Abstract
Objectives
To analyse the clinical presentation, histological type, management, and prognosis of cases diagnosed with uterine sarcomas.
Methodology
This was a hospital-based retrospective study conducted at the Institute of Obstetrics and Gynaecology, Chennai, and Meenakshi Medical College and RI, Kancheepuram, from 2009 to 2015. Thirty patients who were diagnosed with uterine sarcoma were analysed for type of sarcoma, clinical details, treatment, and prognosis.
Results
Leiomyosarcoma was the commonest type seen in ten cases followed by mixed mullerian tumours in nine cases and endometrial stromal sarcomas in six cases. Leiomyosarcomas and mixed mullerian tumours were seen between the ages of 45 and 65 years. Women with endometrial stromal tumours were younger in the age group between 35 and 45 years. Pelvic mass and pain were the predominant symptom in leiomyosarcoma and mixed mullerian tumours. Endodermal stromal tumours presented predominantly with abnormal uterine bleeding. Forty percentage of cases were diagnosed with stage I disease. Twenty-six patients were managed surgically. Post-operative adjuvant therapy was given in 12 patients. Median duration of follow-up was 52 months. During the above period, 11 were alive, eight were lost to follow-up, and 11 were dead. In those who were alive, two cases presented with local recurrences.
Conclusion
The pre-operative diagnosis of sarcoma is difficult and prognosis is poor even in early stage disease because of the aggressive nature of the tumours.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uterine sarcomas are rare tumours of the uterus accounting for 3% of all uterine malignancies [1]. These are aggressive tumours, and the mortality associated with this tumour is very high. These tumours also have a varied histological picture. Depending on the cell of origin, and their growth pattern, WHO in 2003 classified uterine sarcomas into two main groups, namely the mesenchymal tumours and the mixed epithelial and mesenchymal tumours. The mesenchymal tumours include leiomyosarcoma, endometrial stromal sarcomas, and undifferentiated endometrial sarcomas. The mixed epithelial and mesenchymal tumours include carcinosarcoma, mullerian adenosarcomas, and the adenofibromas. The aim of this study was to analyse the clinical presentation, the histological type, management, and prognosis of cases diagnosed with uterine sarcoma.
Methodology
This was a hospital-based retrospective study conducted at the Institute of Obstetrics and Gynaecology, Chennai, and Meenakshi Medical College and RI, Kancheepuram, from 2009 to 2015. During the above period, 30 women were diagnosed with sarcoma of the uterus. The hospital records of these patients were analysed for demographic details, clinical presentation, the histopathological features, treatment, and the prognosis.
Results
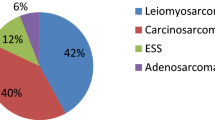
During the study period, there were 6897 gynaecological malignancies, and sarcomas were diagnosed in 30 (0.43%) cases which accounted for 16.2% of all uterine malignancies. Based on the histological features, leiomyosarcoma was the commonest type seen in ten patients (33.3%), followed by mixed mullerian tumours (MMT) seen in nine patients (30%), endometrial stromal sarcoma (ESS) in six patients (20%), and undifferentiated sarcomas were seen in five patients (16.6%).
Clinical Profile of the Patients: (Table 1).
