Abstract
Understanding women’s psychological barriers to getting Papanicolaou (Pap) screening has potential to impact cancer disparities. This study examined pain perceptions of Pap testing among black, Latina, and Arab women and goal setting to receive Pap tests. Data on 420 women, in a longitudinal study, were analyzed using Chi-square tests of differences and generalized linear mixed models. At baseline, 30.3 % of black and 35.5 % of Latina women perceived Pap tests to be very painful compared to 24.2 % of Arab women. Perceptions of pain influenced goal settings, such as scheduling a first ever Pap test (odds ratio = 0.58, 95 % confidence interval 0.14–0.94). Immediately following the intervention, women’s perception that Pap tests are very painful significantly declined (P value <0.001) with Arab and black women registering the greatest improvements (20.3 and 17.3 % reduction, respectively, compared to 8.4 % for Latina). Having the perception that the Pap test is very painful significantly reduces the likelihood of black, Latina, and Arab women setting the goal to schedule their first ever Pap test. Latina women are the least likely to improve their perception that the Pap test is very painful, though national statistics show they have the highest rates of morbidity and mortality from cervical cancer. These findings are instructive for designing tailored interventions to break down psychological barriers to Pap screening among underserved women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer ranked 13th as the most common cancer among US women in 2005 [1, 2], and in 2011, the American Cancer Society [3] predicted that over 12,000 new cases of invasive cervical cancer would be diagnosed with 4,290 deaths resulting from cervical cancer. It is well established that the majority of invasive cervical cancer cases occur among inadequately screened women [4] and that timing of screening is crucial for early detection, which in turn is crucial for survival [5]. A major factor associated with earlier diagnosis is use of available early detection (screening) services such as the Papanicolaou (Pap) test, which is the universally endorsed screening method for cervical cancer. To be most effective, women must receive the Pap test on a regular basis, in adherence to clinically recommended guidelines. This may require women to purposely set goals to receive regular Pap tests and follow through on their commitments. While steady declines in cervical cancer mortality rates have been recorded in the last 50 years, largely due to efficacy of early detection and screening with the Pap test, considerable gaps persist in early detection, morbidity, and mortality among racial and ethnic minorities, with black and Latina women carrying the heaviest burdens [6–9].
Black women experience higher morbidity and mortality due to invasive cervical cancer compared to white women [2], and this disparity increases with age [7]. Black women are also twice as likely to die of cervical cancer compared to white women [10]. A recent national study [9] mapping the cervical cancer burden in the USA also found that Latina women had increased incidence of cervical cancer compared to white non-Hispanic women and were diagnosed at a younger median age. The same study found increased rates of cervical cancer among black women compared to white women, and black women were diagnosed at an older median age compared to white women. To a large extent, poverty and low socioeconomic status are the overriding factors that limit access to cervical cancer screening and treatment services for black and Latina women [3]. However, other factors including psychological barriers such as the perception of pain or personal experiences during a Pap test can potentially affect women’s screening behaviors [7, 11].
The status of cervical cancer screening and barriers to early detection among Arab women in the USA are understudied, yet Arabs constitute one of the fastest growing racial–ethnic populations in the nation. According to the US census data, the population claiming Arab ancestry stood at about 1.2 million in 2000 with large concentrations in metropolitan areas such as New York, NY, Los Angeles, CA, and Detroit, MI [12]. More recently, the 2008 American Community Survey [13] shows Michigan’s Arab population at approximately 500,000, with nearly half residing in Detroit. Given the increase in the Arab population and the lack of large sample studies that include Arab women as a separate ethnic group, understanding their cervical cancer screening behaviors and barriers is imperative.
