Abstract
Malignant germ cell tumors (GCT) of the ovary account for 2–3% of all ovarian neoplasms and occur mostly in the second and third decade of life. Over the past three decades, survival rates for germ cell tumors have dramatically improved, coincident with more aggressive surgical staging and combination chemotherapy. Although there are several studies describing ovarian GCT and fertility-preserving surgery in the western population, there is very little Indian data. We present our experience of germ cell tumor ovary in the Department of Surgical Oncology, King George’s Medical University over the last 5 years with special emphasis on treatment outcome and role of fertility preservation surgery. A retrospective review of medical records of patients with ovarian germ cell tumors, treated at our center from January 2012 to December 2016, was performed. Epidemiological and clinical profile of patients was reviewed. Clinical stage of presentation, neoadjuvant treatment, surgical treatment, and adjuvant treatment data were analyzed, and treatment outcome data was recorded. Patient follow-up was done to ascertain disease-free interval, treatment outcome, ability to conceive following fertility-preserving surgery, and quality of life. A total of 39 patients with ovarian germ cell tumor were treated during this period. Their median age at diagnosis was 22 years (range 11–65 years) and most common mode of presentation was abdominal lump without ascites. Around 36.8% (n = 14) patients had conservative surgery with preservation of opposite ovary and uterus. Most patients (71.1% n = 27) received neoadjuvant chemotherapy due to advanced disease in form of ascites or large mass, and five of these patients were amenable to fertility-preserving surgery after chemotherapy. Nine out of the fourteen patients have had return of menstrual function after a mean period of 3.5 + 0.5 months. One patient who underwent fertility-preserving surgery has delivered healthy children after treatment. Stage distribution for stage I to IV was as follows: 15.4% (n = 6), 35.9% (n = 14), 46.2% (n = 18), and 2.6% (n = 1), respectively. Dysgerminoma was the commonest histology (37.1% n = 13) followed by teratoma (22.9% n = 8). 17.1% (n = 6) patients had recurrence, with a median time to recurrence 16 months (range 5.5 to 37 months) and they were treated with second-line chemotherapy. Germ cell tumor of the ovary is an eminently treatable disease and selected patients can be managed with fertility-preserving surgery. BEP is the most effective chemotherapy regimen. Disease-free survival rates in these patients are quite high and recurrences can be managed with second-line chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignant germ cell tumors (GCT) of the ovary are uncommon neoplasms arising from primitive germ cells of the embryonic gonad. They occur mostly in the second and third decade of life and constitute 2–3% of all ovarian neoplasms [1]. Over the past three decades, survival rates for germ cell tumors have dramatically improved coincident with more aggressive surgical staging and combination therapy [2]. In western literature, the most common histology encountered is teratoma followed by dysgerminoma [2]. There is not much data on GCT from India. In this paper, we aim to analyze our experience of ovarian GCT treatment outcomes in the Department of Surgical Oncology, King George’s Medical University (KGMU), Lucknow, Uttar Pradesh, India, over the last 5 years with special emphasis on long-term follow-up and outcomes of fertility preservation surgery.
Materials and Methods
This is a retrospective study wherein medical records of all patients treated in the Department of Surgical Oncology, KGMU with a diagnosis of malignant germ cell tumor of the ovary between January 2012 and December 2016 were retrieved and analyzed. Epidemiological and clinical profile of patients was reviewed. Clinical stage of presentation and treatment received (neoadjuvant chemotherapy, surgery, and adjuvant treatment) data was analyzed. Patient follow-up was done to ascertain disease-free interval, treatment outcome, and the ability to conceive following fertility-preserving surgery. The data was analyzed using SPSS 21. Statistical significance was tested for categorical data using chi-square test, and the Kaplan Meier survival curves were plotted for disease-free survival and overall survival.
