Abstract
Cancer patients report significant levels of unmet needs in the realm of communication. Communication skills training programs have been shown to improve clinical communication. However, advanced communication skills training programs in oncology have lacked institutional integration, and thus have not attended to institutional norms and cultures that may counteract explicit communication skills training. We developed and implemented an advanced communication skills training program made up of nine teaching modules for faculty, fellows, and residents. Training included didactic and experiential small group work. Self-efficacy and behavior change were assessed for individual participants. Since 2006, 515 clinicians have participated in this training program. Participants have shown significant gains in self-efficacy regarding communicating with patients in various contexts. Our initial work in this area demonstrates the implementation of such a program at a major cancer center to be feasible, to be acceptable, and to have a significant impact on participants' self-efficacy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cancer brings a host of challenging encounters: emotionally charged bad news, uncertainty, threatening prognoses, burdensome treatments, declining health, and despair at the end-of-life. Though medical schools increasingly train students in basic communication skills, an applied curriculum that addresses these issues is needed within cancer centers. Two brief vignettes highlight the necessary curriculum:
-
1.
Mrs. Williams' recent diagnosis with Stage II colon cancer has left her confused and uncertain. She has received differing opinions on whether to have adjuvant chemotherapy and wonders about the possibility of a clinical trial. She wants to be involved in the decision, and desires to find a doctor she can trust. This example suggests the need for a communication curriculum aimed at shared decision making about treatment options.
-
2.
Mr. Jones' pancreatic cancer encased the mesenteric artery, rendering the diagnostic news more challenging because his tumor was inoperable. “How long do I have? Will I suffer?” wondered Mr. Jones. Fearing pain during his dying process, he wanted to discuss what to expect over the last days of his life. Who would speak to his wife and young children? This case illustrates the need for addressing advanced care planning and end-of-life communication in the curriculum.
There is an increasing recognition and acceptance that quality healthcare requires patient-centered communication. This consensus is supported by a growing evidence base (see the National Cancer Institute's monograph [1] for a review of this literature). It is also reflected by accreditation requirements in graduate medical education [2] and standards set by the reports and initiatives from the Institute of Medicine [3] and the US Department of Health and Human Services [4].
Distinct features of cancer care make the need for patient-centered communication in this context particularly important [1]. These distinct features include diseases that are both life-threatening and potentially curable, numerous and changing clinicians making up a healthcare team, multiple treatment modalities, and long periods of uncertainty following treatment. There is ample evidence that communication in cancer care has room for improvement. Cancer patients report significant levels of unmet needs in the realms of communication, specifically information provision, psychosocial support, and appropriate response to emotional cues [5–7]. Attending to the unmet needs of cancer patients is crucial for optimal care.
The notion of advanced communication skills training in oncology has grown out of this research, as has the development of specific guidelines that assist in identifying effective strategies in complex communication settings such as delivering bad news [8–12], collaborative decision making regarding standard treatments and clinical trials [13], and the discussion of prognosis and realistic hope in the context of advanced disease [14, 15]. Short immersion courses in cancer communication training, following a residential model, have shown success in improving communication skills [16–19]. These types of courses have contributed to the development of an evidence base that communication skills training is effective. However, training in immersion courses is generally offered only to select oncologists from various institutions who attend the training as participants in research studies. These interventions have thus have lacked the ability to address effectively the “hidden curriculum”—an organization's implicit messages and culture that may counter the message of a patient-centered communication curriculum. It is our assertion that advanced communication training in oncology should be made available to all practicing clinicians and should be part of an overall strategy for improving the quality of care at an institution, being integrated into an institution's graduate and continuing medical education practices.
The purpose of this paper is to describe the development and implementation of the Comskil Training Program, a communication skills training initiative, at Memorial Sloan-Kettering Cancer Center (MSKCC). The development and implementation of this program have followed several steps: first, development of the curriculum; second, faculty development; third, implementation of the program for MSKCC fellows, residents, and faculty, as well as local and national dissemination; and fourth, assessment of the program.
Curriculum Development
We have developed nine teaching modules that focus on specific communication challenges in oncology consultations (e.g., Breaking Bad News, Discussing Prognosis, Communicating with Patients via Interpreters). The module development process included a series of five consecutive steps: (1) systematic literature review, (2) modular blueprint development, (3) training materials development, (4) role play scenario development, and (5) making revisions and adaptations iteratively [20]. The teaching modules are based upon the Comskil Conceptual Model which explicitly defines the important components of a consultation [21]. This model explicates 26 communication skills, organized into six categories, that are fundamental to patient-centered clinical communication. Each of our modules incorporates appropriate skills.
