Abstract
Colorectal cancer is the second most common cause of death in the USA. The need for screening colonoscopies, and thus adequately trained endoscopists, particularly in rural areas, is on the rise. Recent increases in required endoscopic cases for surgical resident graduation by the Surgery Residency Review Committee (RRC) further emphasize the need for more effective endoscopic training during residency to determine if a virtual reality colonoscopy simulator enhances surgical resident endoscopic education by detecting improvement in colonoscopy skills before and after 6 weeks of formal clinical endoscopic training. We conducted a retrospective review of prospectively collected surgery resident data on an endoscopy simulator. Residents performed four different clinical scenarios on the endoscopic simulator before and after a 6-week endoscopic training course. Data were collected over a 5-year period from 94 different residents performing a total of 795 colonoscopic simulation scenarios. Main outcome measures included time to cecal intubation, “red out” time, and severity of simulated patient discomfort (mild, moderate, severe, extreme) during colonoscopy scenarios. Average time to intubation of the cecum was 6.8 min for those residents who had not undergone endoscopic training versus 4.4 min for those who had undergone endoscopic training (p < 0.001). Residents who could be compared against themselves (pre vs. post-training), cecal intubation times decreased from 7.1 to 4.3 min (p < 0.001). Post-endoscopy rotation residents caused less severe discomfort during simulated colonoscopy than pre-endoscopy rotation residents (4 vs. 10 %; p = 0.004). Virtual reality endoscopic simulation is an effective tool for both augmenting surgical resident endoscopy cancer education and measuring improvement in resident performance after formal clinical endoscopic training.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical trainees need to learn a basic set of endoscopic skills to perform screening colonoscopy and an even more complex set of skills for therapeutic or hybrid surgical procedures, such as natural orifice transluminal endoscopic surgery [1]. Mastery of such endoscopic skills requires both technical as well as cognitive skill sets [2]. A construct-validated virtual reality (VR) simulator may verify actual endoscopic skill acquisition and augment traditional endoscopic training. With the onset of the new fundamentals of endoscopic surgery (FES) requirement for general surgery residents, enhancing endoscopic skill acquisition will become increasingly important.
Recent studies have shown that the traditional method of acquiring endoscopic skills via an apprenticeship model can be enhanced with the use of endoscopic VR simulation [3]. The augmentation of skill acquisition during training expedites an endoscopist’s mastery of basic techniques in addition to decreasing hospital costs [4]. Simulated experiences must first be shown to have construct validity (demonstrate the ability to measure their designed purpose accurately). While the Immersion Medical Endoscopy Accutouch System (AccuTouch) has been validated on novice GI fellows, its efficacy at detecting differences in surgical residents has yet to be demonstrated [5].
In this study, we sought to determine if the AccuTouch VR simulator could discriminate between surgical residents before and after 6 weeks of formal clinical endoscopic training.
Material and Methods
Second to fifth year surgical residents performed multiple simulated colonoscopy scenarios on the AccuTouch system over a 5-year period from 2007 to 2012. Procedural data from the residents were stored and analyzed retrospectively. Residents were subdivided into two groups: “novice” endoscopists, who had undergone no formal training and “experienced” endoscopists, who had a 6-week endoscopy rotation. During the endoscopy rotation, residents were trained in the traditional apprenticeship model in both upper and lower endoscopy by an experienced gastroenterologist. Residents averaged 80–100 endoscopy cases per rotation. Institutional Review Board (IRB) approval with waiver of consent was obtained prior to the initiation of the study.
The AccuTouch is a VR colonoscopic model simulator that features a combination of a model endoscope for manual manipulation along with high-fidelity computer graphics, realistic environment simulation (scope angulation, air insufflation, variable lens conditions, aspiration), complex haptic feedback (independent force feedback with patient tube insertion and twist), and real-time dynamic modeling of colonic deformation (looping, insufflation). Performance metrics during each clinical scenario were recorded by the AccuTouch and include total procedure time, time to cecal intubation, amount of red-out (time that the lens is obscured by contact with mucosa), and patient discomfort level. Simulation scenarios are categorized in three case categories (introduction, biopsy, polypectomy) and ranked by increasing technical difficulty. Residents would complete 2–3 scenarios from each of the three categories during their simulator sessions. The average number of simulator encounters for residents having received endoscopy training was eight: four before and four after their endoscopy rotation. For those residents who did not undergo endoscopy training, two endoscopy sessions comprised of four simulator encounters each took place, on average, 6 months in between each encounter.
The primary endpoints were time to cecal intubation, red-out time, and the number of times the simulation patient experienced mild, moderate, severe, and extreme pain. A non-paired student’s t-test was used to compare cecal intubation times between novice and experienced residents. A paired student’s t-test was used to compare residents’ performance before and after their endoscopy rotation. Patient discomfort levels were grouped into two broader categories: mild and moderate versus severe and extreme. Patient discomfort scores were analyzed by chi-square analysis.
