Abstract
The Friend to Friend plus Patient Navigation Program (FTF+PN) aims to build an effective, sustainable infrastructure to increase breast and cervical screening rates for underserved women in rural Texas. The objective of this paper is to identify factors that (1) distinguish participants who chose patient navigation (PN) services from those who did not (non-PN) and (2) were associated with receiving a mammogram or Papanicolaou (Pap) test. This prospective study analyzed data collected from 2689 FTF+PN participants aged 18–99 years from March 1, 2012 to February 28, 2015 who self-identified as African American (AA), Latina, and non-Hispanic white (NHW). Women who were younger, AA or Latina, had less than some college education, attended a FTF+PN event because of the cost of screening or were told they needed a screening, and who reported a barrier to screening had higher odds of being a PN participant. Women who were PN participants and had more contacts with program staff had greater odds of receiving a mammogram and a Pap compared with their reference groups. Latina English-speaking women had lower odds of receiving a mammogram and a Pap compared with NHW women and Latina Spanish-speaking women had higher odds of receiving a Pap test compared with NHW women. Women with greater need chose PN services, and PN participants had higher odds of getting a screening compared with women who did not choose PN services. These results demonstrate the success of PN in screening women in rural Texas but also that racial/ethnic disparities in screening remain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Racial/ethnic minority and rural women experience lower screening rates and delays in mammograms and Papanicolaou (Pap) tests compared to non-Hispanic white (NHW) women and urban residents leading to a greater cancer burden for these individuals [3, 9]. Diagnostic and therapeutic delays may lead to greater treatment difficulty and increased cost for both the individual and healthcare system as breast is the leading and cervical is the fourth leading cancer diagnosis among women nationally and in Texas [24]. Early detection of breast and cervical cancer through screening may improve survival and decrease mortality rates by detecting malignancies at a noninvasive stage, resulting in more successful treatment [6]. As a result, improving the well-being of underserved communities by reducing the impact of these cancers for minority and rural women remains a priority for policy makers, researchers, and clinicians [18].
Researchers have developed interventions aimed at improving screening rates for racial/ethnic minority and rural women through health education and patient navigation (PN) [19, 1]. PN, an evidence-based practice within the cancer care continuum and other diseases, is a patient-centered healthcare delivery model that utilizes trained lay navigators to integrate a fragmented system of care in order to reduce barriers to timely care for individuals and subsequently reduce disparities for population groups [13].
The objective of this paper is to evaluate programmatic outcomes of a health education and PN intervention for rural women in Texas by identifying sociodemographic and other screening-related factors that (1) distinguish participants who chose PN services from those who did not (non-PN) and (2) were associated with receiving a mammogram or Pap test.
Intervention
In 2010, the Texas A&M AgriLife Extension Service was awarded outreach education funding by the Cancer Prevention Research Institute of Texas (CPRIT) to adapt the evidence-based program, Friend to Friend (FTF) in rural and border counties in Texas [23]. FTF consists of “pink parties” targeting an audience of lower income, un-/underinsured women aged 40+ who may be disabled, self-employed, and/or have limited English proficiency (LEP).
The CPRIT funding supported hiring four, full-time equivalent regional cancer prevention specialists to work with county extension agents to organize local work groups of women to deliver the FTF program and educate women about the need for mammograms and Pap tests. However, the funding did not allow for follow-up or active support for women to obtain the screenings. To address these issues and increase the number of women screened, clinical service funding was sought and awarded by CPRIT, allowing the addition of four full-time equivalent patient navigators to join the team of regional cancer prevention specialists, payment for clinical services when needed, and transportation services.