The process of teaching each module has been based on best practices from around the world [22, 23]. One of these best practices is a focus on experiential learning through role play [24]. Many effective communication skills training programs have relied on small group role play sessions as a key part of their training. Role plays that simulate an actual consultation, using an actor taking the role of a patient (commonly called a simulated patient), are an integral component of accepted communication skills training programs [25]. Role play provides an opportunity for trainees to practice new skills and receive feedback about their performance from a variety of sources. The Comskil Training Program utilizes small group role play sessions as a core component of training, devoting at least half of every 3-h training module to these role play sessions. During these sessions, learners can receive feedback from their facilitator and others in their small group in addition to watching instant video playback of their interaction with the simulated patient. Our facility has six role play rooms, equipped with two wall-mounted cameras and video playback using picture-in-picture software, supported by a main frame computer for storage and transfer of digital movie-pegs. We have trained 25 actors to play simulated patients, spanning a range of ages as needed for scenarios.
Faculty Development
In developing a communication training program for a comprehensive cancer center, we were mindful of the challenge of the hidden curriculum. In medical education, teaching and learning occur on many levels: on the level of the explicit, intended curriculum endorsed by teaching institutions, on the level of ad hoc interpersonal exchanges among students and educators, and on the level of implicit transmission that promotes the continuance of the organizational structure and culture of the learning institution [26]. Exerting a countercultural influence on the negative effects of hidden curriculum involves taking into account relational aspects of care and promoting the moral, ethical, and emotional efforts of the trainees, and highlighting their individual strengths [27].
Our approach from the start was to engage the leadership of the institution in the process of improving communication by training a group of faculty from the institution to play a key role in the training as facilitators. A group of attending physicians and surgeons from MSKCC, well regarded as educators, clinicians and good communicators, were invited to train as facilitators. The interested faculty first trained in the communication training modules as learners. Following this, they trained further as facilitators [28] and have returned to facilitate groups of fellows, residents, and junior faculty from their own disciplines (i.e., surgeons teach surgeons).
Between 2006 and the present time, 40 attending physicians and surgeons from the Departments of Medicine, Surgery, Radiation Oncology, Neurology and Pediatrics have been clinical facilitators in the program. In order to supplement the clinical facilitators, 23 members from the Departments of Psychiatry and Behavioral Sciences and Social Work, including psychiatrists, psychologists, behavioral scientists and social workers, have also trained to facilitate. These facilitators bring an expertise in the psychosocial aspects of cancer care that complements the physicians' and surgeons' clinical expertise. When possible, a clinical facilitator co-facilitates each session with a psychosocial facilitator. In this model, the discipline-specific facilitator is sensitive to the hidden curriculum, by providing role models for effective communication, and the psychosocial facilitator adds a level of expertise of patients’ experiences. Furthermore, we offer faculty development to participating facilitators through assessment and feedback [29]. This process allows us to give corrective feedback to those who have not met the facilitation standards.
Implementation of Training
As shown in Table 1, the Comskil Training Program has been implemented with physicians and surgeons within our institution and from other institutions in various career stages: graduate medical trainees (interns, residents, and fellows), junior faculty, and attending faculty. Graduate medical trainees, in particular, are at an ideal level of medical training to be engaged in an advanced communication skills curriculum, as they have enough experience to feel comfortable with the clinical content [30], but have not yet established engrained communication patterns that are difficult to change.
We have completed four academic years of training residents and fellows in the Comskil Training Program. All of the modules are not required of all fellows and residents. We work closely with the program directors of the training programs to develop programs that meet the needs of the trainees. Nearly all graduate medical education training programs in patient care specialties participate in the modules on Shared Decision Making about Treatment Options, Responding to Patient Anger, and Discussing Prognosis. We also regularly offer training for attending physicians and surgeons at MSKCC, including those who work in the MSKCC community-based networks. We estimate that approximately 15% of the clinical attending physicians and surgeons at MSKCC have attended the Comskil Training Program to date. Some clinicians attend faculty trainings to improve their own communication skills, while others develop a desire to work in the program as a facilitator.
