Abstract
Studies indicate that women in China are not frequently carrying out breast cancer prevention practices. This is assumed to be due to lack of knowledge and/or lack of personalized instruction. This study was to explore the effect of breast cancer health education on women’s knowledge and attitudes on breast cancer and breast self-examination, behavior related to breast self-examination among women living in the catchment area of a community health center. A pretest and posttest assessment of a 1-h health education session was conducted with 38 participants. A telephone reminder and questionnaires were administered at 1 and 3 months after the education. Three instruments were administered at each contact to assess the knowledge and attitudes on breast cancer and behavior related to breast self-examination and accuracy of breast self-examination before education, 1- and 3-month follow-ups after education. The findings showed the incidence of self-examination, and scores on the accuracy of breast self-examination practice were significantly increased immediately following the intervention and at 1- and 3-month follow-ups. Furthermore, the scores of the health belief regarding perceived benefits, perceived competency, and perceived seriousness significantly improved. The current findings imply community-based intervention could be used to teach women about the general knowledge of breast cancer and how to perform breast self-examination correctly, especially for women who are lack of such information.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Breast cancer is the most prevalent cancer and the leading cause of cancer death among women accounting for 23 % (1.38 million) of the total new cancer cases and 14 % (458,400) of the total cancer deaths in 2008 all over the world [1]. In China, breast cancer has become one of the most prevalent cancers among women, and in recent years, the incidence rate of breast cancer has increased by 3 % per year, higher than the global growth rate [2]. The China Population Association [3] points out that every year, about 20 million females suffer from breast cancer and the mortality rate of breast cancer increases by 38.91 % in urban cities. In Shanghai, Beijing, Tianjin, and Guangzhou, breast cancer is now the most frequently diagnosed among women [4]. The Center of Disease Prevention and Control in Wuhan in 2012 reported that since 2007, breast cancer has ranked first in the female cancer death.
There are three basic methods in diagnosing breast cancer early including breast self-examination (BSE), clinical breast examination (CBE), and mammography [5]. Of the three methods, BSE is highly recommended for all women since it is a simple, very low cost, and noninvasive adjuvant screening method for detection of early breast cancer in women, which can be performed by themselves without any special equipment at home [6]. When women do BSE, they could be aware of the normal look and feel of their breasts and looking for changes in size or shape of their breasts, the presence of lumps, skin dimpling, redness, and discharge [7], potentially making them more aware of breast problems. When performed accurately and regularly, it provides women with the opportunity to notice differences in breast tissue and to detect lumps at an early stage [8]. It is recommended that women should begin BSE when they are in their 20’s since patients diagnosed with breast cancers are getting younger and younger in China with the average age between 40 and 50 years old, nearly 10–15 years younger than women in the Western countries [9].
However, although BSE is an important early-detection tool for women, few people actually examine themselves and the majority of women do not even know how to do BSE [10]. In China, there is limited information about practice of BSE; and in some communities, lots of women do not know the risk factors of breast cancer, the importance of early screening, and the knowledge and skills of BSE [4]. Therefore, it is necessary to implement this study to help community women get the knowledge of breast cancer and BSE.
Methods
Design
This study was a one-group pretest, posttest design.
Setting and Sampling
Participants were recruited by convenience sampling in the Honggang street community in Wuhan, China. Female residents, who aged over 20 years old and had never been diagnosed with breast cancer, were invited to participate in this program.
Sample Size
The sample was calculated based on moderate effect size = 0.4, power = 0.8, and alpha = 0.05 [11]. Using G-Power methods, 52 people were needed for this study. Increasing the failure rate of 15 %, 60 participants were recruited. Finally, 3 months after the education, 38 women finished the whole study. It is shown in Fig. 1.
Instruments
Instruments were used in this study including demographic questionnaire, breast cancer-related knowledge questionnaire, Champion’s health belief model scale [12], and the 14-item BSE checklist.
Demographic Questionnaire
The demographic questionnaire included age, marital status, education level, monthly income, number of children, family history of breast cancer, and sources of information about BSE.