Age analysis showed that leiomyosarcomas and mixed mullerian tumours were seen between the ages of 45 and 65 years and women with endometrial stromal sarcomas tend to be between 35 and 45 years of age. Pelvic mass and lower abdominal pain were the predominant symptoms seen in nearly 50% of leiomyosarcomas and mixed mullerian tumours. Leiomyosarcomas also presented with post-menopausal bleeding (PMB) in two cases, and one case presented with perimenopausal abnormal uterine bleeding (AUB) at the age of 44. PMB was also seen in four of the nine cases who were diagnosed with mixed mullerian tumours. Patients with endometrial stromal sarcomas were younger, and five of the six cases presented with perimenopausal AUB and one case presented with a pelvic mass. Abnormal vaginal discharge was the only presenting symptom in one case each of leiomyosarcoma and mixed mullerian tumour. Interestingly, one case of leiomyosarcoma presented with chronic inversion of the uterus (Fig. 1). There were five cases of undifferentiated sarcomas of the uterus, where all women were post-menopausal more than 50 years of age. The predominant symptom was post-menopausal bleeding in four cases, and one case presented with pelvic mass and pain. There was no past history of uterine or adnexal masses in all 30 patients studied. There was history of loss of weight in seven patients, and general weakness was present in 14 patients. There was no family history of malignancy in all the 30 cases analysed. All of them have delivered more than two children. On clinical examination, in 17 patients, the size of the uterus varied from 12 to 18 weeks. There was no lymphadenopathy, and the breast examination was found to be normal.
USG was reported as leiomyoma in 25 patients and intrauterine polypoidal lesions in four patients. In one of these cases, the findings were suggestive of sarcoma with extensive degeneration and were subsequently confirmed on MRI. USG confirmed inversion of the uterus in one case. Pre-operatively, uterine malignancy was suspected based on the history of PMB in ten patients and intrauterine polypoidal lesions on USG in four patients. In these cases, endometrial curetting was carried out and the HPE was reported as endometrial stromal tumour in two cases, adenosarcoma in one case (Fig. 2) and carcinosarcoma in one case, atrophic endometrium in six patients, and the material was inadequate in four patients.
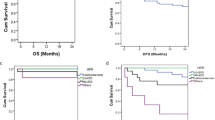
During the study period, 7621 hysterectomies were performed for benign gynaecological conditions and among them, in 15 patients (0.19%), a diagnosis of uterine sarcomas was made after surgery. All these 15 patients had undergone open hysterectomy for fibroids/AUB. In 15 patients in whom uterine malignancy was suspected pre-operatively, surgery could not be undertaken in four cases due to the advanced stage of the disease and poor surgical risk. FNAC of the pelvic mass in these cases showed undifferentiated sarcoma in two cases and carcinosarcoma in one case and leiomyosarcoma in one case. One patient presented with chronic inversion of the uterus and biopsy of the lesion confirmed high-grade leiomyosarcoma, and this case was managed by vaginal hysterectomy. The remaining ten patients were managed by debulking surgery/TAH + BSO/TAH + BSO + omentectomy/and TAH + BSO + omentectomy + pelvic lymphadenectomy (Table 2). On metastatic workup, four cases had stage IV disease with distant metastasis. Liver was involved in one case of leiomyosarcoma; liver and lungs were involved in one case each of malignant mixed mullerian tumour and undifferentiated sarcoma of the uterus. Liver and para-aortic nodes were involved in one case of high-grade ESS. Majority of leiomyosarcomas and mixed mullerian tumours were diagnosed with stage I disease, but were of high-grade lesions, whereas majority of endometrial stromal sarcomas were low grade and were diagnosed at an early stage. Undifferentiated sarcomas were high-grade lesions and were diagnosed with more than stage II disease (Table 3). In 14 patients, only surgery was undertaken. In four patients who were inoperable, chemotherapy was given. Two patients received adjuvant radiotherapy, and ten patients received adjuvant chemotherapy. The median duration of follow-up was 52 months. Because of the high-grade nature, the survival was only 14 months for the follow-up period of 52 months for MMT (Table 4). During the follow-up period, two patients presented with local recurrences. One patient with high-grade leiomyosarcoma had a disease-free survival for 31 months, overall survival was 37 months, and the patient died during the 6 month follow-up. The second case was an adenosarcoma, where the patient developed vaginal metastasis after a disease-free interval of 19 months and was treated with radiotherapy.
