Abstract
Cancer is the second leading cause of death in the USA, but there is minimal data on how oncology is taught to medical students. The purpose of this study is to characterize oncology education at US medical schools. An electronic survey was sent between December 2014 and February 2015 to a convenience sample of medical students who either attended the American Society for Radiation Oncology annual meeting or serve as delegates to the American Association of Medical Colleges. Information on various aspects of oncology instruction at participants’ medical schools was collected. Seventy-six responses from students in 28 states were received. Among the six most common causes of death in the USA, cancer reportedly received the fourth most curricular time. During the first, second, and third years of medical school, participants most commonly reported 6–10, 16–20, and 6–10 h of oncology teaching, respectively. Participants were less confident in their understanding of cancer treatment than workup/diagnosis or basic science/natural history of cancer (p < 0.01). During the preclinical years, pathologists, scientists/Ph.D.’s, and medical oncologists reportedly performed the majority of teaching, whereas during the clinical clerkships, medical and surgical oncologists reportedly performed the majority of teaching. Radiation oncologists were significantly less involved during both periods (p < 0.01). Most schools did not require any oncology-oriented clerkship. During each mandatory rotation, <20 % of patients had a primary diagnosis of cancer. Oncology education is often underemphasized and fragmented with wide variability in content and structure between medical schools, suggesting a need for reform.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cancer and heart disease are by far the two most common causes of death in the USA, with approximately 611,000 deaths from heart disease and 589,000 deaths from cancer per year [1, 2]. Approximately 1.6 million Americans will be newly diagnosed with cancer in 2015, and 14.5 million Americans with a history of cancer will be living [2]. Oncology subspecialists of various types play the largest role in managing cancer, but primary care physicians also play a crucial role in cancer outcomes through their role in prevention, screening, early diagnosis, and the management of issues related to long-term survivorship. The role of primary care physicians may be even greater in medically underserved regions of the country with scarce subspecialty care, as for instance, only 5.5 % of medical oncologists practice in rural areas and one-way travel times to a cancer center exceed 1 h for some segments of the population [3, 4]. As such, adequate oncology education for all medical students regardless of their career aspirations is likely to be beneficial to society as a whole.
Despite the high prevalence of cancer in the USA, the way in which most medical students learn about oncology is not clearly defined. Gaffan et al. published a comprehensive literature review assessing various interventions for teaching oncology to medical students, finding only 48 publications in the medical literature, many of which only address a specific component of oncology education (e.g., communication skills, physical examination for a specific cancer type, cancer prevention, or a summer course) [5]. These studies for the most part also only present descriptive findings, making it difficult to draw definitive conclusions on the efficacy of the tested interventions. Europe and Australia have published on broader curricular guidelines as well as specialized comprehensive classes for select students interested in a career in oncology [6–9], but in the USA, there is no analogous set of consensus guidelines or robust single institution data on which to base the construction of oncology curricula at the undergraduate medical student level [10].
Part of the reason for this may stem from the fact that oncology practice is uniquely multidisciplinary among medical disciplines, providing challenges for educators and administrators alike in cross-discipline organization and development of a comprehensive oncology curriculum. Unfortunately, any lack of communication between educators may lead to inefficiencies, potentially resulting in excessive redundancy or inadvertent omission of content. Furthermore, an imbalance in the curriculum between medical oncology, surgical oncology, radiation oncology, pathology, radiology, and basic science may lead to bias in the material presented or a failure of students to grasp the multidisciplinary nature of cancer care. In addition, a large percentage of cancer patients are managed in the outpatient setting, making it harder for students to take part in their care since the majority of clinical clerkships are inpatient-based. The goal of this study is to characterize how oncology is presented to medical students throughout the USA. This will be assessed by an electronic survey sent to the students themselves. Our goal is to collect information that will be useful both to individual institutions, and also in the potential development of national guidelines for education in oncology.