The purpose of the, now, Friend to Friend plus Patient Navigation Program (FTF+PN) is to build an effective, sustainable infrastructure and overcome barriers to breast and cervical screening and diagnostic services to increase screening rates for underserved, un-/underinsured, and older women in approximately 50 rural and border counties. The goal is to increase the number of women screened according to American Cancer Society (ACS) guidelines for breast and cervical cancer, thereby increasing the probability any cancers detected would be diagnosed in earlier stages. At the time, ACS guidelines recommended annual mammograms for women aged 40–54 and biannual mammograms for those aged 55+ with average risk of breast cancer [2]. For cervical cancer screenings, recommendations included Pap tests every 3 years for women aged 21–29 and every 5 years for women aged 30–65 with no additional screenings needed for women aged 65+ if their previous results were normal [22].
Methods
This prospective study analyzed program evaluation data collected from FTF+PN participants and events from March 1, 2012 to February 28, 2015. The Institutional Review Board (IRB) of The University of Texas at Austin reviewed and approved (FWA no. 00002030) the proposed study prior to analysis. Data included responses to pre- and posttest surveys of the education intervention (FTF) and follow-up surveys of screening behavior by non-PN and PN participants, totaling N = 2689 unique respondents meeting inclusion criteria for the final analytic sample. The sample included women aged 18 to 99, who self-identified exclusively as African American (AA), Latina, and NHW. Individuals indicating multiple race/ethnicities (n = 123), American Indian or Native American (n = 29), Asian, Asian-American, or Pacific Islander (n = 20), and other race/ethnicity or missing (n = 21) were excluded due to small sample sizes. Also, subsequent responses for women attending multiple parties (n = 346) were excluded.
Two survey items identify Latinas. The first asked the respondent to identify their race/ethnicity, with “Latino, Hispanic, Chicano, Mexican or Mexican-American, Central American, or other Latin American” as one response option. The second asked about primary language used at home. Primary language use at home, conceptualized as a marker of acculturation, distinguished Latinas who only spoke English (Latina English-speaking women (ES); n = 399) from those who only spoke Spanish or used Spanish and English equally (Latina Spanish-speaking women (SS); n = 1261). Language accounts for most of the explained variance in studies of acculturation measures [5], and brief, language-based measures of acculturation have been validated among Latino groups with English or Spanish language preferences [16]. This variable helps to distinguish nuances among Latina participants using an available survey item approximating this measure. Thus, four demographic groups were defined according to race/ethnicity and acculturation (AA, Latina ES, Latina SS, and NHW).
Dependent variables recorded on the follow-up surveys included PN status, receipt of mammogram screening, and receipt of Pap screening. Each FTF participant was offered a “help request form” to indicate the need for PN and screening services following the education program. Respondents providing contact information on the posttest survey and/or help request were subsequently interviewed by patient navigators to determine if they received a mammogram or Pap test. The total number of contacts, summing the number of direct contacts (calls, emails, texts, etc.) with a participant and indirect contacts made on behalf of a participant (calls, emails, texts, etc. coordinating services with providers made by the patient navigator or regional cancer specialist that did not include the participant), was also noted on the follow-up survey. Those not providing contact information on the posttest survey or help request and those who had not completed a follow-up interview were excluded from the analysis (see Table 1). Of note, women with and without follow-up information did not differ on important characteristics (data not shown, reviewers see Appendix 1).
Several independent variables from the pretest and posttest surveys were included in the analysis. The pretest captured the respondents’ demographic data including race/ethnicity (self-identified exclusively as AA, Latina, or NHW), primary language use at home (English only, Spanish only, or English and Spanish equally), age (calculated based on year of birth), and education level (categorized as did not complete high school, high school graduate, or some college or more). Participants also self-reported mammogram and Pap test history (dichotomized as receiving a mammogram or Pap test prior to FTF+PN or not) in addition to the main reason for attending FTF (need help paying for tests, came with friend/family member, family history of cancer, doctor/nurse said tests were needed) on the pretest. Individuals reported barriers to screening on the posttest with options including worry about cost, transportation, not having time, problems with child/elder care, nervousness about testing, bad experiences getting care, testing not offered where they live, not knowing where to go, problems getting through the application process for assistance programs, or other reason. All analyses were conducted using SPSS software, version 21 (IBM Corp., Armonk, NY). Findings were considered statistically significant using two-tailed P values of less than 0.05, 0.01, and 0.001.