We have also begun disseminating the Comskil Training Program to both local and national healthcare providers and educators. With support from the Josiah H. Macy Jr. Foundations across 2 years, we opened the faculty trainings described above to attending physicians and surgeons from academic hospitals across the Greater New York City area. We specifically targeted those in leadership roles (e.g., department chairs and training program directors) with a focus on training them to also be facilitators. This has allowed us to build collaborative educational and research relationships with other institutions. More recently, we have begun offering faculty trainings to clinicians both nationally and internationally, with fees to cover costs of producing such trainings.
Assessment
Assessment of the program and learners' individual abilities is central to our implementation for several reasons. First, by assessing individuals' communication competence, we are able to give them feedback on their current communication strengths and areas for improvement before they begin training and following their completion of training. Second, the assessment of improvement of communication skill usage between pre- and post-training as well as learners' evaluations of the course allows us to ensure the effectiveness of training and informing our knowledge of which skills can most easily be improved. Third, the role of assessment is critical to training program directors who need to give evidence of such to Accreditation Council for Graduate Medical Education (ACGME) and other accrediting institutions.
To guide our assessment, we use a modified version of Kirkpatrick's Triangle, a model for evaluating the success of a training program that proposes four steps to test for efficacy of training [31, 32]. The first step involves eliciting a reaction from the trainees about their feelings about the training; the second step proposes that participants’ learning be tested in an objective, quantitative manner; the third step suggests that a participants’ on-the-job performance be statistically compared after the training to their behavior before the training as it relates to the objectives of the training program; and the fourth step to test for efficacy of the program is to evaluate if the overarching desired result was accomplished [31]. By quantifying evaluation in such a way, Kirkpatrick proposes that the efficacy of a training program is monitored adequately.
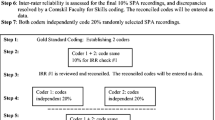
We have applied this model to the evaluation of the Comskil Training Program as shown in Fig. 1. At the base or “evaluation of reaction” level, trainees are asked to complete anonymous course evaluations rating their satisfaction with the module with space to write suggestions and comments. On the “evaluation of learning” level, trainees are assessed in two ways pre- and post-training: Standardized Patient Assessments (SPAs), similar to Objective Structured Clinical Examination (OSCEs), and participants’ reports of their self-efficacy. On the third level of evaluation, behavior is assessed by comparing the use of skills pre- and post-training in on-the-job recordings of consultations with patients in clinic. For the second and third levels, we developed an assessment tool called the Comskil Coding System, which was developed to be partnered with our curriculum [29]. We are in the early stages of evaluating training using Kirkpatrick’s fourth and highest level where training is evidenced in broad, real-world contexts, the “result” level, with patient outcomes. We are gathering data from patient ratings of how their doctor demonstrated the intended skills taught in training and their satisfaction with that communication. Implementing this series of evaluation yields a complex picture of how training impacts reactions, knowledge, attitudes, behavior, and outcome.
Given varying schedules and rotations of the fellows, residents, and faculty who have participated in the program, as well as the needs of the particular training program, we have offered a flexible menu of assessment tools. For example, pediatric fellows come to training during their first fellowship year, the year in which they are primarily on in-patient service, thus making it difficult to capture real clinical consultations. These fellows participate instead in SPAs, allowing us to assess skill uptake as a result of the training as well as give feedback. Attending physicians who have participated in the program have had clinical video recordings completed [33].
Results
As shown in Table 1, 515 unique clinicians have participated in the Comskil Training Program since its inception. Participants' reaction to the training was assessed through course evaluation items assessing how strongly participants agreed with the following statements: “The skills I learned in this module will allow me to provide better patient care”; “This module prompted me to critically evaluate my own communication skills”; and “The facilitator was effective.” Each item was ranked between 1 and 5, with 5 = strongly agree. Ratings of these items were generally high, as shown in Table 2. Some modules have had fewer participants than others because they are less applicable to some disciplines (e.g., radiology and radiation oncology faculty tend to not participate in the modules on Discussing the Transition to Palliative Care and Discussing Death and Dying).
