Abstract
Background
The squamous cell carcinoma (SCC) of the oral tongue is a common cancer in India. Elective lymphadenectomy is generally performed in all patients with T2-T4 tumors. In this study we have tried to analyze the pattern and risk factors associated with lymph node metastasis in T1 tongue cancers.
Methods
A retrospective review of the records of 57 patients undergoing surgery for treatment of T1 sqamous cell carcinoma of oral tongue was carried out. The clinicopatological features of the tumor, pattern of nodal metastasis and the risk factors associated with lymph node metastasis were studied.
Results
Totally 57 patients with T1 tumor underwent excision of the primary and modified neck dissection (MND). Lymph node metastasis was found in 36.8 % of the patients. Level I to Level II was the commonest site of metastasis. Skip metastasis at level III and IV was found in 8.5 % of the patients and isolated skip metastasis at level IV in 1.5 % of the patients. The risk factors associated with the lymph node metastasis on univariete analysis were; higher grade, tumor size >1 cm and tumor thickness >3 mm. On multivariate analysis only the tumor thickness was found to be a risk factor for the lymph node metastasis (hazard ratio of 21.59).
Conclusions
T1 sqamous cell carcinoma of tongue is associated with a high incidence of lymph node metastasis. Elective neck dissection should be considered in all patients with tumors more than 3 mm in thickness
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carcinoma of oral tongue is the most common cancer of the oral cavity in the world and the second most common cancer of oral cavity in India. Tongue, because of its structure and function is prone for early local and regional spread of cancer. Lymph node metastasis is the strongest predictor of prognosis in head and neck cancers with the survival decreasing by 50 % in the presence of metastasis [1–3]. Elective lymphadenectomy is recommended whenever risk of metastasis is >20 % [4]. All the patients of cancer of tongue stage T2-T4, generally undergo elective neck dissection because of high incidence micro metastasis.
Our aim in this study was to study the incidence, pattern of lymph node metastasis and the risk factors associated with metastasis in T1(<2 cm) tongue cancers.
Patients and Methods
A retrospective analysis of 57 patients undergoing primary surgical resection with modified neck dissection (MND 1 or MND 2) for T1 (<2 cm) tongue cancers with N0 neck b/n July 2006 to December 2007(18 months) was carried out. Only patients with AJCC staging of T1 (<2 cm) undergoing primary surgery with modified neck dissection of the neck were included in the study. Exclusion criteria were tumor size >T1 (2 cm), recurrent tumor, post radiation tumors, multiple tumors, prior neck surgery and patients undergoing supraomohyoid neck dissection. Patient variables like sex, age, size of the tumor, grade of the tumor, tumor thickness, lymphovascular invasion, perinueral invasion and histopathological levels of nodal involvement were obtained from the case records.
Statistical analysis was done using SPSS 13 for Windows ( SPSS Chicago Ill). Risk factor analysis was done using ×2 test and Fisher T test. Multivariate analysis was done using logistic regression analysis. P value <0.05 was taken as significant.
Results
All patients underwent primary tumor excision with modified neck dissection. The age of the patients ranged from 25 to 65 years (mean 44.89). There were 43 Males and 14 females (3.07 to 1).
The mean size of tumor was 1.34 cm (range 0.6–2 cm ). Tumor thickness varied from 0.1 to1.2 cm (mean 0.39 cm). Tumor was grade1 in 22 patients (38.6 %), grade 2 in 32 patients (56.1 %) and grade 3 in 3 patients (5.6 %).
No patient had a positive margin after excision. Two patients showed lymphovascular invasion and perinueral invasion.
All the57 patients underwent modified neck dissection (MND). Twenty two patients underwent MND1 and 35 patients underwent MND2. The average nodal yield after neck dissection was 23.59(range 7–38).
Thirty six (63.15 %) patients were N0 after pathological examination and 21 patients (36.85 %) showed neck node metastasis. Pattern of nodal metastasis is depicted in the Table 1.
Out of the 21 patients with nodal metastasis 15 patients had a single node metastasis (N1). Level I and Level II was the commonest site to be involved (ten patients). Four patients had metastasis at level III without level I or II involvements. Two patients had metastasis at level IV (3.51 %) with 1 patient having skip metastasis at level IV (1.75 %). One patient (1.75 %) showed presence of level V metastasis along with metastasis at other levels.