Methods
An electronic survey was developed by the authors of this paper, in accordance with applicable CHEcklist for Reporting Results of Internet E-Surveys (CHERRIES) criteria [11]. The first page of the survey provided information on the investigator, length of the survey (5–10 min), and purpose of the study. The design of questions and their selection for inclusion was guided by our study group’s clinical and curricular design/teaching experience. The validity of the survey was based on the judgement of our study group, additional medical colleagues, and administrators from the organizations being surveyed. The first section of questions (nos. 1–6) collected demographic information from the participants, including their year in medical school, type of medical school (public or private) they attend, class size, US state of their medical school, whether they have any other advanced degrees, and their likelihood of pursuing an oncologic specialty during residency or fellowship. The second section of questions (nos. 7–13) was a subjective assessment of various aspects of the oncology curriculum at the participant’s school, pertaining to the curriculum’s level of structure, their satisfaction with it, how much they think it could be improved, their personal confidence in various aspects of oncology, and the perceived knowledge of their classmates. Participants were also asked to rank a randomized list of the six most common causes of death in the USA in terms of the amount of curricular time that they felt was devoted to each topic at their school. The third section (nos. 14–23) asked for more objective details about the specifics of oncology instruction during both the preclinical years and mandatory clinical clerkships, assessing the amount of time devoted to oncology didactics, the amount of time spent on specific cancer topics, the type of educators involved, which clinical clerkships are mandatory, and the percentage of patients on a given clerkship with a primary diagnosis of cancer. The survey can be found in Supplementary Fig. 1. Question formats were predominantly multiple choice and Likert scales (from 1 to 5, with 1 being the worst, lowest, or least likely option and 5 being the best, highest, or most likely option, depending on the question). The answer options to multiple choice questions were chosen to be fully inclusive and as unambiguous as possible.
A single survey was disseminated via e-mailbetween December 2014 and February 2015 to two separate groups in two distinct styles: (1) using SurveyGizmo, with the assistance of the Association of Residents in Radiation Oncology (ARRO) committee, to all US medical student attendees of the American Society for Radiation Oncology (ASTRO) 2013 and 2014 annual meetings, and (2) using Google forms, with the assistance of the Association of American Medical Colleges (AAMC) medical student committee, to all current AAMC medical student delegates. The “ARRO” survey uniquely tied the survey link to a given e-mail address to ensure that each participant only filled out a single survey. Up to four weekly e-mail reminders were sent to nonresponders. Individual e-mail addresses were not made available for the “AAMC” survey; as such, the initial survey link and all four subsequent reminder e-mails were sent to the entire list-serve of AAMC delegates. The sample size was 281 for the ARRO survey and approximately 444 for the AAMC survey (calculated as 148 medical schools with approximately three delegates per school).
Participation was voluntary. As an incentive to participate, those who completed the ARRO survey were entered into a raffle to receive a $10 gift card. There was no compensation offered for the AAMC survey. Participants were encouraged to complete every question that they could appropriately answer at their level of training, though they were allowed to skip any questions that they preferred not to answer. Only participants who completed at least 75 % of the questionnaire were included in the subsequent analysis, and only fully completed individual questions for a given participant were included in the analysis of that question. Participants were able to edit or go back to previous questions until the survey was submitted, at which point no further editing was possible. Responses were anonymous, and participants were not asked to report their specific institution.
Descriptive (summary) statistics including mean and standard deviation or median and range were used for the entire population of participants and the two subgroups of participants that completed either the ARRO or AAMC survey. These subgroups were compared using the chi-squared test and two-tailed Student’s t test where appropriate. Likert scales were treated as continuous variables, with two-tailed Student’s t tests used to compare the mean ratings between subgroups. The Friedman test was used to compare ranked items, with post hoc analysis using the Wilcoxon signed-rank tests with a Bonferroni correction. Statistical analysis was performed using Statistical Package for Social Sciences 20.0 (IBM Corporation, Armonk, NY). Unless otherwise indicated, a p value of <0.05 was considered statistically significant. This study was approved by the local institutional review board.
Results
A total 76 responses to the survey were received, 47 from the ARRO survey (response rate 16.7 %) and 29 from the AAMC survey (response rate 6.5 %). Participants represented 28 different states (21 from the ARRO survey and 15 from the AAMC survey), and the average reported age of matriculating students at the represented schools was 24.3 years (1.2). Table 1 shows participant demographics for the entire group and the two subgroups. Those completing the ARRO survey were more likely than those completing the AAMC survey to be further along in their education (p = 0.01), attend a private medical school (p < 0.01), have another advanced degree (p < 0.01), and be pursuing an oncologic specialty during residency or fellowship (p < 0.01). The most common other advanced degrees besides a medical doctorate were a master of science (9.2 %), doctor of philosophy (7.9 %), other (6.6 %), and master of public health (1.3 %).
