Abstract
Cancer patients are increasingly using the Internet to learn about their disease, connect with others undergoing similar treatments and obtain support outside of the clinical encounter. The goal of this project was to explore how patients with gynecological cancers (ovarian, cervical, and endometrial) used the Internet as an information resource and how this influenced their treatment decisions and interactions with their health care specialists. From 2013 to 2014, ovarian, endometrial, and cervical cancer patients attending a comprehensive cancer centre were invited to complete a 24-item paper questionnaire detailing their experiences in searching the Internet. Twenty-eight patients completed survey. The largest portion of participants had an ovarian cancer diagnosis (61 %), followed by endometrial (29 %) and cervical cancer (11 %). Results indicate that the majority (85 %) of patients used the Internet as a resource to learn about their gynecological cancers. Most respondents (89 %) used Google as their search engine, and some used multiple search engines. The most frequently searched topics included treatment information (85 %), management of symptoms/treatment toxicity (59 %), and alternative treatments (37 %). Many patients (74 %) felt that the Internet was a useful tool for understanding their diagnosis; however, 33 % reported that the Internet was somewhat hard to understand. Most (78 %) patients reported that Internet information increased their understanding of their diagnosis, and 56 % felt it did not affect their decision-making. This study highlights how gynecological patients are accessing cancer information online and how physicians may support this within the clinical setting.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The Internet is becoming an increasingly prevalent tool for patients to access information about their health [1]. It is readily available, supplements information given to them by their physician, and connects them with resources that may not be available within the constraints of an office visit [2]. Patients report that it prompts them to ask questions to their physician that they may not have otherwise considered and clarify information discussed with their health care provider [2, 3].
Upwards of 80 % of patients and caregivers are accessing the Internet to learn more about their health [4]. Cancer patients and caregivers use the Internet to obtain a second opinion, seek information from other patients, learn more about tests and treatments, and raise awareness about specific cancers [4, 5]. Some studies suggest that while patients seek information on the Internet before initiating contact with their physician, this does not impact the emphasis placed on the doctor’s role in prescribing treatment or their trust in their competency [1, 6].
Undoubtedly for cancer patients, the Internet may be an excellent tool for reinforcing information given to them by their health care provider, supplementing gaps in knowledge, and supporting any unmet needs [2, 7]. Despite these benefits, many cancer websites have been shown to have variable content, contain data that is either irrelevant or outdated, and may conflict with treatments recommended by their physicians [6, 7]. More, the websites often require a reading level of grade 11 or higher and may be difficult to navigate [7]. As a result, this breadth of information may result in more confusion than clarification when patients are accessing information about their disease and negatively impact treatment decisions.
In North America, the incidence rate of gynecological cancer (i.e. ovarian, cervical, and endometrial cancers) has increased significantly [8, 9]. The most recent US statistics estimate that 89,060 new cases of gynecological cancers will be diagnosed each year (endometrial 54,870; ovarian 21,290; cervical 12,900), and approximately 28,450 will die of this disease [9]. Based on 2015 estimates, the 5-year survival rate for ovarian, cervical, and endometrial cancer is 45 %, 68 %, and 82 %, respectively. Moreover, although the mortality rate appears to be declining for both ovarian and cervical cancers, the endometrial death rate has increased by 1.9 % each year since 2007 [9].
Despite the prevalence in gynecological malignancies, there has been little research into the informational needs of this patient population. Specifically, there is little information on the use of the Internet as a resource for patients with gynecological cancers and how the Internet influences decision-making. Becoming more familiar with the information patients are seeking regarding their cancer, how their Internet searches support this process, and difficulties encountered will better enable physicians to translate their findings in a meaningful manner. It will also provide guidance on how to best direct patients to online resources that will meet their needs and provide reliable information regarding their gynecological cancer.
The purpose of this study was to characterize the use of the Internet by gynecological cancer patients, identify specific search strategies and patterns used, and describe how this impacted their clinical interactions and treatment decision-making with their specialists.
