Abstract
Aim and Objectives
To review the effects of obesity (BMI > 30) on antepartum risk/intrapartum risk. To study neonatal outcome of pregnant women with raised BMI.
Material Method
BMI of 500 pregnant women booked before 12 weeks calculated and categorised as normal, overweight, obese and morbidly obese at GMCH, Aurangabad. Pregnant women with systemic disease and previous LSCS were excluded. Antepartum, intrapartum and neonatal variables were studied, and statistical analysis was carried out.
Results
Antepartum variables: prolonged pregnancy (<0.05), severe PIH (<0.05), PPROM (<0.05), gestational DM (<0.05) and anaemia (<0.05) are strongly associated with raised BMI, whereas abortion (>0.05), oligohydramnios (>0.05), UTI (>0.05) and abruption (>0.05) are not associated with raised BMI. Postpartum variables: PPH (<0.05), pyrexia (<0.05), prolonged hospital stay (<0.05) and lactational dysfunction (<0.05) are strongly associated with raised BMI, whereas UTI (>0.05), thrombophlebitis (>0.05) and endometritis (>0.05) are not associated with raised BMI. BMI Neonatal outcome: IUGR (<0.05), preterm (<0.05), postterm (<0.05), LBW (<0.05) and macrosomia (>0.05) are strongly associated with raised BMI, whereas stillbirth (>0.05), intubation (>0.05), RDS (>0.05) and baby died within 24 (>0.05) are not associated with raised BMI.
Conclusions
Overweight and obesity are risk factors for AP/IP/PP complication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a state of excess adipose tissue mass. Adipose mass increases by enlargement of adipose cells as well as by an increase in number of adipocytes [1]. In recent times body mass index (BMI) is widely accepted as a better measure of overweight, obesity and underweight. World Health Organisation (WHO) has defined the criteria of overweight as BMI > 25 and that for obesity as >30 [2].
The WHO reported in 2005 that 1.6 billion adults were overweight (BMI > 25) and 400 million were obese (BMI > 30). The prevalence of morbid obesity has increased by 50 % between 2000 and 2005 with 8 % of women in the reproductive age group being morbidly obese [3]. This study aimed to examine the prevalence and trends of overweight, obesity and undernutrition in recent decades in India. Based on a systematic literature search on PubMed and other data sources, most published studies were regional or local surveys in urban areas, while good representative data from the India National Family Health Surveys (NFHS, 1992–1993, 1998–1999 and 2005–2006) allowed for examining the trends at the national level. Overall, the available data showed that in India, prevalence of overweight was low while that of undernutrition remained high. Overweight was more prevalent among female [4]. Overweight and obesity in Indian women have increased from 10.6 to 14.5 %. The obesity epidemic affects all including women on reproductive age [5].
Gestational diabetes mellitus, preeclampsia, induction of labour, increase rate of caesarean section, postpartum haemorrhage, anaemia, urinary tract infection, wound infection, prolonged pregnancy and preterm labour were significantly more common in pregnant women with higher BMI [6]. The infants born to obese women are at higher risk of having perinatal complications. The incidence of low APGAR scores, birth defects, macrosomia, birth injuries, shoulder dystocia require admission to neonatal intensive care units more often than do infants of normal weight mothers [7].
Aims and Objectives
-
To review the effects of obesity (BMI > 30) on antepartum risk/intrapartum risk.
-
To study neonatal outcome of pregnant women with raised BMI.
Materials and Methods
A prospective study was conducted at the Government Medical College hospital Aurangabad. Study population was 500.
Methodology
Inclusion and exclusion criteria for study were defined. Pregnant women who visited to outpatient department of obstetrics in first trimester were registered. Details regarding name, age, religion and address were taken. At the first visit, height and weight of pregnant women were taken and BMI was calculated. Written valid informed consent was taken. Detailed history was taken and examination was carried out. Maternal BMI at the time of booking was used to determine the effect of BMI on pregnancy outcome. For the purpose of our study, the subjects were classified into groups using Garrow’s grading [7] of obesity based on Quetelet’s index or BMI which was calculated as weight in kilogram/height in metre square [8].
