Abstract
A total of 194 enterococcal isolates were recovered from 198 fecal samples of pigs, cattle, and sheep obtained in a Portuguese slaughterhouse. The enterococcal species most prevalent were Enterococcus faecium and E. hirae. High percentages of resistance were detected for tetracycline in pig isolates (95.7%), sheep isolates (76.7%), and cattle isolates (49%); erythromycin resistance was higher in pig isolates than in cattle or sheep isolates. Intermediate level of resistance was obtained to quinupristin/dalfopristin in all animal isolates (15.1–23.5%). High-level resistance to aminoglycosides was detected, HLR-S and -K was higher in pig isolates (44.3 and 32.9%, respectively) compared with cattle or sheep isolates, and modest percentages of HLR-G were obtained in pig and cattle isolates (7.1 and 3.9%, respectively). The aac(6`)-aph(2”), aph(3`)-IIIa, ant(6)-Ia, cat(A), erm(B), and tet(M) genes were demonstrated in most of the gentamycin-, kanamycin-, streptomycin-, chloramphenicol-, erythromycin- and tetracycline-resistant isolates, respectively. The association between the tet(M) gene and Tn916/Tn1545-like or Tn5397-like transposons was detected in 30.8 and 11.2% of the isolates, respectively. Food animals could be a reservoir for antibiotic resistance genes, and slaughterhouse cross-contamination of animals carcasses may be a food safety risk.
Similar content being viewed by others
Introduction
Enterococci are ubiquitous bacteria that inhabit the gastrointestinal tract of humans and many animals (mammals, birds, insects, and reptiles) and are commonly found in soil, plants, and water (Hayes et al. 2003; Kuhn et al. 2005).
Although these organisms are not considered as primary pathogens in animals and humans, they have emerged as an increasingly important cause of human nosocomial infections (Kuhn et al. 2005). Enterococci are intrinsically resistant to several commonly used antibiotics (cephalosporins and aminoglycosides) and, perhaps more importantly, is their ability to acquire resistance to all currently available antibiotics (Hayes et al. 2003; Cetinkaya et al. 2000). They acquire resistance to antimicrobial agents through transfer of plasmids and transposons, chromosomal exchange, or mutation (Cetinkaya et al. 2000; Hayes et al. 2003), and might act as reservoir of antibiotic resistance genes that could be transmitted to other bacteria, and, for this reason, might represent a worldwide problem with large repercussions for public health.
The possibility of transfer of antimicrobial-resistant bacteria (pathogens or commensal organisms) from animals to humans has caused increased interest in antimicrobials that are used in both human and veterinary medicine (Jackson et al. 2011). In human medicine, enterococcal infections are often treated with a combination of an aminoglycoside (e.g., gentamycin) and a cell-wall-active agent, such as penicillin or a glycopeptides (e.g., vancomycin), but due to the emergence of resistant strains, new agents like quinupristin/dalfopristin are also used (Hammerum et al. 2010). The use of avoparcin, gentamicin, and virginiamycin for growth promotion and therapy in food animals has led to the emergence of vancomycin- and gentamicin-resistant enterococci and quinupristin/dalfopristin-resistant E. faecium in animals and meat, which implies a potential risk for transfer of resistance genes or resistant bacteria from food animals to humans (Hammerum et al. 2010).
In Portugal, resistant enterococci have been previously isolated from food-producing animals (Poeta et al. 2006; Novais et al. 2005; de Fatima Silva Lopes et al. 2005; Goncalves et al. 2010; Freitas et al. 2009; Costa et al. 2010), from wild animals (Poeta et al. 2005, 2007; Figueiredo et al. 2009), and from the environment (Macedo et al. 2011; Araujo et al. 2010; Freitas et al. 2009).
The cross-contamination of edible carcass tissues during the slaughter process represents a significant food safety hazard. The contamination of carcass tissues occurs mainly with fecal material during the evisceration and the skinning process, and in most of the Portuguese abattoirs these two operations are performed manually, increasing the risk of fecal contamination. The objective of this work was to analyze the prevalence of antibiotic resistance and the mechanisms implicated in non-selected enterococci recovered from fecal samples of animals (pigs, cattle and sheep) in a slaughterhouse located in the center of Portugal.
