Abstract
Colorectal cancer (CRC) screening and early detection can effectively decrease the morbidity and mortality associated with this disease. Health care providers (HCPs) working in primary care settings as the first contact with the health care system can play a pivotal role in cancer prevention and screening for early detection. The purpose of this study was to explore the knowledge, experiences, and perceived barriers to CRC screening among HCPs working in primary care settings. A cross-sectional design and a self-administered questionnaire (SAQ) was used to collect data from 236 HCPs working in health centers in Jordan. The 236 HCPs were nurses (45.8 %), physicians (45.3 %), and others (7.2 %). A third of the HCPs (30 %) knew the recommended age to begin CRC screening for patients with average risk. Overall physicians scored higher than nurses on questions assessing CRC screening knowledge. The majority of HCPs were not knowledgeable about CRC screening recommendations but believed that CRC is preventable (75.8 %). The main perceived barriers to CRC screening were patient’s fear of finding out that they have cancer and lack of awareness about CRC screening tests, shortage of trained HCPs to conduct invasive screening procedures, and lack of policy/protocol on CRC screening. HCPs working in primary care settings in Jordan do not have adequate knowledge about CRC screening. There is a need for tailored continuing educational programs and other interventions to improve HCPs’ knowledge, as this can increase CRC screening in primary care settings and compliance with current screening guidelines.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cancer is the leading cause of death worldwide and accounts for 7.6 million deaths annually (13 % of all world deaths) [1]. Additional estimates from the World Health Organization (WHO) show that approximately 70 % of all cancer deaths occur in middle- and low-income countries [2–4]. Specifically colorectal cancer (CRC) is the fourth most common type of cancer affecting males and third most common affecting females in the Middle East Region, and is responsible for 9.4 % of the world wide cancers [2–4]. Predictions specific to the Middle East Region indicate that generally countries in this part of the world will experience an increase in cancer mortality of approximately 181 % over the next 15 years [5].
Trends of the past 10 years show that the incidence of cancer in Jordan (a country located in the Middle East Region) is rapidly increasing. In the year 2009, the Ministry of Health in Jordan (MOH) reported that the crude incidence rate of all cancers among Jordanians was 80.2 per 100,000 populations (74.0 for males and 86.9 for females) [6]. More recent reports show that in Jordan, malignant neoplasms are the second leading cause of death and CRC is currently the first ranked cancer among Jordanian males and second commonest among females, with the age adjusted incidence rate of 18.2 per 100,000 and 16.5 per 100,000, respectively [7].
The common risk factors for CRC include dietary practices such as high consumption of fat, red meat, and low consumption of fiber and vegetables [8, 9]. The other risk factors are obesity, smoking, age older than 50 years, lack of exercise, genetic predisposition, including hereditary polyposis and nonpolyposis syndromes, and chronic use of alcohol [6, 7]. Specific diseases such as chronic inflammatory bowel disorders (ulcerative colitis and Crohn’s disease) and diabetes are also risk factors for CRC [9]. All the above factors are common and becoming more prevalent in countries located in the Middle East. The estimated overall prevalence of obesity in Middle East countries is close to 25 % with much higher figures among women (35–75 %) than men (30–60 %) [10, 11]. Therefore, in Jordan, the incidence of CRC is likely to increase even more because of the high prevalence of risk factors mentioned above and others such as diabetes (16 %), obesity or overweight (44.6–64.8 %), and smoking (29 %) [1].
The picture painted by the current cancer incidence rates and prevalence of risk factors highlights CRC as an emerging health problem in the Middle East Region and Jordan. However, this trend can be effectively addressed using proven measures such as screening, early diagnosis, and treatment. There is evidence from clinical studies that CRC screening and early diagnosis can effectively reduce mortality and incidence rates of CRC [12]. The findings of several clinical trials focusing on CRC screening and prevention conducted in developed countries have been recently appraised by international organizations such as the World Health Organization, the American Cancer Society, US Multi-Society Task Force on Colorectal Cancer, the American College of Radiology, and US Preventive Services Task Force (USPSTF) and used to develop evidence-based CRC screening guidelines [13]. The most widely accepted and followed screening guidelines are those of the National Comprehensive Cancer Network (NCCN 2012) [14]. The NCCN offers the most current evidenced-based cancer information to patients and their families and has guidelines which can be utilized by healthcare providers to conduct CRC screening.