Results
During the 5 years of the retrospective study (2012–2016), 39 patients of malignant GCT ovary were treated in our department. The median age of these patients was 22 years (11–65). 89.7% (n = 35) of these patients were premenopausal while three were postmenopausal and one was premenarche. Most of these patients (76.92% n = 30) were nulliparous. Majority of our patients (82.1%) were diagnosed to have stage II and stage III disease. The stage distribution of patients in our series is listed in Table 1. The most common finding on computerized tomography (CT) was solid cystic ovarian masses with omental nodules and gross ascites. Figure 1 shows the various presentations of malignant GCT on contrast-enhanced CT of the abdomen.
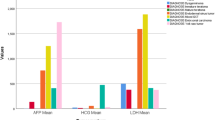
One patient presented with metastatic disease and was treated with palliative chemotherapy. Among the rest (n = 38), majority received neoadjuvant chemotherapy (71.1%, n = 27/38) with weekly bleomycin and bleomycin, etoposide, and cisplatin (BEP) combination three weekly. Grade two or higher toxicity was reported in 30.3% (n = 10/33) patients. Chemotherapy had to be stopped in three patients due to recurrent grade three toxicity. Post-NACT 92.6% (n = 25/27) patients underwent complete cytoreduction. Out of the 38 patients, 11 underwent primary cytoreductive surgery. Table 2 describes the treatment given to these patients. Fertility-preserving surgery was done in 14 patients (36.8%) and nine of these patients (64.3%) had resumption of menstrual function after a mean duration of 3.5 months; however, only one patient was able to conceive. Dysgerminoma was the most common histological type seen followed by teratoma and mixed germ cell tumors (Table 3). Two of our patients were diagnosed with stage I dysgerminoma. No adjuvant chemotherapy was administered and these patients were kept under surveillance. The other nine patients who underwent primary surgery were given adjuvant chemotherapy in view of advanced disease stage. One patient was diagnosed with stage III choriocarcinoma. She had pulmonary metastasis at the time of diagnosis. She was treated initially with single-agent methotrexate but disease progression was observed with rising b-hCG levels. Subsequently, she was treated with a combination of etoposide, methotrexate, actinomycin D, cyclophosphamide, and vincristine (EMA-CO regime). The patient responded well to chemotherapy. Post complete radiological and serological response, chemotherapy was continued for a further 6 weeks. Subsequently, the patient was kept on monthly serum b-hCG level monitoring for 6 months followed by six monthly evaluation. The patient is currently on surveillance with a progression-free survival of 2 years. Patients with dysgerminoma had normal levels of serum AFP and b-hCG; serum LDH was raised in one third patients (5/16). Serum AFP was raised in yolk sac tumors with mean prechemotherapy level of 892.3 ± 182 ng/mL and postchemotherapy level of 2.4 ± 1.3 ng/mL. b-hCG was raised in one patient with choriocarcinoma with a prechemotherapy level of 4452 mIU/ml and posttreatment level of 0.9 mIU/ml. Endodermal sinus tumors and mixed germ cell tumors were commonly associated with elevation of both b-hCG and AFP to varying extent. Mean prechemotherapy level of AFP in these patients was 581.4 ± 139 ng/mL and posttreatment level was 1.1 ± 0.5 ng/mL. The mean prechemotherapy b-hCG level was 1887.9 ± 454 mIU/ml and posttreatment level was 0.45 mIU/ml. The decline in tumor marker level following neoadjuvant therapy correlated well with clinical and radiological response.
Disease-free survival and overall survival were studied and the Kaplan Meier survival curves were plotted (Figs. 2 and 3). There were eight (20.5%) patients with recurrence and seven of these had received neoadjuvant chemotherapy due to advanced disease at presentation. Four of these recurrences were in mixed germ cell tumors, two patients had dysgerminoma, and each one had yolk sac tumor and teratoma. There was no statistically significant correlation of histological type with stage at presentation (p = 0.672), complete cytoreduction (p = 0.386), fertility preservation (p = 0.616), and recurrence (p = 0.408). There was also no significant survival advantage for patients whose fertility was preserved compared to those in whom fertility was not preserved (p = 0.198). The patient with metastatic disease at presentation was treated with palliative chemotherapy (BEP) and expired 9 months after being diagnosed. Of the two patients who had inoperable disease, one underwent secondary cytoreduction after second-line chemotherapy and one was lost to follow-up after 16 months while on second-line chemotherapy (Table 4).
