Abstract
The burden of cervical cancer is on the increase in sub-Saharan Africa mainly due to inadequate provision and utilisation of cervical cancer prevention services. Several evidence-based strategies have been deployed to improve cervical cancer screening uptake without much success. However, patients’ experiences and satisfaction with service provision has not been adequately studied. Inefficiencies in service delivery and less fulfilling experiences by women who attend cervical cancer screening could have considerable impact in future voluntary uptake of cervical cancer screening. Six hundred and eighty women who underwent Pap smear screening in three health care facilities in two states in south eastern Nigeria were interviewed to evaluate their satisfaction, willingness to undertake future voluntary screening, unmet needs and correlation between satisfaction level and willingness to undergo future screening. Satisfaction with Pap smear screening correlated positively with willingness to undertake future voluntary screening (Pearson’s correlation coefficient = 0.78, P = 0.001). The mean satisfaction score was significantly higher among participants handled by nurses than those handled by the physicians (3.16 ± 0.94 vs 2.52 ± 0.77, P = 0.001). ‘Scrapping discomfort’ of the spatula was reported as the most dissatisfying aspect of Pap smear experience. The need for less invasive screening procedures was the most unmet need. It was concluded that improving the Pap smear screening experience of women and providing less invasive methods of cervical cancer screening with immediate results could improve uptake of cervical cancer screening in south eastern Nigeria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is the fourth most common cancer among women globally with about 528,000 new cases and 266,000 deaths in 2012. In Nigeria, it is the second most common cancer in women after breast cancer with 14,089 new cases and 8, 240 deaths in 2012 [1]. Cervical cancer is one of the very preventable cancers that afflict the human body. It is regarded as a sexually transmitted disease because the sexually transmitted human papilloma virus has been implicated as the causative agent in about 99.7 % of cases [2]. Cervical cancer precursor lesions exist in their pre-malignant stages many years before malignant transformation. These pre-malignant stages are fully detectable and treatable. Detection and treatment of cervical pre-malignant lesions have been the bedrock of cervical cancer prevention for many decades. Cervical smear cytology is the time-honoured method of detecting pre-malignant lesions of the cervix [3].
Cytology-based cervical cancer prevention programmes have proved successful in reducing the burden of cervical cancer in several countries of the world, especially high-income countries [4, 5]. This success story has not been replicated in many resource-constrained countries of the world, especially sub-Saharan Africa, and one of the reasons is the poor uptake of voluntary cervical cancer screening services by the female population in resource-poor countries of the world [5]. The reasons for this poor uptake include poor health-seeking behaviour of the populace, ignorance, poor education, poverty, low status of the female gender, distance, culture and religion [5–9]. Several evidence-based strategies have been deployed to improve uptake in resource-poor settings without much success, and these include reduction in the cost of screening and increasing the awareness of cervical cancer [10, 11]. However, patients’ experiences and satisfaction with service provision has not been adequately studied and relevant evidence-based strategies relating to patients’ experiences and satisfaction with service provision have not been formulated and implemented.
Patient satisfaction with medical services and procedures is viewed as an important aspect of health care delivery. ‘Investigation of patient experiences and preferences provides valuable information that can be fed back to service providers in order to improve service delivery and ultimately improve patient satisfaction and attendance’ [12]. Inefficiencies in service delivery and less fulfilling experiences by women who attend cervical cancer screening could have considerable impact in the voluntary uptake of cervical cancer screening. This is more so in Africa where the prevailing culture is communal in nature. Experiences with health care personnel are easily shared within and outside the community, and this could have potential impact on the voluntary uptake of such services. Anecdotal evidences show that patients referred for Pap smear screening by their physicians express considerable misgivings at such referrals and would rather not go for the test if other options exist. It is very possible that this attitude to Pap smear referral could be borne out of tales from women who had Pap smear test previously. It therefore becomes important to analyse the experiences of women who had Pap smear test in order to address this important question.
A Medline search did not yield any previous studies on the experiences of women undergoing Pap smear cytology in sub-Saharan Africa. This study evaluates the experiences of women undergoing Pap smear cytology in southeast Nigeria and their effects on potential voluntary uptake of Pap smear cervical cytology. It is hoped that the findings of this study will provide valuable information to service providers and policy makers towards improving patient satisfaction and voluntary uptake of cervical cancer screening.