Materials and methods
Samples and bacterial isolates
Fecal samples were recovered from September 2008 to March 2009 in a slaughterhouse located in the center of Portugal where every day around 200 growing pigs, 100 bovines and 100 sheep (lambs and adult animals) are killed for human consumption; the animals stem from production units located in different regions of Portugal. Enterococcal isolates were recovered from a total of 198 fecal samples obtained from slaughtered animals (73 sheep, 71 pigs and 54 beef cattle). Animals were selected randomly and samples collected on different days of the week and during different periods of the day, to guarantee samples collected from each animal had different origins.
Fecal material was collected from each animal, directly from the rectum after animal evisceration. Samples were collected in sterilized tubes and transported on the same day to the laboratory. A portion of approximately 3 g of each sample was suspended in 3 ml of sterile saline solution and this dilution was seeded on Slanetz-Bartley agar plates and incubated for 48 h at 37°C (Torres et al. 2003). Colonies with typical enterococcal morphology were presumptively identified to the genus level by Gram-staining, catalase test and bile-aesculin reaction (Torres et al. 2003). DNA was extracted by the Instagene™ Purification Matrix protocol (Bio-Rad) and PCR experiments with specific primers, described in Table 1, were performed for the different enterococcal species (Arias et al. 2006; Dutka-Malen et al. 1995).
Antimicrobial susceptibility testing
Susceptibility for 11 antibiotics (vancomycin, 30 μg; teicoplanin, 30 μg; ampicillin, 10 μg; streptomycin, 300 μg; gentamycin, 120 μg; kanamycin, 120 μg; chloramphenicol, 30 μg; tetracycline, 30 μg; erythromycin, 15 μg; quinupristin/dalfopristin, 15 μg; and ciprofloxacin, 5 μg), were tested by the disk diffusion method (C.L.S.I. 2010). High-level aminoglycosides resistance was considered to streptomycin, kanamycin and gentamycin. Minimal inhibitory concentrations (MICs) of vancomycin and teicoplanin were also determined by the agar dilution method (C.L.S.I. 2010). Enterococcus faecalis ATCC 29212 and Staphylococcus aureus ATCC 25923 strains were used as a control.
PCR detection of antibiotic resistance genes
Vancomycin resistance mechanisms (vanA, vanB, vanC-1, vanC-2/3, and vanD genes) were analyzed by PCR in all enterococcal isolates that showed resistance or reduced susceptibility for glycopeptides (Dutka-Malen et al. 1995; Miele et al. 1995). The presence of genes encoding resistance to erythromycin [erm(A) and erm(B)], tetracycline [tet(M), tet(L) and tet(K)], kanamycin [aph(3’)-IIIa], streptomycin [ant(6)-Ia], quinupristin-dafopristin [vat(E) and vat(D)], chloramphenicol [cat(A)], and gentamycin [aac(6’)-aph(2”)] were analyzed by PCR using primers (Table 1) and conditions previously reported (del Campo et al. 2000; Aarestrup et al. 2000; Robredo et al. 2000; Van de klundert and Vliegenthart 1993; Sutcliffe et al. 1996). PCR-assays were used to demonstrate the presence of specific genes of the Tn5397-like and Tn916/Tn1545-like transposons (tdnX and int genes, respectively) (Agerso et al. 2006). Positive and negative controls from the collection of strains from the University of Trás-os-Montes and Alto Douro (Portugal) were included in all PCR assays.
Results and discussion
A total of 194 enterococcal isolates were recovered from the 198 fecal samples of pigs, cattle and sheep analyzed in this study. No enterococcal isolates were recovered from 4 of the tested fecal samples. Table 2 shows the distribution of enterococcal species found in the samples of different origin. Enterococcus faecium (45.7%) was the prevalent species detected in pigs, while in cattle and sheep this enterococcal species was the second most detected and was found in similar percentages (29.4 and 26%, respectively). E. hirae was the most detected in cattle and sheep (56.8 and 58.9%, respectively). E. faecium and E. hirae were also the predominant enterococcal species isolated from cattle and/or pigs by others (Jackson et al. 2011; Kuhn et al. 2003; Anderson et al. 2008; Poeta et al. 2007). The prevalence of E. faecalis in pigs, cattle and sheep was identical (12.9, 11.8 and 8.2%, respectively); higher prevalence of E. faecalis has been detected in food-producing animals by others (Cortes et al. 2006; Aarestrup et al. 2000). E. durans was only detected in cattle (2%) and sheep (4.2%), and E. casseliflavus only in sheep (2.7%).