Breast Cancer-Related Knowledge Questionnaire
The breast cancer-related knowledge questionnaire was developed by Chen et al. [2], the original authors at Fudan University in China. It includes three major items, breast cancer risk factors, clinical symptoms, and early screening methods, and there were a total of 17 items with yes and no response options. Then each correct response was scored one point, and each wrong response was scored zero. The total mark was 17 scores. Higher scores indicated better mastery of the knowledge. Internal consistency Cronbach’s alpha coefficient was 0.72 [2]. In this study, the value of Cronbach’s alpha was 0.54.
Champion’s Health Belief Model Scale
The Champion’s health belief model scale (CHBMS) was first developed in 1984 and was revised in later works by Champion in 1993 to measure the health belief model constructs. It is a 35-item about breast cancer and breast self-examination, representing five scales including susceptibility of breast cancer (five items); seriousness of breast cancer (seven items); benefits of BSE (six items); barriers of BSE (six items), and confidence to do the BSE practice (eleven items). It is also a five-point Likert scale ranging from disagreement to agreement; strongly disagreement, disagreement, neutral, agreement, and strongly agreement responses gained 1,2,3,4, and 5 scores, respectively. The CHBMS had been shown to have good internal consistency with Chronbach’s alpha coefficients, 0.93 for susceptibility, 0.80 for seriousness, 0.80 for benefits, 0.88 for barriers, and 0.88 for confidence [12]. Dr. Lu had translated it into Chinese in 2001, and the internal consistency Cronbach alpha coefficient of the Chinese version ranged from 0.78 to 0.91 [13]. In this study, the Chronbach’s alpha coefficients were 0.78 for susceptibility, 0.68 for seriousness, 0.63 for benefits, 0.74 for barriers, and 0.89 for confidence, respectively.
Lashley’s 14 Breast Self-Examination Steps
The 14-item BSE checklist was based on the American Cancer Society and National Cancer Institute recommendations to measure the accuracy of BSE. The BSE test consisted of 14 steps and response choices for each item was yes and no. Scores on the BSE steps range from 0 to 14, with 14 indicating complete performance of all the recommended BSE steps. The Cronbach alpha coefficient was 0.77 [14]. The researcher translated the English scale into Chinese, and another English teacher, an associate professor of Wuhan University, did the back translation. The Chinese version of 14 BSE steps was approbated both by the original author Lashley and Dr. Hu, an associate professor of the University of North Carolina at Greensboro. In this study, Cronbach alpha coefficient was 0.89.
BSE Practice
BSE practice as one of the outcome measures was determined by asking the participants whether they performed BSE last month.
Procedure
Ethics
The study was reviewed and approved by Wuhan University HOPE School of Nursing and the Honggang street community health center in Wuhan. Participants who voluntarily participated in this study would sign written informed consent.
It was a one-group pretest-posttest design, implementing breast cancer health education and BSE training program. Before the intervention, the participants were invited to complete the demographic questionnaire, breast cancer-related knowledge questionnaire, Champion’s health belief model scale (CHBMS), Lashley’s 14 breast self-examination checklists and BSE practice as baseline to evaluate their knowledge, attitudes about breast cancer, BSE practice, and the accuracy of BSE. Then the researcher carried out the breast cancer health education and BSE training. One- and 3-month telephone follow-ups after the intervention, all the participants were asked to finish the same questionnaires again to evaluate the effect of the health intervention. All participants were guaranteed anonymity and separation of questionnaires information from others. It generally took every participant 15 min to finish all the questionnaires.
The intervention included two sessions: health education and a 3-month telephone follow-up.
Health Education
The first component was health education including breast cancer education and BSE training, which was held in the demonstration classroom of Honggang street community health service center. This educational session, a total of six times, focused on 1 h with a maximum of 10 participants each time.
The breast cancer education, lasting about 20 min, involved the prevalence of breast cancer, the characteristics of breast cancer, the risk factors for breast cancer, the early detection methods of breast cancer, the importance of early detection, the signs of breast cancer, and the healthy diet and exercise guidance to prevent breast cancer [15]. During this educational session, teaching methods, for example, PowerPoint presentation, pictures, and examples of case were used.
