Abstract
Mefloquine was retrieved as a glucagon -like peptide-1 receptor agonist and, therefore, evaluated for its antidiabetic potential against non-insulin-dependent diabetes mellitus (NIDDM) in experimental animals. NIDDM was induced by single intraperitoneal injection of streptozotocin and nicotinamide (60 + 110 mg/kg) in albino wistar rats. The experimental animals were scrutinised for electrocardiographic (ECG) and heart rate variability (HRV) factors to study the autonomic dysfunction along with blood glucose, serum insulin, and liver glycogen levels for glycemic control. Simultaneously, antioxidant markers (TBARs, protein carbonyl, GSH, SOD, catalase) and inflammatory markers (COX, LOX, NO) were scrutinized as well. Oral administration of mefloquine normalised the heart rate with favourable regulation of time and frequency domain HRV parameters. Mefloquine restored the blood glucose, serum insulin, and liver glycogen levels favourably in diabetic rats. Treatment with mefloquine curtailed the antioxidant markers with favourable regulation of inflammatory signals. Mefloquine was also found to be less hepatotoxic in contrast to the standard metformin, providing an integrated advantage as an antidiabetic agent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The glucagon-like peptide-1 receptor (GLP-1R) gene resides on chromosome 6 and the protein encoding for this gene is a glucagon receptor family of G protein-coupled receptor (Dillon et al. 1993). The GLP-1R has an explicit binding affinity for GLP-1 and glucagon with the noteworthy appearance in pancreatic β cells (Hölscher 2014). The activation of GLP-1R leads to stimulation of adenyl cyclase (AC) pathway, which subsequently catalyses the conversion of adenosine tri-phosphate (ATP) to 3,5-cyclic AMP (cAMP). The cAMP appears as a regulatory signal via specific cAMP binding protein/transcription factor/enzyme (kinase) (Idevall-Hagren et al. 2010). GLP-1R can distress the glucose homeostasis in manifold ways; primarily, GLP-1 can facilitate the Ca2+-dependent exocytosis of insulin through cAMP-dependent pathway intervened by protein kinase A (PKA), which phosphorylates the secretory granule-associated protein (Nakazaki et al. 2002). Moreover, GLP-1 can also modulate the cAMP-regulated guanine nucleotide exchange factor which subsequently promotes phosphatidyl inositol 4,5-bisphosphate (PIP2) hydrolysis and intracellular Ca2+ ion mobilisation (Seino and Shibasaki 2005; Garber 2011).
All in all, this research has demonstrated GLP-1 as an insulin secretagogue and in the same line class of drug has been developed called GLP-1R agonist/incretin mimetics. Recently, GLP-1R agonists are most prominently used for the treatment of type-2 diabetes due to low risk of hypoglycaemia in comparison with sulfonylureas and meglitinides (Sivertsen et al. 2012). However, currently GLP-1R agonist (e.g. exenatide, liraglutide) have been reported to have adverse effects such as increase in heart rate (HR), renal impairment/renal failure, acute pancreatitis, and trophic effect upon the pancreatic duct cells (Bjerre Knudsen et al. 2010; Elashoff et al. 2011). Recently, FDA has also approved the revision to the drug label for exenatide to include information on post-marketing reports on acute renal failure and renal insufficiency.
In view of the pharmacological importance of GLP-1R in glycemic control and their upcoming toxicities, it was considered to be the need of the hour to enumerate agonists for GLP-1R which is safer than currently accessible choices. Henceforth, liraglutide (GLP-1R agonist) was selected and drugs with 50% chemical structure similarity were retrieved from the drug data bank. A total of 73 drug molecules were retrieved, who were further evaluated for their GLP-1R (PDB-ID-3IOL) binding efficacy using the virtual tool (Autodock 4.2).
Visualising the binding energies and number of hydrogen bond formation along with the binding partners, authors considered mefloquine to be a prospective target for GLP-1R. Consequently, mefloquine was evaluated for its antidiabetic potential against streptozotocin (STZ)- and nicotinamide (NA)-induced diabetes in albino wistar rats.