The USPSTF (2008) guidelines for CRC screening are also utilized widely in USA and have the following key recommendations for health care providers (HCPs) to follow: (1) CRC screening in average risk women and men should be initiated beginning at age 50 years until 75 years; (2) CRC screening should be done using fecal occult blood testing (FOBT), sigmoidoscopy, colonoscopy, and double-contrast barium enema (DCBE); (3) no routine screening for CRC in adults of age 76 to 85 years; (4) no screening for CRC in adults older than 85 years; (5) intervals recommended for screening tests: FOBT annually, sigmoidoscopy every 5 years with 3-year interval FOBT, and colonoscopy every 10 years. The USPSTF guidelines emphasize prevention and early detection in at risk individuals and making the procedures accessible [15]. When the guidelines are followed and used according to the recommendations, their potential benefits in detecting adenomatous polyps/cancer outweigh the harms or complications [13–15]. In Jordan, the national health authorities have not yet adopted a specific strategy or guidelines to enhance CRC screening despite the high prevalence of the disease in the country. Therefore, lack of specific guidelines about CRC screening could be a significant barrier to CRC screening.
The other barriers to receiving preventive health care services such as CRC screening that have been reported in other settings include financial cost, lack of insurance coverage, fear and discomfort of screening tests, and lack of awareness [16–18]. The lack of awareness can be both by the patient and the health care providers. And for preventive services to be effective, the awareness of health care providers working in primary care settings is very important. HCPs working in primary care settings are uniquely positioned to provide CRC screening and other preventive services through health education, counseling, conducting screening tests, referring patients for advanced care, and follow-up care. In fact, it has been shown that HCP recommendations for CRC screening may be one of most important predictors of patients’ acceptance of screening. However, in order for their contribution to have a significant impact on the trend of CRC, HCPs must have knowledge about the screening tests and procedures, eligibility criteria, and recommended intervals for each CRC screening procedure or test. Studies conducted in developed countries show that HCPs working in primary care settings have knowledge gaps, but those with adequate CRC screening knowledge tend to implement the recommended guidelines and track their patients to ensure receipt of screening [9, 19, 20].
In addition to knowledge about CRC screening guidelines, HCPs may experience other barriers attributable to themselves, the patients, or the health care system and these also affect CRC screening [21]. An emerging body of literature also shows that HCPs with personal experiences such as a family member or patient with CRC tend to follow or recommend such screening to all their eligible patients [22]. The purpose of this study was to explore the knowledge, experiences, and perceived barriers to CRC screening among HCPs working in primary care settings in Jordan. This study focuses on HCPs working in primary care settings because the health professionals working in these settings are more likely to get regular and multiple contacts with clients eligible for CRC screening and therefore likely to have a good understanding of the barriers. The information gained from the HCPs has profound significance in terms of implementation of accessible CRC screening services, enhancing the human resource capacity for cancer prevention, follow-up care for eligible patients, and increasing the community awareness of CRC and screening.
Methods
A descriptive cross-sectional design was used to collect data from HCPs working in comprehensive health centers located in three different geographic areas in Jordan (central, northern, southern). According to recent Jordan population census data, the country has a total population of approximately 7,009,000 million people. Statistics from MOH show that the country has an extensive network of primary health care centers, with about 2.3 centers per 10,000 populations, and with an average patient travel time to the nearest center of 30 min, which represents a high-density system by international standards. The centers are staffed by nurses, physicians, and other categories of HCPs. Fifty percent of Jordanians rely on primary health care centers and clinics for their outpatient health care services. The comprehensive health center provides specialty care in the areas of pediatrics, gynecology, internal medicine, orthopedics, ear nose and throat, ophthalmology, dermatology, and dentistry. Health care at the health centers emphasizes preventive and screening services for communicable and noncommunicable diseases such as cancer, obesity, diabetes, and cardiovascular diseases. Most of these health centers have radiological and laboratory facilities and as the first points of contact in the health care system, they initiate referrals to the local and regional hospitals whenever necessary.
The data for this study was collected from 236 HCPs working in the comprehensive health care centers using convenience sampling strategy. All the HCPs found in each comprehensive health center between December 2012 and May 2013 were approached to participate in the study if they meet the inclusion criteria. In order to participate in the study, a participant had to be a HCP officially employed and directly involved in patient care at the health center and able to read and write English. The HCPs working only with and in clinics caring for only pediatrics and maternity clients were excluded.