In a pilot study, Matin and LeBaron [14] include Arab Muslim women and highlight that when it comes to gynecologic care, Muslim women often feel threatened by the American healthcare system’s broad screening guidelines because they lack sensitivity towards Islamic values and customs. Similarly, traditionalism and degree of acculturation have been shown to significantly influence Pap testing among Arab women [15]. The 2008 Michigan Special Cancer Behavioral Risk Factor Survey found that 73.3 % of Arab American women 40 years of age and older received an appropriately timed Pap exam, which is lower than the statewide average of 79.0 % [16], suggesting disparities in cervical cancer screening. Since census statistics do not allow analysis of Arab Americans since they have been historically categorized as part of the “non-Hispanic whites,” it is difficult to gather a complete picture of Arab women’s health. The current study makes a contribution by including Arab women and treating them as a separate ethnic group. By analyzing their perceptions of pain associated with the Pap test together with those of black and Latina women, the study provides new evidence on the psychological barriers to cervical cancer screening in diverse racial–ethnic groups. The study also analyzes how the perceptions of pain affect women’s personal goal setting to receive future Pap tests.
Methods
This manuscript represents a discrete study associated with a larger study, Health Disparities: Survey Validation for Black, Latina, and Arab Women, that received human subjects’ approval from the Michigan State University Institutional Review Board in November 2008, when the U.S. Preventive Services Task Force guidelines recommended Pap testing every 1–3 years depending on risk.
Research Design and Setting
The data analyzed were collected in the context of the Kin KeeperSM Cancer Prevention Intervention in partnership with the Detroit Department of Health and Wellness Promotion and the Arab Community Center for Economic and Social Services. Kin KeeperSM is a home-based education intervention that can be described by the human ecological framework, which views an individual woman, her health, and the health of her family within the context of the physical, psychological, social, and cultural environments [17]. While described in detail elsewhere [17], in brief, the Intervention utilizes black, Latina, and Arab community health workers (CHWs) affiliated with a non-cancer public health program, e.g., a maternal–child health program. The CHWs recruit women (aged 21–70) of their respective race–ethnicity from their public health program caseload. After the client signs the informed consent, she becomes a kin keeper and assembles her female adult family (any combination of mother, daughter, grandmother, sister, aunt) for a home education visit. During the visit, participants complete a sociodemographic form, a pre/post Cervical Cancer Literacy Assessment Tool (C-CLAT) and a personal action plan. Participants also use the personal action plan to set cervical cancer screening goals after receiving the intervention. All the material is read aloud by the CHW for women to follow, and individuals complete their forms in their language of choice. Latina and Arab CHWs are bilingual and administer the education intervention in the participant’s preferred language.
Data and Variables
The analysis was based on a sample of 420 women (185 black, 128 Arab, and 107 Latina) who responded to the question, “Getting a Pap test is very painful, TRUE or FALSE?” as part of the C-CLAT administered at three different times (baseline, posttest 1, and 12-month follow up posttest 2). Data from the personal action plans were also used to generate the outcome variable on goal setting to receive a Pap test: (a) “Find a healthcare provider to do first ever Pap test”; (b) “Schedule first ever Pap test”; and (c) “Continue getting yearly Pap test”. These goals were viewed as the three major steps towards adherence to clinically recommended cervical cancer screening. As such, an ordinal outcome variable ranging from 1 to 3 was constructed representing these three steps, with “Continue to getting a yearly Pap test” being the highest third-level goal, “Schedule first ever Pap test” being the second/middle level, and “Find a health care provider to do first ever Pap test” being the first level of the ordinal variable.
In setting their Pap test goals, women could have selected all three applicable goals listed in their personal action plans or provided an alternative goal of their own not listed. Thus, some women had multiple cervical cancer screening goals implying that the outcome variable constructed assumed that a woman who set a higher-step goal (continue Pap testing) would be more advanced in her empowerment and ability to overcome psychological barriers to screening than one who only set a first-step goal. The ordinal dependent variable was based on the highest-step goal selected by a woman in her personal action plan. Thus, if a woman set all three goals, she was considered as being at the third step although she was yet to achieve her first step of finding a healthcare provider to do her first ever Pap test.