Materials and methods
Virtual screening and molecular docking studies
Total 73 compounds were retrieved from drug bank (http://www.drugbank.com) with 50% chemical structurally similarity criteria with liraglutide (GLP-1 agonist). Among the 73 drugs, 62 molecules have already been reported for their antidiabetic potential by various research groups. Subsequently, remaining seven compounds (mefloquine, zolmitriptan, frovatriptan, carfilzomib, pergolide, tigecycline, trandolapril) were evaluated for their in silico binding energy for GLP-1R (PDB-ID-3IOL) using Autodock 4.2. Mefloquine was observed to have binding energy (− 4.3 kcal) binds with GLP-1R (Fig. 1). Considering the binding affinity, binding partners, and binding orientation, authors considered mefloquine as a candidate molecule for further evaluation of its antidiabetic potential.
Animals
Albino wistar rats (100–150 g) were obtained from the central animal house. The animals were housed under the standard condition of temperature (25 ± 1 °C) with 12 h light/dark cycle and had free access to commercial pellet diet and water ad libitum. The animals were given a week time to get acclimatised within the laboratory condition. All experiments were performed according to the Committee for the purpose of control and supervision of Experiments on Animals (CPCSEA) guidelines for laboratory animals and ethics, Department of animal welfare, Government of India (approval no. SDCOP&VS/AH/CPCSEA/01/0033).
Drugs and chemicals
Streptozotocin (STZ) (Catalogue No. 18883-66-4) and nicotinamide (NA) (Catalogue No. 98-92-0) were purchased from Himedia Laboratories Private Ltd, Mumbai, India. All other chemicals were of analytical grade and procured from Loba Chemie, Mumbai, India, else otherwise stated in the text. The chemical structure and chemical formula of mefloquine are given below:

Induction of non-insulin-dependent diabetes mellitus (NIDDM)
NIDDM was induced in the overnight fasted experimental animals (100–150 gm) by a single intraperitoneal (i.p.) injection of STZ + NA (60 + 110 mg/kg, i. p.). NA was administered 15 min before STZ administration. STZ and NA were dissolved in 0.1 M citrate buffer (pH 4.5) and normal saline, respectively. Diabetes was confirmed in STZ + NA-treated rats by measuring the fasting blood glucose concentration 96 h after the injection of STZ + NA (Masiello et al. 1998).
The rats with fasting blood glucose level (BGL) between 200 and 450 mg/dl were considered for inclusion in the experiments. The animals were randomised and divided into five groups of six animals each and subjected to the treatment for 12 days (Table 1). The animals were scrutinised for the paradigms of electrocardiograph (ECG) and heart rate variability (HRV) on the 11th day. Blood samples were collected in pre-heparinised tubes under light ether anaesthesia and a portion of the same was immediately processed for blood glucose estimation. Remaining blood samples were centrifuged at 8161g for 15 min to collect serum. The serum samples were stored at − 20 °C till further use. The animals were sacrificed by cervical dislocation under light ether anaesthesia. Pancreatic and liver tissues were collected for further biochemical estimation.
Hemodynamic evaluations
The animals were anaesthetised using ketamine hydrochloride (50 mg/kg, i.m.) and diazepam (2.5 mg/kg, i.m.) combination and subsequently mounted on a wax tray. The platinum hook electrodes were placed on the skin of the dorsal and ventral thorax to record the ECG signals. The electrodes were connected to Bioamplifier (ML-106) and two-channel power lab (ML826) to convert analogue to digital signals (AD Instruments, Australia). The ECG signals were saved on the hard-disc and analysed offline using Lab chart Pro-8 (AD Instruments, Australia).
HRV analysis was conducted on multiple segments of continuous ECG signals perceived in the preceding paragraph. First, all the raw signals were inspected manually to ensure that all the R waves are detected correctly. Subsequently, HR was calculated by plotting the number of R waves per unit time. Following the same, time and frequency domain parameters of HRV were calculated using the Lab Chart Pro-8 (AD Instruments, Australia).