On univariete analysis the risk factors associated with the lymph node metastasis were the tumor size, tumor grade and the tumor thickness. T1 tumors were divided into size <1 cm and size >1 cm. Only one patient with tumor size less than 1 cm had lymph node metastasis making the tumor size a significant risk factor for metastasis (p < .005).
It was seen that patients with higher grade had a higher risk of metastasis (grade 1–18.2 %, grade2-46.9 %, grade 3–66.7 %) although it did not reach statistical significance (P = 0.054). Tumors with the depth of invasion >3 mm had a very high risk of metastasis. (P < .0002), as compared to tumor less than 3 mm in thickness (Table 2).
On multivariate analysis only the tumor thickness >3 mm was found to be a significant risk factor for lymph node metastasis (Hazard ratio of 21.59) (Table 3).
Discussion
The lymph node metastasis is the strongest predictor of survival of head and neck cancers with the survival coming down by 50 % in the presence of lymph node metastasis [1–3] cancer of tongue is notorious for its early metastasis. Radical neck dissection has been the gold standard for the regional control of the disease ever since George Crile described it more than a century ago [5]. The functional morbidity associated with radical neck dissections made people to refine this technique over the years. Presently modified neck dissection (MND) is the standard procedure for the neck control. As metastasis in the neck follows a stepwise pattern it has been recommended that supraomohyoid selective neck dissection should suffice for N0 neck [6, 7].
In our study a very high proportion of male patients (3.07:1) could be attributed to the habit of gutka chewing (form of tobacco) particularly prevalent among males in this part of India.
Twenty one of the 57patients had nodal metastasis (36.85 %) making strong case for elective treatment of the neck. Studies have shown differing rates of lymph node metastasis in T1 tumors. While An et al. reported metastasis rate of 15.4 % in their study Nithya et al. had 47 % [8, 9].
Level I and Level II was the commonest site of metastasis. Of all the patients, five patients (8.75 %) had metastasis at level III or IV without involvement of level I and II (4 at level III and 1 direct skip metastasis at level IV). The incidence of Skip Metastasis at level IV has ranged from 3 to 28 % in different studies [10–12]. Level V metastasis was seen in only one patient that too in presence of metastasis at other levels. Routine level V dissection can be avoided in most of the patients [13].
It was seen that patients with higher grade had a higher risk of metastasis. The risk of metastasis was 18.2 % for grade I tumors and 66.6 % for grade 3 tumors, all though it failed to reach statistical significance (p = .054). Various studies have shown grade to be predictor of lymph node metastasis. Shear et al. in nearly 900 patients found grade and size as predictive factors of lymph node metastasis [14]. Byers et al. found that an increasing tumor grade predicted lymph node metastasis (odd ratio2.40) [15]. Sparano et al. and Lim et al. also showed positive correlation between grade of the tumor and lymph node metastasis [16, 17].
On dividing the tumors to size <1 cm and >1 cm it was seen that only one patient with tumor less than 1 cm had lymph node metastasis (p < 0.005). Byers et al. and Sparano et al. in their studies described the correlation between increasing tumor size and lymph node metastasis [15, 16].
Strongest predictor of lymph node metastasis in our study was tumor thickness. 7.4 % of the patients with Tumors less than 3 mm in thickness had lymph node metastasis where as 63.33 % of patients with tumors more than 3 mm had metastasis (p < .0002). Spiro et al. first described the relationship between tumor thickness and lymphatic metastasis in tongue and floor of mouth tumors [18]. Many studies subsequently have shown a strong correlation between the thickness of tumor and lymph node metastasis. Using <3 mm as a cutoff value Yuen et al. reported an incidence of 8 % versus 50 % [19]. Kurokawa et al. reported nodal relapse of 2.9 % vs. 37.5 % taking 4 mm as a cutoff value [20]. Byers et al., Lim et al. and Asakage et al. also identified a threshold thickness of 4 mm [15, 17, 21]. Whereas Fukano et al. and Hyashi et al. suggested 5 mm as the cutoff value [22, 23].
In our study there was no correlation between lymphovascular and perinueral invasion and neck metastasis but other studies have found them to be independent predictors [16, 20].
It has been found that clinical examination is notoriously inadequate in neck staging with very high false negative rates. Use of radiological means like ultrsonography and CT scan has not contributed much to improvement in the staging [24, 25]. Even the intra operative assessment has been found to be grossly inaccurate [26, 27]. New imaging methods like PET-CT scan is not sensitive enough to modify the indication of elective neck dissection [28]. USG guided FNAC has been shown to be the most accurate method of detecting cervical lymph node metastasis among all the diagnostic methods [29]. US-FNA had a very high specificity; if the US-FNA cytology had a positive result, almost all of the histology specimen results also proved positive. US is preferred for neck status follow-up in “watchful waiting” patients, and US-FNA can be performed if nodal metastasis is suspected [30].
