Abstract
Objective
The objective of this study was to identify clinical practices worldwide, which would help in recognizing women at risk of excessive bleeding or of developing pelvic infection following trans-vaginal ovum pick-up (TV-OPU), measures taken to minimize risks and their management.
Method
A prospective, web-based questionnaire with distinct questions related to the practice of TV-OPU.
Results
A total of 155 units from 55 countries performing 97,200 IVF cycles annually responded to this web-based survey. A majority (65 %) responded that they would routinely carry out full blood count, while 35 % performed coagulation profile. Less than a third agreed screening women for vaginal infections. About a third used both sterile water and antiseptic to minimize ascending infection, and 52 % used antibiotics for prophylaxis. Doppler ultrasound was routinely used by 20 % of clinicians. 73 % of the clinicians preferred conservative management as their first line management for patients diagnosed with intra-abdominal bleeding.
Conclusion
The study has identified a wide variation in the practices of minimizing infection and bleeding complications. The dearth of good quality evidence may be responsible for the lack of published guidelines, and therefore a lack of consensus on the optimum practice for minimizing the risk of infection and bleeding during TV-OPU.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trans-vaginal ultrasound-guided ovum pick-up (TV-OPU) under ultrasound guidance is an essential procedure of assisted reproductive technique (ART). TV-OPU is a relatively straight forward and a safe procedure, compared with the historical laparoscopic and complex trans-abdominal approaches. All surgical procedures are associated with complications and therefore, a sharp needle introduced through the vaginal walls into the ovaries at TV-OPU carries the risks of bleeding, infection, and injury to the surrounding abdominal viscera. Though uncommon, severe bleeding and infection are the most commonly quoted complications with TV-OPU.
IVF-Worldwide.com is the most comprehensive IVF focused website for clinicians, embryologists, fertility nurses, and social workers from over 3,000 clinics across the world. The website is managed by two founders and a 58 member advisory board who are internationally recognized fertility experts. This website serves as a platform for clinicians to discuss specialist treatments and to further research activities related to ART. It offers significant educational material to the clinicians and provides an opportunity to locate IVF units around the world and to communicate directly with the unit. IVF-Worldwide has been conducting surveys on various aspects of fertility practices and provides a large and diverse sample size from across the world and therefore, possibly, a better evaluation.
The objective of this study was to identify clinical practices worldwide that would enable clinicians in recognizing women at risk of excessive bleeding or of developing pelvic infection following TV-OPU. Further it would aid in identifying measures taken to minimize these risks and their subsequent management.
Materials and Methods
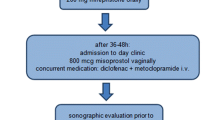
This study involved a prospective, web-based questionnaire with 14 distinct questions related to the practice of egg retrieval. The questionnaire entitled ‘Minimising the risk of infection and bleeding at trans-vaginal ultrasound guided ovum pick-up’ was approved by the advisory board members of the IVF-Worldwide.com website. The questions were related to recognition of women at risk of developing excessive bleeding and infection following TV-OPU, the precautionary measures taken to minimize these risks and the management of these complications, if they occurred. The questionnaire also had five demographics questions that included the clinician’s name, name of the IVF unit, e-mail address, country of practice, and the estimated number of total IVF cycles undertaken by the unit per year.
The survey was published on IVF-Worldwide.com on 23 October 2013, and an e-mail was sent on the same day to all registered members of the website requesting to complete the questionnaire with a series of ‘yes’ or ‘no’ and multiple choice questions and finally their comments. The website does not have a registration fee and is accessible to all clinicians who manage couples with subfertility. Two e-mail reminders were sent each week after the initial questionnaire was sent, requesting the members to complete the survey if they had not already done so. The survey was closed after one month, and the results of the survey were published on the website on 12 January 2014. An e-mail publishing the results of this survey was circulated to all members on 14 January 2014.
Quality Assurance Methods
To overcome the possibility of wrong or duplicate reports from a unit, a software assessed the consistency of four demographics parameters between the self-reported data of the unit surveyed and the existing data of units registered on the IVF-Worldwide website. If a minimum of three of these parameters from the survey matched the website archive data, this reporting site’s data was included in the statistical analyses.
Statistical Analysis
The raw data were uploaded into an automated spreadsheet using Microsoft Excel 2010 (Microsoft, USA), and the analysis was based on the number of IVF cycles reported by the unit, but not on the number of units in the study. Incomplete surveys were excluded from the analysis. For most of the questions, the survey provided ‘yes or ‘no’ or multiple choice answers where only one answer was acceptable. For two questions, multiple answers were accepted. For a question with four answers (a, b, c, d), the following results were calculated.