Blood glucose estimation
Blood glucose level was estimated by one touch select glucometer (Johnson and Johnson, NJ, USA), on 12th day of treatment.
Insulin estimation
Serum insulin level was estimated using Insulin ELISA Kit (catalogue no. INS 4565) (Cal biotech, Austin Drive, Spring Valley, CA).
Nitric oxide estimation
Generation of nitric oxide (NO) in the serum samples was arbitrated by measuring nitrite accumulation, using Griess reagent (1% sulphanilamide, 0.1% N-(1-naphthyl)-ethylenediamine dihydrochloride in 5% H3PO4). The equal quantity of serum and Griess reagent was mixed and incubated at 37 °C for 5 min. The test mixture was subsequently read on UV–Vis spectrophotometer (Cary 60, Agilent Technologies, CA95051, US) at 540 nm using appropriate blank. Sodium nitrite was used to prepare standard curve (Giustarini et al. 2008).
Glycogen estimation
Liver tissue was homogenised in 30% KOH and digested by heating for 20 min in a boiling water bath. The digested sample was diluted with distilled water up to 50 ml. The content of the flask was thoroughly mixed and further diluted to give the glycogen concentration of 3-30 µg/ml. The 5 ml of the final dilution for each sample was used for the evaluation of total liver glycogen using Anthrone method (Carroll et al. 1956).
where U = the optical density of the unknown test solution, S = the optical density of the 100 µg glucose standard, and 1.11 = Factor determined by Morris for the conversion of glucose to glycogen.
Antioxidant markers
A 10% tissue homogenate of the pancreatic tissue was prepared in ice-cold KCL (0.15 M) and centrifuged at 2040g for 15 min at 4 °C. The tissue supernatant was used to study various markers of oxidative stress including thiobarbituric acid reactive substances (TBARs), superoxide dismutase (SOD), catalase (CAT), glutathione (GSH), and protein carbonyl using the methods previously established at our laboratory (Reznick and Packer 1994; Kaithwas et al. 2011; Kaithwas and Majumdar 2012).
Inflammatory markers: cyclooxygenase (COX) and lipoxygenase (LOX) estimations
A 10% pancreatic tissue homogenate in TRIS buffer (50 mM) was centrifuged at 2040g for 5 min followed by sonication. The tissue supernatant (10 µl) was incubated for 5 min with TRIS buffer (160 µl). A 10 µl each of TMPD reagent and arachidonic acid (AA) solution were added and read at 630 nm using multiplate reader (ALERE Microplate Reader, AM-2100) at 0 and 30 s intervals. AA solution was prepared by mixing 50 µl of the AA (40 mM) with 50 µl of 0.1 N potassium hydroxide using vortexing and subsequently 900 µl of double distilled water. TMPD stock solution was prepared by dissolving 0.3 mg of TMPD in 1 ml of distilled water and subsequent 1:10 dilution was prepared for the assay (Riendeau et al. 2001).
For LOX assay, 25 µl of AA solution was added to the 475-µl supernatant (as prepared for COX assay) and incubated for 6 min. A 500 µl of ferrithiocyanate (FTC) reagent was added and read at 480 nm using UV spectrophotometer (Cary 60, Agilent Technologies International Private Limited, CA United States) after 5 min. FTC reagent was prepared by mixing the reagent 1 (4.5 mM FeSO4 in 0.2 M HCl) and reagent 2 (3% NH4SCN methanolic solution) in 1:2 ratio (Lu et al. 2013).
Statistical analysis
All the data are presented as mean ± SD and analysed using one-way ANOVA followed by Bonferroni test for the possible significance identification between the various groups. *p < 0.05, **p < 0.01, ***p < 0.001 was considered statistically significant.
Results
Mefloquine revealed dose-dependent curtailment of blood glucose level with significant regulation of insulin levels (Fig. 2). The amount of liver glycogen was significantly depleted after STZ + NA treatment (54.74 ± 10.22 µg/ml). Concomitantly, mefloquine administration facilitated to restore liver glycogen levels (Fig. 3).