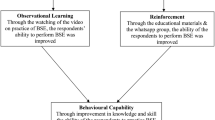
The BSE training, lasting about 30 min, was the BSE step by step instruction. Its contents involved the definition of BSE, the importance and benefit of BSE, and when to do and how to perform BSE, and watching two videos [16] was present to show the steps and technique of BSE. During this educational session, teaching methods, for example, BSE color images, PowerPoint presentation, BSE diagrams, and videos were used. The last 10 min was left to discuss the learning about BSE.
Each participant was given breast health booklet and shower card both made by the investigator.
Three-Month Telephone Follow-up
The second component was monthly telephone follow-up. Through the phone, the researcher asked the participants about the situation of doing BSE. For all of the participants, the researcher recommended them to mark on the calendar or set the phone alert function to help them to remember to do BSE. They were also encouraged to put the shower cards on their shower heads as reminders to perform BSE. Therefore, the telephone follow-up played the role of strengthening and served as a reminder.
Data Analysis
First, descriptive statistical analysis was used to describe the levels of knowledge, attitudes about breast cancer, BSE practice, accuracy of BSE, and demographic data. Second, repeated measure ANOVA analysis and chi-square test were used to compare the differences on the levels of knowledge, attitudes about breast cancer, BSE practice, and accuracy of BSE among participants before education, 1- and 3-month follow-ups after education. The level for statistical significance is p = 0.05.
Results
Demographic Characteristics of Participants
Descriptive statistics of the study participants were displayed in Table 1. Twenty-two respondents were between 40 and 49 years old, accounting for 57.9 %. Thirty-three (86.8 %) respondents were married. Nineteen (50.0 %) received high level of education in universities. Nineteen (50.0 %) had monthly income of less RMB 2,000. Most participants had one child (84.2 %, n = 32). Only 2.6% of the participants had a family history of breast cancer. Four (10.5 %) did not hear of BSE, and 34 (89.5 %) heard of BSE from resources of television, newspaper, the Internet, and health workers.
Comparisons of Knowledge, Attitude, BSE Practice, and BSE Accuracy Before and After Education
The difference of general knowledge, attitudes towards breast cancer, and the accuracy of BSE practice before and after education are displayed in Table 2.
The descriptive statistics of BSE practice frequency were shown that 15 (39.5 %) performed BSE during the last month before education and 1- and 3-month after education, 32 (84.2 %) and 35 (92.1 %) did practice BSE, respectively.
Effect of the Intervention on Knowledge, Attitude, BSE Practice, and the Accuracy of BSE
Repeated measure ANOVA was used to examine changes in the mean scores of knowledge, attitude about breast cancer, and BSE accuracy from baseline to the 3-month follow-up among the participants. The results are presented in Table 3. No significant difference was recorded on the perceived susceptibility and perceived barriers (p > 0.05).
Chi-square test was performed to compare the differences on BSE practice at the three-point time. The finding is found in Table 4. It significantly improved the rate of BSE practice among participants after the education (X 2 = 30.33, p < .001).
Discussion
Knowledge of Breast Cancer
In the present study, knowledge scores about breast cancer were increased significantly 1- and 3-month follow-ups after the intervention. The finding demonstrated that breast cancer health education can improve the level of knowledge about breast cancer. Similar to the finding of other studies, the education highlighted the positive impact of the breast cancer knowledge including symptoms, risk factors, and early screening methods [17–20].
The improvement on knowledge about breast cancer may be attributed to the well-designed intervention. Firstly, this study was 1 h intensive training, consistent with Ludwick and Gaczkowski [21] and Budakoglu et al. [22], which showed that the short and one-time education was highly effective in improving the knowledge on breast cancer. Secondly, in this study, color pictures combination of representative examples and written materials could make participants better informed about the risk factors of breast cancer, the signs of breast cancer, and the benefits of early screening methods. This result was consistent with Leslie et al. [23], who stated that using the video kit was also very useful to improve knowledge about breast cancer, but it is not convenient as written materials.