Data Collection Questionnaire
A self-administered questionnaire (SAQ) was used for data collection. The SAQ was written in English because all HCPs in Jordan are able to read and write in English. After obtaining approval for the study, the SAQ was given to 10 experts (gastroenterology, nursing, and researcher or statistician) to review it for accuracy and face and content validity. Adjustments based on the experts comments (where necessary) were made. The SAQ was pretested among 30 HCPs working in the family medicine and day care (outpatient sections) at a University Hospital for clarity, logical flow, and time required to respond to all the items. The feedback about the SAQ from experts was mostly about the time required to complete and coding of responses. The SAQ had five sections and a total of 48 items developed by the investigators based on literature and international guidelines for CRC screening. The items in the SAQ about screening interval were based on the intervals of CRC screening tests stated in the ACS and USPSTF guidelines for average risk of adults aged ≥50 years that were current in 2012. The first section of the SAQ asked for data about participants’ demographic characteristics such as age, gender, level of education status, work experience, and marital status. The second section asked for data about participants’ clinical practice setting characteristics such as typical patient load, number of patients paying for their own health care, and frequency of patients of age 50 years and above. The third section elicited data about HCPs’ personal and professional experiences with CRC screening such as having received the test, taking care of patients with CRC, participation in continuing education on cancer prevention, and having ordered, health educated, or referred a patient to get CRC screening.
The fourth section had 13 items, and the first eight formed as scale to measure participants’ CRC screening knowledge. Six (of the eight items) asked about eligibility for CRC screening, procedures used for CRC screening, and the respective recommended time interval for each procedure. Each correct answer on the first six items was scored as “1” and incorrect answer as “0.” The other two knowledge items required the participants to state four common signs and four common risk factors for CRC (each correct sign or risk factor was scored as 0.25). The highest possible score on the knowledge scale is 8. A total knowledge score was constructed by summing all the scores on the eight items. The knowledge scores were categorized as poor knowledge (score = 0.00–3.75), good knowledge (score = 4.00–5.75), and very good knowledge (score = 6.00–8.00). The reliability of the knowledge scale was analyzed in this study and found to be 0.79. The fifth section had a list of 14 patient barriers and system-related barriers. The participants were required to state their opinion whether each is a major, minor, or not a barrier to CRC screening. Participants had a chance to state other barriers to CRC screening that were not part of the list.
Data Collection and Analysis
The study was reviewed and approved by the Institutional Review Board at Jordan University of Science and Technology (JUST) and Ministry of Health. After obtaining approval to conduct the study, the investigators recruited eight research assistants (RAs). The RAs were oriented on the study purpose, procedures, SAQ, research ethics, and consent process. On data collection days RAs went to a specific health center and introduced themselves to the head of the health centers. The RAs were given letters introducing them to the health center. After meeting the administrators, the RAs proceeded to approach available HCPs to explain the purpose of the study. The HCPs who agreed to participate in the study were given the SAQ and consent form to be completed. In cases where the HCP was willing to participate but busy with patient care, a convenient time was arranged to come back and administer the SAQ on the same day. The HCPs were asked to read and sign a consent form before data collection. Participants were provided with an opportunity to ask questions before completing the SAQ. The study did not collect participants identifying information and/or any patient-related information. Data collection from each health center was done in 1 day to reduce the possibility of discussing the contents of the SAQ. Completing and returning the SAQ to the RA was considered as an indicator that the HCP have read the consent form and voluntarily agreed to participate in the study. Data obtained from the participants was analyzed using descriptive statistics and chi-square tests (for categorical variables) to examine if there were any differences in knowledge. The significance level was set at p ≤ 0.05 for all statistical tests.
Results
Characteristics of Health Care Providers Included in the Sample
The detailed characteristics of the 236 participants are presented in Table 1 and show that physicians (45.3 %) and nurses (45.8 %) were equally represented in the sample. The mean age and length of time spent working in health care center by the HCPs was 35.37 and 9.39 years, respectively. The physicians were mostly general practitioners (not specialized = 93.1 %), and the others specialized in family medicine (7.6 %). About 10.6 % of HCPs had been involved in teaching of health professional students from medical schools affiliated with their health center. Approximately, a third of the physicians (31 %) and nurses (29.3 %) reported that they were involved in the care of at least 100 patients during a typical week.
Health Care Providers’ Experiences to CRC Screening
The findings shown in Table 2 indicate that very few HCPs had experience with CRC and CRC screening at a personal or professional level. On a personal level, very few HCPs had a family member who was diagnosed with CRC or had undergone a CRC screening procedure. At the professional level, again the experience of HCPs with CRC and CRC screening was very minimal. For instance, very few had undertaken professional continuing education on cancer prevention/screening or CRC screening education, taken care of patients with CRC, or regularly came across patients diagnosed with CRC in their clinical practice. A large number of HCPs rated themselves as having little experience in working with patients who require CRC screening.