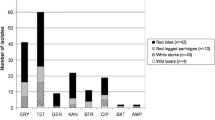
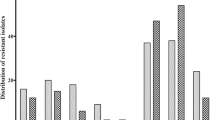
Table 3 shows the percentage of antibiotic resistances in our collection of enterococcal isolates. Higher percentages of resistance were detected for tetracycline and erythromycin in pig isolates (95.7 and 84.3%, respectively) compared with sheep isolates (76.7 and 17.3%, respectively); lower percentages of resistance to these antibiotics were obtained in cattle isolates (49 and 15.7%, respectively). Tetracycline has been the most commonly used antimicrobial agent for therapy in food-production animals in Portugal, and the frequent occurrence of resistance observed probably reflects this use. Similar percentages of tetracycline and erythromycin resistance were detected in the three enterococcal species isolated in pigs (82–100%); in sheep, resistance to these antibiotics was higher among E. faecium species (78.9 and 36.8%, respectively), while in cattle, E. hirae isolates showed higher tetracycline resistance (62.1%) compared to other enterococcal species.
Glycopeptide resistance was not detected among the enterococci isolates of this study. Nevertheless, vanA enterococci were recovered from fecal samples of pigs and sheep in a previous study carried out by our group using vancomycin-supplemented agar plates (4 μg/mL) for enterococci isolation in these fecal samples (unpublished observations). This fact could indicate that vancomycin-resistant enterococci could be present within the fecal enterococcal population of pigs and sheep but in a low proportion with respect to the vancomycin-susceptible ones, and thus could not be detected when non-supplemented plates were used for bacterial isolation.
Ampicillin-resistant isolates were not found in cattle fecal samples; the same result was obtained by Anderson et al. (2008). Ampicillin resistance was only observed among E. hirae and E. faecium isolates of pigs and sheep (pigs, 13.8 and 43.8%, respectively; sheep, 2.3 and 15.8%, respectively). Our results are in accordance with those obtained by Butaye et al. (2001) that detected ampicillin resistance among E. faecium, but not in E. faecalis, of pig origin. In sheep, ampicillin resistance detected was only 5.5%, but others had no ampicillin resistance among sheep (de Fatima Silva Lopes et al. 2005; Mannu et al. 2003)
Lower percentages of high-level resistance for gentamycin (HLR-G) were detected in our enterococci from pigs and cattle (7.1 and 5.9%, respectively), but all our sheep isolates were susceptible for HLR-G. Similar percentages of HLR-G were observed by others in pigs and cattle (Aarestrup et al. 2000, 2002; Hershberger et al. 2005). Higher percentages were found for high-level resistance for kanamycin (HLR-K) and high-level resistance for streptomycin (HLR-S), especially in the isolates recovered from pigs (32.9 and 44.3%, respectively). In cattle and sheep isolates, HLR-K and HLR-S detected were lower (5.9–13.7%). In pigs, HLR-K and HLR-S were more associated with E. faecalis, while in sheep, this type of resistance was more associated with E. faecium. HLR-K and HLR-S were also detected by others in food-producing animals (Butaye et al. 2001; Aarestrup et al. 2002; Poeta et al. 2006).
Similar percentages of quinupristin/dalfopristin resistance were observed in isolates from pigs, cattle and sheep (23.5–15.1%). Other reports showed a higher level of quinupristin-dalfopristin resistance in enterococci from pigs and lower levels of resistance in beef cattle isolates (Aarestrup et al. 2000; Donabedian et al. 2006; Hershberger et al. 2005).