Materials and Methods
Between 2013 and 2014, patients diagnosed with a gynecological cancer (e.g. ovarian cancer, endometrial cancer, or cervical cancer) and who had seen their oncologist (medical, surgical, or radiation) at the BC Cancer Agency were invited to participate in this study. A database of patients attending the clinic was searched and those eligible for the study were approached during their office visit. Exclusion criteria included patients less than 18 years of age, those unable to provide voluntary consent, and non-English speaking patients. Responses were anonymous and participation was obtained with informed consent prior to completing the survey. Participants were provided with a paper copy of the questionnaire and consent form in addition to a stamped envelope so they would have adequate time to consider their participation and complete the survey. The study was approved by the BC Cancer Agency Research Ethics Board.
The questionnaire consisted of 24 open and closed questions. It was developed based on questionnaires used in previous malignancy studies (e.g. lung, breast, colorectal, melanoma) and has been found to be a reliable assessment of patient Internet use and preferences [10]. The survey included questions with relation to patient demographics (i.e. age, date of diagnosis, and primary malignancy) and Internet use patterns (e.g. overall use of the Internet, use of the Internet as a cancer resource, frequency, and location access). More specific questions detailed Internet search patterns (e.g. reasons for Internet use and search terms used), ease of understanding, and the impact on decision-making. The quantitative data obtained from the questionnaires were evaluated with descriptive statistics. Individual responses were evaluated through a qualitative methodology using a grounded theory approach [11]. Two researchers evaluated the narrative data separately by reading and re-reading the responses, and through a constant-comparison analysis, arrived at a consensus regarding the nature of the responses.
Results
Forty-four subjects diagnosed with a gynecological cancer were approached and agreed to participate in the study (21 ovarian, 14 endometrial, 7 cervical). A total of 28 questionnaires were completed and returned, for a 64 % response rate. Table 1 demonstrates subjects’ demographic characteristics and response based on staging (Table 2).
Twenty-seven (96 %) respondents identified themselves as using the Internet; these patients were described as ‘Internet users.’ Eighteen (67 %) Internet users reported accessing the Internet 1–4 times/day. Most participants (96 %, n = 26) accessed the Internet at home, while ten (37 %) used the Internet at work.
Most respondents (85 %, n = 23) had used the Internet as a gynecologic cancer resource. A small number (7 %, n = 2) had a friend/family member access the information for them. For the four patients that did not access the Internet for information about their cancer described that they do not use the Internet (n = 2), were not sure where to look (n = 2), sceptical of the quality of information available (n = 4), confused/overwhelmed by the information available (n = 2), or were satisfied with the information provided by their healthcare provider (n = 3).
The most common search engine used was Google (89 %), followed by Yahoo (7 %), Bing (4 %), and Pubmed (4 %). Some participants used multiple search engines. When selecting websites to view, half (52 %) chose gynecological websites based on the top hits returned and 48 % because they were associated with a reputable source. Interestingly, only 11 % chose a website that had been recommended by their physician. Over half (63 %) viewed 1–5 gynecological websites during their search, 19 % viewed 6–10 websites, and 7 % viewed 11–15 websites.
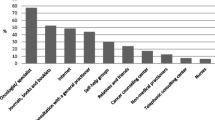
Most patients searched for information regarding gynecological treatment (85 %) and management of symptoms and treatment toxicity (59 %). About a third of patients were interested in prevention methods (33 %), screening (33 %), and alternative/complementary treatments (37 %). Other topics investigated included clinical trials (22 %) and support groups (22 %). The most common search terms included respective cancer names (e.g. ovarian, endometrial, cervical) (70 %) and specific treatments such as chemotherapy, radiation, and hysterectomy (33 %).
Many patients (70 %) viewed institution-based websites (e.g. BC Cancer Agency, Mayo clinic) and less (15 %) viewed general search engines (e.g. Wikipedia, WebMD). Others chose academic sites to supplement their research (11 %). The remaining patients (33 %) could not remember the names of specific websites. The most common websites patients recalled viewing are described in Table 3.
Many patients (63 %) felt that the information provided on the websites was easy to understand, while 33 % reported some difficulty in understanding the material. Interestingly, 63 % of patients did not discuss their findings with their physician. Narrative responses of these patients indicated they had obtained the appropriate information they were looking for (n = 2), the information supported what had been previously discussed with their physician (n = 2), others felt there wasn’t sufficient time to discuss during appointment (n = 2), or their physician wouldn’t be interested/familiar with the details of their findings (n = 3). Of those who did discuss their findings (33 %), their reasons included wanting to clarify information provided by the websites (n = 3), interest in learning more about treatment options not previously discussed (n = 1), and interest in support groups available in the community (n = 1).