Effect of mefloquine on blood glucose and insulin level. I—Control (Normal saline, 3 ml/kg); II—Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); III—Mefloquine (45 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); IV—Mefloquine (90 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); V—Metformin (25 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg). Values are Mean ± SD), each group contains six animals. Comparisons were made on the basis of the one-way Anova followed by Bonferroni test. All groups were compared to the toxic control group (*p < 0.05, **p < 0.01, ***p < 0.001)
Effect of mefloquine on glycogen level. I—Control (Normal saline, 3 ml/kg); II—Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); III—Mefloquine (45 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); IV—Mefloquine (90 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); V—Metformin (25 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg). Values are Mean ± SD), each group contains six animals. Comparisons were made on the basis of the one-way Anova followed by Bonferroni test. All groups were compared to the toxic control group (*p < 0.05, **p < 0.01, ***p < 0.001)
A noteworthy upsurge in TBARs (103.76 ± 32.46 nmol of MDA/μg of protein) and protein carbonyl (22.81 ± 6.61 nmol/ml unit) level was observed in the pancreatic tissue of STZ–NA-treated animals along with the non-significant upsurge in the levels of GSH (0.57 ± 0.03 µg/mg).
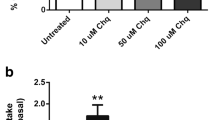
Mefloquine treatment down-regulated the TBARs, protein carbonyl, and GSH levels at low dose. Momentous down-regulation in the enzymatic activity of SOD (1.14 ± 0.14 unit of SOD/µg of protein) and catalase (1.36 ± 0.42 nmol of H2O2/min/µg of protein) was perceived with STZ treatment and same was reinstated towards normal by mefloquine (45 mg/kg) (Table 1). STZ–NA up-regulated the enzymatic activity of COX, which was significantly curtailed down by the mefloquine and metformin treatment. Neither the STZ–NA nor mefloquine could modulate the LOX activity (Fig. 4a). NO levels were markedly diminished after STZ–NA treatment, which was restored towards normal by metformin and mefloquine (Fig. 4b). Furthermore, treatment with metformin and mefloquine increased SGOT and SGPT when compared with STZ–NA-treated rats (Fig. 5).
Effect of mefloquine on inflammatory markers and NO level. I—Control (Normal saline, 3 ml/kg); II—Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); III—Mefloquine (45 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); IV—Mefloquine (90 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); V—Metformin (25 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg). Values are Mean ± SD), each group contains six animals. Comparisons were made on the basis of the one-way Anova followed by Bonferroni test. All groups were compared to the toxic control group (*p < 0.05, **p < 0.01, ***p < 0.001)
Effect of mefloquine on SGOT and SGPT level. I—Control (Normal saline, 3 ml/kg); II—Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); III—Mefloquine (45 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); IV—Mefloquine (90 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); V—Metformin (25 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg). Values are Mean ± SD), each group contains six animals. Comparisons were made on the basis of the one-way Anova followed by Bonferroni test. All groups were compared to the toxic control group (*p < 0.05, **p < 0.01, ***p < 0.001)
STZ–NA treatment demonstrated momentous abnormalities in the ECG profile characterised by QT prolongation (0.062 ± 0.010), QRS prolongation (0.018 ± 0.002), marginal increase in HR (361.9 ± 22.336), and increased dispersion of P wave amplitude (0.072 ± 0.046) in comparison with control (Table 2, Fig. 6).
Effect of mefloquine on ECG tracing. I Control (Normalsaline, 3 ml/kg); II Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); III Mefloquine (45 mg/kg) + Toxicant (STZ, 60 mg/kg + NA, 110 mg/kg); IV Mefloquine (90 mg/kg) + Toxicant (STZ, 60 mg/kg + NA,110 mg/kg); V Metformin (25 mg/kg) + Toxicant (STZ, 60 mg/ kg + NA, 110 mg/kg)
Distorted HRV profile was recorded for the time domain (Average RR, Median RR, SDRR, SDARR, and CVRR) and frequency domain (LF, HF, and LF/HF) parameters after STZ–NA treatment. Treatment with metformin and mefloquine exerted favourable effects towards restoring the HRV paradigms towards normal (Table 3).
