Abstract
Although rare over most of the world, Gallbladder cancer is very common in northern india. A delayed presentation, aggressive nature,lack of randomised trials and a poor prognosis have all contributed to the nihilistic halo encircling gallbladder cancer. None of the advances in oncology have been exploited enough to shatter the nihilistic halo. In this background we sought to analyze if the addition of neoadjuvant chemotherapy had any impact on the resectability, overall and disease free survival in patients with advanced carcinoma of the gallbladder. We reviewed the records of all patients who underwent surgery for carcinoma of the gall bladder from 2004 to 2010 at our institute retrospectively. Twenty-one patients received neoadjuvant chemotherapy and subsequently taken up for surgery. Outcome analysis of these 21 patients were done by Kaplan meier method and graphs plotted. Out of the 21 patients who were taken up for surgery after neoadjuvant chemotherapy, fourteen patients underwent R0 resection (Group 1). Seven patients had been rendered inoperable on exploration (Group 2). Thus about 66.67 % of patients deemed resectable after neoadjuvant chemotherapy on imaging underwent R0 resection. The mean overall survival of the group 1 was 42.8 months versus 6.6 months of group 2(Hazard Ratio: 3.42). Neoadjuvant chemotherapy improves resectability in some patients with unresectable gall bladder cancer. Resection after neoadjuvant chemotherapy is feasible and may improve survival in a select group of patients. However randomized studies are required to establish its definitive role.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maximilian Stoll from Vienna first described gallbladder cancer in 1777 [1]. It is a rare malignancy in most of the world contributing to just 4 % of gastrointestinal cancers. However there is a very high incidence of this cancer among women in Northern India (21.5/100,000) [2]. Carcinoma Gall bladder is an aggressive disease with late presentation, rapid progression, early recurrence,and dismal outcome. In 1924 Alfred Blalock concluded “in malignancy of the gallbladder when a diagnosis can be made without exploration, no operation should be performed, in as much as it only shortens the patient’s life”. In a review of the literature up to 1978, Piehler and Crichlow reported only a 5 % 5-year survival and a median survival of 5 to 8 months for 5,836 cases. Even for the 25 % who were treated by resection with curative intent, only 16.5 % survived 5 years [3].
George Pack was the first to advocate radical liver resection as treatment for gallbladder cancer, reporting in 1955 on the first three gallbladder cancers treated by right hepatic lobectomy and portal lymph node dissection [4]. V.K. Kapoor observed that the pessimistic attitude of the western world resulted in inadequate treatment while the Japanese aggressivism reported high mortality. The Indian “middle path” — surgical resection for “less-advanced” GBC and nonsurgical palliation for “more-advanced” GBC — is probably most appropriate [5].
In this background we sought to analyze if the advocation of neoadjuvant chemotherapy in the setting of locally advanced & metastatic gallbladder cancer had any significant benefit in terms of cure.
Materials & Methods
We reviewed the medical records of patients who underwent surgery for gallbladder cancer in our institute from June 2004 to June 2010 retrospectively. The distribution of various surgical procedures were studied. Twenty-one of them received neoadjuvant chemotherapy and subsequently taken up for surgery. Outcome analysis of these 21 patients were done by Kaplan meier method and graphs plotted. The data were analysed using SPSS 16 for windows.
Results
Sixty-seven patients underwent surgery for gallbladder cancer. Mean age of onset was 55.8 years. Eleven were men. Fifty six were women. Seventeen patients were incidental carcinoma of gallbladder. They had undergone laparoscopic/simple cholecystectomy elsewhere and diagnosed adenocarcinoma on final histopathological evaluation. They underwent wedge resection of liver with porta lymph node dissection and port site excision. Ten patients deemed resectable on imaging, however had undetected metastatic disease or were unresectable on exploration. Eighteen patients underwent either radical/extended cholecystectomy (R0). One patient underwent R1 resection. Twenty-one patients who were either unresectable (locally advanced N2) or metastatic (liver only) were given neoadjuvant chemotherapy. They were reassessed after completion of 3 cycles. Ten patients showed significant response on imaging (rendered resectable) after 3 cycles. The rest of the patients were downstaged after 6 cycles. They were subsequently taken up for surgery. Twelve patients underwent radical cholecystectomy. One patient underwent right hepatectomy and one underwent radical cholecystectomy with hepatic metastectomy. In short 14 patients had R0 resection(group 1). Seven patients had been rendered inoperable on exploration (group 2). Thus 66.67 % of the patients who were taken up for surgery after neoadjuvant chemotherapy were resectable.