Groups | Status | BMI (kg/m2) |
|---|---|---|
Group A | Normal | 20.0–24.9 |
Group B | Overweight | 25.0–29.9 |
Group C | Obese | 30.0–40.0 |
Group D | Morbidly obese | >40.0 |
The antepartum variables analysed were gestational diabetes, gestational hypertension, pre-eclampsia, eclampsia, anaemia, preterm, prolonged pregnancy, intrauterine growth retardation (IUGR), severe oligohydramnios, urinary tract infection (UTI) and spontaneous abortions.
Intrapartum variables studied were mode of delivery (vaginal delivery/caesarean section), instrumental delivery and shoulder dystocia. The postpartum variables studied were postpartum haemorrhage, pyrexia, urinary tract infection (UTI), prolonged hospital stay, impaired wound healing and wound infection, thrombophlebitis and lactational dysfunction.
The neonatal variables analysed were low birth weight baby (<2000 gm), macrosomia [9] (>4000 gm), prematurity, postmaturity syndrome, neonatal resuscitation, admission to neonatal intensive care unit (NICU), early neonatal death, still birth, neonatal hypoglycaemia, neonatal jaundice and respiratory distress syndrome.
Definitions and Criteria Used
Macrosomia is defined as birth weight more than 4000 g.
GDM was diagnosed when blood sugars were more than 140 mg% 2 h after ingestion of 75 g glucose (DIPSI).
Severe PIH was diagnosed with BP more than 160/110 mm Hg on two occasions 6 h apart, proteinuria more than 2+, E/O oliguria (<400 ml/24 h), cerebral or visual changes, epigastric pain, pulmonary oedema, low platelets and raised LFTs.
Inclusion Criteria
Pregnant women who are booked before 12 weeks of gestational age and delivered at Government Medical College and Hospital, Aurangabad.
Exclusion Criteria
-
Pregnant women who are unbooked.
-
Pregnant women who are registered in second trimester.
-
Pregnant women with previous history of caesarean section.
-
Pregnant women with history of medical disorders, e.g. DM, hypertension, etc.
Statistical Analysis
Statistical comparison between cases and controls was performed using Chi-square test whichever was appropriate, and p value below 0.05 was considered to be statistically significant. Strength of association was studied by calculating odds ratio.
Observations
Results
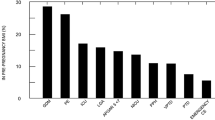
In our study 119 overweight, 97 obese women, and 20 morbidly obese women were compared with 264 women with normal BMI for obstetric behaviour and pregnancy outcome and statistically analysed.
Antepartum variables: prolonged pregnancy (<0.05), severe PIH (<0.05), PPROM (<0.05), gestational DM (<0.05) and anaemia (<0.05) are strongly associated with raised BMI, whereas abortion (>0.05), oligohydramnios (>0.05), UTI (>0.05) and abruption (>0.05) are not associated with raised BMI.
Postpartum variables: PPH (<0.05), pyrexia (<0.05), prolonged hospital stay (<0.05) and lactational dysfunction (<0.05) are strongly associated with raised BMI, whereas UTI (>0.05), thrombophlebitis (>0.05) and endometritis (>0.05) are not associated with raised BMI.
Neonatal outcome; IUGR (<0.05), preterm (<0.05), postterm (<0.05), LBW (<0.05) and macrosomia (>0.05) are strongly associated with raised BMI, whereas stillbirth (>0.05), intubation (>0.05), RDS (>0.05) and baby died within 24 (>0.05) are not associated with raised BMI.
Discussion
Concordant to the literature [9–11], in our study there was significantly higher occurrence of prolonged pregnancy (p < 0.05), severe preeclampsia (p < 0.05), PPROM (p < 0.05), gestational diabetes (p < 0.05) and anaemia (p < 0.05) in obese and overweight women, whereas abortion (p > 0.05), oligohydramnios (p > 0.05), UTI (p > 0.05), abruptio placentae (p > 0.05) and prolonged pregnancy (p > 0.05) are not significantly associated with raised BMI. There were significantly higher rates of caesarean sections (<0.05). These results are consistent with many previous reports [12, 13].