To control for relevant covariates, standard sociodemographic variables were included in the multivariate analysis: the women’s age in years, annual income category, highest level of education attained, marital status, health insurance status, and employment status. Additional variables included are the women’s self-rated health status and self-reported family history of cancer, which was defined as whether a woman’s family had a history of breast cancer (FHC + breast), a history of other cancer (FHC + other), or no family history of cancer (FHC−). These were included because a previous research has shown these variables to predict women’s cervical cancer screening behaviors [18–20].
Statistical Analysis
To test reliability of the outcome variable, we computed the Cronbach alpha statistic. While the three separate goals are not items of a scale measuring an underlying construct, we performed the reliability analysis because we considered them as measuring three levels of the stages in goal setting towards regularly receiving a Pap test in compliance with clinically recommended guidelines.
Descriptive statistics by race–ethnicity and corresponding Chi-square tests of associations were calculated. Similarly, descriptive statistics of the women’s responses to the Pap pain question were tested for differences between race–ethnicity and over time. For example, the percentage difference between the baseline and posttest 1 response of black women was tested to evaluate if the change over time was statistically significant.
In order to analyze how women’s perception that the Pap test is very painful influenced their cervical cancer screening goal setting decisions, we estimated generalized linear mixed models for ordinal response variables (proportional odds model with random effects) and for binary variables (logistic regression with random effects) [21, 22]. Generalized linear mixed models are well-suited for analyzing multilevel and longitudinal data that have correlation [23]. Given that the women were clustered within families, we estimated two-level models with family-level random effects. We used the likelihood ratio tests to select the best fitting models, whose results are reported in this manuscript. All statistical analyses were performed using SAS statistical software, version 9.2, with the generalized linear mixed models being fitted using the PROC NLMIXED statement [24].
Results
Results of the reliability analysis of the outcome variable show that the Cronbach’s alpha statistics is 0.72 (average inter-item covariance = 0.037). This is with the third item reverse-coded because it would be expected that the third-level goal signifies aspirations to adhere to regular Pap testing while the other two goals do not. This result implies internal consistency of the outcome variable that was used in the multivariate analysis.
Table 1 summarizes the sociodemographic characteristics of the women sampled and shows that there were significant differences across the three racial–ethnic groups. Results on the women’s perceptions of pain from getting a Pap test are presented in Table 2. Before the intervention, 30.3 % of black and 35.5 % of Latina women perceived the Pap test to be very painful compared to 24.2 % of Arab women. Post intervention, the number of women responding “TRUE” to the same pain statement declined significantly among black and Arab women (P values <0.001). However, the decline among Latinas was not statistically significant suggesting that Latina women have greater psychological barriers that prevent them from viewing the Pap test as not very painful.
Unexpectedly, the percentage of women who answered TRUE during the 12-month follow up (posttest 2) was significantly higher than the percentages observed in posttest 1 for all racial–ethnic groups, with black women actually recording a higher percentage than in the baseline (36.2 % in posttest 2 compared to 30.3 % at baseline).
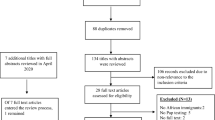
Compared to the baseline results, Arab women showed the largest improvement in their response to the pain question, having the smallest percentage of women that answered “TRUE” in posttest 1 and posttest 2 (3.9 % and 14.8 %, respectively). Moreover, results show Arab women as being the only group to register a significant decline between baseline and the 12-month follow up (P = 0.051). These findings imply that there are significant racial–ethnic differences in whether women perceive the Pap test to be very painful or not, not only in the baseline but also after the same education intervention has been delivered (tests of differences across race–ethnicity yield P values <0.001 in both posttest 1 and posttest 2). The percentages of women who set different Pap screening goals are depicted in Fig. 1. Racial–ethnic differences in the Pap screening goals set were significant, with more Arab women setting the third step goal: continue to get a yearly Pap test (94.3 %). Black women, on the other hand, had the highest percentage, setting the goal to find a healthcare provider; while Latina women, who set to get their first ever Pap test, had the highest percentage (12.9 %). These results are consistent with national statistics that show Latina women as having higher cervical cancer incidence and mortality rates.