Participants expressed moderate satisfaction with their oncology education during the first 3 years of medical school (mean Likert score 3.12 (0.94)) and were equivocal regarding whether it could be improved (mean Likert score 3.06 (1.00)). There was no statistical difference between ARRO and AAMC participants in these questions. Among the six most common causes of death in the USA, the most curricular time was thought to be spent on heart disease (mean rank 5.10 (1.68)), followed by cerebrovascular disease/stroke (mean rank 4.06 (1.08)), chronic obstructive pulmonary disorder (COPD)/chronic lung disease (mean rank 3.86 (1.30)), cancer (mean rank 3.38 (1.17)), Alzheimer’s disease (mean rank 2.45 (1.49)), and accidents/trauma (mean rank 2.32 (1.56)). There was a statistically significant difference in these ranks (χ 2(5) = 106.2, p < 0.001). Post hoc analysis using a significance level of p < 0.008 resulted in statistically significant differences between the rankings of all topics except for cerebrovascular disease/stroke and COPD/chronic lung disease (Z = −0.862, p = 0.389), COPD/chronic lung disease and cancer (Z = −1.683, p = 0.092), and Alzheimer’s disease and accidents/trauma (Z = −0.189, p = 0.850).
Based on the first 3 years of medical school, participants were significantly more confident in their knowledge of basic science/natural history of cancer (mean Likert score 3.71 (0.81)) than workup/diagnosis (mean Likert score 3.20 (1.02), p < 0.01), interacting with oncologists (mean Likert score 3.08 (1.14), p < 0.01), and cancer treatment (mean Likert score 2.75 (1.07), p < 0.01). A similar trend was observed for participants’ assessment of their classmates’ knowledge; however, the mean Likert rating of the participants’ own knowledge in all categories was significantly higher than the rating of the classmates’ knowledge (3.18 vs 2.68, respectively, p < 0.01).
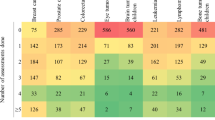
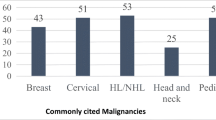
The number of hours of dedicated oncology teaching in each of the first 3 years of medical school is shown in Fig. 1a–c. While a wide range was observed during each year, the most frequently reported amount was 6–10 h during the first year, 16–20 h during the second year, and 6–10 h during the third year of medical school. As demonstrated in Fig. 2, hematologic malignancies received the greatest average amount of teaching time during the preclinical years of medical school (7.8 h (5.4)), followed by breast (5.1 h (4.6)), colorectal (4.8 h (4.1)), lung (4.5 h (3.5)), endocrine (3.8 h (3.3)), gynecologic (3.7 h (3.0)), brain (3.5 h (2.9)), skin (3.1 h (2.4)), pediatric (3.0 h (2.3)), prostate (2.8 h (2.1)), other GI (2.7 h (2.5)), other GU (2.5 h (2.0)), head and neck (2.2 h (2.1)), and sarcoma (2.0 h (1.7)).
The relative degree of involvement of different types of physicians/professors during the preclinical years and mandatory clinic clerkships of medical school are shown in Fig. 3. During the preclinical years, pathologists, scientists/Ph.D.’s, and medical oncologist were reported to do the majority of the teaching, whereas during the clinical clerkships, medical oncologists and surgical oncologists were reported to do the majority of the teaching. Statistically significant differences in the mean Likert rating were observed between all types of professors in the preclinical years except for the difference between medical oncologists and scientist/Ph.D.’s (3.60 vs 3.87, respectively, p = 0.32), and between all types of professors during the mandatory clinic clerkships except for the difference between medical oncologists and surgical oncologists (3.78 vs 3.34, respectively, p = 0.08), radiation oncologists and radiologists (2.03 vs 2.33, respectively, p = 0.18), radiations oncologists and scientist/Ph.D.’s (2.03 vs 1.89, respectively, p = 0.50), and pathologists and radiologist (2.57 vs 2.33, respectively, p = 0.29).