Opinions about CRC Screening
The results presented in Table 3 show that all HCPs had favorable opinions about CRC screening. The majority of HCPs believed that CRC is preventable (75.8 %) and that CRC screening is of benefit to patients (85.6 %) and important (55.5 %). However, half of the HCPs reported that the professional education and training they received did not address or inadequately prepared them to provide cancer prevention and screening services.
Health Care Providers’ Knowledge About CRC Screening
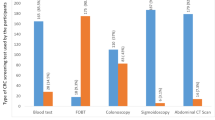
The finding about HCPs CRC screening knowledge are summarized in Table 4 and show that very few knew that ultrasound is not a recommended procedure for CRC screening (25 %), the age at which CRC screening should be initiated in patients of average risk (33.2 %), and age at which CRC screening is not recommended (12.5 %). The majority of nurses (40 %) and physicians (49 %) had poor knowledge about CRC screening and related recommendations. Significantly, more physicians knew the manifestation of CRC and the procedures used for CRC screening. However, there was no significant different between the knowledge scores of nurses and physicians. And when asked which categories of patients they consider as having a high risk for CRC for the purposes of screening, their responses were as follows: 24.6 % identified at least one first degree relative who had a CRC at age less than 50 years, 19.6 % for at least two first degree relative who had CRC diagnosis, 18.6 % a personal history of ulcerative colitis, and an equal number of providers (16.1 %) choose the category of family history of adenomatous polyps (not related to genetic syndrome) and at least one first degree relative who had CRC diagnosis. The HCPs stated that their practices related to CRC screening are mainly very much influenced by the barriers of limited availability of a specialist in cancer (65.3 %), health facility policy on cancer screening (61.9 %), continuing education opportunities on issues related to cancer (59.7 %), regular availability of patients who need cancer screening services (55.5 %), and access to clinical evidence studies published in peer reviewed journals about cancer screening (48.3 %).
Perceived Barriers to CRC Screening
As shown in Table 5, the top three patient barriers to CRC screening as perceived by HCPs were patient’s fear of finding out that they have cancer (68 %), patient’s lack of awareness about CRC screening tests and when those should be done (68 %), and patient’s embarrassment or anxiety about screening tests (56 %). The top three perceived system barriers are shortage of trained health care providers to conduct follow-up invasive procedures (73 %), shortage of trained HCPs to conduct screening (66 %), and lack of policy/protocol on screening (63 %).
Discussion
To our knowledge, this study is the first to explore HCPs’ knowledge, experiences, and perceived barriers to CRC screening in primary care settings in Jordan. The results of the current study show that majority of the HCPs working in primary care settings do not have adequate knowledge about CRC screening but have favorable opinions and attitudes toward cancer prevention and CRC screening. Many of HCPs were not up-to-date with information about CRC screening and specific recommendations for common CRC screening modalities such as FOBT, DCBE, sigmoidoscopy, and colonoscopy. Indeed, the majority of the HCPs reported that they had inadequate preparation with regard to CRC prevention and screening. Similar findings have been reported by studies especially focusing on physicians and have showed that many of them lack proper training and confidence in basic cancer prevention and detection techniques and that most medical students graduate without skills necessary to assist patients in cancer prevention and detection [23–25].
The lack of knowledge about CRC screening in general, and inadequate knowledge about efficacy of specific CRC screening tests such as FOBT, DCBE, sigmoidoscopy, and colonoscopy, has been noted to be a significant barrier that prevents HCPs from recommending specific types of CRC screening tests or procedures or any screening at all [26]. In 2004, O’Malley and colleagues conducted series of focus groups discussion with physicians and patients in primary care clinics in Washington (USA) to examine barriers to CRC screening, and the findings showed that characteristics such as clinician’s recommendations, completion of screening process, and knowledge of CRC screening tests had a major influence on the CRC screening rates [27]. In the current study, when the HCPs were asked if they had ordered or recommended, referred, or health educated a patient about CRC screening, the majority had done none of these actions.