Discussion
Malignant GCT of the ovary forms a minor part of the spectrum of gynecological malignancies, but the fact that they occur mostly in the second and third decade of life when women are entering their reproductive phase makes their clinical impact enormous. Inability to conceive causes women to experience anxiety, depression, poor self-esteem, and feelings of sexual inadequacy [3]. Accumulated evidence regarding the biology of malignant ovarian GCT has led to the understanding that they can be treated effectively with a combination of chemotherapy and conservative surgery. Although patients tend to choose radical surgery due to anxiety regarding a life-threatening disease, it has been proven that radical surgery does not have a survival advantage over conservative surgery in carefully selected patients [4].
In the present study, dysgerminoma was the most common histological subtype followed by teratoma. This is similar to other reports from India [5]. In the USA, there was a different distribution of histological subtypes reported. Smith et al. [2] analyzed surveillance, epidemiology, and end results data of 30 years (1973–2002) and identified 1262 patients of GCT out of which 38.5% were teratomas and 32.8% patients had dysgerminoma. The peak incidence of GCT in their series was in the 15–19 year age group, while in our series, the median age of presentation was 22 years.
A large number of our patients presented with advanced disease usually due to delay in diagnosis due to a variety of reasons. These patients are usually illiterate and come from poor socioeconomic backgrounds. They prefer to first consult alternate systems of medicine when symptoms arise, due to lack of access to modern medicine and fear of cost. Many patients present to us after having undergone laparotomy for removal of ovarian mass with complete or incomplete cytoreduction and no proper documentation. In many instances, the specimen was not even sent for histopathology. Patients were also not properly advised about need for adjuvant chemotherapy and completion surgery. Patients with advanced disease were treated with neoadjuvant chemotherapy for three to four cycles followed by cytoreductive surgery. In most cases, this was a total abdominal hysterectomy with bilateral salphingoophrectomy and omentectomy. In 14 patients, we could do fertility-preserving surgery. Five of these patients had advanced disease initially and were operated following neoadjuvant chemotherapy. There was no evidence of peritoneal disease intraoperatively and the contralateral ovary was grossly normal. BEP chemotherapy is effective for treating germ cell tumors of the ovary and it has been validated in several trials [6,7,8].
There was complete pathological response in 22.2% (n = 6/27) patients receiving neoadjuvant chemotherapy. This is less than the reported 40.7% (22/54) incidence of complete pathological response reported in literature [9]. This is mainly due to poor compliance which in turn can be attributed to two factors; financial issues and toxicity. Patients not adhering to chemotherapy schedule result in inconsistent response to chemotherapy. Figure 4 shows the prechemotherapy and postchemotherapy imaging of a patient who had complete pathological response and successfully underwent fertility-preserving surgery.
One in five of our patients recurred but was managed effectively with second-line chemotherapy regimens like VIP (etoposide, ifosfamide, and cisplatin) and VeIP (vinblastine, ifosfamide, and cisplatin). Patients with early disease and those having a good response to neoadjuvant therapy were treated with conservative surgery wherein the uterus and normal-looking ovary were preserved. Biopsy was not routinely done in all patients due to the risk of mechanical ovarian failure, but thorough palpation of the normal ovary was done and suspicious nodules if any were biopsied and sent for frozen section.
Perrin et al. [10] described 45 patients with fertility preservation out which seven delivered healthy babies. Ezzat et al. [11] described 44 patients out of a total of 67 patients of GCT ovary who underwent fertility-preserving surgery and 16 patients in their series delivered babies. Brewer et al. [12] described 26 patients of dysgerminoma in whom 16 underwent fertility-preserving treatment and five pregnancies were noted. Gershenson [13] reported 230 patients of GCT ovary, 40 of these underwent fertility-preserving surgery and 11 patients in this group have delivered 22 healthy infants. In the present study, only one out of 14 patients undergoing fertility-preserving surgery has conceived. This number maybe low as most of our patients were unmarried prior to diagnosis and due to societal taboos continue to remain unmarried long after completing treatment. The patient who conceived has delivered two healthy children following completion of treatment with no history of miscarriages or developmental anomalies. Good outcomes to fertility preservation have been documented in many other studies [10,11,12]. Unlike epithelial ovarian carcinoma, malignant germ cell tumors are amenable to fertility preservation, and hence, conservative surgery should be the standard of care whenever possible.