To assess the quality of the information available on the Internet, over half (56 %) of patients compared information from credible sources and slightly less (44 %) compared the information available between different websites. Others (26 %) examined the references cited and credentials of the website authors. The same proportion (26 %) discussed the information retrieved from their searches with their family doctor or oncologist.
Most patients (74 %) felt that the Internet was a useful tool for obtaining cancer information and 78 % felt that it increased their understanding of their cancer. More, 56 % felt that the information obtained did not affect their interaction with their oncologist and 26 % indicated that it helped their decision-making. Benefits that were identified as unique to the Internet include ease of access (70 %) and having access to greater volume and detail of information (52 %). Patients also indicated that the anonymity and consideration of different perspectives (37 %) were helpful in their searches.
Some additional themes emerged from the narrative data. Primarily, some patients identified that they were using the Internet for support and ways to cope with the “emotional impact of receiving a cancer diagnosis” and for strategies how to best support their family members/close friends. Others indicated that managing the reaction of their family members ‘was one of the most difficult aspects of the diagnosis’ and were interested in learning about cancer support pages.
Two individuals felt that complementary and alternative treatments for gynecological cancers were poorly represented on government websites, and wished for guidance on nutritional and environmental factors that might contribute to their disease. Finally, one woman identified the search process as being isolating as she was not able to ‘find anyone [with a similar diagnosis].’
Discussion
This study examined how patients with gynecological cancers use the Internet to search for cancer information and its influence on their understanding, treatment decisions, and interactions with their health care specialist. The survey methodology and analysis used for this paper has been validated for previous studies (e.g. melanoma, lung, colorectal, breast cancer) and provides consistency when comparing findings [10, 12].
Almost all of the gynecological cancer patients (96 %) who responded to our survey had used the Internet as a resource. Findings are consistent with the 2013 Canadian Internet use and e-Commerce report that 88 % of Canadian households use the Internet and the growth rate of 3 % has remained relatively stable since 2009 [13]. This is also consistent with US statistics, indicating that 87 % of American adults use the Internet and has been rising steadily since 1997 [14]. This number is slightly higher than in our previous studies (breast cancer, 80 %; melanoma, 93 % were Internet users) [10, 12], but consistent with the rising rates of Internet use among North Americans. The average age range of Internet users in this study was 40–59, slightly lower than in our previous studies of melanoma (average range = 60–79) and breast cancer (average age = 61). This further supports the trend that patients are increasingly likely to access the Internet as a resource when researching their disease.
Most respondents felt that the Internet improved their understanding of their diagnosis, and compared to our prior findings (e.g. melanoma, colorectal), more patients identified the content as easy to understand (63 % in current study vs. 46 % for melanoma and 59 % for colorectal patients). Several reasons may account for these findings. Recent research examined the quality and content of 100 gynecological websites [15] noting the average Flesh-Kencaid readability score of grade 10.3. Prior studies of the reading level of other cancers reveal the average level to be higher [15] and thus the information for gynecologic malignancies may be better aligned with the average aptitude of health consumers [10, 12, 16]. It is also possible that patients are beginning their searches more informed about gynecological health and, therefore, better able to discern useful content on the websites. The increased use of the Internet may also inherently increase patient ease of navigation when searching about their health condition.
The majority of patients indicated that they reviewed 1–5 websites when searching for information about their cancer; however, a portion of patients indicated that they would review 6–10 websites or 11–15 sites. Although we are unaware of any studies assessing the number of websites viewed during each search, studies of patient searching frequency show that patients typically search about their disease once per week for 1 h each session [17]. Interestingly, a review of the current surveys showed that the 11–15 cohort consisted solely of ovarian cancer patients and 80 % of those reviewing 6–10 websites were also ovarian patients. Moreover, all endometrial cancer patients viewed only 1–5 websites. This may reflect the staging of the cancer and relative support needed by these patients. This is congruent with the current findings that a majority of ovarian cancer patients (59 %) in our study were stage IV at the time of survey completion, while cervical and endometrial patients trended towards stages II and II (100 and 76 %, respectively).