Li et al. found that modern imaging modalities had fair diagnostic performance in cN0 neck patients. For positive imaging results, elective neck dissection is indicated; for some select low-risk patients with pre-test probability below 30 % of nodal metastasis, a “watchful waiting policy” may be an acceptable alternative to neck dissection if strict adherence to a cancer surveillance protocol is followed [30].
Since our patients were carcinoma tongue with possible high pre test possibility >30 % of occult metastasis we were justified in not doing any pre test imaging modality before offering neck dissection.
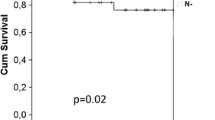
Whether survival benefit is achieved by elective neck dissection in all patients with early tongue cancer remains uncertain. Only three small RCTs have been performed to date [31–33] out which one study has shown survival benefit for the elective neck dissection group [33]. But at the same time the salvage rate after neck recurrence has been very poor. Ho et al. reported that the salvage rate after the appearance of the nodal metastasis was 30 % [34].
Conclusion
The high incidence of neck metastasis in T1 tumors with N0 neck, especially with poor grade, larger size (>1 cm) and thickness(>3 mm.) and the unreliability of clinical examination and adjunct investigations in detecting occult metastasis makes elective treatment of the neck either by surgery or radiotherapy necessary. We suggest that all the patients of T1 tongue cancers treated with tumor thickness more than 3 mm should undergo at least a supraomohyoid neck dissection.
References
Ferlito A, Rinaldo A, Devaney KO, MacLennan K, Meyers JN, Petruzzelli GJ (2002) Prognostic significance of microscopic and macroscopic extracapsular spread from metastatic tumor in the cervical lymph nodes. Oral Oncol 38:747–751
Magnano M, De Stefani A, Lerda W, Usai A, Ragona R, Bussi M (1997) Prognostic factors of cervical lymph node metastasis in head and neck squamous cell carcinoma. Tumori 83:922–926
Mamelle G, Pampurik J, Luboinski B, Lancar R, Lusinchi A, Bosq J (1994) Lymph node prognostic factors in head and neck squamous cell carcinomas. Am J Surg 168:494–498
Weiss MH, Harrison LB, Issacs RS (1994) Use of decision analysis in planning and management for N0 neck. Arch Otolaryngol Head Neck Surg 120:699–702
Kazi RA (2003) The life and times of George Washington Crile. J Postgrad Med 49:289–290
Byers RM (1991) Neck dissection: concepts, controversies, and technique. Semin Surg Oncol 7:9–13
Stringer SP (1995) Current concepts in surgical management of neck metastases for head and neck cancer. Oncology 9:547–554
SY A, Jung EJ, Lee M, Kwon TK (2008) Factors related to regional recurrence in early stage squamous cell carcinoma of the oral tongue. Clin Exp Otorhinolaryngol 1:166–170
Nithya C, Pandey M, Naik B, Ahamed IM (2003) Patterns of cervical metastasis from carcinoma of the oral tongue. World J Surg Oncol 1(1):10
Byers RM, Weber RS, Andrews T, McGill D, Kare R, Wolf P (1997) Frequency and therapeutic implications of “skip metastases” in the neck from squamous carcinoma of the oral tongue. Head Neck 19:14–19
Shah JP, Candela FC, Poddar AK (1990) The patterns of cervical lymph node metastases from squamous carcinoma of the oral cavity. Cancer 66:109–113
Woolgar JA (1997) Detailed topography of cervical lymph-node metastases from oral squamous cell carcinoma. Int J Oral Maxillofac Surg 26:3–9
Davidson BJ, Kulkarny V, Delacure MD, Shah JP (1993) Posterior triangle metastases of squamous cell carcinoma of the upper aerodigestive tract. Am J Surg 166:395–398
Shear M, Hawkins DM, Farr HW (1976) The prediction of lymph node metastases from oral squamous carcinoma. Cancer 37:1901–1907
Byers RM, El-Naggar AK, Lee YY, Rao B (1998) Can we detect or predict the presence of occult nodal metastases in patients with squamous carcinoma of the oral tongue? Head Neck 20:138–144