Discussion
Uterine sarcoma accounts for approximately 1% of all genital tract malignancies [1]. In our analysis, uterine sarcoma was diagnosed in 0.43% of all gynaecological malignancies. Various studies have shown that uterine sarcoma accounts for 3–8% of all uterine malignancies [1, 2]. However, in our study, the prevalence of uterine sarcoma among all uterine cancers was 16.2%. The incidence of sarcoma is fourfold higher in women more than 50 years compared with younger women [3]. The commonest histological type of uterine sarcoma seen in this study was leiomyosarcoma. Various reports have also shown leiomyosarcoma to be the most common histological type of uterine sarcoma, and it is reported to be a highly aggressive tumour associated with poor prognosis even in early stage disease. Majority of them are primary tumours; rarely, 0.2% may result from a sarcomatous degeneration of a benign leiomyoma [4]. In this analysis, none of the cases had prior history of benign leiomyoma of the uterus. Leiomyosarcomas occur in women more than 40 years of age, and the common symptoms are abnormal vaginal bleeding reported in 56%, palpable pelvic mass in 54%, and pelvic pain in 22% [1]. In this analysis, our youngest patient was 44 years and the oldest was 67 years and 90% of the cases occurred in women of more than 50 years of age. Mass and lower abdominal pain were the predominant symptoms seen in nearly 50% of cases, followed by PMB. Pelvic pain was a common symptom, probably due to the rapid growth of the tumour. One post-menopausal patient presented with profuse vaginal discharge and was subsequently diagnosed with leiomyosarcoma. The presence of a uterine mass and abnormal vaginal discharge should alert the clinician as to the possibility of uterine sarcomas.
Benign uterine leiomyomas (fibroids) are the most common pelvic neoplasms in women, and both leiomyosarcomas and benign leiomyomas have similar symptoms presenting with AUB and pelvic mass. Therefore, it is difficult to differentiate leiomyosarcomas from benign leiomyomas clinically. USG is used as a first-line study to evaluate a uterine mass. USG features suggesting uterine sarcomas are mixed echogenic pattern, central necrosis, and irregular vascularity on Doppler. However, the same features are seen in benign leiomyomas as well [5]. In this analysis, all women were evaluated by USG either for PMB, pelvic mass or for pain. However, only in one case, there was mixed echogenic pattern with extensive necrosis and the MRI suggested the diagnosis of sarcoma. On T1-weighted images in MRI, leiomyosarcomas present as infiltrating heterogeneous hypointensity lesions with irregular margins, and on T2-weighted images, there is hyperintensity indicating extensive necrosis. Benign leiomyomas can also show increased signal intensity on T2-weighted images due to various types of degeneration. It has been recommended to use diffusion-weighted imaging (DWI), which has the potential to delineate malignant lesions when high signal intensity is seen on T2-weighted images [4, 5]. Authors have suggested that with the recent advances in conservative management of fibroids with uterine artery embolization and focused ultrasound surgery, the pre-treatment imaging to diagnose uterine sarcomas is important [4]. In a meta-analysis of women who underwent surgery for presumed leiomyoma, the prevalence of leiomyosarcoma was one in 2000 surgeries [6]. In a study looking at unexpected malignant neoplasm in women who underwent morcellation, 0.27% had uterine cancers/sarcomas [7]. In our study, occult sarcoma was diagnosed in 0.19% of cases.
Management of leiomyosarcoma includes total abdominal hysterectomy and debulking, if the tumour is present outside the uterus. Pelvic and para-aortic lymphadenectomy is not recommended as the lymph node involvement is seen in < 3% of cases. Moreover, they metastasize early to the lungs by haematogenous spread. Post-operative pelvic radiation is also not generally recommended [8]. In this study, seven patients underwent TAH with BSO, debulking was carried out in one patient, vaginal hysterectomy for chronic inversion in one patient, and surgery could not be done in one case. Majority of leiomyosarcomas (40%) were diagnosed at stage I disease, but were high-grade lesions. Adjuvant chemotherapy was given in four patients and radiotherapy in one patient, and the overall survival was 21 months.