Results
Table 1 presents the number of sample participants by race/ethnicity and follow-up status. NHWs were the largest group represented (45.2 %) followed by Latina SS (37.5 %), Latina ES (12.6 %), and finally AAs (4.8 %). The sample was further separated by PN cases (27.7 %), non-PN cases (37.9 %), and those with no follow-up (34.5 %) who either omitted contact information effectively closing their case or were still awaiting follow-up at the time of the analysis.
Table 2 provides descriptive statistics of independent variables for the two follow-up categories (PN and non-PN cases) by race/ethnicity. Women aged 40 to 64 consistently represented the largest proportion of PN and non-PN participants in each racial/ethnic category reflecting the goal of FTF+PN as well as ACS guidelines for women most in need for mammogram screening [2]. Latina SS women reported the lowest educational achievement for both PN cases (63.1 %) and non-PN cases (39.2 %). PN participants designated cost as the reason for attending at much higher rates compared to non-PN respondents. Finally, PN participants received mammogram and Pap screenings after the FTF event at much higher rates compared to non-PN respondents.
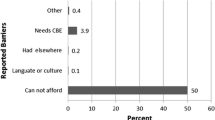
The logistic regression model results for odds of PN status, mammogram screening, and Pap screening appear in Table 3. The first step of the PN hierarchical model identifies that all sociodemographic variables significantly impact PN status. Older women had lower odds of being a PN participant, women of color had 2.4 to 8.5 higher odds of being a PN participant compared with NHW women, and women with lower levels of education had higher odds of being a PN participant compared with women with at least some college education. The second step of the model includes additional screening-related variables. Age, race/ethnicity, and education remained statistically significant, and respondents reporting cost of screening or that a health professional advised them to attend as a reason for attending a FTF+PN event had higher odds of being a PN participant compared with women who did not endorse those reasons. Women reporting a barrier to screening also had higher odds of being a PN participant compared with women reporting no barriers (OR = 4.42, CI = 3.30–5.93). Finally, women reporting that they attended a FTF+PN event because a friend or family member was attending had lower odds of being a PN participant compared with women who did not endorse that reason.
The logistic regression models for mammogram screening follow the PN status models. In the sociodemographic model (step 1), older and Latina SS women and those with lower education had higher odds of receiving a mammogram compared with their respective reference groups. In the second step of the model including screening-related factors, Latina SS women were no longer statistically significantly different from NHW women in the odds of screening, but Latina ES women had lower odds of screening compared with NHW women. Women with a history of a screening and those who came to FTF primarily because a doctor or nurse say that the test was needed had higher odds compared with women with no history and who did not select a doctor or nurse’s recommendation as the main reason for attending. Cost of screening as a reason for participating in a FTF+PN event was associated with 1.8 higher odds of receiving a mammogram compared to those not endorsing that reason. Also, both being a PN participant (OR = 2.64, CI = 1.02–1.91) and respondents with more contacts (OR = 1.14, CI = 1.11–1.17) had greater odds of receiving mammograms compared with non-PN participant status and women with fewer contacts.
Finally, Table 3 presents logistic regression models for getting a Pap test at follow-up in the last two columns. In the sociodemographic model, older women had lower odds and Latina SS women and those with lower education had higher odds of receiving a Pap test compared with younger, NHW, and college educated women. Once the screening-related factors were added in step 2, older women still had lower odds compared with younger women, and Latina SS women still had higher, although attenuated, odds, compared with NHW women. However, Latina ES women were found to have lower odds of receiving a Pap test compared with NHW women and the education odds were no longer statistically significant. As with mammograms, participants indicating cost as a reason for attending a FTF+PN event had higher odds of receiving a Pap screening (OR = 1.80, CI = 1.40–2.32) than those not endorsing this reason. PN participants also had higher odds of receiving a Pap test compared to non-PN participants (OR = 2.72, CI = 2.00–3.69), and a greater number of contacts was associated with higher odds of receiving a Pap screening compared to those with fewer contacts (OR = 1.13, CI = 1.10–1.17).