Sparano A, Weinstein G, Chalian A, Yodul M, Weber R (2004) Multivariate predictors of occult neck metastasis in early oral tongue cancer. Otolaryngol Head Neck Surg 131(4):472–476
Lim SC, Zhang S, Ishii G, Endoh Y, Kodama K (2004) Predictive markers for late cervical metastasis in stage I and II invasive squamous cell carcinoma of the oral tongue. Clin Cancer Res 1:166–172
Spiro RH, Huvos AG, Wong GY, Spiro JD, Gnecco CA, Strong EW (1986) Predictive value of tumor thickness in squamous carcinoma confined to the tongue and floor of the mouth. Am J Surg 152:345–350
Yuen AP, Lam KY, Chan AC, Wei WI (1999) Clinicopathological analysis of elective neck dissection for N0 neck of early oral tongue carcinoma. Am J Surg 177:90–92
Kurokawa H, Yamashita Y, Takeda S, Zhang M (2002) Risk factors for late cervical lymph node metastases in patients with stage I or II carcinoma of the tongue. Head Neck 24:731–736
Asakage T, Yokose T, Mukai K, Tsugane S, Tsubono Y, Asai M (1998) Tumor thickness predicts cervicalmetastasis in patientswith stage I/II carcinoma of the tongue. Cancer 82:1443–1448
Fukano H, Matsuura H, Hasegawa Y, Nakamura S (1997) Depth of invasion as a predictive factor for cervical lymph node metastasis in tongue carcinoma. Head Neck 19:205–210
Hayashi T, Ito J, Taira S, Katsura K (2001) The relationship of primary tumor thickness in carcinoma of the tongue to subsequent lymph node metastasis. Dentomaxillofacial Radiol 3:242–245
Merritt RM, Williams MF, James TH, Porubsky ES (1997) Detection of cervical metastasis: a meta-analysis comparing computed tomography with physical examination. Arch Otolaryngol Head Neck Surg 123:149–152
Giancarlo T, Palmieri A, Giacomarra V, Russolo M (1998) Pre-operative evaluation of cervical adenopathies in tumours of the upper aerodigestive tract. Anticancer Res 18:2805–2809
Rassekh CH, Johnson JT, Myers EN (1995) Accuracy of intraoperative staging of the NO neck in squamous cell carcinoma. Laryngoscope 105:1334–1336
Finn S, Toner M, Timon C (2002) The node-negative neck: accuracy of clinical intraoperative lymph node assessment for metastatic disease in head and neck cancer. Laryngoscope 112:630–633
Schoder H, Carlson DL, Kraus DH, Stambuk HE, Gonen M, Erdi YE (2006) 18F-FDG PET/CT for detecting nodal metastases in patients with oral cancer staged N0 by clinical examination and CT/MRI. J Nucl Med 47:755–762
de Bondt RB, Nelemans PJ, Hofman PA, Casselman JW, Kremer B, van Engelshoven JM et al (2007) Detection of lymph node metastases in head and neck cancer: a meta-analysis comparing US, USgFNAC, CT and MR imaging. Eur J Radiol 64:266–272
Liao L-J, Lo W-C, Hsu W-L, Wang C-T, Lai M-S (2012) Detection of cervical lymph node metastasis in head and neck cancer patients with clinically N0 neck-a meta-analysis comparing different imaging modalities. BMC Cancer 12:236
Vandenbrouck C, Sancho-Garnier H, Chassagne D, Saravane D, Cachin Y, Micheau C (1980) Elective versus therapeutic radical neck dissection in epidermoid carcinoma of the oral cavity: results of a randomized clinical trial. Cancer 46:386–390
Fakih AR, Rao RS, Borges AM, Patel AR (1989) Elective vs. therapeutic neck dissection in early carcinoma of the oral tongue. Am J Surg 158:309–313
Kligerman J, Lima RA, Soares JR, Prado L, Dias FL, Freitas EQ (1994) Supraomohyoid neck dissection in the treatment of T1/T2 squamous cell carcinoma of oral cavity. Am J Surg 168:391–394
Ho CM, Lam KH, Wei WI, Lau SK, Lam LK (1992) Occult lymph node metastasis in small oral tongue cancers. Head Neck 12:359–363
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
S, V., Rohan, V. Cervical node metastasis in T1 squamous cell carcinoma of oral tongue- pattern and the predictive factors. Indian J Surg Oncol 5, 104–108 (2014). https://doi.org/10.1007/s13193-014-0301-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-014-0301-z