On a similar note, 60 % of all returned surveys were from ovarian cancer patients. We surveyed patients at any stage of their treatment in surgical, radiation and medical oncology clinics. To ensure there was no sampling bias, an audit of clinics over a 2-week period during study collection showed a relatively equal number of visits for endometrial (n = 17) and ovarian patients (n = 16) and less cervical patients (n = 7). Although ovarian cancer is a less common malignancy, these patients attend for more cycles of chemotherapy and may attend medical oncology follow-ups more frequently. However, we also conducted the survey in surgical and radiation oncology clinics that treat and follow more cervical and endometrial cancer patients. Thus, in the end, we approached relatively equal numbers of ovarian and endometrial patients. Of the forty-four subjects approached, 21 ovarian, 14 endometrial, and 7 cervical agreed to participate. Thus the frequency of clinic visits did not seem to affect the response rate.
While many websites contain relevant disease information, it is well established that the content is often variable and out of date [18]. This places responsibility on the patient to find information relevant to their diagnosis, interpret their findings in a meaningful manner, and discuss this with their physician. Respondents identified several ways they assessed the quality of information, including accessing websites from credible sources (e.g. academic or government websites), examining cited references and identifying author credentials on the website. Although these are reliable methods of evaluating the quality of online material, this information is often not available [18]. Several guidelines have been established to improve the quality of online health information (e.g. HONcode), however, depend on individual health and not necessarily useful tools for the average reader [19]. More, a recent study of online health information-seeking behaviours in German women indicated that, in absence of objective identifiers of quality, websites that were easy to navigate and aligned more closely with patient beliefs were most likely to be used as a resource [20]. This emphasizes the need for physicians to create an open discussion with their patients about their search patterns, reviewing online material together, and providing their patients with reliable websites they can access.
It is interesting to note the websites patient recall viewing while searching about their cancers. Our previous systematic review of gynecological cancer websites assessed top listings on search engines such as Google [21]. While some of the websites recalled by our study patients (e.g. Wikepedia, WebMD) are congruent with ‘top hits’, the list accessed by our patients includes some additional websites which may not be on a common Google search (e.g. www.bccancer.bc.ca, cancer.ca). This may be that patients are choosing to view websites relevant to their demographic or recall affiliated websites recommended by their oncologist. Patients may also find the general websites difficult to navigate or contain material irrelevant to their searching needs.
The vast majority of patients in this study searched for website information related to treatment (85 %) and management of symptoms/treatment toxicity (59 %). This is consistent with previous findings that cancer patients are most interested in learning about management of their disease and prevention strategies for long-term follow-up [22, 23]. While the majority of Internet users rated information online to be useful and increased their understanding of their disease, less than half considered this information to be influential or helpful in their decision-making. There are several reasons that might account for this discrepancy. There is a general consensus that despite the breadth of health information available on the Internet, patients are still placing emphasis on physician recommendations and trust this over online resources [24, 25]. It may be that patients are able to validate or demystify website findings with their physician, increase confidence in treatment decisions, and develop an improved working relationship. The breadth of information may also be overwhelming or not specific for the needs of the user, and patient preference is to rely on discussions with their physicians.
The goal of this study was to evaluate the Internet search patterns in patients with gynecological cancers. Our study had a good participation rate, and the patients seen at this centre represent a fairly diverse cultural background and age range. However, this study has some limitations. Our sample size was relatively small and the survey was conducted at one institution; therefore, the findings may not be generalizable to all gynecological populations. The returned surveys suffer from selection bias; those who do not use the Internet or do not feel strongly about the survey topics may have been less likely to participate in the survey. Our understanding of patient Internet search patterns are characterized solely by the items elicited on the paper; therefore, there may be other aspects considered to be important by patients that aren’t included on this survey.
In summary, gynecological patients are using the Internet as an information resource and this may impart valuable support outside of the clinical encounter. Characterizing the search patterns and needs of these patients will enable physicians to open discussion regarding their findings on the Internet, clarify ambiguous or false information, and direct their patients to more reliable websites.