Results of the generalized linear mixed models are shown in Table 3. Four sets of results are presented, with the generalized linear mixed model for ordinal responses shown in the second column (model 1) followed by the results of the binary responses shown in the last three columns (models 2 to 4). In the binary response generalized linear mixed models, each screening goal (step) was treated as a separate independent goal and estimated separately. However, it is likely that these response variables are not independent, hence the reformulation of the variables to form a single ordinal response which is modeled in model 1.
Model 3 results suggest that women who do not perceive the Pap test as being very painful are nearly 50 % more likely to schedule their first ever Pap test (odds ratio = 0.58; CI 0.14–0.94). Since a majority of these women would have already received their first ever Pap test, their goal was much higher: that of continually receiving a yearly Pap test (adherence). While only significant at the 10 % alpha level, model 1 seems to support this finding, showing that women who do not perceive a Pap test to be very painful have a higher likelihood of setting a higher-level goal in general (odds ratio 2.01, 95 % confidence interval 0.98–4.10).
This appears to be especially the case among Arab women who, at the 10 % significance level, were more likely to set goals to receive a yearly Pap test than black and Latina women (OR = 2.95, 95 % CI 0.82–10.62). Age was also found to be a significant predictor, with older women less likely to set a lower-level Pap screening goal (model 3 result: schedule first ever Pap test, OR = 0.74, 95 % CI 0.58–0.93). This result on the marginal effect of age is quite expected and consistent with the well-established evidence that older women are more likely to have received a Pap test before, but, as they get older, they are less likely to continue receiving a yearly Pap test [15]. Of note is that while the age-squared variable was significant in almost all models, its magnitude was very small. Thus, non-linearity in the age effect is negligible and barely increases the likelihood of setting a higher-level goal.
Family history of cancer was found not to be significant at the 5 % level (model 4: odds ratio = 0.06, 95 % CI 0.00–0.82), suggesting that women with a family history of cancer are more likely to have already received a Pap test and thus set a higher goal to continue getting yearly Pap test (model 1: odds ratio = 4.86, CI 0.89–26.64). Overall, the findings suggest that the perception that the Pap test is very painful is more likely to deter women from setting the goal to schedule their first ever Pap test but is not a significant predictor of the other goals (find a healthcare provider or continue getting a yearly Pap test).
Discussion
This study assessed black, Latina, and Arab women’s perceptions of pain due to the Pap test in order to better understand psychological barriers to cervical cancer screening among medically underserved women. These findings are similar to those of Hoyo et al. [7] that focused only on black women and found them to be less likely to adhere to Pap screening guidelines if they perceived the Pap test as painful; yet the current study advances the literature by also including the perspectives of Latina and Arab women. The finding that perceived pain has the potential to deter women from setting a lower-level goal of scheduling a first ever Pap test brings into focus a vulnerable area with regards to a woman proactively accessing the healthcare system and being receptive to cancer education messages. In effect, a woman who perceives the Pap test as very painful may be more apt to disregard cervical cancer screening recommendations and educational messages, thus deterring her from taking the crucial step in cervical cancer prevention, scheduling the screening test. The concern about pain has been identified in the literature as a barrier among other groups as well as limiting follow up of an abnormal Pap test in Latinas, implying that breaking down the barrier of perceived pain is important to increase cervical cancer screening among diverse groups of women [25]. There is potential for women who set higher-level goals to serve as educators and facilitators of knowledge regarding the Pap test and their experience to women considering having their first ever Pap test.