Of women in the follow-up sample who received a mammogram, 201 had an abnormal finding, 103 received a diagnostic screening, and 22 women were diagnosed with breast cancer. For Pap tests, 70 women had an abnormal finding, 14 received a diagnostic screening, and eight women received a cervical cancer diagnosis. The grant provided funding for continued navigation and clinical services following screening if the women did not qualify for other programs such as Breast and Cervical Cancer Services (BCCS), Medicaid, private insurance, or other options.
Discussion
The results of this study yield several promising findings regarding the impact of adding PN to the FTF health education program to increase breast and cervical cancer screening among women in rural Texas. Participation in PN was associated with an increase in the odds for both mammogram and Pap screenings. In addition, more contacts to the participants themselves or on their behalf increased the odds for screening in these same models. These variables illustrate that PN status and follow-ups are clear points of intervention that can be leveraged to increase the likelihood of participants in FTF+PN to screen successfully for breast and cervical cancer and reflect similar successes reported in preventative screening PN programs. Comparable studies include a promotora-based intervention that significantly increased mammograms in a randomized sample of 381 women living in the US–Mexico border region of Arizona [17]. A quasi-experimental study of 1181 rural women in Louisiana reported higher odds of mammogram screening for those receiving navigation compared to women receiving health education only [8].
The FTF+PN program was successful in reaching its intended target population of women who are at higher risk of unfavorable breast and cervical cancer outcomes [11] and who could benefit from PN services. Rural women of color, those with lower education, those who attended FTF because of concerns about screening cost, and those reporting a barrier to screening had higher odds of being a PN participant compared with their reference groups. While ACS guidelines for mammogram and Pap tests [2, 22] have a limited age range compared to the sample, the intervention did not exclude any participants aged 18+ based on recommendations as women outside of these ranges may need services depending on their individual health status and history. Instead, we chose to include all adults and to control for age for increased power and a consistent sample size. Furthermore, this intervention leverages aspects of social cognitive theory that describes the role of observational learning in behavioral performance through positive reinforcement [15]. Peer networks, including friends and family, model a behavior that the individual incorporates through observation into their own behavior. Observational learning increases self-efficacy, the individual’s belief in her ability to get screened for breast and cervical cancer, as these women learn from interpersonal and community role models. As indicated in Table 3, 31–49 % of women identified attendance to FTF with a friend or family member as the main reason for participating. Women often attend FTF with friends and relatives and respond to the pre- and posttest but may not seek screening. Thus, these women have a lower odds of being a PN participant. Still, FTF educates women of all ages to increase health literacy of these cancers that may affect them directly or other women in their social networks. In sensitivity analyses, we re-ran the logistic regression models according to ACS age guidelines (aged 40 years and over for mammogram screening, aged 21–65 years for Pap screening) and found similar results (reviewers see Appendices 2 and 3).