References
Shea-Budgell M, Kostaras X, Myhill K, Hagen N (2014) Information needs and sources of information for patients during cancer follow-up. Curr Oncol 21:165–173
Lee K, Kreshnik H, Jeffery H, Lynne E (2014) Dr. Google and the consumer: a qualitative study exploring the navigational needs and online health information-seeking behaviors of consumers with chronic health conditions. J Med Internet Res 16:e262
Sawka A, Straus S, Gafnis A, Brierley J, Tsang R et al (2011) How can we meet the information needs of patients with early stage papillary thyroid cancer considering radioactive iodine remnant ablation? Clin Endocrinol 74:419–423
Goto Y, Nagase T (2012) Oncology information on the Internet. Jpn J Clin Oncol 42:368–374
Hesse B, Nelson D, Kreps G, Croyle R, Arora N et al (2005) Trust and sources of health information: the impact of the Internet and its implications for health care providers: findings from the first Health Information National Trends Survey. Arch Int Med 165:2618–2624
Ziebland S, Chapple A, Dumelow C, Evans J, Prinnjha S et al (2004) How the Internet affects patients’ experience of cancer: a qualitative study. Br Med J 328:564
Selman T, Prakash T, Khan K (2006) Quality of health information for cervical cancer treatment on the internet. BMC Womens Health 6:9
Canadian Cancer Society. 2015. Canadian Cancer Statistics. http://www.cancer.ca/en/cancer-information/cancer-101/canadian-cancer-statistics-publication/?region=on. Accessed 15 June 2015.
American Cancer Society. 2015. Cancer facts and figures. http://www.cancer.org/research/cancerfactsstatistics/. Accessed 16 June 2015.
Ngyuen S, Ingledew P-A (2013) Tangled in the breast cancer web: an evaluation of the usage of web-based information resources by breast cancer patients. J Cancer Educ 28:662–668
McHugh S, Corrigan M, Morney N, Sheikh A, Lehane E et al (2011) A quantitative assessment of changing trends in Internet usage for cancer information. World J Surg 35:253–257
Hamilton, Sarah, Scali, Elena, Yu, Irene, Gusnowski, Eva, Ingledew, Paris-Ann. 2014. Sifting through it all: characterizing melanoma patients’ utilization of the Internet as an information source. Journal of Cancer Education epublication
Statistics Canada. 2014. Canadian Internet Use and e-Commerce in Canada Survey. http://www.statcan.gc.ca/eng/survey/household/4432b. Accessed 12 June 2015
Pew Research Center. 2014. Internet use over time. http://www.pewinternet.org/data-trend/internet-use/internet-use-over-time/. Accessed 16 June 2015.
Ingledew P-A, El-Zammar D, Scali E, Brar B, Lin J et al (2014) Caught in the web: the quality of online resources for cancer patients. Int J Radiat Oncol 90:S604
Harris I (2003) What does “The discovery of grounded theory” have to say to medical education? Adv Health Sci Educ 8:49–61
Castleton K, Fong T, Wang-Gillam A, Waqar M, Jeffe D et al (2011) A survey of Internet utilization among patients with cancer. Support Care Cancer 19:1183–1190
Solomonides A, Mackey T (2015) Emerging ethical issues in digital health information. Camb Q Healthc Ethics 24:311–322
Diviani N, van den Putte B, Stephano G, van Weert J (2015) Low health literacy and evaluation of online health information: a systematic review of the literature. J Med Inf Res 17:e112
Zschorlich B, Gechter D, Janben I, Swinehart T, Wiegard B et al (2015) Health information on the Internet: who is searching for what, when and how? J Evid Qual Health Care 109:144–152
Ann IP, Irene Y (2014) Sifting through it all: the quality of online resources for ovarian cancer patients. Radiother Oncol 1162(s1):66
Ofran Y, Paltiel O, Pellag D, Rowe J, Yom-Tov E (2012) Patterns of information-seeking for cancer on the internet: an analysis of real world data. PLoS One 7:e45921
Metz J, Devine P, DeNittis A, Jones H, Hampshire M et al (2003) A multi-institutional study of Internet ultilization by radiation oncology patients. Int J Radiat Oncol Biol Phys 56:1201–1205
Laugesen J, Hassanein K, Yuan Y (2015) The impact of Internet health information on patient compliance: a research model and an empirical study. J Med Inf Res 17:e143
Chen X, Siu L (2001) Impact of the media and the internet on oncology: survey of cancer patients and oncologists in Canada. J Clin Oncol 19:4291–4297
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McLeod, J., Yu, I. & Ingledew, PA. Peering into the Deep: Characterizing the Internet Search Patterns of Patients with Gynecologic Cancers. J Canc Educ 32, 85–90 (2017). https://doi.org/10.1007/s13187-016-1002-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-016-1002-9