Discussion
The study reveals a strong and favourable association between the use of low-dose mefloquine against type-2 diabetes. Hyperglycaemia mostly associated with hypoinsulinemia is the core symptom of type-2 diabetes causing majority of pathological damage evident in the experimental animal consequent to STZ–NA treatment. Mefloquine at the low dose was apparent with momentous regulatory effects towards glycaemic control. Glycogen is a stored form of glucose and is accumulated in response to insulin (Jensen et al. 2011). Experimental diabetes is attributed to deteriorated liver glycogen stores and same was perceived after STZ–NA treatment (Bischof et al. 2002). Mefloquine at low dose exerted substantial upregulation of the liver glycogen. It would be appropriate to mention that high dose of mefloquine and metformin could not perceive any favourable effects on liver glycogen stores rather deteriorated the glycogen levels.
Associated hyperlipidemia and increased risk of cardiovascular complications are the hallmarks of type-2 diabetes in clinical cases. A similar pattern of lipid profile deterioration has been reported after STZ–NA induced diabetes in preclinical models (Shirali et al. 2013). However, treatment with mefloquine (45 mg/kg) regulated the lipid profile favourably. Prima facia, one can commensurate that mefloquine at low dose can impart momentous glycemic and lipidemic control in experimental animals.
Inflammatory signalling in the pathogenesis of type 2 diabetes and associated complications are now well established (Wulffelé et al. 2004). To address the same, authors considered it worth to scrutinize the levels of COX, LOX, and NO. Augmented COX activity in diabetics is a well-settled phenomenon and same was evident in the present experiment as well (Komers et al. 2001). In fact, inflated COX-2 activity has been deliberated to be the consequence of inflammation and essential for the maintenance of vascular tone of the blood vessels in diabetes aroused through the decreased synthesis of NO (Garcia et al. 2014). Both the changes were well evident in the present study, consequent to STZ–NA administration. Metformin and mefloquine were evident for significant favourable regulation over the COX, and NO synthesis, with more marked effect by the low-dose mefloquine. It would be appropriate to remark that neither STZ–NA nor mefloquine could modulate LOX either way. The above observation reflects that mefloquine can also regulate inflammatory pathways associated with diabetes.
Association between ROS inflammation (oxidative stress and inflammation) and diabetes is well established and to inculcate all aspects of the interaction between them, authors considered it worth to evaluate the enzymatic (SOD/catalase/GSH) and per-oxidative (TBARs/protein carbonyl) markers of oxidative stress in pancreatic tissue (Przygodzki et al. 2015). Augmented production of MDA and protein carbonyl is the unchallenged markers for oxidative damage to lipids and proteins, respectively. Authors perceived compelling upsurge in the MDA and protein carbonyl content in the STZ–NA-treated animals, which is in consonance with previous reports (Sharma et al. 2012). Concomitant administration of low-dose mefloquine depreciated the MDA and protein carbonyl levels.
SOD, catalase, and GSH together constitute a major team of defence against ROS-associated oxidative stress. SOD nullifies the superoxide free radicals to produce hydrogen peroxide, which through a subsequent reaction is abolished by catalase to water and molecular oxygen. Both the enzymes work in tandem and decrease in SOD with decrease in catalase is expected, widely reported, and was perceived through the current experiment as well. Treatment with low-dose mefloquine manifested significant upsurge in the SOD and catalase levels. The similar pattern of restoration was available for GSH after the mefloquine treatment (Kaithwas and Majumdar 2012; Gupta et al. 2015).