The current study also assessed women’s perceptions of pain due to the Pap test over time, before and after the Kin KeeperSM Cancer Prevention Intervention. Immediately after receiving the intervention, the percentage of women who perceived the Pap test as very painful significantly decreased, especially among the Arab and black women. The percentage of Latina women who perceived the Pap test as very painful also declined; however, this was to a lesser extent suggesting that Latina women have stronger psychological barriers to overcome the perception that the Pap test is very painful. This finding may be a result of cultural nuances that are specific to the Latina community or unique challenges and experiences that Latina women face when engaging with the healthcare system. Additional study analyzing the link between personal experiences of women with the healthcare system and their perception of pain could further illuminate the issue to enhance interventions designed to break down psychological barriers to Pap screening.
The surprising result that even after the one-time education intervention all women regress towards their baseline perceptions of pain associated with the Pap test over a year’s period implies that concerted long-term efforts are needed for interventions to be effective at breaking down psychological barriers to Pap screening. The findings also suggest that women’s perceptions about pain from a Pap test may evolve differently over time, potentially reinforced or transformed by personal experiences and interaction with the healthcare system all of which are likely different for each racial–ethnic group.
Limitations of the current study include the use of a single measure to assess the complex psychological issues of perception of pain related to cervical cancer screening and the lack of data on women’s personal experiences and interaction with the medical healthcare system that could influence goal setting and screening behaviors. Future research is needed to develop scales that better measure women’s psychological barriers to cervical cancer screening. Also, detailed analyses of women’s history of interactions and personal experiences with the healthcare system could be informative and help understand the dynamics involved in goal setting and adhering to clinically recommended cervical cancer screening guidelines. Nevertheless, a crucial contribution of this study is the inclusion of Arab women together with black and Latina women, who encompass both growing and established racial–ethnic populations in the USA.
Conclusion
Perceived pain from the Pap test is more likely to serve as a barrier to women setting the lower-level goal of scheduling their first Pap test rather than the higher-level goal of maintaining yearly Pap screening. This finding underscores the importance of designing interventions that specifically educate women who have never received a Pap test about the Pap test procedure and instruments used, as well as educating healthcare providers about women’s attitudes and beliefs regarding the Pap test, and useful communication techniques to allay women’s discomfort during a Pap test.
Racial and ethnic differences play a significant role in women’s perceptions of pain from the Pap test, even after educational interventions are implemented. Since there appears to be a stronger psychological barrier to overcome with regards to pain and Pap screening among Latinas specifically, future research should investigate cultural factors that may impact Latina women’s experience with Pap screening. Additionally, knowledge reinforcement about the Pap test must occur over time to ensure knowledge retention and prevent unintended psychological barriers from resurfacing between interventions. Further exploration in order to elucidate the degree to which perceived pain functions as a psychological barrier among black, Latina, and Arab women will advance efforts to circumvent non-adherence to cervical cancer screening guidelines among medically underserved women.