Results
During the 5-year study period, 94 residents underwent evaluation via VR colonoscopic simulation. The majority (64 %) of residents received no previous endoscopy training during the study period. Most residents were in their third year of clinical training during their simulator course. There was an equal split between second and fifth year residents (Table 1).
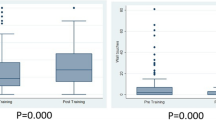
Cecal intubation times were significantly shorter in the experienced residents (4.4 vs. 6.8 min, p < 0.001). Experienced residents also spent less time in “red-out” as compared with their untrained counterparts (p < 0.001). Rates of patient discomfort were significantly higher in the novice residents as compared with experienced residents when simulated pain events were grouped into a mild-moderate and extreme-severe group and compared with one another (10 vs. 4 %, p < 0.001), (Table 2). Fourteen residents completed the simulator exercises before and after their endoscopy rotation. When compared against themselves, these residents demonstrated statistically significant improvement after their formal endoscopy training: cecal intubation times decreased from 7.1 to 4.3 min (p < 0.001).
Discussion
Endoscopic skills have now become an essential component of a general surgeon’s practice. Colonoscopy constitutes up to 8 % of all rural general surgeons’ case volume [6]. With the recent increase in the minimum number of endoscopic cases required by the Accreditation Council for Graduate Medical Education (ACGME) for graduating general surgery residents to 85 (35 upper endoscopies and 50 colonoscopies), the needs for improving colonoscopy training and for finding a validated means of measuring endoscopic competency have become increasingly important [7]. Our study shows that VR endoscopy simulation is a sensitive tool for detecting differences in skill level between novice and experienced surgical resident endoscopists. This is consistent with previous studies examining the training of gastroenterology residents; however, to date, there is no data describing the role of endoscopy simulation in surgical resident education [3, 5, 8–11].
For all examined metrics, including time to cecal intubation, red-out time, and patient discomfort levels, those general surgery residents who had undergone a 6-week endoscopic rotation outperformed surgical residents with no formal training. This observation is supported by Grantcharov et al. [11], who showed that experienced endoscopists, when compared with novice endoscopists, were faster, saw a greater degree of mucosal surface area, had less “red-out” time, and produced less local colonic wall pressure on VR simulators. While it can be reasonably anticipated that those who have undergone formal instruction will have a higher level of technical competency, this initial advantage may diminish if a sufficient degree of simulation experience were obtained by their colleagues. This was demonstrated by Cohen et al. [2], who showed that simulator-trained GI fellows had a higher overall competence for the first 80 clinical cases; however, both simulator and non-simulator trained fellows required the same number of cases (mean, 160) to obtain a 90 % competency level during real colonoscopies. The average improvement in performance between novice and experienced residents of 2.4 min was obtained after an average of 80–100 endoscopy cases obtained during their endoscopy rotation. These findings agree with Marshall et al. [12], who found that roughly 100 endoscopy cases were needed to obtain a 75 % competency rate in GI fellows.
Our finding of a decrease in patient discomfort from 10 to 4 % of the time is consistent with previous studies demonstrating that VR simulation training leads to decreased simulated patient discomfort [13]. This improvement in simulated patient findings corroborates subjective reporting from real patients as well. Ahlberg et al. [14] found that real patients rated those gastroenterology fellows who had first undergone VR simulation prior to the patient’s colonoscopy as causing significantly less pain than their counterparts who had no prior VR training. These findings suggest that parameters used by the VR simulators can be translated into real patient scenarios.
While our study demonstrated that resident performance improves after endoscopic training and that VR simulators are sensitive enough tools to detect those differences, the role of VR simulation as an educational adjunct versus replacing traditional endoscopic training remains unclear. A large Cochrane meta-analysis by Walsh et al. [15] involving 13 randomized trials with 278 participants concluded that VR endoscopic simulation conveyed a competency advantage on those who had it versus those who did not (assuming all participants had little prior endoscopy experience). Ritter et al. [16] suggest that VR simulation can additionally be used to predict those trainees who will require further adjuncts to their training due to lack of fundamental visuospatial and psychomotor abilities.
There were three major limitations in our study. First, at the beginning of the study, the four scenarios done by experienced residents were not the same as the four by the novice residents. Those scenarios performed by the experienced residents were considered harder than those performed by the inexperienced group. One would expect less improvement in cecal intubation time in a harder scenario. Despite this, our study still found improvement in cecal intubation time. To improve comparison in the later part of the study, the scenarios done by both groups were the same. Second, to demonstrate the validity of this simulator, experienced endoscopists, e.g. practicing colorectal surgeons or gastroenterologists, would be required to perform all four scenarios to establish simulator benchmarks. While there were no expert endoscopists included in this pilot study, we are currently accruing data from their performance on our simulator for subsequent studies. Finally, in this retrospective study, we could not assess the impact that endoscopy simulation had on resident performance during real clinical colonoscopies while on their endoscopy rotation. It should also be noted that our study was limited to the use of the AccuTouch simulator, while the GI Mentor simulator is the simulator used during the fundamentals of endoscopic surgery.