Attitudes Towards Breast Cancer and BSE
In the current study, the results confirmed health belief in perceived benefits, perceived competency increased, and perceived seriousness decreased after education intervention. These findings indicated that the health education could improve the participants’ attitudes towards breast cancer and BSE.
The susceptibility dimension of CHBMS evaluated the individual perception of possibility of developing breast cancer [24]. In this study, there was no change of perceived susceptibility after education, which is consistent with Hall et al. [25]. However, Lu [13] indicated a decrease of perception of susceptibility to breast cancer after 3 months, and Hacihasanoglu and Gozum [24] showed increase immediately following the education. The explanation for the difference might be due to individual culture differences. In China, some people are tended to attribute the sufferings to one’s fate or the God’s arrangement rather than their physical conditions. Another reason might be that they are confident in their current health condition since in this study, only one person had family history of breast cancer, which may be the reason of participants not perceiving the susceptibility.
In the present study, the finding showed that the perceived seriousness was decreased after education which was different from Moodi et al. [19] and Gürsoy et al. [26]. In the current study, there were two follow-up time periods after education, 1-month and 3-month, while 1 week follow-up of Moodi et al. [19] study and 1-month follow-up of Gürsoy et al. [26] study. This probably results in this dissimilar consequence.
In the study, before the education, most participants believed that breast cancer was serious, but after the 3-month follow-up, participants could perform BSE for several months and they were familiar with their breasts. If they found something unusual, they could get professionals’ help at once which could decrease the perception of seriousness of breast cancer.
Perceived benefits meant refer to the relative subjective effectiveness of BSE in reducing the threat of breast cancer. In the current study, it was demonstrated that perceived benefits of BSE after the education increased significantly, which was in accordance with the result of Hacihasanoglu and Gozum [24], Hall et al. [25], and Liu et al [27]. The reason may be that participants were generally more concerned about the benefits of early detection of cancer, and they were easy to understand. In this study, participants were educated about the benefit of doing BSE through the objective data, cases of example, and videos which could make them aware of the importance of doing BSE. They also realized that if they completed BSE monthly, it can help them to find a lump which might be cancer before it was detected.
Perceived barriers of CHBMS estimated the individual perception of possibility obstacle in adopting health behavior. In this study, perceived barriers were not significant after intervention. This finding corresponded with Hall et al. [25], Moodi et al. [19], and Gürsoy et al. [26]. However, Hacihasanoglu and Gozum [24] and Cohen and Azaiza [28] found that perceived barriers can be decreased after the intervention. Cohen and Azaiza [28] carried out the culture-based intervention which was effective to reduce the barriers of BSE. The one reason, small sample size, may have contributed to the nonsignificance [25]. Lack of awareness about breast cancer and BSE may be the second reason due to attitudinal barriers. Another reason may be due to the forgetfulness of the participants to perform BSE 87 % of the participants aged 30–50 years old who were busy taking care of the whole family and work in the current study, and they could easily forget to perform BSE.
In the current study, the education intervention significantly increased perceived competence of BSE, which is in line with Dündar et al. [29] and Gürsoy et al. [26] highlighting the importance of introducing breast cancer health education to improve confidence. This positive effect may be attributed to the pictures and videos of BSE, which could help the participants get a good direct experience, enhance the correct understanding of the benefits of performing BSE, and hence increase their confidence of doing BSE. Park et al. [30] and Sørensen et al. [31] revealed that utilizing video as well as demonstration and prompt feedback through individualized training strategy provided opportunities for enhancing confidence of BSE.