Chloramphenicol resistance was not detected among our enterococcal isolates from sheep, and low percentages of resistance were observed in pig and cattle isolates (1.4 and 3.9%, respectively). Although chloramphenicol has been used in the past in food-producing animals, it was banned more than 20 years ago and this fact could explain the low chloramphenicol resistance detected among our isolates (Poeta et al. 2006). Only E. faecalis from pigs (44.4%) and E. faecium from pigs and sheep (9.4 and 21%, respectively) presented ciprofloxacin resistance. Among our cattle isolates, no ciprofloxacin resistance was detected, but resistance to this antibiotic has been detected in cattle by others (Anderson et al. 2008; Hershberger et al. 2005). Ciprofloxacin resistance of 21% in sheep isolates is higher than that obtained by de Fatima Silva Lopes et al. (2005), were only a few dairy isolates showed ciprofloxacin resistance.
Table 4 shows the different antibiotic resistance phenotypes detected in the series of 194 enterococci in relation to the species and origin. The enterococcal species (E. hirae, E. faecium, and E. faecalis) isolated from different origins show resistance to 4 or 5 antibiotic groups at the same time. Resistance to erythromycin and tetracycline was commonly observed alone, especially among E. hirae and E. faecium isolates, whereas resistance to quinupristin/dalfopristin, aminoglycosides or ampicillin were observed mainly in combination with resistance to other antimicrobial agents. In human medicine, enterococcal infections are often treated with a combination of these antibiotics (Hammerum et al. 2010), and the fact that our isolates showed resistance to them can be a cause of concern since successful therapy for infection may be impossible.
The only two E. casseliflavus detected, recovered from sheep, were susceptible to all tested antibiotics. E. casseliflavus is often associated with water and plants, and a constant supply of plant-associated E. casseliflavus, by grazing, can explain their presence in sheep intestinal tracts (Muller et al. 2001).
The presence of antibiotic resistance genes was studied by PCR in all resistant enterococci and the results are presented in Table 5. The catA gene, encoding a chloramphenicol acetyl-transferase, was found in all but one E. faecium isolate recovered from cattle; this gene has been previously detected in chloramphenicol-resistant enterococci of different origins by other authors (Aarestrup et al. 2000; Poeta et al. 2006).
Enterococci can show high level resistance to aminoglycosides, generally due to the acquisition of genes encoding for aminoglycoside modifying enzymes. Enterococci which contain the aac(6’)-aph(2”) gene that encodes the bifunctional enzyme AAC(6’)-APH(2”) are resistant to virtually all the clinically available aminoglycosides, including gentamycin, tobramycin, amikacin, kanamycin, and netilmicin, but not streptomycin (Chow 2000). All our enterococcal isolates that show HLR-G contained the aac(6’)-aph(2”) gene; this gene has been found as a common mechanism of HLR-G in enterococci (Jackson et al. 2010; del Campo et al. 2003; Aarestrup et al. 2002). The ant(6)-Ia gene responsible for high-level streptomycin resistance was detected in most of our streptomycin-resistant isolates. The same gene has been reported among HLR-S enterococci from animals and humans (del Campo et al. 2000; Poeta et al. 2006).
The aph(3’)-IIIa gene encodes the aminoglycoside phosphotransferase Aph(30)-IIIa, which confers high-level kanamycin resistance; this gene was detected in almost all our resistant isolates, and other studies report this gene as the most frequent in animals (Jackson et al. 2010; Aarestrup et al. 2002; Poeta et al. 2006). In four of our HLR-K isolates, the aph(3’)-IIIa gene was not detected, but other mechanisms can be implicated. Two of this isolates were HLR-G and harbored the aac(6’)-aph(2”) gene, also implicated in HLR-K. Other studies referred that these two genes, aph(3’)-IIIa and aac(6’)-aph(2”), alone or associated, were responsible for HLR-K (del Campo et al. 2003).
The erm(B) gene was the only one found among the erythromycin-resistant enterococci. Others reports refer to the erm(B) has the most frequently resistant gene found among the erythromycin-resistant enterococci (Poeta et al. 2006; Donabedian et al. 2006; Aarestrup et al. 2002).