A main reason for attending FTF+PN was needing help paying for the screening(s). Participants had to connect with a patient navigator or regional cancer prevention specialist in order to pay for the screenings using the funds provided by CPRIT or from other programs of which participants may have been unaware, such as BCCS, other screening programs, private insurance, etc. Despite mandates for full coverage of breast and cervical cancer screening costs under the Affordable Care Act (ACA), additional supportive services are needed to help increase breast and cervical cancer screening for women who remain uninsured after ACA’s implementation and still face cost as a barrier to screening [14]. Therefore, FTF+PN is providing a safety net for rural, low SES women to access mammograms and Pap tests, as Medicaid coverage was not expanded in Texas to increase insurance coverage for the uninsured poor living between 101 and 133 % of the federal poverty level (FPL). The program aimed to provide screening services to un-/underinsured women; however, insurance status was not recorded systematically although navigators may have collected this information from some participants during their initial intake. Future analyses of this data should include measures of health insurance status at the county-level.Advice from a medical service provider has been demonstrated to increase preventative cancer screening [4, 10, 21]. Though this variable was significant in the regression on mammogram screening and not for Pap screening, advice from a nurse or doctor as a reason for attending FTF was associated with nearly a threefold increased odds (OR = 2.54) in choosing PN (see Table 3). This finding highlights the impact of medical provider advice on shaping screening behavior by increasing the readiness of these women to take a step towards screening. Consequently, medical providers must be aware of current prevention recommendations in order to provide accurate health education to their patients based on risk factors including age and family history. This duty is compounded by the evolving nature of the recommendations.
Latina ES women experienced higher odds of PN status and lower odds of receipt of a mammogram or a Pap test compared to NHWs after controlling for other important sociodemographic and screening-related factors. These findings are in contrast with the experience of Latina SS women, who also had higher odds of PN status, but no differences in receipt of a mammogram, and higher odds of a Pap screening compared to NHWs. This positive finding for less acculturated Latinas is important to highlight as Latinas experience much higher incidence and mortality rates of cervical cancer compared to other groups in Texas; further, this finding appears to substantiate the “Hispanic paradox” theorized as the protective effect of immigration on health as less acculturated Latinos born outside the USA consistently exhibit lower morbidity and mortality compared to US born Latinos and NHWs [24]. However, data regarding country of origin and time living in the USA was not collected from this sample; thus, this effect can only be suggested by the limited measure of acculturation based on language. Although the FTF+PN data cannot differentiate Latinas into heterogeneous subgroups, census data indicate 87 % of Latinas in Texas are of Mexican origin [25]. It may be possible that regional differences in PN efforts and providers may have accounted for the differences or that the PNs were more successful at navigating SS women compared with ES women for reasons that would require further research.
While AAs experienced greater odds of PN status compared to NHWs, there was no significant difference in their receipt of mammogram or Pap screening compared to NHWs in the adjusted models, indicating that navigation was successful for these women, or at least as successful as it was for NHWs. While not considered in the statistical analysis, the success in screening AA women may be due in part to racially and culturally congruent intervention staff able to reach women in their community. This finding demonstrates the success of the intervention considering observational studies that indicate lower breast and cervical cancer screening rates for AA women compared to NHW women after controlling for sociodemographic variables in both urban [9] and rural [7] settings. Other population-based [20] and rural [12] studies point to lower screening rates and later stage breast cancer diagnosis for AA women compared to NHWs.
The results of this study include several limitations. First, the study sample is nonrepresentative as there was a concerted effort to target women who were lower SES and un- or underinsured. There is no way to determine whether the FTF+PN sample is representative of all lower SES and un-/underinsured women in these rural counties. All evaluation instruments recorded information based on self-report with possible recall bias a potential limitation. As noted in Table 1, 35 % of the FTF+PN participants had not completed a follow-up interview, though comparisons of these respondents with those in the follow-up sample did not reveal any substantial differences. Also, program implementation differed in each of the four regions. The role of the patient navigator and cancer prevention program specialist varied by region, and protocols of when and how to follow-up may not have been consistent across regions. Ideally, the study aimed to measure time from FTF participation to screening; however, delays in contracts with providers and protocol variations threatened measurement fidelity of this variable. Finally, we had a very limited measurement of SES (i.e., educational attainment) in our study. We were unable to examine other measures, such as income, wealth, and/or occupational status.
Despite these limitations, the study includes a large sample of women living in rural and border areas within the second largest state by area and population in the USA. Given the large Spanish-speaking population involved in the study, the FTF+PN program and survey materials were available in Spanish. Furthermore, several of the patient navigators and program assistants are bilingual to assist monolingual Spanish speakers and bilingual Spanish speakers with LEP.