Only a few HCPs were familiar with the guidelines, and their familiarity with the guidelines was not associated with their responses on items of the self-reported screening practices. A large number of the participants stated that they found the guidelines or recommendations of Jordanian MOH to be very helpful and had varied responses on effectiveness of guidelines by ACS and USPSTF. However, the Jordan Ministry of Health has not adopted specific guidelines or recommendation regarding CRC screening, which also shows that HCPs had no adequate knowledge about CRC screening. In this study, very few HCPs knew the risk factors for CRC and only 25.9 % were able to identify family history (genetics) as risk factor for CRC. The HCPs were also not engaged in learning activities to improve their knowledge because only 23.7 % had undertaken professional continuing education on cancer prevention and screening and 5.5 % undertaken CRC screening education specifically. A large number of HCPs rated themselves as having little experience with CRC screening, and this needs to be addressed.
The HCPs reported that the most common factors that influence their practice on issues related to CRC screening are availability of specialists in cancer and having a health facility policy on cancer screening. This shows a window of opportunity which can be utilized to enhance CRC screening. In addition to improving knowledge of HCPs through continuing education programs, having specific health facility policies or protocols and guidelines for CRC screening is likely to enhance CRC screening. Apart from continuing education programs, the knowledge of HCPs about CRC screening can be improved starting from the formal professional training programs. Literatures show that knowledge and attitudes that the students acquired in medical schools or professional training programs significantly affect their professional habits and practice [23].
The main perceived barriers to CRC screening expressed by HCPs were shortage of trained providers to conduct follow-up with CRC screening modalities and patient fear of finding out that they have cancer. These barriers could be partly enhanced by HCPs’ lack of knowledge and inability to explain to patient the benefits of CRC screening, options of screening tests, and associated side effects or nature of the procedures. When the HCPs are knowledgeable about the CRC screening tests, they are likely to encourage more participation and positively influence patient’s uptake of CRC screening. However, the other system barriers reported by the HCPs such as shortage of trained providers/patients follow-up, cost, availability of screening services, lack of setting policy, long-waiting appointments time, and patient load are important and need to be addressed. These barriers have also been reported in other studies. In 2009, Ramos and colleagues reported that the main barriers to CRC screening expressed by the primary care providers were lack of knowledge, lack of time, patients’ fear of invasive feature of colonoscopy, and patients’ lack of perceived benefits of FOBT [26].
The current study is the first one to report about HCPs’ knowledge about CRC screening and perceived barriers to CRC screening in Jordan. However, the findings of the study should be interpreted putting into consideration the limitations of the study such as a small sample size generated by convenience sampling technique, cross-sectional design, collection of data using self-report method, and an SAQ that was not previously tested. Therefore, the findings about HCPs’ knowledge, experiences, and perceived barriers to CRC screening may not be representative of all private and governmental primary care health centers in Jordan. Despite its limitations, the current study highlights some of the major barriers to CRC screening in Jordan which is inadequate knowledge of HCPs. The current study findings suggest that in order to enhance CRC screening in Jordan, there is a need first to increase HCPs’ knowledge about CRC and CRC screening test and procedures. Intervention to increase knowledge and awareness among HCPs and patients about CRC and CRC screening are needed before any population screening-based program is launched. Continuing professional development (CPD) programs for HCPs in primary care settings can be one of the ways used to bridge the existing knowledge and skill deficiencies. The CPD programs are likely to be cost-effective, less time-consuming, and can be implemented close to where the HCPs work in order to prevent lost time away from work. Additionally, curricula used to train HCPs’ need to be updated with specific content about cancer prevention and screening to ensure that graduates have this knowledge and skills before entry into practice. The targeted audience for these programs and courses are the nursing staff, physicians, and other health care providers.