It is assumed that virginiamycin, a streptogramin compound, used in animal feed as a growth promoter, is responsible for quinupristin-dalfopristin resistance in animals (Aarestrup et al. 2000; Donabedian et al. 2006). In our results, none of the genes, vat(D) or vat(E), mediating quinupristin/dalfopristin resistance were observed (Table 4). The same results were obtained in other studies (Donabedian et al. 2006; Poeta et al. 2005), and most likely different mechanisms of resistance could be involved in those quinupristin/dalfopristin-resistant strains where no genes were detected (Poeta et al. 2006; Donabedian et al. 2006; Jackson et al. 2007).
The tet(M) or tet(L) genes (alone or associated) were demonstrated in all our E. hirae and E. faecium pig isolates; but in cattle and sheep isolates, these two genes were not detected among any tetracycline-resistant E. hirae and E. faecium. However, Anderson et al. (2008) reported the tet(O) gene as the most frequently associated with tetracycline resistance in cattle. The majority (75%) of the tetracycline-resistant E. faecalis isolates from pigs harbored the tet(M) gene alone or in association with the tet(L) gene. All the E. faecalis and E. durans isolates from sheep harbored the tet(M) and the tet(L) genes in association, and the same association was detected in all but one E. faecalis isolate from cattle. In tetracycline resistance, the tet(M) gene is implicated in ribosomal protection and tet(L) encodes an efflux pump; as reported by others, these two genes are the most frequently detected among tetracycline-resistant isolates in animals (Poeta et al. 2005, 2006; Aarestrup et al. 2000).
The Tn916/Tn154-like transposons were associated with the tet(M) gene in 30.8% of the isolates. The Tn5397-like transposon alone was detected in 11.2% of the isolates, mainly among E. hirae and E. faecium from pigs and cattle, and in all E. durans from sheep. Rizzotti et al. (2009) also detected the association between the tet(M) gene and Tn916/Tn154-like transposons in enterococci isolated from a total food chain. They concluded that Enterococcus species can be an important source of antibiotic resistance genes for potentially pathogenic bacteria occurring in the food chain through the transfer of mobile genetic elements, such as transposons (Rizzotti et al. 2009).
The association between the tet(M) gene and the two studied transposons (Tn916/Tn154-like and Tn5397-like) at the same time was detected in 7 of our isolates; this association has also been detected by others (Agerso et al. 2006).
Conclusion
Enterococci are ubiquitous bacteria and are frequently associated with mobile genetic elements, which make them the ideal reservoir for antibiotic resistance genes that can be transferred between different environments and bacterial species.
Food-borne diseases often follow the consumption of contaminated food-stuffs especially from animal products such as meat. Carcasses can be contaminated with pathogenic bacteria, and the majority of these bacteria result from fecal contamination occurring during the slaughtering process. Our study shows that the presence of enterococci resistant to different antibiotics groups and carrying antibiotic resistance genes can be frequent among animals slaughtered for human consumption. These genes are similar to those found in enterococci of human origin indicating the possible circulation of bacteria and resistance genes between the animal and human ecosystem.
These facts and the detection of mobile genetic elements (Tn916/Tn154-like and Tn5397-like transposons) indicate that enterococci can be a source of antibiotic resistance genes for potentially more pathogenic bacteria occurring in the food chain.
In conclusion, surveillance studies should be continued to follow the evolution of antibiotic resistance in saprophytic bacteria of the intestinal tract of animals in order to assess the potential risk for human health of these resistant bacteria.