Prima facia, it appears that low dose of mefloquine can be considered for the management of type-2 diabetes. Nonetheless, to put an affirmative remark and considering the cardiomyopathic complications associated with type-2 diabetes, the author considered it worth to scrutinize the ECG and HRV changes implicated after mefloquine treatment. Cardiovascular autonomic neuropathy is one of the most serious but overlooked complication of diabetes and encompasses damage to the autonomic nerve fibres that innervate the heart and blood vessels (Schumer et al. 1998; Maser et al. 2000). In the present study, we perceived marginal inflation in the HR of the STZ–NA-treated animals, which is in line with the various clinical findings. High level of resting HR in diabetics reflects parasympathetic damage rather a sympathetic deterioration (Ewing et al. 1981; Vinik and Ziegler 2007). It would be appropriate to mention that most of the preclinical reports have opined increase in HR of the STZ-treated animals (Howarth et al. 2005a, b). STZ–NA treatment was also evident for prolongation of QRS, QT, and QTc intervals. QT prolongation is an important manifestation of clinical diabetic cases and is used to screen diabetic patients at risk for sudden cardiac death. QTc represent corrected QT interval, whereas the QRS interval reflects the rapid depolarisation of the right and left ventricle. ECG tracing affirmed the prolongation of QRS, QT, and QTc interval in the diabetic rats. Treatment with mefloquine helped to nudge down the HR, with no effect or marginal curtailment of QRS, QT, and QTc interval (Jia et al. 2009). Elevated R wave amplitude is an independent risk factor for cardiovascular events and represents left ventricular hypertrophy in diabetic patients and same was evident in our study after the STZ–NA treatment (Nakamura et al. 2006). Treatment with mefloquine at high dose helped to push down the R-wave amplitude in comparison with low dose. Increased P wave dispersion and widened PR interval are expected to be associated with obesity and subsequently atrial fibrillation. In the present study, no changes in the P wave dispersion and PR interval was accorded in the diabetic animals and could be accredited to the short duration of the study (Seyfeli et al. 2006; Homoud 2009).
Diabetes as a syndrome creates a sympathetic predominance with corresponding parasympathetic imbalance by denervation of the vagus nerve and decreased HRV is one indicator of diabetic autonomic neuropathy and is a marker for increased mortality risk. In other words, decrease in HRV reflects the impaired cardiac autonomic control and the same was very well evident in the STZ–NA-treated animals. Treatment with mefloquine helped to restore the HRV in the time and frequency domain parameters. Restoration of HRV as scrutinised for mefloquine was better than the standard metformin.
The LF/HF ratio is a widely accepted tool to assess cardiovascular autonomic regulation and presumed that the increases in LF/HF reflect a shift to “sympathetic dominance” and decreases in this index correspond to a “parasympathetic dominance” (Lorsheyd et al. 2005; Vinik and Ziegler 2007). The STZ–NA-treated animals were evident with upregulated LF/HF which was marginally inflated by low-dose mefloquine. On the contrary, high-dose mefloquine was able to regulate the LF/HF more competitively. It would be appropriate to mention that low dose of mefloquine regulated the biochemical markers for hyperglycaemia and high dose was much more effective/comparative while regulating the electrocardiographic and HRV parameters. Accordingly, authors would like comment that the median dose of mefloquine could be a target for future evaluations.
Metformin is one of the most reliable and widely used drugs in the management of diabetes. Notwithstanding long-term use of metformin is often clubbed with severe hepatotoxicity and therefore, it was considered worth to scrutinize the hepatotoxic potential of the mefloquine (Ren et al. 2011). The SGOT and SGPT levels in the metformin-treated groups were significantly high in comparison with the treatments including the test drug. Mefloquine affirmed dose-dependent toxicity associated, which was significantly less than the metformin (Miralles-Linares et al. 2012). It would be appropriate to remark, that long-term use of mefloquine is often associated with serious side effects such as mental health problems. Considering the short duration of our study, it was not well in purview to scrutinize the same. However, during the entire course of study, no neurological abnormality was observed in the experimental animals.
All in all, the present study establishes the efficacy of low-dose mefloquine in diabetics and other associated cardiovascular symptoms ascertained through biochemical, inflammatory and the markers of oxidative stress. Mefloquine was observed to impart noticeable protection against the cardiovascular complications associated with diabetics.