Method
Women attending the cervical cancer screening clinic of the University of Teaching Hospital, Mt Carmel Specialist Hospital, Enugu, Nigeria, and the Federal Teaching Hospital Abakaliki, Ebonyi, Nigeria, between January 2011 and April 2013 were recruited into the survey (Fig. 1). The University of Nigeria Teaching Hospital Enugu and Federal Teaching Hospital, Abakaliki, are government-owned tertiary health institutions while Mt Carmel Specialist Hospital is a private specialist hospital. These centres provide fee-based Pap smear cervical cancer screening and Pap smear specimen obtained mainly by nurses. Trainee gynaecologists and consultant gynaecologists occasionally obtain cervical smear samples. The University of Nigeria Teaching Hospital and Mt Carmel Hospital have a policy of referring every woman who presented to the gynaecological clinic for Pap smear screening irrespective of the patient’s complaints.
The study protocol was reviewed by the Federal Teaching Hospital Medical Research Ethics Board. Sampling was by simple random sampling, using computer-generated random numbers. Women who picked odd numbers were counselled to participate in the study and verbal consents obtained. Women who picked even numbers and those who withheld their consent were excluded from the study. Recruitment was by trained research assistants. The sample size was estimated to be a minimum of 385 using an assumed satisfaction rate of 50 % and sampling error of 5 %. Pre-tested structured interviewer-administered questionnaires containing both open-ended and close-ended questions were used to obtain information. Participants were interviewed after undergoing Pap smear screening test. The questionnaires were primarily based on a previously developed instrument [13]. The final study questionnaire involved modification of the original instrument, based on results of in-depth interviews with non-participating women who had Pap smear cytology test (N = 15). The modified questionnaires were pre-tested for clarity on another set of non-participating women who had Pap smear cytology test (N = 15).
The questionnaires obtained demographic data, Pap smear history and level of satisfaction with care. Satisfaction with care was assessed using a four-point Likert-like scale ranging through very dissatisfied (1), dissatisfied (2), satisfied (3) and very satisfied (4). Participants were asked to state their unmet needs regarding the Pap smear experience. Participants were also asked to indicate the most satisfying and dissatisfying aspects of the Pap smear procedure. Willingness to undertake future voluntary cervical cancer screening was also evaluated using a four-point Likert-like scale ranging through very unwilling (1), unwilling (2), willing (3) and very willing (4). Satisfaction scores were correlated with willingness scores using Pearson’s correlation analysis. Content analysis was done for the verbatim responses to the open-ended questions, and this was done by two independent researchers.
The data were analysed with SPSS version 12.0 using descriptive statistics.
Result
A total of 700 women were approached for participation. Six hundred and seventy-eight women (96.9 %) agreed to participate. Majority of the participants (97.3 %) were referred by physicians. Four hundred and forty-seven (65.9 %) Pap smears were taken by nurses while doctors handled 231 (34.1 %) Pap smears.
The mean age of participants was 43.2 ± 4.1 years (range 25–86). Majority of the participants (53.2 %) were aged 40–49 years. One hundred and thirty-seven respondents (20.2 %) had tertiary education, 441 (65.0 %) had secondary education, 83 (12.2 %) had primary education and 17 (2.5 %) had no education. Some (613, 90.4 %) participants were married, 42 (6.3 %) were widowed, 12 (1.8 %) were single, 6 (0.9 %) were separated and 5 (0.7 %) were separated. Five hundred and fifty-five (81.9 %) participants were multiparous, 81 (11.9 %) were grandmultiparous, 23 (3.4 %) were primiparous and 19 (2.8 %) were nulliparous. More than half of the women (51.3 %) indicated unwillingness to undertake voluntary Pap smear screening in the future. The main reasons for unwillingness are summarised in Table 1.