Results
Of the 195 of respondents who initially started the survey, 40 did not complete the survey. We received the completed survey data from 155 IVF clinics, originating from 52 countries. These clinics across six continents performed 97,200 IVF cycles annually. The highest participation was from the clinics in Europe (n = 64, 41.3 %, 43,300 cycles) followed by Asia (n = 30, 19.4 %, 25,100 cycles) and only 9 (5.8 %, 11,800 cycles) units from Australia and New Zealand and 10 (6.5 % 3,200 cycles) African units contributed to the survey. 19 clinics (12.3 %, 7,400 cycles) from North America and 23 clinics (14.8 %, 6,400 cycles) from South America also participated in the survey. The majority of self-reported IVF cycles from the completed surveys originated from European (44.5 %) and Asian (25.8 %) units (Table 1).
The results of the survey are summarized in Table 2. A majority of clinicians (65 %) responded that they would routinely carry out full blood count (FBC) to assess hemoglobin concentration and platelet count pre-operatively and more than a third (35 %) routinely performed coagulation profile. Only about a third of all participants replied that they perform routine screening tests for vaginal and cervical infections by undertaking high vaginal (32 %) and chlamydia swabs (33 %). According to 39 % of the clinicians who responded to the survey, obesity significantly increased the risk of bleeding complications following OPU, whereas in the opinion of 32 %, retrieving more than 10 oocytes at OPU increased the risk. 34 % of the respondents perceived that women with polycystic ovarian syndrome have a greater risk of bleeding complication following TV-OPU.
Fifty-eight percent of the survey respondents cleaned the vagina with sterile water, 9 % used antiseptic solution, and one-third (33 %) used both sterile water and antiseptic solution before the procedure to minimize the risk of ascending infection. Fifteen percent of the clinicians who perform TV-OPU do not routinely administer prophylactic antibiotics, where as 52 % prefer to use antibiotics prophylactically and a third (34 %) of the clinicians administered antibiotics to women with risk factors such as the presence of endometrioma or past history of pelvic inflammatory disease (PID). There was no uniform agreement in the duration and type of antibiotics used. A Single dose of a single antibiotic was the preferred antibiotic prophylaxis used by 43 % clinicians, but 9 % preferred to use antibiotics for 5 days.
Single lumen needle was the most preferred needle used (81 %), and a majority of the clinicians (51 %) used 17 gage needle for follicular aspiration. A quarter of the clinicians replied that they prefer to use finer needles (15–16 gage). The use of Doppler ultrasound during the egg retrieval procedure is not used by a large majority (62 %) of the clinics. However, Doppler ultrasound-guided egg retrieval is routinely used by 20 % of the clinicians.
A majority (57 %) of the clinicians who answered the survey discharged women home within two hours of the procedure, but 13 % of the clinicians kept women under observation for up to 6 h. The nurses discharged the patients in 59 % of the clinics. Eighty-eight percent of the respondents did not routinely perform a pelvic ultrasound scan, and 98 % did not regularly check FBC before discharging women from the unit.
In the opinion of 73 % of respondents, a conservative approach with hospitalization and close monitoring was the preferred first line management of a woman with a diagnosed intra-abdominal bleeding, where as 25 % stated that they would undertake a diagnostic laparoscopy and proceed. 70 % of the respondents answered that a firm vaginal compression for 3–5 min could be used as a measure to arrest continued vaginal bleeding not responding to initial vaginal compression, whereas, 55 % perceived that suturing of the bleeding area may be required and 45 % favored vaginal packing for 2 or more hours. 17 % of the clinicians who responded preferred admitting the women to hospital for an overnight observation.
Discussion
TV-OPU is an essential procedure in ART and is routinely undertaken as a day case procedure under sedation or general anesthesia. TV-OPU is now considered as the gold standard procedure for oocytes retrieval for its simplicity, thereby gaining extensive popularity. However, the practice of pre-procedural preparation, the actual procedure, and the subsequent management varies considerably among practitioners due to a lack of published guidelines. The results from this world-wide survey offer interesting results with a majority of controversies still unanswered.