The data from the evaluation of FTF+PN lends itself to further analysis in order to determine additional factors that may be related to breast and cervical cancer screening outcomes for this sample. This analysis lays the groundwork for future studies nesting participants by county and region to develop a multilevel model testing the effects of ecological variables on PN participation and mammogram and Pap screening outcomes.
Conclusion
PN is an effective intervention approach to increase breast and cervical cancer screening among women in rural and border Texas. The study’s findings add to the evidence base that demonstrates the positive impact of PN on mammograms and Pap tests in varied settings across the USA. The analyses suggest that FTF+PN successfully captures participants who are underrepresented in breast and cervical preventative screening (rural women, women of color) and suffer poorer cancer-related outcomes.
References
Allen JD, Perez JE, Tom L, Leyva B, Diaz D, Idali Torres M (2014) A pilot test of a church-based intervention to promote multiple cancer-screening behaviors among Latinas. J Cancer Educ 29(1):136–143. doi:10.1007/s13187-013-0560-3
American Cancer Society (2013) Breast cancer: early detection. http://www.cancer.org/acs/groups/cid/documents/webcontent/003165-pdf.pdf. Accessed Sept 20 2013
Ashing-Giwa KT, Gonzalez P, Lim JW, Chung C, Paz B, Somlo G, Wakabayashi MT (2010) Diagnostic and therapeutic delays among a multiethnic sample of breast and cervical cancer survivors. Cancer 116(13):3195–3204. doi:10.1002/cncr.25060
Borrayo EA, Thomas JJ, Lawsin C (2004) Cervical cancer screening among Latinas: the importance of referral and participation in parallel cancer screening behaviors. Women Health 39(2):13–29. doi:10.1300/J013v39n02_02
Carter-Pokras O, Zambrana R, Yankelvich G, Estrada M, Castillo-Salgado C, Ortega A (2008) Health status of Mexican-origin persons: do proxy measures of acculturation advance our understanding of health disparities? J Immigr Minor Health 10(6):475–488. doi:10.1007/s10903-008-9146-2
Centers for Disease Control and Prevention (2013) National breast and cervical cancer early detection program (NBCCEDP). http://www.cdc.gov/cancer/nbccedp/about.htm#1. Accessed Sept 20 2013
Chowdhury R, David N, Bogale A, Nandy S, Habtemariam T, Tameru B (2016) Assessing the key attributes of low utilization of mammography screening and breast-self exam among African-American women. J Cancer 7(5):532–537. doi:10.7150/jca.12963
Davis T, Rademaker A, Bennett C, Wolf M, Carias E, Reynolds C, Liu D, Arnold C (2014) Improving mammography screening among the medically underserved. J Gen Intern Med 29(4):628–635. doi:10.1007/s11606-013-2743-3
Doescher MP, Jackson JE (2009) Trends in cervical and breast cancer screening practices among women in rural and urban areas of the United States. J Public Health Manag Pract 15(3):200–209. doi:10.1097/PHH.0b013e3181a117da
Emery JD, Shaw K, Williams B, Mazza D, Fallon-Ferguson J, Varlow M, Trevena LJ (2014) The role of primary care in early detection and follow-up of cancer. Nat Rev Clin Oncol 11(1):38–48. doi:10.1038/nrclinonc.2013.212
Engelman KK, Cupertino AP, Daley CM, Long T, Cully A, Mayo MS, Ellerbeck EF, Geana MV, Greiner A (2011) Engaging diverse underserved communities to bridge the mammography divide. BMC Public Health 11:47. doi:10.1186/1471-2458-11-47
Farooqi B, Smith B, Chowdhary M, Pavoni S, Modi A, Schnell F (2015) Racial disparities in breast cancer diagnosis in Central Georgia in the United States. J Community Support Oncol 13(12):436–441. doi:10.12788/jcso.0179
