tool. This model would be particularly effective in low resource settings and would be useful in guiding the clinicians for active intervention and thus aid in its prevention.
References
American College of Obstetricians and Gynecologists. Hypertension in pregnancy Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122–31.
Saleem S, Tikmani SS, McClure EM, et al. Trends and determinants of stillbirth in developing countries: results from the Global Network’s Population-Based Birth Registry. Reprod Health. 2018;15(Suppl 1):100.
Singh A, Kumar M. An Analysis of Cause of Stillbirth in a Tertiary Care Hospital of Delhi: A Contribution to the WHO SEARO Project. J Obstet Gynaecol India. 2019;69(2):155–60.
Liu L-C, Wang Y-C, MuHsien Yu, et al. Major risk factors for stillbirth in different trimesters of pregnancy a systematic review. Taiwan J Obstet Gynecol. 2014;53:141–5.
Goldenberg RL, McClure EM, Saleem S, et al. Infection-related stillbirths. Lancet. 2010;6736(09):61712–8.
Akolekar R, Machuca M, Mendes M, et al. Prediction of stillbirth from placental growth factor at 11–13 weeks. Ultrasound Obstet Gynecol. 2016;48:618–23. https://doi.org/10.1002/uog.17288.
Yerlikaya G, Akolekar R, McPherson K, Syngelaki A, H NK. Prediction of stillbirth from maternal demographic and pregnancy characteristics. Ultrasound in Obstetrics and Gynecology. 2016;48(5):607–612.
Mastrodima S, Akolekar R, Yerlikaya G, Tzelepis T, Nicolaides K Prediction of stillbirth from biochemical and biophysical markers at 11–13 weeks. Ultrasound in obstetrics & gynecology 48 (2016).
Antwi E, Amoakoh-Coleman M, Vieira DL, et al. Systematic review of prediction models for gestational hypertension and preeclampsia. PLoS ONE. 2020;15(4): e0230955. https://doi.org/10.1371/journal.pone.0230955.
Acog practice bulletin no. 102: Management of stillbirth. Obstet Gynecol. 2009;113(3):748–61.
Villar J, Cheikh Ismail L, Victora CG, et al. International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet. 2014;384:857–68.
Kumar M, Vajala R, Bhutia P, et al. Factors contributing to late stillbirth among women with pregnancy hypertension in a developing country. Hypertens Pregnancy. 2020;12:1–7.
Kumar M, Singh A, Garg R, et al. Hypertension during pregnancy and risk of stillbirth: challenges in a developing country. J Matern Fetal Neonatal Med. 2019;25:1–7.
Koivu A, Sairanen M. Predicting risk of stillbirth and preterm pregnancies with machine learning. Health Inf Sci Syst. 2020;8:14. https://doi.org/10.1007/s13755-020-00105-9.
Kayode GA, Grobbee DE, Amoakoh-Coleman M, et al. Predicting stillbirth in a low resource setting. BMC Pregnancy Childbirth. 2016;16:274.
Acknowledgements
The Project has been funded by WHO SEARO. We are thankful to Mr. Yogember Negi for his contribution as a computer data operator of the project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no relevant financial, personal, political, intellectual or religious interests among authors to disclose.
Ethical Statement
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Manisha Kumar, Professor, Department of Obstetrics and Gynecology, Lady Hardinge Medical College, New Delhi. V Ravi, Assistant Professor, Department of Statistics, Lady Sri Ram College, New Delhi. Deepika Meena, Associate Professor, Department of Obstetrics and Gynecology, Lady Hardinge Medical College, New Delhi. Kanika Chopra, Assistant Professor , Department of Obstetrics and Gynecology, Lady Hardinge Medical College, New Delhi. Shilpi Nain, Professor, Department of Obstetrics and Gynecology, Lady Hardinge Medical College, New Delhi. Manju Puri, Director Professor and HOD, Department of Obstetrics and gynecology, Lady Hardinge Medical College, New Delhi.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kumar, M., Ravi, V., Meena, D. et al. Predictive Model for Late Stillbirth Among Antenatal Hypertensive Women. J Obstet Gynecol India 72 (Suppl 1), 96–101 (2022). https://doi.org/10.1007/s13224-021-01561-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-021-01561-3