BSE Practice and Accuracy of BSE
In the present study, the education program significantly increased BSE practice and the accuracy of BSE, which presented the similar findings of Lindberg et al. [32], Öztür et al. [33], Park et al. [30], and Chen et al. [2] owing to the combination of BSE demonstration and telephone follow-up. The telephone follow-up played the role of reminders to remind the participants performing BSE. In this study, every participant received a 3-month telephone follow-up and they could insist on doing BSE monthly. Secondly, shower card posted on the bathroom could also serve as a role of reminder when the participants took a shower in the present study. Thirdly, videotaped education on BSE was feasible and effective in enhancing participants’ adherence to BSE and facilitating the accurate procedures about BSE. Watching video on BSE could encourage participants to perform accurately and master the key steps of practicing BSE. Liu et al. [27] and Lindberg et al. [32] believed that silicone breast model used for BSE practice was an effective way to increase mastery of BSE.
In short, the findings of this study indicated that an education program about breast cancer and BSE not only improved the knowledge, attitude about breast cancer, and BSE but also increased BSE practice and accuracy.
Limitation and Future Research
There were several limitations in this study. First, the sample size was small, which limited the power to explore the health education on knowledge, the health belief variables, and practice. Furthermore, a convenience sample could cause bias. Second, it was only a one-group education without a control group. Third, participants were selected only in one community health service center. Future research should consider recruiting a larger sample through random sampling in more communities with a control group.
Clinical Implication
This study would provide community health nurses with evidence to implement effective breast cancer health education. Community-based intervention with group education strategy could be used to teach women about the general knowledge of breast cancer and how to perform BSE correctly, especially for young women who are lack of such information.
Conclusion
In conclusion, the health education intervention increases the knowledge about breast cancer, positive health belief regarding breast cancer and BSE, and practice and accuracy of BSE among community women. However, more evidence should be needed to decrease the barriers and hence increase the frequency of doing BSE.
References
Jemal A, Bray F, Center M, Ferlay J, Ward E, Forman D (2011) Global cancer statistic. CA Cancer J Clin 61(2):69–90
Chan SS, Chow DM, Loh EK, Wong DC, Cheng KK, Fung WY (2007) Using a community-based outreach program to improve breast health awareness among women in Hong Kong. Public Health Nurs 24(3):265–273
China Population Association (2010) Available from: http://lxjk.org/details.asp?classid=1&id=157. Accessed 12 Dec 2010
Liu CY, Xia HO, Isaman DM, Deng W, Oakley D (2010) Nursing clinical trial of breast self-examination education in China. Int Nurs Rev 57:128–134
American Cancer Society (2006) American Cancer Society Guidelines for the Early Detection of Cancer, 2006. Retrieved from: http://CAonline.AmCancerSoc.org. Accessed 6 Mar 2011
Shalini, Varghese D, Nayak M (2011) Awareness and impact of education on breast self examination among college going girls. Indian J Palliat Care 17(2):150–154
Cancer Council Australia (2004) Position statement: early detection of breast cancer. Available from: http://www.cancersa.org.au/cms_resources/PS-Early_detection_of_breast_cancer_reviewed_May04_updated_Jun09.pdf. Accessed 8 Jan 2011
Memis S, Balkaya NA, Demirkiran F (2009) Knowledge, attitudes, and behaviors of nursing and midwifery students regarding breast self-examination in Turkey. Oncol Nurs Forum 36(1):39–46
Zhao YL (2005) Evaluating the effect of health education of 1215 women about breast cancer with health belief model. Chin J Nurs 41(8):683–686 (In Chinese)
Simi A, Yadollahie M, Habibzadeh F (2009) Knowledge and attitudes of breast self examination in a group of women in Shiraz, Southern Iran. Postgrad Med J 85(1004):283–287
Alkhasawneh IM, Akhu-Zaheya LM, Suleiman SM (2009) Jordanian nurses’ knowledge and practice of breast self-examination. J Adv Nurs 65(2):412–416