Endometrial stromal sarcomas are the second most common pure mesenchymal tumours of the uterus, and they account for 10% of all uterine sarcomas [1]. However, in our analysis, ESS was the third most common uterine sarcomas. Endometrial stromal tumour is composed of cells that resemble endometrial stromal cells of proliferative endometrium. They occur in younger women and the mean age is 42.58, and 10–25% of the affected women are premenopausal [3]. Our patients were also younger and presented at the mean age of 46 years. The usual clinical presentation was AUB in 90% of cases and uterine enlargement. In our analysis, five of the six cases presented with perimenopausal AUB and one case presented with a pelvic mass. In two of these patients, USG showed intrauterine polypoidal lesion and HPE of the endometrium was reported as ESS. Authors have suggested that endometrial sampling can detect some uterine sarcomas [9]. However, the sensitivity of an endometrial biopsy to detect leiomyosarcoma is low [10]. MRI has been shown to be a useful tool in the diagnosis of ESS, which appears as a polypoidal endometrial mass with low-signal on T1-weighted images and high-intensity signals on T2-imaging. Characteristically, they show myometrial, vascular, and lymphatic invasion. On MRI, on T2-weighted imaging, they show worm-like extension bands of low signal intensity within areas of myometrial involvement [5]. These are low-grade, well-differentiated tumours, generally with a favourable prognosis. The 5-year survival rate for stage I disease is reported to be 98%. However, the prognosis is related to the stage of the disease at diagnosis and the 5-year survival for stage II and III disease drops significantly [1, 11]. In our analysis, five of the six were diagnosed with stage I disease and low-grade lesions and one case was diagnosed with stage IV disease with metastasis in the liver and para-aortic nodes. Treatment of ESS is hysterectomy with bilateral salpingo-oophorectomy. Patients may receive adjuvant radiation or hormonal treatment. Even if diagnosed at early stages, ESS can present with late recurrences; therefore, long-term follow-up is mandatory. These tumours have oestrogen and progesterone receptors. Therefore, hormone therapy seems to be effective in preventing recurrences [12]. In this study, one case received chemotherapy and none received hormonal therapy.
Mixed mullerian tumours (MMT) are composed of an epithelial and a stromal component. There are various types of MMT, namely: adenofibroma, adenosarcomas, and carcinosarcomas. In this study, nine patients were diagnosed with mixed mullerian tumours. The commonest histological variant was adenosarcoma which was seen in seven cases. Carcinosarcoma, the most aggressive tumour, was seen in two cases. Majority of them presented after the age of 50 years with pelvic mass and PMB. They were high-grade lesions with poor prognosis. In spite of adjuvant chemotherapy, the overall survival was only 14 months. Adenosarcoma is a slow-growing tumour with low malignant potential. Typically, the uterus is filled with a polypoidal mass and microscopically, there is an admixture of benign, sometimes atypical glandular epithelium and low-grade sarcoma. Occasionally, heterologous elements such as fat, cartilage may be present. On MRI, they present as well demarcated polypoidal mass within the endometrial cavity. Treatment of choice is total abdominal hysterectomy with bilateral salpingo-oophorectomy. Carcinosarcoma is a highly aggressive tumour with epithelial and mesenchymal elements. They present as large polypoidal mass projecting through the cervical os. Microscopically, the epithelial component may be serous or endometrioid type. The mesenchymal component may be homologous with spindle cell sarcoma or heterologous with cartilage or skeletal muscle. The treatment includes total abdominal hysterectomy with salpingo-oophorectomy, removal of pelvic and aortic lymph nodes, omentectomy, and peritoneal cytology. The overall 5-year survival rate is only 30% [13]. Post-operative radiation reduces local recurrence, and overall survival may be improved with adjuvant chemotherapy [14].
Undifferentiated endometrial sarcomas exhibit myometrial invasion, severe nuclear pleomorphism, high mitotic activity, cell necrosis and lack muscle or stromal cell differentiation [3]. Undifferentiated endometrial sarcomas have very poor prognosis. Local recurrences and distant metastasis are common.