In patients who underwent neoadjuvant chemotherapy, three of them received 5FU based regimen whereas the rest of them received Gemcitabine based therapy. Patients in the 5FU group received Inj Oxaliplatin [85 mg/m2 D1],Inj 5-Fluorouracil [400 mg/m2 D1-2 IV bolus and 600 mg/m2 D1-2 by IV infusion] and Inj Leucovorin [200 mg/m2 D1-2]. In the Gemcitabine group patients received Inj Gemcitabine [1000 mg/m2 D1& D8] and Inj Cisplatin [35 mg/m2 D1-2] or Carboplatin[AUC 5] in case of compromised renal function. In the subgroup who underwent exploratory laparotomy, the follow up was dismal ranging from 0 days to a maximum of 11 months. In the subgroup who underwent definitive resection following neoadjuvant chemotherapy, follow up ranged from 4 to 60 months. Three patients received adjuvant radiation. Patients who received 3 cycles of neoadjuvant chemotherapy went on to complete three more cycles of chemotherapy after surgery. The histology was adenocarcinoma in 20 patients and collision tumor in one patient.
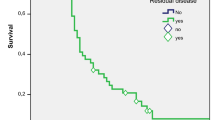
The mean overall survival of the group 1 was 42.8 months versus 6.6 months of group 2. It is remarkable to note that group 1 failed to achieve the median survival time. To simplify, At 11 months, only 40 % of group 2 survived whereas 67 % of group 1 survived (Figs. 1 and 2). The survival analyses were compared by means of Cox Mantel log rank test that reported a p value of 0.112 (Table 1). Though the tests did not achieve statistical significance (which would have been possible had the study population been larger), they have demonstrated a hazard ratio of 3.42(95 % CI 0.6822–17.15).
Discussion
Gall bladder cancer may be rare to the rest of the world. But it is common in northern india. Despite advances in diagnosis and treatment of gall bladder, long term outcomes remain dismal. Surgery alone provides a reasonable probability of long term survival in patients with carcinoma of the gall bladder [6].
Unfortunately, over 60 % of gall bladder cancer patients present at an advanced stage and are not candidates for surgical resection. Thus resectablity is the limiting factor. An aggressive approach is required to resect advanced carcinoma of the gallbladder. However, an extended surgical procedure often brings about a poor surgical outcome.
In a study by Ishikawa et al. about 59 patients with stage IV primary carcinoma of the gall bladder were divided into three treatment groups for the survival analysis: group A (resectional surgery, n = 29), group B (low-dose cis-diamminedichloroplatinum-II and 5-fluorouracil therapy, n = 10), and group C (exploratory laparotomy, other treatment modalities, or no treatment, n = 20). The prognosis of group A patients was significantly better than that of group B (P = 0.018) or group C (P = 0.0009). Furthermore, group A patients were divided into subgroups. The prognosis of patients resected with no distant metastasis (group A1) was significantly better than that of patients resected with distant metastases of the distant lymph nodes and the liver (group A2) (P = 0.0004). Also, there was no significant difference in the survival rate between the patients resected with distant metastasis (group A2) and chemotherapy cases (group B) [7].
Behari et al. performed a survival analysis of 42 patients who underwent extended resections for gallbladder cancer. R0 status was achieved in 18 patients (43 %): 100 %, 100 %, 45 %, and 0 % in stages I, II, III, and IV, respectively. Patients with R0 resections had a significantly better survival than those with R1 resections (median 25.8 months versus 17.0 months; p = 0.03). R0 status was achieved in only three of 20 patients (15 %) with node positive (N1) disease compared with 14 of 17 patients (82 %) with node negative (N0) disease. Adjuvant therapy did not have a significant effect on survival [8].
The course of 66 patients operated for advanced gallbladder carcinoma was evaluated in a retrospective study by Bloechle et al.; 14 % of patients had stage II, 29 % had stage III, and 57 % had stage IV tumors. Complete tumor resection (R0) was achieved in six patients with cholecystectomy (CHE) and lymphadenectomy (LA), in 14 patients with CHE combined with segment IV/V liver resection (LR) and LA, and in all patients with right extended hemihepatectomy (EHH). Resections with microscopic residual tumor (R1) were performed in nine patients. In R0 resections, mean survival was 23.3, 25.0, and 26.3 months for the patients who underwent CHE and LA, CHE combined with segment IV/V LR and LA, and right EHH, respectively. After 24 months, 46.4 % of the patients with R0 resection were still alive compared with none of the patients with residual tumor [9].
In short, R0 resection even in advanced carcinoma of the gall bladder had an impact on survival. But the question is how to achieve R0 resection in advanced carcinoma of the gall bladder with limited morbidity & mortality?In an attempt to resolve this issue we sought to analyze if the addition of neoadjuvant chemotherapy would impact the survival of patients with advanced carcinoma of the gall bladder.