Champion VL (1993) Instrument refinement for breast cancer screening behaviors. Nurs Res 42:139–143
Lu ZJ (2001) Effectiveness of breast self-examination nursing interventions for Taiwanese community target groups. J Adv Nurs 34(2):163–170
Lashley ME (1987) Predictors of breast self-examination practice among elderly women. Adv Nurs Sci 9(4):25–34
Hao M, Ma XJ (2010) Handbook of knowledge and treatment of breast cancer. Shandong Science and Technology Press (In Chinese)
Bickley L (2008) Bates’ Guide to physical examination and history taking. (9th ed). Lippincott Williams & Wilkins
Yousuf SA (2010) Breast cancer awareness among Saudi nursing students. JKAU Med Sci 17(3):67–78
Soyer MT, Ciceklioglu M, Ceber E (2007) Breast cancer awareness and practice of breast self-examination among primary health care nurses: influencing factors and effects of an in-service education. J Clin Nurs 16:707–715
Moodi M, Mood MB, Sharifirad GR, Shahnazi H, Sharifzadeh G (2011) Evaluation of breast self-examination program using health belief model in female students. JRMS 16(3):316–322
Hanan M, Ola A, Hala K (2009) Impact of a health education intervention. Program about breast cancer among women in a semi-urban area in Alexandria, Egypt. J Egypt Public Health Assoc 84(1):219–243
Ludwick R, Gaczkowski T (2001) Breast self-exams by teenagers: outcome of a teaching program. Cancer Nurs 24(4):315–319
Budakoglu I, Maral I, Ozdemir A, Bumin A (2007) The effectiveness of training for breast cancer and breast self-examination in women aged 40 and over. J Cancer Educ 22:108–111
Leslie NS, Deiriggi P, Gross S, DuRant E, Smith C, Veshnesky JG (2003) Knowledge, attitudes, and practices surrounding breast cancer screening in educated Appalachian women. Oncol Nurs Forum 30(4):659–667
Hacihasanoglu R, Gozum S (2008) The effect of training on the knowledge levels and beliefs regarding breast self-examination on women attending a public education center. Eur J Oncol Nurs 12:58–64
Hall CP, Hall JD, Pfriemer JT, Wimberley PD, Jones CH (2007) Effects of a culturally sensitive education program on the breast cancer knowledge and beliefs of Hispanic women. Oncol Nurs Forum 34(6):1195–1202
Gürsoy AA, Yiğitbaş C, Yilmaz F, Erdöl H, Bulut HK, Mumcu HK (2009) The effect of peer education on university students’ knowledge of breast self-examination and health beliefs. J Breast Health 5(3):135–140
Liu CY, Yu MY, Zhao YL, Song LX (2006) Evaluating the effect of health education of 1215 women about breast cancer with health Belief model. Chin J Nurs 41(8):683–686 (in Chinese)
Cohen M, Azaiza F (2010) Increasing breast examinations among Arab women using a tailored culture-based intervention. Behav Med 36(3):92–99
Dündar PE, Özmen D, Öztürk B et al (2006) The knowledge and attitudes of breast self-examination and mammography in a group of women in a rural area in western Turkey. BMC Cancer 6(43):1–9
Park S, Song HY, Hk H, Kim G (2009) Effects of a cognition-oriented breast self-examination intervention for Korean women and their spouses. Public Health Nurs 26(3):259–268
Sørensen J, Hertz A, Gudex C (2005) Evaluation of a Danish teaching program in breast self-examination. Cancer Nurs 28(2):141–147
Lindberg NM, Stevens VJ, Smith KS, Glasgow GE, Toobert DJ (2009) A brief intervention designed to increase breast cancer self-screening. Am J Health Promot 23(5):320–323
Öztürk M, Engin VS, Kisioglu AV, Yilmazer G (2000) Effects of education on knowledge and attitude of breast self examination among 25+ years old women. East J Med 5(1):13–17
Acknowledgments
We would like to thank Dr. Jie Hu, an associate Professor of University of North Carolina at Greensboro School of Nursing, USA, for the expertise in checking the instrument translation. We are especially grateful to all who participated in this study. This study could not have been possible without their assistance.
Conflict of Interest
There is no conflict of interest.
Funding Statement
This research received no specific grant from any funding agency.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ouyang, YQ., Hu, X. The Effect of Breast Cancer Health Education on The Knowledge, Attitudes, and Practice: A Community Health Center Catchment Area. J Canc Educ 29, 375–381 (2014). https://doi.org/10.1007/s13187-014-0622-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-014-0622-1