Conclusion
Pre-operative diagnosis of uterine sarcoma is often difficult. Women with early stage uterine sarcoma have the same clinical presentation as that of uterine leiomyoma. In the diagnosis, endometrial sampling has a low predictive value for identifying uterine sarcomas. Imaging modalities are unlikely to differentiate uterine leiomyoma from leiomyosarcoma. However, the use of DWI seems to be promising in identifying women who are at high risk for uterine sarcomas. In the management of uterine sarcomas, surgery remains the main stay of management. There is no standard recommendation regarding adjuvant therapy with chemotherapy, radiation, and hormones.
References
D’angelo E, Prat J. Uterine sarcomas: a review. Gynecol Oncol. 2010;116:131–9.
Wu TI, Yen TC, Lai CH. Clinical presentation and diagnosis of uterine sarcoma, including imaging. Best Pract Res Clin Obstet Gynaecol. 2011;25(6):681–9.
Hosh M, Antar S, Nazzal A, et al. Uterine sarcoma, analysis of 13,089 cases based on surveillance, epidemiology and end results database. Int J Gynecol Cancer. 2016;26:1098–104.
Santos P, Cunha TM. Uterine sarcomas: clinical presentation and MRI features. Diagn Interv Radiol. 2015;21:4–9.
Amant F, Coosemans A, Debiec-Rychter M, et al. Clinical management of uterine sarcomas. Lancet Oncol. 2009;10:1188–98.
Pritts EA, Vanness DJ, Berek JS, et al. The prevalence of occult leiomyosarcoma at surgery for presumed uterine fibroids, a meta-analysis. Gynecol Surg. 2015;12:165–77.
Wright JD, Tergas AI, Burke WM, et al. Uterine pathology in women undergoing minimally invasive hysterectomy using morcellation. Obstet Gynaecol Surv. 2014;69:653–4.
Reichardt P. The treatment of uterine sarcomas. Ann Oncol. 2012;23(10):151–7.
Jin Y, Pan L, Wang X, et al. Clinical characteristics of endometrial stromal sarcoma from an academic medical hospital in China. Int J Gynecol Cancer. 2010;20:1535–9.
Hinchcliff EM, Esselen KM, Watkins JC, et al. The role of endometrial biopsy in the preoperative detection of uterine leiomyosarcoma. J Minim Invasive Gynecol. 2016;23(4):567–72.
Shaan SH, Jagannathan JP, Krajewski K, et al. Uterine sarcomas then and now. AJR Am J Roentgenol. 2012;199:213–23.
Tse KY, Crawford R, Ngan HYS. Staging of uterine sarcomas. Best Pract Res Clin Obstet Gynaecol. 2011;25:733–49.
Ferguson SE, Tornos C, Hummer A, et al. Prognostic features of surgical stage I uterine carcinosarcoma. Am J Surg Pathol. 2007;31:1653–61.
Chern JY, Boyd LR, Blank SV. Uterine sarcomas: the latest approaches for these rare but potentially deadly tumors. Oncol J. 2017;31:229–36.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflict of interest.
Informed Consent and Ethical Committee Approval
Being a retrospective hospital records-based study, informed consent and ethical committee approval were not required.
Additional information
Dr. Radha Bai Prabhu Thangappah, MD, DGO, MNAMS, FRCOG, FRCS, PhD is a Professor of Obstetrics and Gynaecology at Meenakshi Medical College and Research Institute, Enathur, Kancheepuram, 631552, Tamil Nadu.
Rights and permissions
About this article
Cite this article
Thangappah, R.B.P. Uterine Sarcoma: A Clinico-Pathological Study. J Obstet Gynecol India 69 (Suppl 2), 147–152 (2019). https://doi.org/10.1007/s13224-018-1141-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-018-1141-5