Conclusion
With the incorporation of FES into general surgical training, the need for increasingly sophisticated ways of demonstrating clinical competency will be required. Additionally, with increasing hospital costs and resident work hour restrictions, finding more cost-effective and efficient ways of augmenting traditional endoscopic training will become increasingly important. Larger, more uniform, prospective trails with concurrent “gold standard” validation are needed to clarify the role and efficacy that VR simulators will play in the future of surgical education or even potentially testing competency in recertifying general surgeons. Our study supports the use of VR endoscopy in objectively and safely measuring the ability of a surgery resident to perform colonoscopy.
References
Sugden C, Aggarwal R, Banerjee A, Haycock A, Thomas-Gibson S, Williams CB, Darzi A (2012) The development of a virtual reality training curriculum for colonoscopy. Ann Surg 256(1):188–192
Cohen J, Cohen SA, Vora KC, Xue X, Burdick JS, Bank S, Bini EJ, Bodenheimer H, Cerulli M, Gerdes H, Greenwald D, Gress F, Grosman I, Hawes R, Mullin G, Schnoll-Sussman F, Starpoli A, Stevens P, Tenner S, Villanueva G (2006) Multicenter, randomized, controlled trial of virtual-reality simulator training in acquisition of competency in colonoscopy. Gastrointest Endosc 64(3):361–368
Plooy AM, Hill A, Horswill MS, Cresp AS, Watson MO, Ooi SY, Riek S, Wallis GM, Burgess-Limerick R, Hewett DG (2012) Construct validation of a physical model colonoscopy simulator. Gastrointest Endosc 76(1):144–150
McCashland T, Brand R, Lyden E, de Garmo P (2000) The time and financial impact of training fellows in endoscopy. CORI Research Project. Clinical Outcomes Research Initiative. Am J Gastroenterol 95(11):3129–3132
Sedlack RE, Kolars JC (2003) Validation of a computer-based colonoscopy simulator. Gastrointest Endosc 57(2):214–218
Sariego J (2000) The role of the rural surgeon as endoscopist. Am Surg 66(12):1176–1178
Spier BJ, Durkin ET, Walker AJ, Foley E, Gaumnitz EA, Pfau PR (2010) Surgical resident’s training in colonoscopy: numbers, competency, and perceptions. Surg Endosc 24(10):2556–2561
Desilets DJ, Banerjee S, Barth BA, Kaul V, Kethu SR, Pedrosa MC, Pfau PR, Tokar JL, Varadarajulu S, Wang A, Wong Kee Song LM, Rodriguez SA (2011) Endoscopic simulators. Gastrointest Endosc 73(5):861–867
Sedlack RE, Kolars JC (2002) Colonoscopy curriculum development and performance-based assessment criteria on a computer-based endoscopy simulator. Acad Med J Assoc Am Med Coll 77(7):750–751
Koch AD, Haringsma J, Schoon EJ, de Man RA, Kuipers EJ (2008) A second-generation virtual reality simulator for colonoscopy: validation and initial experience. Endoscopy 40(9):735–738
Grantcharov TP, Carstensen L, Schulze S (2005) Objective assessment of gastrointestinal endoscopy skills using a virtual reality simulator. JSLS : J Soc Laparoendosc Surg/Soc Laparoendosc Surg 9(2):130–133
Marshall JB (1995) Technical proficiency of trainees performing colonoscopy: a learning curve. Gastroint Endosc 42(4):287–291
Sedlack RE, Kolars JC (2004) Computer simulator training enhances the competency of gastroenterology fellows at colonoscopy: results of a pilot study. Am J Gastroenterol 99(1):33–37
Ahlberg G, Hultcrantz R, Jaramillo E, Lindblom A, Arvidsson D (2005) Virtual reality colonoscopy simulation: a compulsory practice for the future colonoscopist? Endoscopy 37(12):1198–1204
Walsh CM, Sherlock ME, Ling SC, Carnahan H (2012) Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy. Cochrane Database Syst Rev 6, CD008237
Ritter EM, McClusky DA 3rd, Gallagher AG, Enochsson L, Smith CD (2006) Perceptual, visuospatial, and psychomotor abilities correlate with duration of training required on a virtual-reality flexible endoscopy simulator. Am J Surg 192(3):379–384
Acknowledgments
Study Design: Lu
Data Collection: White
Statistical Analysis: White
Manuscript Drafting: White, Vetto, Lu
Critical Revision of the Manuscript: Buchberg, Vetto, Herzig, Tsikitis, Lu
Study Supervision: Lu
Ian White had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
White, I., Buchberg, B., Tsikitis, V.L. et al. A Virtual Reality Endoscopic Simulator Augments General Surgery Resident Cancer Education as Measured by Performance Improvement. J Canc Educ 29, 333–336 (2014). https://doi.org/10.1007/s13187-014-0610-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-014-0610-5