Only 341 (50.3 %) respondents were satisfied with the overall process of Pap smear cytology. Table 2 shows the reasons for non-satisfaction. Satisfaction with the overall process of Pap smear was correlated positively with willingness to undertake future voluntary screening (Pearson’s correlation coefficient = 0.78, P = 0.001). Almost all the women indicated the willingness to repeat the procedure if so recommended by their physician. The mean satisfaction score was significantly higher among participants handled by nurses than those handled by the physicians (3.16 ± 0.94 vs 2.52 ± 0.77, P = 0.001).
Scrapping discomfort of the spatula was reported as the most dissatisfying aspect of Pap smear experience followed by invasion of privacy. The reassuring attitude of the health staff was reported as the most satisfying aspect of the procedure.
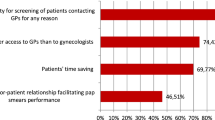
The need for a less invasive screening procedure ranked highest on the unmet needs of the participants (Table 3).
Discussion
This study gives an insight into the experiences of women who undergo Pap smear screening in Nigeria. The positive correlation of satisfaction scores with willingness to undertake future voluntary screening is very instructive. It can be deduced that willingness to undertake voluntary Pap screening is related to the woman’s satisfaction with the process of the previous Pap smear screening. This is in contrast to the findings of a study in a high-income country [14]. This finding is very significant considering the socio-cultural attributes of the study setting. News of experiences of people at health facilities spread very rapidly within communities. The more positive the experience is, the better for the overall population’s acceptance and uptake of the health services.
The findings of this study also indicate a high willingness to undertake Pap screening if recommended by the physician. This is also noteworthy. The lesson here is that while the Nigerian woman is willing to undertake physician-recommended Pap smear screening irrespective of her experience with a previous Pap screen, willingness to undertake future voluntary Pap screen may be related to a satisfactory experience with a previous screen. This demonstrates the enormous role health workers can play in improving the uptake of cervical cancer screening in Nigeria. Making cervical cancer screening an optional but routine investigation for women attending health care facilities in Nigeria can make significant contribution in reducing the cervical cancer burden in Nigeria. This would mean that every health worker should be made to recommend cervical cancer screening for every woman seen in the health facility, while the woman should have the option to opt out of the test [8]. This strategy is currently being used for human immunodeficiency virus (HIV) screening in antenatal clinics in Nigeria, and has recorded tremendous success.
Scrapping discomfort of spatula while taking the Pap smear was reported as the most dissatisfying aspect of the procedure. This points a finger towards the skills of the attending health personnel. Regular training and re-training will improve the skills of health care personnel, reduce the discomfort experienced with the procedure, improve the experience of women undergoing Pap smear screening and improve the voluntary uptake of Pap smear cervical cancer screening.
Invasiveness of the procedure and discomfort associated with it ranked the highest as reasons for unwillingness to undertake future voluntary screening. Many women consider Pap smear as a procedure that invades their privacy. A previous study from a developed country indicated that women generally consider gynaecological examination as embarrassing [15]. The fear of invasion of privacy has also been reported in a previous study as a deterrent for cervical cancer screening in south eastern Nigeria [6]. The need for less invasive methods of screening also appeared top on the unmet needs of the women. This calls for efforts to intensify research on self-collecting and self-testing methods of cervical cancer screening. These self-care methods might receive high acceptability and uptake in low-income settings and has the prospect to improve the uptake of cervical cancer screening.
The need for immediate result of the screening test is worthy of note. A previous study in this setting also reported similar findings [16]. At the moment, visual inspection with acetic acid satisfies the need for immediate result and might find useful applicability in this setting. Future researches should also consider a combination of self-care or self-testing and immediate result. Such a combination may well prove to be the magic wand needed to improve the uptake of cervical cancer screening in low-income populations and ultimately reduce the burden of cervical cancer.
The findings of the study showed better satisfaction with nurses than doctors. Although the reasons for this difference were not directly evaluated in this study, it is possible that the gender of the nurses who were all females could have been contributory. Another important reason could have been the special training giving to nurses who partook in cervical cancer screening. These nurses received post-employment special training on Pap smear sampling while the doctors who were mainly resident doctors were still receiving the training as part of the overall residency training programme. This might be a pointer to the necessity for special training in Pap smear sampling for health workers involved in cervical cancer screening.