No drug therapy has proven efficacious for gallbladder cancer. Traditional adjuvant chemotherapeutic regimens have generally included fluorouracil. Recently, gemcitabine has been compared to 5-FU (Fluorouracil) and Leucovorin in a phase-II trial in advanced biliary tract cancers including Gallbladder cancer. The results suggest that gemcitabine has equivalent activity compared to 5-FU and leucovorin.
In a Phase II study of gemcitabine and cisplatin in chemotherpy naive,unresectable gall bladder cancer, Doval et al. have achieved an RR of 36.6 % (95 % CI 34–40 %) in 30 evaluable patients, with median response duration of CR/PR being 58/20 weeks. With an additional 23.3 % patients experiencing stable disease, chemotherapy resulted in abrogation of progression in 60 % of the patients [10].
Chatni et al. studied 65 patients of inoperable gall bladder carcinoma who were given 5FU and CDDP. The results were promising including a response rate of 33.9 % and a I year survival of 18.5 % [11]. One patient with locoregional disease and complete response after three cycles of chemotherapy underwent surgical resection followed by chemoradiation. She remained diseasefree at 48 months.
There have been such anecdotal reports of resection of carcinoma gall bladder after neoadjuvant chemotherapy. Morimoto et al. have reported a case report of carcinoma gallbladder resected after chemotherapy [12].
Conclusions
Neoadjuvant chemotherapy enables R0 resection in some patients with initially unresectable gall bladder cancer. R0 resection following neoadjuvant chemotherapy has shown superior survival rates than the unresectable group. Even though the results are promising,this is a retrospective study of a small population. Both R0 resection and neoadjuvant chemotherapy contribute to the survival advantage,but the proportion to which each of them contribute independently is yet to be evaluated. Prospective studies are required further to define the response and resectability rate of neoadjuvant chemotherapy and thereafter the survival advantage.
References
Stoll M In: Rationismedendi in nosocomiopracticoVindobonensi.Pars prima; Sumtibus August Bernardi- Wien, 1777: 254–8
Miller G, Jarnagin WR (2008) Gallbladder carcinoma. Eur J Surg Oncol 34:306–312
Piehler JM, Crichlow RW (1978) Primary carcinoma of the gallbladder. Surg Gynecol Obstet 147:929–942
Pack GT, Miller TR, Brasfield RD (1955) Total right hepatic lobectomy for cancer of the gallbladder: report of three cases. Ann Surg 142(1):6–16
Kapoor VK (2007) Advanced gallbladder cancer: Indian “middle path”. J Hepato-Biliary-Pancreat Surg 14:366–373
Kaushik SP (2001) Current perspectives in gallbladder carcinoma. J Gastroenterol Hepatol 16:848–854
Ishikawa T, Horimi T, Shima Y, Okabayashi T, Nishioka Y, Hamada M et al (2003) Evaluation of aggressive surgical treatment for advanced carcinoma of the gallbladder. J Hepato-Biliary-Pancreat Surgery 10(3):233–238
Behari A, Sikora SS, Wagholikar GD, Kumar A, Saxena R, Kapoor VK (2003) Long term survival after extended resections in patients with gallbladder cancer. J Am Coll Surg 196(1):82–88
Bloechle C, Izbicki JR, Passlick B, Gawad K, Passow C, Rogiers X et al (1995) Is radical surgery in locally advanced gallbladder carcinoma justified? Am J Gastroenterol 90(12):2195–2200
Doval DC, Sekhon JS, Gupta SK, Fuloria J, Shukla VK, Gupta S, Awasthy BS (2004) A phase II study of gemcitabine and cisplatin in chemotherapy-naive, unresectable gall bladder cancer. Br J Cancer 90:1516–1520
Chatni SS, Sainani RS, Mehta SA, Mohandas KM (2008) Infusion chemotherapy with cisplatinum and fluorouracil in the treatment of locally-advanced and metastatic gallbladder cancer. J Can Res Ther 4:151–155
Morimoto H, Ajiki T, Takase S, Fujita T, Matsumoto T, Mita Y, Matsumoto I et al (2008) Resection of gallbladder cancer with hepatic metastasis after chemotherapy with gemcitabine. J Hepato-Biliary-Pancreat Surg 15(6):655–658
Ethical statement
The authors disclose no actual or potential conflicts of interest. This type of study does not require formal consent. This article does not include any study involving animals or human participants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Selvakumar, V.P.P., Zaidi, S., Pande, P. et al. Resection After Neoadjuvant Chemotherapy in Advanced Carcinoma of the Gallbladder: a Retrospective Study. Indian J Surg Oncol 6, 16–19 (2015). https://doi.org/10.1007/s13193-015-0377-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-015-0377-0