According to the literature, the reported complication rates following TV-OPU vary and mainly come from observational studies and case reports. The most common complication is minor vaginal bleeding (1.4–18.4 %) secondary to accidental injury to the vaginal vessels [1]. The risk of pelvic infection (0.1–0.6 %) [2] and severe intra-abdominal bleeding (0.05–0.2 %) [2–5] is very low. Though severe intra-abdominal bleeding usually occurs as a result of injury to sub-capsular ovarian vessels or small intra-follicular vessels [1], injury to pelvic vessels and coagulation abnormalities can also cause hemoperitoneum and retroperitoneal bleeding [6–9].
Pre-operative surgical preparation is absolutely essential for a safe and successful surgical outcome. It is well recognized that FBC is a basic investigation that is routinely undertaken before any surgical procedure and that anemia and thrombocytopenia both increase the risk of bleeding. El-Shawarby et al. [10] reported an interesting case of essential thrombocythemia related hemoperitoneum following TV-OPU and some case reports have described bleeding complications as a result of coagulopathy [8, 9]. Siristatidis et al. [11] reported that four out of 542 women (0.74 %) who underwent TV-OPU were found to have abnormal platelets, and Fatum et al. [12] reported of eight women in a cohort of 1,800 women (0.44 %) who had bleeding tendency disorder. While some units have a protocol of screening women routinely for coagulopathy [11] and some studies have emphasized the importance of undertaking coagulation profile before the procedure [5], a cross-sectional retrospective study [13] identified the need to screen 534 women for coagulation defects to prevent one case of excessive bleeding associated with abnormal coagulation.
Obesity is recognized to be a risk factor for surgical complications as well as causing technical difficulties at surgery. It is generally believed that large, fragile, over-stimulated and hyper vascularized ovaries, particularly in women with polycystic ovarian syndrome (PCOS) are at an increased risk of having bleeding complications following TV-OPU. However, in their retrospective analysis of 3,241 women undergoing TV-OPU, Liberty et al. [14] found that all the seven women who had significant ovarian hemorrhage were lean with a body mass index (BMI) of 19–21 kg/m2. Zhen et al. [5], in their retrospective analysis of 10,251 IVF cycles, reported five women (0.05 %) with severe intra-peritoneal bleeding and 17 women (0.17 %) with mild intra-peritoneal bleeding. They found that the women who had severe bleeding following the procedure had significantly lower BMI when compared to women with mild or no intra-abdominal bleeding. Interestingly, they also found that significantly more number of oocytes were retrieved from women who had mild bleeding (29.5 ± 5.97) when compared to women with severe (12 ± 4.30) or no (12.1 ± 5.30) intra-abdominal bleeding.
A single lumen needle is technically easier to use, but we did not find any evidence to suggest that the single lumen needle is superior over the double lumen needle in minimizing the risk of bleeding or infection, and also there is no evidence to suggest that a needle with smaller diameter would minimize bleeding and infection risks. The use of color Doppler may detect small blood vessels in the vaginal walls and inside the ovary and may thus reduce the risk of hemorrhage at TV-OPU [15]. Though Serour et al. [16] recommend the routine use of color Doppler at TV-OPU, Risquez and Confino [17] advice that the identification of smaller blood vessels on ultrasound Doppler may not entirely remove the risk of moderate to severe bleeding. Shalev et al. [15] recommend the use of a pelvic ultrasound scan before discharging the women from the unit to identify any pelvic bleeding as patients may become symptomatic some days after the bleeding.
Iatrogenic pelvic infection following TV-OPU can occur as a result of ascending infection (follicular aspiration needle carrying micro-organisms from the vagina into the pelvis), by the reactivation of a dormant infection (from a previous PID) or very unlikely, from fecal peritonitis secondary to bowel injury [6]. Pelvic infections occur within a few days to couple of weeks’ of the procedure, but delayed pelvic infection in early pregnancy and in late pregnancy has also been reported [18–20]. Though, it is widely agreed that the vaginal and chlamydia swabs cannot rule out the infection in all cases, it is essential that every imaginable effort is made to minimize the risk of pelvic infections which can cause significant maternal morbidity.
There is conflicting evidence on the use of antiseptics for vaginal cleaning before OPU. In a prospective randomized study, van Os et al. [21] reported no significant difference in the fertilization and pelvic infection rates, when normal saline was used compared with povidon iodine, but reported a significantly increased clinical pregnancy rates when normal saline was used. However, in a further prospective randomized study, Hannoun et al. [22] identified that vaginal preparation using betadine before TV-OPU did not affect the IVF outcome.