Freeman HP (2012) The origin, evolution, and principles of patient navigation. Cancer Epidemiol Biomark Prev 21(10):1614–1617. doi:10.1158/1055-9965.EPI-12-0982
Levy AR, Bruen BK, Ku L (2012) Health care reform and women’s insurance coverage for breast and cervical cancer screening. Prev Chronic Dis 9:E159. doi:10.5888/pcd9.120069
McAlister AL, Perry CL, Parcel GS (2008) How individuals, environments, and health behaviors interact: social cognitive theory. In: Glanz K, Rimer BK, Viswanath K (eds) Health behavior and health education. Jossey-Bass, San Francisco, CA, pp. 169–188
Mills S, Malcarne V, Fox R, Sadler GR (2014) Psychometric evaluation of the Brief Acculturation Scale for Hispanics. Hisp J Behav Sci 36(2):164–174. doi:10.1177/0739986314526697
Nuño T, Martinez ME, Harris R, Garcia F (2011) A promotora-administered group education intervention to promote breast and cervical cancer screening in a rural community along the U.S.-Mexico border: a randomized controlled trial. Cancer Causes Control 22(3):367–374. doi:10.1007/s10552-010-9705-4
Office of Disease Prevention and Health Promotion. n.d. Healthy People 2010. https://www.healthypeople.gov/2010/. Accessed Mar 3 2015
Primeau SW, Freund KM, Ramachandran A, Bak SM, Heeren T, Chen CA, Morton S, Battaglia TA (2014) Social service barriers delay care among women with abnormal cancer screening. J Gen Intern Med 29(1):169–175. doi:10.1007/s11606-013-2615-x
Rao SR, Breen N, Graubard BI (2016) Trends in Black-White disparities in breast and colorectal cancer screening rates in a changing screening environment: the Peters-Belson approach using United States National Health Interview Surveys 2000-2010. Med Care 54(2):133–139. doi:10.1097/mlr.0000000000000450
Roman L, Meghea C, Ford S, Penner L, Hamade H, Estes T, Williams KP (2014) Individual, provider, and system risk factors for breast and cervical cancer screening among underserved Black, Latina, and Arab women. J Women’s Health (Larchmt) 23(1):57–64. doi:10.1089/jwh.2013.4397
Saslow D, Solomon D, Lawson HW, Killackey M, Kulasingam SL, Cain JM, Garcia FAR et al (2012) American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin 62(3):147–172. doi:10.3322/caac.21139
Slater JS, Ha CN, Malone ME, McGovern P, Madigan SD, Finnegan JR, Casey-Paal AL, Margolis KL, Lurie N (1998) A randomized community trial to increase mammography utilization among low-income women living in public housing. Prev Med 27(6):862–870
U.S. Cancer Statistics Working Group (2014) United States cancer statistics: 1999–2011 incidence and mortality web-based report. http://apps.nccd.cdc.gov/uscs/. Accessed Aug 15 2014
U.S. Census Bureau 2016 American fact finder. http://factfinder.census.gov/. Accessed Nov 1 2016
Acknowledgements
The authors would like to thank the team of patient navigators, program specialists, research assistants, and women who participated in the program and its evaluation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the Doctoral Training Grant in Oncology Social Work (125672-DSW-14-115-01-SW) from the American Cancer Society and Evidence-Based Prevention Programs and Services grants (PP120099 and PP150089) from the Cancer Prevention Research Institute of Texas.
Conflict of Interest
The authors report no conflict of interest.
Electronic Supplementary Material
ESM 1
(DOCX 23 kb)
Rights and permissions
About this article
Cite this article
Falk, D., Cubbin, C., Jones, B. et al. Increasing Breast and Cervical Cancer Screening in Rural and Border Texas with Friend to Friend Plus Patient Navigation. J Canc Educ 33, 798–805 (2018). https://doi.org/10.1007/s13187-016-1147-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-016-1147-6