Conclusion
Authors would like to conclude that the antidiabetic effects of mefloquine could be attributed to its GLP-1 agonistic activity. However, the same needs to be cross-checked using more stringent markers. Therefore, mefloquine stands as one of the target for further evaluations.
References
Bischof MG, Bernroider E et al (2002) Hepatic glycogen metabolism in type 1 diabetes after long-term near normoglycemia. Diabetes 51(1):49–54
Bjerre Knudsen L, Madsen LW et al (2010) Glucagon-like peptide-1 receptor agonists activate rodent thyroid C-cells causing calcitonin release and C-cell proliferation. Endocrinology 151(4):1473–1486
Carroll NV, Longley RW et al (1956) The determination of glycogen in liver and muscle by use of anthrone reagent. J Biol Chem 220:583–593
Dillon JS, Tanizawa Y et al (1993) Cloning and functional expression of the human glucagon-like peptide-1 (GLP-1) receptor. Endocrinology 133(4):1907–1910
Elashoff M, Matveyenko AV et al (2011) Pancreatitis, pancreatic, and thyroid cancer with glucagon-like peptide-1—based therapies. Gastroenterology 141(1):150–156
Ewing D, Campbell I et al (1981) Heart rate changes in diabetes mellitus. Lancet 317(8213):183–186
Garber AJ (2011) Long-acting glucagon-like peptide 1 receptor agonists. Diabetes Care 34(Supplement 2):S279–S284
Garcia FAO, Pinto SF et al (2014) Pentoxifylline decreases glycemia levels and TNF-alpha, iNOS and COX-2 expressions in diabetic rat pancreas. Springerplus 3(1):283
Giustarini D, Rossi R et al (2008) Nitrite and nitrate measurement by Griess reagent in human plasma: evaluation of interferences and standardization. Methods Enzymol 440:361–380
Gupta SK, Gautam S et al (2015) Efficacy of variable dosage of aspirin in combating methotrexate-induced intestinal toxicity. RSC Adv 5(13):9354–9360
Hölscher C (2014) Central effects of GLP-1: new opportunities for treatments of neurodegenerative diseases. J Endocrinol 221(1):T31–T41
Homoud MK (2009) ACP journal club: prolonged PR intervals were associated with increased risk for atrial fibrillation, pacemaker implantation, and mortality. Ann Intern Med 151(10):JC5–JC13
Howarth F, Jacobson M et al (2005a) Short-term effects of streptozotocin-induced diabetes on the electrocardiogram, physical activity and body temperature in rats. Exp Physiol 90(2):237–245
Howarth F, Jacobson M et al (2005b) Long-term effects of streptozotocin-induced diabetes on the electrocardiogram, physical activity and body temperature in rats. Exp Physiol 90(6):827–835
Idevall-Hagren O, Barg S et al (2010) cAMP mediators of pulsatile insulin secretion from glucose-stimulated single β-cells. J Biol Chem 285(30):23007–23018
Jensen J, Rustad PI et al (2011) The role of skeletal muscle glycogen breakdown for regulation of insulin sensitivity by exercise. Front Physiol 2:112
Jia J, Zhang X et al (2009) Evaluation of in vivo antioxidant activities of Ganoderma lucidum polysaccharides in STZ-diabetic rats. Food Chem 115(1):32–36
Kaithwas G, Dubey K et al (2011) Effect of aloe vera (Aloe barbadensis Miller) gel on doxorubicin-induced myocardial oxidative stress and calcium overload in albino rats. Indian J Exp Biol 49(4):260–268
Kaithwas G, Majumdar DK (2012) In vitro antioxidant and in vivo antidiabetic, antihyperlipidemic activity of linseed oil against streptozotocin-induced toxicity in albino rats. Eur J Lipid Sci Technol 114(11):1237–1245
Komers R, Lindsley JN et al (2001) Immunohistochemical and functional correlations of renal cyclooxygenase-2 in experimental diabetes. J Clin Investig 107(7):889–898