The debate on the use of prophylactic antibiotics for all women before TV-OPU is still open. Egbase et al. [23] reported that prophylactic antibiotics at TV-OPU, not only reduced the number of microbiology positive embryo catheter tips 48 h after the procedure, but also significantly increased implantation and clinical pregnancy rates. The pelvic infection rate was between 0.4 and 0.6 % in some studies where routine antibiotics prophylaxis was not administered [4, 6]. Prophylaxis has been strongly advocated by some authors [24], but substantial evidence for its usefulness seems to be lacking. We, the authors feel that consideration should be given to the use of prophylactic antibiotics to at least women with risk factors such as the presence of endometrioma or previous PID, if not routinely. There is no uniform agreement on the type of antibiotics and the duration of prophylaxis.
It is vital for the clinicians to be aware of various options that can be used to arrest continued vaginal bleeding not responding to initial vaginal compression. Vaginal exploration of the bleeding site using a large speculum with application of pressure using a sponge forceps or a vaginal pack may be required if the vaginal bleeding does not stop after an initial compression and in a minority, suturing may be required if the tear is wide and deep or if it is not responding to the initial measures [25].
Individual approach is essential for the management of a diagnosed haemoperitoneum. Women who are hemodynamically stable can be managed by a conservative approach with close monitoring in the hospital, but diagnostic laparoscopy to arrest the on-going bleeding may be required in some cases.
One of the strengths of our study is that it is the first comprehensive study to evaluate practice patterns of clinicians from across the world focusing on many aspects related to TV-OPU complications, ranging from clinical assumption to various treatment modalities for unexpected complications that can have an impact on patient outcome. The study was available as an open-access questionnaire, and the data collected were anonymous. This approach differs from the traditional surveys where a questionnaire is sent to specific individuals. The other strength of our study is that we were effective in obtaining responses from a large number of IVF units across the world, which may not be possible with traditional surveys. However, our study may be limited by a selection bias as only those clinicians who are members of the website or those who are acquainted with the website would have participated in the survey.
The dearth of published guidelines based on good quality evidence may be responsible for the lack of consensus on many important aspects of TV-OPU procedure related to bleeding and pelvic infection risks. Patients have rights and responsibilities to make an informed decision about their care and treatment, but due to a lack of best evidence from good quality studies, it may not be possible to appropriately advise women about the merits and de-merits of the different practices that are followed. Large prospective multi-centered randomized control studies, taking into consideration the couples’ characteristics and treatment protocols would provide a better understanding of these complications and the ways to prevent them.
We conclude that there is a wide variation in the practice of minimizing the risk of infection and bleeding complications following OPU and in the subsequent management. There is an urgent need to formulate uniform guidelines based on good quality evidence to enable clinicians to undertake safer practices during TV-OPU.
References
El-Shawarby S, Margara R, Trew G, et al. A review of complications following transvaginal oocyte retrieval for in vitro fertilization. Hum Fertil (Camb). 2004;2:127–33.
Ludwig AK, Glawatz M, Griesinger G, et al. Perioperative and post-operative complications of transvaginal ultrasound-guided oocyte retrieval: prospective study of >1,000 oocyte retrievals. Hum Reprod. 2006;21(12):3235–40.
Tureck RW, García CR, Blasco L, et al. Perioperative complications arising after transvaginal oocyte retrieval. Obstet Gynecol. 1993;81(4):590–3.
Govaerts I, Devreker F, Delbaere A, et al. Short-term medical complications of 1,500 oocyte retrievals for in vitro fertilization and embryo transfer. Eur J Obstet Gynecol Reprod Biol. 1998;77(2):239–43.
Zhen X, Qiao J, Ma C, et al. Intraperitoneal bleeding following transvaginal oocyte retrieval. Int J Gynaecol Obstet. 2010;108(1):31–4.
Bennett SJ, Waterstone JJ, Cheng WC, et al. Complications of transvaginal ultrasound-directed follicle aspiration: a review of 2,670 consecutive procedures. J Assist Reprod Genet. 1993;10(1):72–7.
Azem F, Wolf Y, Botchan A, et al. Massive retroperitoneal bleeding: a complication of transvaginal ultrasonography-guided oocyte retrieval for in vitro fertilization-embryo transfer. Fertil Steril. 2000;74(2):405–6.
Battaglia C, Regnani G, Giulini S, et al. Severe intraabdominal bleeding after transvaginal oocyte retrieval for IVF-ET and coagulation factor XI deficiency: a case report. J Assist Reprod Genet. 2001;18(3):178–81.
Moayeri SE, Coutre SE, Ramirez EJ, et al. Von Willebrand disease presenting as recurrent hemorrhage after transvaginal oocyte retrieval. Am J Obstet Gynecol. 2007;196(4):e10–1.