The mean number of months of mandatory clinical clerkships during the third and fourth years of medical school was 14.3 months (7.4), and the mean number of elective clerkships was 5.7 months (2.8). There was no significant difference in the mean number of mandatory or elective clerkships between the ARRO and AAMC subgroups. Table 2 describes the number of months that each of a variety of clerkships are mandatory at participants’ medical schools, the number of hours per week of any type of didactics during each clerkship, the total number of hours of oncology-related didactics during each clerkship, and the approximate percentage of patients with cancer as their primary diagnosis during each clerkship. In summary, there were no mandatory oncology-oriented clerkships at most medical schools. While 4–6 h of didactics per week were most common during the mandatory clerkships, only 3–4 h were typically devoted to oncology didactics during the entire duration of each of the internal medicine and surgery clerkships. The percentage of patients on each clerkship with a primary diagnosis of cancer varied markedly between institutions.
Discussion
As our understanding of human disease expands and treatment paradigms shift, determining the ideal method to educate medical students becomes more challenging, specifically in regard to which elements of complex, multidisciplinary care should receive greatest emphasis in a time-constrained curriculum. It is important to question what medical students need to know at each stage of their education in respect to meeting both academic and clinical benchmarks. Likewise, it is at least equally important to develop a curriculum that provides an adequate foundation to imbue all students with durable knowledge and skills, allowing their development into well-rounded clinicians. Ideally, national standardized examinations would reflect evolutions in practice patterns, but this may not always be the case, and as such medical schools must design curricula that balance the goals of examination preparation and clinical preparation, the latter clearly being more difficult to define. In this study, we have characterized how oncology teaching is perceived by medical students in the USA, and while there appears to be wide variability between institutions, our findings suggest that cancer generally receives less attention and is taught in a more disorganized fashion than is warranted, given its prevalence [1, 2].
The most comprehensively described oncology curriculum in the USA, at least according to the available medical literature, is at Boston University School of Medicine, where a 63-session oncology block during the second year of medical school covers both the scientific and clinical aspects of oncology in approximately equal proportions, and is taught by a variety of professors from several disciplines [10]. This highly organized program addresses many of the shortcomings in oncology education observed in our study. For instance, our data suggests that most students feel more confident in their knowledge of basic science than in workup/diagnosis or treatment, which is most likely due to the fact that most of the instruction in the preclinical years appears to come from pathologists and basic scientists who are often less knowledgeable about the workup and treatment of cancer than oncologic subspecialists. As one participant commented, “Our instruction misses big picture application. We learn a good deal about the pathology/basic science components of oncology, but any practical information (diagnosis/treatment/prognosis) is taught at the clerkship level, where we learn essentially only what is on the shelf exams. I would prefer more clinically oriented oncology instruction.” Involving more clinicians in the preclinical years would provide a more balanced, comprehensive education. Our data also suggest that most students are subject to curricula with some level of fragmentation throughout the first 3 years of medical school, whereas organizing the curriculum into a single block has the distinct advantage of enabling greater efficiency in presenting the material, so that certain topics like prostate and breast cancer are covered more in proportion to their incidence in the population in comparison to less frequent diseases such as hematologic malignancies. In the Metsovo statement, which provided a framework for oncology education in developing countries, a recommendation was made that each medical school assign and fund a designated professor to improve the undergraduate oncology education at their particular school [12]. Given the data collected in this study, a similar approach would appear to be both logical and reasonable to reduce the wide variability in cancer education observed in the USA.
One major challenge of adding a dedicated oncology block to the preclinical curriculum is the time constraint to cover all of the necessary material for the step 1 component of the US Medical Licensing Examination®, which assesses relatively little clinical oncology. As such, another potential solution could be the development of a longitudinal, clinically focused didactic oncology curriculum for all medical students that begins in the second year and extends throughout the third year clerkships, which would complement the fundamentals taught predominantly by pathology and basic science faculty during the second year. Since clinical exposure to cancer patients was highly variable during the mandatory clerkships and an oncology-related clerkship was rarely mandatory, this type of core didactic series covering the aspects of cancer management that are unlikely to be covered during the preclinical years may be particularly useful.