Lorsheyd A, De Lange D et al (2005) PR and OTc interval prolongation on the electrocardiogram after binge drinking in healthy individuals. Neth J Med 63(2):59–63
Lu W, Zhao X et al (2013) Development of a new colorimetric assay for lipoxygenase activity. Anal Biochem 441(2):162–168
Maser RE, Lenhard JM et al (2000) Cardiovascular autonomic neuropathy: the clinical significance of its determination. Endocrinologist 10(1):27&hyhen
Masiello P, Broca C et al (1998) Experimental NIDDM: development of a new model in adult rats administered streptozotocin and nicotinamide. Diabetes 47(2):224–229
Miralles-Linares F, Puerta-Fernandez S et al (2012) Metformin-induced hepatotoxicity. Diabetes Care 35(3):e21–e21
Nakamura K, Okamura T et al (2006) Electrocardiogram screening for left high R-wave predicts cardiovascular death in a Japanese community-based population: NIPPON DATA90. Hypertens Res 29(5):353
Nakazaki M, Crane A et al (2002) cAMP-activated protein kinase-independent potentiation of insulin secretion by cAMP is impaired in SUR1 null islets. Diabetes 51(12):3440–3449
Przygodzki T, Talar M et al (2015) Inhibition of cyclooxygenase-2 causes a decrease in coronary flow in diabetic mice. The possible role of PGE2 and dysfunctional vasodilation mediated by prostacyclin receptor. J Physiol Biochem 71(3):351–358
Ren L, Fang X et al (2011) T-wave alternans and heart rate variability: a comparison in patients with myocardial infarction with or without diabetes mellitus. Ann Noninvasive Electrocardiol 16(3):232–238
Reznick AZ, Packer L (1994) [38] Oxidative damage to proteins: spectrophotometric method for carbonyl assay. Methods Enzymol 233:357–363
Riendeau D, Percival M et al (2001) Etoricoxib (MK-0663): preclinical profile and comparison with other agents that selectively inhibit cyclooxygenase-2. J Pharmacol Exp Ther 296(2):558–566
Schumer MP, Joyner SA et al (1998) Cardiovascular autonomic neuropathy testing in patients with diabetes. Diabetes Spectrum 11(4):227
Seino S, Shibasaki T (2005) PKA-dependent and PKA-independent pathways for cAMP-regulated exocytosis. Physiol Rev 85(4):1303–1342
Seyfeli E, Duru M et al (2006) Effect of obesity on P-wave dispersion and QT dispersion in women. Int J Obes 30(6):957–961
Sharma A, Kaithwas G et al (2012) Antihyperglycemic and antioxidant potential of polysaccharide fraction from portulaca oleracea seeds against streptozotocin-induced diabetes in rats. J Food Biochem 36(3):378–382
Shirali S, Zahra Bathaie S et al (2013) Effect of crocin on the insulin resistance and lipid profile of streptozotocin-induced diabetic rats. Phytother Res 27(7):1042–1047
Sivertsen J, Rosenmeier J et al (2012) The effect of glucagon-like peptide 1 on cardiovascular risk. Nat Rev Cardiol 9(4):209–222
Vinik AI, Ziegler D (2007) Diabetic cardiovascular autonomic neuropathy. Circulation 115(3):387–397
Wulffelé EM, Kooy A et al (2004) The effect of metformin on blood pressure, plasma cholesterol and triglycerides in type 2 diabetes mellitus: a systematic review. J Intern Med 256(1):1–14
Acknowledgements
Author would like to acknowledge UGC and DST for giving fellowship to RKY, JKR, SG, MS, and SR.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Yadav, R.K., Rawat, J.K., Gautam, S. et al. Antidiabetic activity of mefloquine via GLP-1 receptor modulation against STZ–NA-induced diabetes in albino wistar rats. 3 Biotech 8, 240 (2018). https://doi.org/10.1007/s13205-018-1250-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13205-018-1250-y