El-Shawarby SA, Margara RA, Trew GH, et al. Thrombocythemia and hemoperitoneum after transvaginal oocyte retrieval for in vitro fertilization. Fertil Steril. 2004;82(3):735–7.
Siristatidis C, Chrelias C, Alexiou A, et al. Clinical complications after transvaginal oocyte retrieval: a retrospective analysis. J Obstet Gynaecol. 2013;33(1):64–6.
Fatum M, Ozcan C, Simon A, et al. The safety of ultrasound-guided oocyte pick-up in IVF patients with haemostatic disorders. Eur J Obstet Gynecol Reprod Biol. 2008;137(2):259–61.
Revel A, Schejter-Dinur Y, Yahalomi SZ, et al. Is routine screening needed for coagulation abnormalities before oocyte retrieval? Fertili Steril. 2011;95(3):1182–4.
Liberty G, Hyman JH, Eldar-Geva T, et al. Ovarian hemorrhage after transvaginal ultrasonographically guided oocyte aspiration: a potentially catastrophic and not so rare complication among lean patients with polycystic ovary syndrome. Fertil Steril. 2010;93(3):874–9.
Shalev J, Orvieto R, Meizner I. Use of color Doppler sonography during follicular aspiration in patients undergoing in vitro fertilization may reduce the risk of blood vessel injury. Fertil Steril. 2004;81(5):1408–10.
Serour GI, Aboulghar M, Mansour R, et al. Complications of medically assisted conception in 3,500 cycles. Fertil Steril. 1998;70(4):638–42.
Rísquez F, Confino E. Can Doppler ultrasound-guided oocyte retrieval improve IVF safety? Reprod Biomed Online. 2010;21(4):444–5.
Sharpe K, Karovitch AJ, Claman P, et al. Transvaginal oocyte retrieval for in vitro fertilization complicated by ovarian abscess during pregnancy. Fertil Steril. 2006;86(1):219.
Patounakis G, Krauss K, Nicholas SS, et al. Development of pelvic abscess during pregnancy following transvaginal oocyte retrieval and in vitro fertilization. Eur J Obstet Gynecol Reprod Biol. 2012;164(1):116–7.
Kim JW, Lee WS, Yoon TK, et al. Term delivery following tuboovarian abscess after in vitro fertilization and embryo transfer. Am J Obstet Gynecol. 2013;208(5):e3–6.
Van Os HC, Roozenburg BJ, Janssen-Caspers HA, et al. Vaginal disinfection with povidon iodine and the outcome of in vitro fertilization. Hum Reprod. 1992;7(3):349–50.
Hannoun A, Awwad J, Zreik T, et al. Effect of betadine vaginal preparation during oocyte aspiration in in vitro fertilization cycles on pregnancy outcome. Gynecol Obstet Invest. 2008;66(4):274–8.
Egbase PE, Udo EE, Al-Sharhan M, et al. Prophylactic antibiotics and endocervical microbial inoculation of the endometrium at embryo transfer. Lancet. 1999;354(9179):651–2.
Weinreb EB, Cholst IN, Ledger WJ, et al. Should all oocyte donors receive prophylactic antibiotics for retrieval? Fertil Steril. 2010;94(7):2935–7.
Orvieto R, Ben-Rafael Z. Bleeding, severe pelvic infection and ectopic pregnancy. In: Gardner DK, Weissman A, Howles CM, Shoham Z, editors. Assisted reproductive techniques: laboratory and clinical perspectives. 4th ed. London: Informa Healthcare; 2012. p. 374–81.
Compliance with ethical requirements and Conflict of interest statement
This article does not contain any studies with human or animal subjects. The survey does not involve human subject research and hence a formal Institutional Review Body approval was not obtained. The study was available as an open-access questionnaire to the members of the IVFWorldwide.com who voluntarily answered the study questions, and the data collected for this research were anonymous. The study does not involve the use of laboratory animals. The authors, Dr. Harish Bhandari, Dr. Rina Agrawal, Dr. Ariel Weissman, Mr. Gon Shoham, Prof. Milton Leong, and Prof. Zeev Shoham declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhandari, H., Agrawal, R., Weissman, A. et al. Minimizing the Risk of Infection and Bleeding at Trans-Vaginal Ultrasound-Guided Ovum Pick-up: Results of a Prospective Web-Based World-Wide Survey. J Obstet Gynecol India 65, 389–395 (2015). https://doi.org/10.1007/s13224-014-0619-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-014-0619-z