References
Aarestrup FM, Agerso Y, Gerner-Smidt P, Madsen M, Jensen LB (2000) Comparison of antimicrobial resistance phenotypes and resistance genes in Enterococcus faecalis and Enterococcus faecium from humans in the community, broilers, and pigs in Denmark. Diagn Microbiol Infect Dis 37(2):127–137
Aarestrup FM, Hasman H, Jensen LB, Moreno M, Herrero IA, Dominguez L, Finn M, Franklin A (2002) Antimicrobial resistance among enterococci from pigs in three European countries. Appl Environ Microbiol 68(8):4127–4129
Agerso Y, Pedersen AG, Aarestrup FM (2006) Identification of Tn5397-like and Tn916-like transposons and diversity of the tetracycline resistance gene tet(M) in enterococci from humans, pigs and poultry. J Antimicrob Chemother 57(5):832–839. doi:10.1093/jac/dkl069
Anderson JF, Parrish TD, Akhtar M, Zurek L, Hirt H (2008) Antibiotic resistance of enterococci in American bison (Bison bison) from a nature preserve compared to that of Enterococci in pastured cattle. Appl Environ Microbiol 74(6):1726–1730. doi:10.1128/AEM.02164-07
Araujo C, Torres C, Silva N, Carneiro C, Goncalves A, Radhouani H, Correia S, da Costa PM, Paccheco R, Zarazaga M, Ruiz-Larrea F, Poeta P, Igrejas G (2010) Vancomycin-resistant enterococci from Portuguese wastewater treatment plants. J Basic Microbiol. doi:10.1002/jobm.201000102
Arias CA, Robredo B, Singh KV, Torres C, Panesso D, Murray BE (2006) Rapid identification of Enterococcus hirae and Enterococcus durans by PCR and detection of a homologue of the E. hirae mur-2 Gene in E. durans. J Clin Microbiol 44(4):1567–1570. doi:10.1128/JCM.44.4.1567-1570.2006
Butaye P, Devriese LA, Haesebrouck F (2001) Differences in antibiotic resistance patterns of Enterococcus faecalis and Enterococcus faecium strains isolated from farm and pet animals. Antimicrob Agents Chemother 45(5):1374–1378. doi:10.1128/AAC.45.5.1374-1378.2001
C.L.S.I. (2010) Performance standards for antimicrobial susceptibility testing 17th edn. Information supplement M100-S17. CLSI, Wayne, PA, USA
Cetinkaya Y, Falk P, Mayhall CG (2000) Vancomycin-resistant enterococci. Clin Microbiol Rev 13(4):686–707
Chow JW (2000) Aminoglycoside resistance in enterococci. Clin Infect Dis 31(2):586–589. doi:10.1086/313949
Cortes C, De la Fuente R, Contreras A, Sanchez A, Corrales JC, Ruiz-Santa-Quiteria JA, Orden JA (2006) Occurrence and preliminary study of antimicrobial resistance of enterococci isolated from dairy goats in Spain. Int J Food Microbiol 110(1):100–103. doi:10.1016/j.ijfoodmicro.2006.01.033
Costa L, Radhouani H, Gomes C, Igrejas G, Poeta P (2010) High Prevalence of Extended-Spectrm beta-lactamases Escherichia coli and vancomycin-resistant enterococci isolates from chicken products. A problem of public health. J Food Safety 30(1):141–153. doi:10.1111/j.1745-4565.2009.00195.x
de Fatima Silva Lopes M, Ribeiro T, Abrantes M, Figueiredo Marques JJ, Tenreiro R, Crespo MT (2005) Antimicrobial resistance profiles of dairy and clinical isolates and type strains of enterococci. Int J Food Microbiol 103(2):191–198. doi:10.1016/j.ijfoodmicro.2004.12.025
del Campo R, Ruiz-Garbajosa P, Sanchez-Moreno MP, Baquero F, Torres C, Canton R, Coque TM (2003) Antimicrobial resistance in recent fecal enterococci from healthy volunteers and food handlers in Spain: genes and phenotypes. Microb Drug Resist 9(1):47–60. doi:10.1089/107662903764736346
del Campo R, Tenorio C, Rubio C, Castillo J, Torres C, Gomez-Lus R (2000) Aminoglycoside-modifying enzymes in high-level streptomycin and gentamicin resistant Enterococcus spp. in Spain. Int J Antimicrob Agents 15(3):221–226