References
Jemal A, Siegel R, Ward E et al (2008) Cancer statistics, 2008. CA Cancer J Clin 58:71–96. doi:10.3322/CA.2007.0010
Jemal A, Thun M, Ries L et al (2008) Annual report to the nation on the status of cancer, 1975–2005, featuring trends in lung cancer, tobacco use, and tobacco control. J Natl Cancer Inst 100(23):1672–1694
American Cancer Society (2011). Cancer Facts & Figures 2011. http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-029771.pdf
Agency for Healthcare Research and Quality. 2008. Cancer screening and treatment in women: recent findings. http://www.ahrq.gov/research/cancerwom.htm#intro
Hakama M, Miller AB, Day NE (eds) (1986) Screening for cancer of the uterine cervix: from the IARC working group on cervical cancer screening and the UICC project group on the evaluation of screening programmes for cancer. Oxford University Press, New York
Jemal A, Thomas A, Murray T et al (2002) Cancer statistics, 2002. CA Cancer J Clin 52:23–47. doi:10.3322/canjclin.52.1.23
Hoyo C, Yarnall KSH, Skinner CS et al (2005) Pain predicts non-adherence to pap smear screening among middle-aged African American women. Preventive Medicine 41:439–445
Morbidity and Mortality Weekly Report (MMWR). Cancer Screening—United States, 2010. Center for Disease Control and Prevention. December 2012, Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6103a1.htm?s_cid=mm6103a1_w
Watson M, Saraiya M, Benard V et al (2008) Burden of cervical cancer in the United States, 1998–2003. Cancer 113:2855–2864. doi:10.1002/cncr.23756
National Cancer Institute (2009). SEER cancer statistics review 1975–2007. Bethesda, MD Retrieved from http://seer.cancer.gov
Jennings-Dozier K (1999) Predicting intentions to obtain a Pap smear among African American and Latina Women: Testing the theory of planned behavior. Nurs Res 48(4):198–205
de la Cruz GP, Brittingham A. The Arab population: census 2000 brief. December 2003, US Census Bureau
American Community Survey. 2008. Selected population characteristics & interactive map. Demographics data from the Arab American Institute. December 2012, Retrieved from http://www.aaiusa.org/pages/demographics/
Matin M, LeBaron S (2004) Attitudes toward cervical cancer screening among Muslim women: a pilot study. Women & Health 39(3):63–77
Salman K (2012) Health beliefs and practices related to cancer screening among Arab Muslim women in an urban community. Health Care for Women International 33(1):45–74
Michigan Department of Community Health and Michigan Public Health Institute. Special cancer behavioral risk factor survey, 2008. www.michigancancer.org/PDFs/MCCReports/SCBRFS_2008-042910.pdf.
Williams KP, Mullan PB, Todem D (2009) Moving from theory to practice: implementing the Kin KeeperSM Cancer Prevention model. Health Educ Res 24:343–56
Williams KP, Reiter P, Mabiso A, Maurer J, Paskett E (2009) Family History of cancer predicts Papanicolaou screening behavior for African American and White women. Cancer 115(1):179–189
Mandelblatt JS, Gold K, O'Malley AS et al (1999) Breast and Cervix cancer screening among multiethnic women: role of age, health, and source of care. Preventive Medicine 28(4):418–425
Harlan LC, Bernstein AB, Kessler LG (1991) Cervical cancer screening: who is not screened and why? Am J Public Health 81(7):885–890
Skrondal A, Rabe-Hesketh S (2009) Prediction in multilevel generalized linear models. Journal of the Royal Statistical Society, Series A 172:659–687
Skrondal A, Rabe-Hesketh S (2004) Generalized latent variable modeling: multilevel, longitudinal, and structural equation models. Chapman & Hall/CRC, Boca Raton, FL
Raudenbush SW, Bryk AS (2002) Hierarchical linear models: applications and data analysis methods, 2nd edn. Sage, Newbury Park, CA
SAS Institute Inc., 2008. SAS/STAT® 9.2 User's guide. Cary, NC: SAS Institute Inc.
Percac-Lima S, Aldrich LS, Gamba MA et al (2011) Barriers to follow-up of an abnormal Pap smear in Latina women referred for colposcopy. J Gen Intern Med 25(11):1198–1204
Acknowledgments
This project has been funded by the National Institutes of Health National Institute of Nursing Research R21NR010366. Each of the authors has contributed writing this manuscript and given their permission for their names to be used. We would like to thank Justice Wilson for formatting this manuscript.
Conflict of Interest
No financial disclosures were reported by the authors of this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gauss, J.W., Mabiso, A. & Williams, K.P. Pap Screening Goals and Perceptions of Pain among Black, Latina, and Arab Women: Steps Toward Breaking down Psychological Barriers. J Canc Educ 28, 367–374 (2013). https://doi.org/10.1007/s13187-012-0441-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-012-0441-1