Another concerning finding from our study was the imbalance in the types of clinicians involved in cancer education. For instance, although there are many fewer radiation oncologists at any institution than surgical or medical oncologists, approximately two thirds of cancer patients receive radiation therapy at some point during their illness [13], and as such, it would be beneficial to give students exposure to radiation oncologists during medical school even if they teach more about the basics of clinical oncology than about the specifics of radiation therapy. Interestingly, the lack of radiation oncology involvement was one of the most frequent areas of comment on ways to improve the curriculum amongst both the ARRO and AAMC survey participants. In a health care climate where referral patterns play such an important (albeit unfortunate) role in cancer management [14, 15], it would also be beneficial for primary care physicians to be better educated on the basic conceptual framework of oncologic treatments in order to help ensure that patients are informed of all of the treatment options available to them. More balance is achieved in Europe, as medical oncology is part of the curriculum in 53 % of medical schools, surgical oncology in 60 %, radiation oncology in 80 %, clinical oncology in 93 %, and palliative medicine in 53 % [16]. In the USA, there does not appear to be any lack of interest in radiation oncologist participation in preparing medical students for a career in radiation oncology [17–20] and at some institutions radiation oncology has integrated itself either into the radiology curriculum or oncoanatomy courses [21–23]. However, it is telling that in our study no participant reported a mandatory radiation oncology rotation within his/her school’s curriculum, while we received reports of mandatory medical, surgical, pediatric, and gynecologic oncology rotations at select schools. One would think that radiation oncologists should be particularly adroit educators, given that a higher percentage of medical students with a Ph.D. apply for radiation oncology than any other field of medicine, and their board certification focuses as much on basic science concepts like cancer biology and physics as clinical oncology [24]. However, our findings suggest that it may take extra enthusiasm on the part of radiation oncologists to advocate for the relevance of their material, as well as assistance on the part of administrators to integrate radiation oncologists into a curriculum that may be more naturally accessible to medical and surgical oncologists through their affiliations with internal medicine and general surgery, respectively.
The most important limitation to this study is the self-selection bias inherent to any survey of this nature, in which those who chose to respond may not be representative of the entire population of medical students in the USA. The population of students surveyed through ARRO and the AAMC was chosen largely out of convenience, as they were some of the few groups of medical students whose contact information we could readily access. However, the ARRO group may have been biased by the fact that most of these students will pursue a career in oncology (especially radiation oncology), and the AAMC list may have been biased by the fact that it contained medical students from all years, some of which may not have been fully aware of all aspects of their curriculum yet. It should be noted that though different in their characteristics, both groups responded similarly to the survey questions as a whole. It is also reassuring that our survey captured students from 28 different states, thus reflecting the practices of a variety of schools. Of note, the ARRO survey did also inadvertently capture some first year residents, though we would argue that data from this group should be relatively accurate, as their recall bias would be limited given that they just finished medical school. Other limitations of any self-reported data is that participants may answer questions differently based on their mood, forget relevant details, exaggerate or give the “socially desirable” response even though their answers are anonymous. Another potential source of bias in this study is that we chose to survey students rather than administrators; however, just as patient reported outcomes are oftentimes more accurate than physician reported outcomes, we believe that student reported outcomes on this issue are more likely to be representative of reality. With any survey of this nature there are also limits to the depth of information that can be obtained while trying to keep the instrument as concise as possible, and as such factors like the quality and format of teaching (e.g., lecture-based vs case-based vs ward-based) were not explored in this study, but are worthwhile topics for future exploration. Finally, we are aware that surveying a larger body of students and administrators would be beneficial to confirm our findings, and our research group is currently working towards that end.
Conclusions
This study suggests that most medical students will never do a clinical rotation in oncology and will have disproportionately fewer oncology didactics than other areas of medicine throughout the preclinical and clinical years. In describing the collective views of students from a variety of institutions, we hope to give administrators information to help adapt their individual programs to contemporary practice, and potentially stimulate a national discourse on guidelines for oncology education to help decrease the wide variability in curricula that was observed.