Conclusion
Survival after fertility-preserving surgery is quite high in ovarian GCT, and return to reproductive function can be expected shortly after completing chemotherapy. BEP is an effective first-line chemotherapy regimen and recurrences if any can be managed effectively with second-line chemotherapy regimens. Longer follow-up is needed to better document miscarriages and malformation that may occur in these patients. High index of suspicion in young females presenting with ovarian lump and timely diagnosis and referral may result in high cure rates with higher possibility of fertility-preserving surgery.
References
Quirk JT, Natarajan N (2005) Ovarian cancer incidence in the United State, 1992-1999. Gynecol Oncol 97(2):519–523
Smith HO, Berwick M, Verschraegen CF, Wiggins C, Lansing L, Muller CY, Qualis CR (2006) Incidence and survival rates for female malignant germ cell tumors. Obstet Gynecol 107(5):1075–1085
Downey J, McKinney M (1992) The psychiatric status of women presenting for infertility evaluation. Am J Orthop 62:196–198
Zanetta G, Bonazzi C, Cantu M, Binidagger S, Locatelli A, Bratina G, Mangioni C (2001) Survival and reproductive function after treatment of malignant germ cell ovarian tumors. J Clin Oncol 19(4):1015–1020
Maheshwari A, Gupta S, Parikh PM, Tongaonkar HB (2004) Malignant germ cell tumor ovary—experience at Tata Memorial Hospital. Indian J Med Paediatr Oncol 25(1):43
Gershenson DM, Morris M, Cangir A, Kavanagh JJ, Stringer CA, Edwards CL, Silva EG, Wharton JT (1990) Treatment of malignant germ cell tumors of the ovary with bleomycin, etoposide and cisplatin. J Clin Oncol 8(4):715–720
De Wit R, Roberts JT et al (2001) Equivalence of three or four cycles of bleomycin, etoposide and cisplatin combination therapy and of a 3 or 5 day schedule in good prognosis germ cell cancer: a randomized study of the European Organization for Research and Treatment of Cancer Genitourinary Tract Cancer Cooperative Group and the Medical Research Council. J Clin Oncol 19(6):1629–1640
Saxman SB, Finch D, Gonin R, Einhorn LH (1998) Long term follow up of a phase III study of three versus four cycles of bleomycin, etoposide and cisplatin in favourable prognosis germ cell tumors: the Indian University experience. J Clin Oncol 16(2):702–706
Culine S, Lhomme C, Kattan J, Michel G, Duvillard P, Droz JP (1997) Cisplatin based chemotherapy in the management of germ cell tumors of the ovary: the Institut Gustave Roussy Experience. Gynecol Oncol 64(1):160–165
Perrin LC, Low J, Nicklin JL Ward BG, Crandon AJ (1999) Fertility and ovarian function after conservative surgery for germ cell tumors of the ovary. Aust N Z J Obstet Gynecol 39(2):243–245
Ezzat A, Raja M, Bakri Y, Subhi J, Memon M, Schwartz P, Stuart R (1999) Malignant ovarian germ cell tumors: a survival and prognostic analysis. Acta Oncol 38(4):455–460
Brewer M, Gerhenson DM, Herzog CE Mitchell MF, Silva EG, Wharton JT (1999) Outcomes and reproductive function after chemotherapy for ovarian dysgerminoma. J Clin Oncol 17(9):2670–2675
Gershenson DM (1988) Menstrual and reproductive function after treatment with combination chemotherapy for malignant ovarian germ cell tumors. J Clin Oncol 6(2):270–275
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lakshmanan, M., Gupta, S., Kumar, V. et al. Germ Cell Tumor Ovary: an Institutional Experience of Treatment and Survival Outcomes. Indian J Surg Oncol 9, 215–219 (2018). https://doi.org/10.1007/s13193-018-0742-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-018-0742-x