References
WHO (2013). Cancer. Downloaded from http://www.who.int/mediacentre/factsheets/fs297/en/index.htmlon Nov 22nd, 2013
Al-Zahrani AN, Ravichandran K, Al-Madouj AN (2003) Cancer incidence among gulf cooperation council states’ nationals. Riyadh, Saudi Arabia 2008
Jemal A, Siegel R, Ward R, Murray T, Jiaquan Xu J, Thun M (2007) Cancer statistics. CA Cancer J Clin 57:43–66
Vir KR, Gill S, Yoshida E et al (2010) Racial differences in the incidence of colorectal cancer. Can J Gastroenterol 24:47–51
Dey S, Soliman AS (2010) Cancer in the global health era: opportunities for the Middle East and Asia. Asia Pac J Public Health 22(3):75S–82S
Ministry of Health of Jordan (MOH) – (2009) Cancer incidence in Jordan, report of 2008. Non-Communicable Diseases Control Section, Amman, Jordan
National Cancer Registry (NCR) (2009) Cancer incidence in Jordan report of 2008. Non-Communicable Diseases Control Section, Amman, Jordan
Umar A, Greenwald P (2009) Alarming colorectal cancer incidence trends: a case for early detection. Cancer Epidemiol Biomarkers Prev 18:1672–1673
Huxley RR, Ansary-Moghaddam AA, Clifton P, Czernichow S, Parr CL, Woodward M (2009) The impact of dietary and life style risks of colorectal cancer: a quantitative overview of the epidemiology evidence. Int J Cancer 125(1):171–180
Musaiger AO (2004) Overweight and obesity in the eastern Mediterranean Region: can we control it? East Mediterr Health J 10:789–793
Motlagh B, O’Donnel M, Yusuf S (2009) Prevalence of cardiovascular risk factors in the Middle East: a systematic review. Eur J Cardiovasc Prev Rehabil 16:268–280
Klabunde CN, Frame PS, Meadow A, Jones E, Nadel M, Vernon SW (2003) A national survey of primary care physicians’ colorectal cancer screening recommendation and practices. Prev Med 36:352–362
McFarland EG, Levin B, Lieberman DA, Pickhardt PJ, Johnson CD, Glick SN, Brooks D, Smith RA (2008) Revised colorectal cancer screening guidelines. Joint effort of the American Cancer Society, USA
National Comprehensive Cancer Network (2010). NCCN guidelines for patients. Downloaded from: http://www.nccn.org/patients/guidelines/colon/index.html#4
U.S. Preventive Services Task Force (2008) Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 149(9):627–637
Seef L, Nadel M, Klabunde C et al (2004) Patterns and predictors of colorectal cancer test use in the adult U.S. population. Cancer 100(10):2093–2103
Greiner K, Engelman K, Hall M, Ellerbeck E (2004) Barriers to colorectal cancer screening in rural primary care. Prev Med 38(3):269–275
Young W, McGloin J, Zittleman L, West D, Westfall J (2007) Predictors of colorectal screening in rural Colorado: testing to prevent colon cancer in the High Plains Research Network. J Rural Health 23(3):238–245
Hannon PA, Martin DP, Harris JR, Bowen D (2008) Colorectal cancer screening practices of primary care physicians in Washington State. Cancer Control 15(2):174–181
Federici A, Rossi PG, Bartolozzi F, Farchi S, Borgia P, Guastcchi G (2005) Survey on colorectal cancer screening knowledge, attitudes and practices of general practice physicians in Lazio, Italy. Prev Med 41:30–35
Jo AM, Maxwell AE, Rick AJ, Cha J, Bastani R (2009) Why are Korean American physicians reluctant to recommend colorectal cancer screening to Korean American patients? Exploratory Interview findings. J Immigr Minor Health 11:302–309
Guerra CE, Schwartz JS, Armstrong K, Brown JS, Halbert CH, Shea JA (2007) Barriers and facilitators to physician recommendation of colorectal cancer screening. J Gen Intern Med 22(12):1681–1688
Boehler M, Advani V, Schwind C, Wietfeldt E, Becker Y, Lewis B, Rakinic J, Hassan I (2011) Knowledge and attitudes regarding colorectal cancer screening among medical students: a tale of two schools. J Cancer Educ 26:147–152
Garr DR, Lackland DT, Wilson DB (2000) Prevention education and evaluation in U.S. medical schools: a status report. Acad Med 75(7Suppl):S14–S21
Zapka JG, Luckmann R, Rulsky SI, Goins KV, Bigelow C, Mazor K, Quirk M (2000) Cancer control knowledge, attitudes, and perceived skills among medical students. J Cancer Educ 15(2):73–78
Ramos M, Esteva M, Almeda J, Cabeza E, Puente D, Salaich R, Boada A, LIagostera M (2010) Knowledge and attitudes of primary health care physicians and nurses with rgard to population screening for colorectal cancer in Balearic Islands and Barcelona. BMC Cancer 10(500):1–9
O’Malley AS, Beaton E, Yabroff KR, Abramson R, Mandelblatt J (2004) Patient and provider barriers to colorectal screening in the primary care safety net. Prev Med 39:56–63
Acknowledgments
The authors thank the HCPs in primary care settings for participating in this study and Jordan University of Science and Technology for funding support for this study.
Conflict of Interest
The authors declare they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Omran, S., Barakat, H., Muliira, J.K. et al. Knowledge, Experiences, and Barriers to Colorectal Cancer Screening: A Survey of Health Care Providers Working in Primary Care Settings. J Canc Educ 30, 53–61 (2015). https://doi.org/10.1007/s13187-014-0676-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-014-0676-0