References
Centers for Disease Control and Prevention. Leading causes of death. http://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm. Accessed 26 Mar 2015
American Cancer Society. Cancer facts and figures 2015. http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2015/index. Accessed 26 Mar 2015
American Society of Clinical Oncology (2015) The state of cancer care in America, 2015: a report by the American Society of Clinical Oncology. J Oncol Pract 11:79–113
Onega T, Duell EJ, Shi X et al (2008) Geographic access to cancer care in the U.S. Cancer 112:909–918
Gaffan J, Dacre J, Jones A (2006) Educating undergraduate medical students about oncology: a literature review. J Clin Oncol 24:1932–1939
Tattersall MH, Langlands AO, Smith W et al (1993) Undergraduate education about cancer. A survey of clinical oncologists and clinicians responsible for cancer teaching in Australian medical schools. Eur J Cancer 29a:1639–1642
Oncology Education Committee (2007) Ideal oncology curriculum for medical schools. The Cancer Council Australia
Pavlidis N, Gatzemeier W, Popescu R et al (2010) The masterclass of the european school of oncology: the ‘key educational event’ of the school. Eur J Cancer 46:2159–2165
Pavlidis N, Vermorken JB, Stahel R et al (2012) Undergraduate training in oncology: an ESO continuing challenge for medical students. Surg Oncol 21:15–21
DeNunzio NJ, Joseph L, Handal R et al (2013) Devising the optimal preclinical oncology curriculum for undergraduate medical students in the United States. J Cancer Educ 28:228–236
Eysenbach G (2004) Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 6(3), e34
Pavlidis N (1997) Undergraduate education in oncology in the Balkans and Middle East. The Metsovo Statement, April 4, 1997. Ann Oncol 8:1281
American Medical Association (2014) Physician characteristics and distribution in the U.S. 2014. American Medical Association, Chicago
Noonan K, Tong KM, Laskin J et al (2014) Referral patterns in advanced non-small cell lung cancer: impact on delivery of treatment and survival in a contemporary population based cohort. Lung Cancer 86:344–349
Bekelman JE, Suneja G, Guzzo T et al (2013) Effect of practice integration between urologists and radiation oncologists on prostate cancer treatment patterns. J Urol 190:97–101
The ESMO MOSES Task Force (2008) Medical Oncology Status in Europe Survey (MOSES). European Society for Medical Oncology. http://www.esmo.org/Policy/Recognition-and-Status-of-Medical-Oncology/Status-of-Medical-Oncology-in-Europe. Accessed 26 Mar 2015
Dennis KE, Duncan G (2010) Radiation oncology in undergraduate medical education: a literature review. Int J Radiat Oncol Biol Phys 76:649–655
DeNunzio N, Parekh A, Hirsch AE (2010) Mentoring medical students in radiation oncology. J Am Coll Radiol 7:722–728
Berman AT, Plastaras JP, Vapiwala N (2013) Radiation oncology: a primer for medical students. J Cancer Educ 28:547–553
Agarwal A, DeNunzio NJ, Ahuja D et al (2014) Beyond the standard curriculum: a review of available opportunities for medical students to prepare for a career in radiation oncology. Int J Radiat Oncol Biol Phys 88:39–44
Hansen JT, Rubin P (1998) Clinical anatomy in the oncology patient: a preclinical elective that reinforces cross-sectional anatomy using examples of cancer spread patterns. Clin Anat 11:95–99
Hirsch AE, Handal R, Daniels J et al (2012) Quantitatively and qualitatively augmenting medical student knowledge of oncology and radiation oncology: an update on the impact of the oncology education initiative. J Am Coll Radiol 9:115–120
Zumwalt AC, Marks L, Halperin EC (2007) Integrating gross anatomy into a clinical oncology curriculum: the oncoanatomy course at Duke University School of Medicine. Acad Med 82:469–474
National Resident Matching Program (2014) Charting outcomes in the match, 2014. National Resident Matching Program, Washington, DC
Acknowledgments
The authors wish to thank Cristin Watson, Assistant Director of Education at ASTRO, for her assistance in developing the survey tool, and the entire ARRO executive committee for their support of this project.
Funding
None to report.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 1
(PDF 349 kb)
Rights and permissions
About this article
Cite this article
Mattes, M.D., Patel, K.R., Burt, L.M. et al. A Nationwide Medical Student Assessment of Oncology Education. J Canc Educ 31, 679–686 (2016). https://doi.org/10.1007/s13187-015-0872-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-015-0872-6