Donabedian SM, Perri MB, Vager D, Hershberger E, Malani P, Simjee S, Chow J, Vergis EN, Muder RR, Gay K, Angulo FJ, Bartlett P, Zervos MJ (2006) Quinupristin-dalfopristin resistance in Enterococcus faecium isolates from humans, farm animals, and grocery store meat in the United States. J Clin Microbiol 44(9):3361–3365. doi:10.1128/JCM.02412-05
Dutka-Malen S, Evers S, Courvalin P (1995) Detection of glycopeptide resistance genotypes and identification to the species level of clinically relevant enterococci by PCR. J Clin Microbiol 33(1):24–27
Figueiredo N, Radhouani H, Goncalves A, Rodrigues J, Carvalho C, Igrejas G, Poeta P (2009) Genetic characterization of vancomycin-resistant enterococci isolates from wild rabbits. J Basic Microbiol 49(5):491–494. doi:10.1002/jobm.200800387
Freitas AR, Novais C, Ruiz-Garbajosa P, Coque TM, Peixe L (2009) Dispersion of multidrug-resistant Enterococcus faecium isolates belonging to major clonal complexes in different Portuguese settings. Appl Environ Microbiol 75(14):4904–4908. doi:10.1128/AEM.02945-08
Goncalves A, Poeta P, Silva N, Araujo C, Lopez M, Ruiz E, Uliyakina I, Direitinho J, Igrejas G, Torres C (2010) Characterization of vancomycin-resistant enterococci isolated from fecal samples of ostriches by molecular methods. Foodborne Pathog Dis 7(9):1133–1136. doi:10.1089/fpd.2010.0548
Hammerum AM, Lester CH, Heuer OE (2010) Antimicrobial-resistant enterococci in animals and meat: a human health hazard? Foodborne Pathog Dis 7(10):1137–1146. doi:10.1089/fpd.2010.0552
Hayes JR, English LL, Carter PJ, Proescholdt T, Lee KY, Wagner DD, White DG (2003) Prevalence and antimicrobial resistance of enterococcus species isolated from retail meats. Appl Environ Microbiol 69(12):7153–7160
Hershberger E, Oprea SF, Donabedian SM, Perri M, Bozigar P, Bartlett P, Zervos MJ (2005) Epidemiology of antimicrobial resistance in enterococci of animal origin. J Antimicrob Chemother 55(1):127–130. doi:10.1093/jac/dkh508
Jackson CR, Fedorka-Cray PJ, Barrett JB, Hiott LM, Woodley TA (2007) Prevalence of streptogramin resistance in enterococci from animals: identification of vatD from animal sources in the USA. Int J Antimicrob Agents 30(1):60–66. doi:10.1016/j.ijantimicag.2007.03.010
Jackson CR, Fedorka-Cray PJ, Davis JA, Barrett JB, Brousse JH, Gustafson J, Kucher M (2010) Mechanisms of antimicrobial resistance and genetic relatedness among enterococci isolated from dogs and cats in the United States. J Appl Microbiol 108(6):2171–2179. doi:10.1111/j.1365-2672.2009.04619.x
Jackson CR, Lombard JE, Dargatz DA, Fedorka-Cray PJ (2011) Prevalence, species distribution and antimicrobial resistance of enterococci isolated from US dairy cattle. Lett Appl Microbiol 52(1):41–48. doi:10.1111/j.1472-765X.2010.02964.x
Kuhn I, Iversen A, Burman LG, Olsson-Liljequist B, Franklin A, Finn M, Aarestrup F, Seyfarth AM, Blanch AR, Vilanova X, Taylor H, Caplin J, Moreno MA, Dominguez L, Herrero IA, Mollby R (2003) Comparison of enterococcal populations in animals, humans, and the environment–a European study. Int J Food Microbiol 88(2–3):133–145
Kuhn I, Iversen A, Finn M, Greko C, Burman LG, Blanch AR, Vilanova X, Manero A, Taylor H, Caplin J, Dominguez L, Herrero IA, Moreno MA, Mollby R (2005) Occurrence and relatedness of vancomycin-resistant enterococci in animals, humans, and the environment in different European regions. Appl Environ Microbiol 71(9):5383–5390. doi:10.1128/AEM.71.9.5383-5390.2005