In conclusion, willingness to undertake future cervical cancer screening is positively related to the level of satisfaction experienced by the woman in a previous screening. Improving the experiences of women undergoing Pap smear test has the potential to improve the uptake of cervical cancer screening in south eastern Nigeria. Enhancing the comfort and privacy of women during the screening process, reducing the waiting time for procedure and result, proper pre-test education and training more female providers may help to improve the Pap experiences of these women and ultimately improve uptake. These have implications for future screening exercises and research directions.
References
International Agency for Research in Cancer (IARC). Globocan 2012. Available online at http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. Retrieved 07 May, 2014.
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Muñoz N (1999) Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 189(1):12–19
St. Clair C, Wright J (2009) Cervical intraepithelial neoplasia: history and detection. Glob Libr Women’s Med (ISSN: 1756-2228). doi:10.3843/GLOWM.10227. Available online at http://www.glowm.com/section_view/heading/Cervical%20Intraepithelial%20Neoplasia:%20History%20and%20Detection/item/227#24711. Retrieved 12 May, 2014.
Denny L (2012) Cervical cancer: prevention and treatment. Discov Med 14(75):125–131
Denny L, Anorlu R (2012) Cervical cancer in Africa. Cancer Epidemiol Biomarkers Prev 21(9):1434–1438
Chigbu CO, Aniebue U (2011) Why southeastern Nigerian women who are aware of cervical cancer screening do not go for cervical cancer screening. Int J Gynecol Cancer 21(7):1282–1286
Nwankwo KC, Aniebue UU, Aguwa EN, Anarado AN, Agunwah E (2011) Knowledge attitudes and practices of cervical cancer screening among urban and rural Nigerian women: a call for education and mass screening. Eur J Cancer Care (Engl) 20(3):362–367
Dim CC, Nwagha UI, Ezegwui HU, Dim NR (2009) The need to incorporate routine cervical cancer counselling and screening in the management of women at the outpatient clinics in Nigeria. J Obstet Gynaecol 29(8):754–756
Anorlu RI (2008) Cervical cancer: the sub-Saharan African perspective. Reprod Health Matters 16(32):41–49
Obi SN, Ozumba BC, Nwokocha AR, Waboso PA (2007) Participation in highly subsidized cervical cancer screening by women in Enugu, South-East Nigeria. J Obstet Gynaecol 27(3):305–307
Dim CC, Ekwe E, Madubuko T, Dim NR, Ezegwui HU (2009) Improved awareness of Pap smear may not affect its use in Nigeria: a case study of female medical practitioners in Enugu, southeastern Nigeria. Trans R Soc Trop Med Hyg 103(8):852–854
Swancutt DR, Greenfield SM, Luesley DM, Wilson S (2011) Women’s experience of colposcopy: a qualitative investigation. BMC Women’s Health 11:11, Available at http://www.biomedcentral.com/1472-6874/11/11
Bonevski B, Sanson-Fisher R, Girgis A, Perkins J (1998) Women’s experience of having a colposcopic examination: self-reported satisfaction with care, perceived needs and consequences. J Obstet Gynecol 18(5):462–470
Idestrom M, Milsom I, Andersson-Ellistrom A (2003) Women’s experience of coping with a positive Pap smear: a register-based study of women with two consecutive Pap smears reported as CIN1. Acta Obstet Gynecol Scand 82(8):756–761
Szymoniak K, Cwiek D, Berezowska E, Branecka-Wozniak D, Dziobek I, Malinowski W (2009) Women’s opinion regarding gynaecological examination in a hospital. Ginekol Pol 80(7):498–502
Chigbu CO, Onyebuchi AK, Ajah LO, Onwudiwe EN (2013) Motivations and preferences of rural Nigerian women undergoing cervical cancer screening via visual inspection with acetic acid. Int J Gynaecol Obstet 120(3):262–265
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chigbu, C.O., Onyebuchi, A.K., Egbuji, C.C. et al. Experiences and Unmet Needs of Women Undergoing Pap Smear Cervical Cancer Screening: Impact on Uptake of Cervical Cancer Screening in South Eastern Nigeria. J Canc Educ 30, 81–85 (2015). https://doi.org/10.1007/s13187-014-0691-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-014-0691-1