Higher maternal BMI is associated with an increased risk of prolonged pregnancy and increase rate of induction of labour [14]. UTI (p > 0.05) and endometritis (p > 0.05) are not associated with obesity in pregnancy, and observations are consistent with observations made by Meenakshi et al. Thrombophlebitis (p > 0.05) was not observed in pregnant women with normal BMI, and single case was found in overweight pregnant woman so it was not significant. This finding is contrary to findings of Mamula st al.
We have demonstrated that obese pregnant women are more likely to deliver macrosomic babies (p < 0.05). An increased incidence of IUGR (p < 0.05), preterm birth (p < 0.05), postterm babies (p < 0.05) and neonatal jaundice (p < 0.05) among overweight and obese women were noted in our study.
Conclusion
Obesity is modifiable and preventable.
Preconception counselling and awareness regarding exercise and healthy, nutritious diet should be done.
Pregnant women with high BMI is considered as high-risk pregnancy.
Screening for hypertension and DM must be performed before conceiving and in first antenatal visit.
References
World Health Organisation. Diet, nutrition, and the prevention of diseases: report of a joint WHO/FAO expert consultation. Technical report series 916. Geneva, Switzerland: World Health Organisation; 2002.
World Health Organisation. Obesity and overweight. The highlighted should be changed to: accessed November 15 2011. http://www.who.int/mediacenter/factsheets/fs311/en/index.html.
Wang Y, Chen HJ, Shaikh S, et al. Is obesity becoming a public health problem in India? Examine the shift from under to overnutrition problems over time. Obes Rev. 2009;10:456–74.
Balranjan Y, Villamor E. Nationally representative surveys show recent increases in the prevalence of overweight and obesity among women of reproductive age in Bangladesh, Nepal, and India. J Nutr. 2009;139:2139–44.
Kumara P, Gupta M, Kahlon P, et al. Association between high BMI and feto-maternal outcome. J Obes Metab Res. 2014;3:143–4.
Vasudevan C, Renfrew M, McGuire W. Fetal and perinatal consequences of maternal obesity. Arch Dis Child Fetal Neonatal Ed. 2011;96:F378–82.
Garrow JS. Indices of adiposity. Nutr Abstr Rev Ser. 1983;A53:697–708.
Sebire NJ, Jolly M, Harris JP, et al. Maternal obesity and pregnancy outcome: a study of 287 213 pregnancies in London. Int J Obes Relat Metab Discord. 2001;25:1175–82.
Srivastava R, Sharma NR, Kushwaha KP, et al. Obstetrics behavior and pregnancy outcome in overweight and obese women. J Obstetrics Gynaecol India. 2012;62(3):276–80.
Mamula O, Severinski N, Mamula M, et al. Complications during pregnancy—labour and puerperium in women with increase BMI at pregnancy term. Cent Eur J Med. 2009;4(1):71–5.
Islam A, Khan NA, Ehsan A. Complications of raised BMI in pregnancy. Professor Med J. 2010;7(3):498–504.
Bhattachrya S, Campbell DM, Campbell WA, et al. Effect of body mass index on pregnancy outcome in nulliparous women delivering singleton baby. BMC Public Health. 2007;7:168.
Arrowsmith S, Susan W, Siobhan Q. Maternal obesity and labour complications following induction of labour in prolonged pregnancy. BJOG Int J Obstet Gynaecol. 2011;118(5):578–588. doi:10.1111/j.1471-0528.2010.02889.x
Yu C, et al. Obesity in Pregnancy. BJOG. 2006;113:1117–25.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Informed Consent
Taken from Patient.
Ethical Committee
Approval taken.
Additional information
Varsha L. Deshmukh is Associate Professor & Unit Incharge of Obstetrics and Gynaecology at Government Medical College; Milind Jadhav is Resident of Obstetrics and Gynaecology at Government Medical College; Kanan Yelikar is HOD of Obstetrics and Gynaecology at Government Medical College.
Rights and permissions
About this article
Cite this article
Deshmukh, V.L., Jadhav, M. & Yelikar, K. Impact of HIGH BMI on Pregnancy: Maternal and Foetal Outcome. J Obstet Gynecol India 66 (Suppl 1), 192–197 (2016). https://doi.org/10.1007/s13224-015-0825-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-015-0825-3