Macedo AS, Freitas AR, Abreu C, Machado E, Peixe L, Sousa JC, Novais C (2011) Characterization of antibiotic resistant enterococci isolated from untreated waters for human consumption in Portugal. Int J Food Microbiol 145(1):315–319. doi:10.1016/j.ijfoodmicro.2010.11.024
Mannu L, Paba A, Daga E, Comunian R, Zanetti S, Dupre I, Sechi LA (2003) Comparison of the incidence of virulence determinants and antibiotic resistance between Enterococcus faecium strains of dairy, animal and clinical origin. Int J Food Microbiol 88(2–3):291–304
Miele A, Bandera M, Goldstein BP (1995) Use of primers selective for vancomycin resistance genes to determine van genotype in enterococci and to study gene organization in VanA isolates. Antimicrob Agents Chemother 39(8):1772–1778
Muller T, Ulrich A, Ott EM, Muller M (2001) Identification of plant-associated enterococci. J Appl Microbiol 91(2):268–278
Novais C, Coque TM, Costa MJ, Sousa JC, Baquero F, Peixe LV (2005) High occurrence and persistence of antibiotic-resistant enterococci in poultry food samples in Portugal. J Antimicrob Chemother 56(6):1139–1143. doi:10.1093/jac/dki360
Poeta P, Costa D, Igrejas G, Rodrigues J, Torres C (2007) Phenotypic and genotypic characterization of antimicrobial resistance in faecal enterococci from wild boars (Sus scrofa). Vet Microbiol 125(3–4):368–374. doi:10.1016/j.vetmic.2007.06.003
Poeta P, Costa D, Rodrigues J, Torres C (2006) Antimicrobial resistance and the mechanisms implicated in faecal enterococci from healthy humans, poultry and pets in Portugal. Int J Antimicrob Agents 27(2):131–137. doi:10.1016/j.ijantimicag.2005.09.018
Poeta P, Costa D, Saenz Y, Klibi N, Ruiz-Larrea F, Rodrigues J, Torres C (2005) Characterization of antibiotic resistance genes and virulence factors in faecal enterococci of wild animals in Portugal. J Vet Med B Infect Dis Vet Public Health 52(9):396–402. doi:10.1111/j.1439-0450.2005.00881.x
Rizzotti L, La Gioia F, Dellaglio F, Torriani S (2009) Molecular diversity and transferability of the tetracycline resistance gene tet(M), carried on Tn916-1545 family transposons, in enterococci from a total food chain. Antonie Van Leeuwenhoek 96(1):43–52. doi:10.1007/s10482-009-9334-7
Robredo B, Singh KV, Torres C, Murray BE (2000) Streptogramin resistance and shared pulsed-field gel electrophoresis patterns in vanA-containing Enterococcus faecium and Enterococcus hirae isolated from humans and animals in Spain. Microb Drug Resist 6(4):305–311
Sutcliffe J, Grebe T, Tait-Kamradt A, Wondrack L (1996) Detection of erythromycin-resistant determinants by PCR. Antimicrob Agents Chemother 40(11):2562–2566
Torres C, Tenorio C, Portillo A, Garcia M, Martinez C, Del Campo R, Ruiz-Larrea F, Zarazaga M (2003) Intestinal colonization by vanA- or vanB2-containing enterococcal isolates of healthy animals in Spain. Microb Drug Resist 9(Suppl 1):S47–52. doi:10.1089/107662903322541892
Van de klundert JAM, Vliegenthart JS (1993) PCR detection of genes for aminoglycosides-modifying enzymes. In: Persing DH, Smith TF, Tenover FC, White TJ (eds) Diagnostic molecular microbiology. Principles and applications. American Society for Microbiology, Washington, pp 547–552
Acknowledgment
Sónia Ramos was supported by a grant (reference SFRH / BD / 47706/ 2008) from Fundação para a Ciência e a Tecnologia (FCT), Portugal.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ramos, S., Igrejas, G., Capelo-Martinez, JL. et al. Antibiotic resistance and mechanisms implicated in fecal enterococci recovered from pigs, cattle and sheep in a Portuguese slaughterhouse. Ann Microbiol 62, 1485–1494 (2012). https://doi.org/10.1007/s13213-011-0402-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13213-011-0402-7