In three of the modules, fellows and residents gave significantly lower ratings than did attendings and nurses, but the magnitude of difference was small. We also assessed participants' retrospective pre–post-self-efficacy data across all modules and all participants. As shown in Table 3, participants reported significant gains in self-efficacy regarding communicating with patients in all of the modules. In addition, as we have reported elsewhere [20, 33], pre- and post-training video consultation data demonstrate an increase in attending physicians' and surgeons' use of certain communication skills that are taught as part of the Comskil Training Program.
Discussion
The Comskil Training Program as described herein uses internationally, well-accepted techniques for communication skills training. We believe the unique nature of our program is its illustration that advanced communication training in oncology can be integrated into an institution’s regular practices and ongoing graduate medical education. A key agenda of this work is developing reflective and mindful practices in clinicians that will help them to be life-long learners.
We have learned several lessons during this process. First, ideal implementation of communication skills training should include facilitators from each discipline facilitating participants from the same discipline, providing effective role models. Furthermore, these facilitators have specific experiences from their disciplines that they can relay to participants. Second, real learning results from the process of role play and feedback that takes place. Participants are sometimes more eager to talk about the issues that are challenging than to try them out in role play. Facilitators must carefully manage the time in the small groups. The third is to trust the process of experiential, learner-centered small group work. We have repeatedly encountered participants who began the training program with low expectations or even doubts about the impact the training would have on their communication, and by the end of the training spoke enthusiastically of what they had learned. Fourth, we have found that it is necessary to have a balanced top-down and bottom-up approach. Institutional commitment has been critically important, providing funding for the communication training laboratory rooms and the credibility to build the program beginning with the train-the-trainer approach. However, the institution did not mandate the program for attending physicians and surgeons or for graduate trainees. In this regard, we have used a bottom-up approach, building a reputation and gradually implementing the program. A mark of success of this approach is that training programs in surgery, medical oncology, pediatrics, radiation oncology, neurology, critical care, psychiatry, and other medical specialties have now made participation of their fellows and residents mandatory.
For those who wish to replicate this work, we have several suggestions. First, if there is not adequate support to pay actors, participants may take turns playing the role of the patient in the role play sessions. One advantage of this method is that it allows the participant to experience what it would be like to be a cancer patient. Second, if there is not a strong enough base of facilitators to support small group role play sessions, large group role play sessions (sometimes called ‘fishbowls’) can be conducted [34]. Third, those without access to a formal communication laboratory with built-in recording equipment could use a tripod-based digital camera connected to a laptop. Thus, portability and adaptability can prevail against common barriers.
Future Directions
There are two major future directions for this work. The first is a more rigorous evaluation of the effects of the Comskil Training Program on patient outcomes. Although there has been significant research examining the effect of patient-centered communication on such outcomes there have been few attempts to link improved outcomes directly to communication skills training. Our review of the literature showed eight studies of cancer communication skills training [19, 35–41] that examined one or more patient outcomes as a result of applied communication skills training for oncology clinicians. Five assessed patient satisfaction using a cohort of each clinician’s patients before training and a cohort after training. Of these, three reported no change in satisfaction [19, 35, 36] one reported a significant improvement [37] and one reported a positive but non-significant change [38]. Of the eight, three [39–41] assessed patient or patient/family member distress or anxiety both pre- and post-training, with none showing any change. Reducing patient worry may be an overly ambitious outcome when bad news has been shared, prognosis discussed or challenging treatments proposed. Clearly, more work needs to be done to assess the impact of communication skills training on patient outcomes.
Second, we recognize the need to provide opportunities for communication skills training to multi-disciplinary healthcare professionals. As nurses play a key role in cancer care, developing a parallel Comskil Training Program for nursing staff [42] at our institution is an important agenda.
Conclusion
Recognition of the centrality of patient-centered communication is critical to improving healthcare quality and outcomes. Thus, the art of better communication is linked to measurable end points. Participation in a comprehensive communication skills training program can be time well spent, potentially impacting the care of thousands of patients over a career. Our initial work in this area demonstrates the implementation of such a program at a major Cancer Center to be feasible and acceptable, and to have a significant impact on participants' self-efficacy about communication.
References
Epstein R, Street RL Jr (2007) Patient-centered communication in cancer care: promoting healing and reducing suffering. In: Institute NC (ed) Bethesda, MD
ACGME Outcome Project (2006) Enhancing residency education through outcomes assessment. Accessed 18 Aug 2006
Institute of Medicine of the National Academies (2004) Improving medical education: enhancing the behavioral and social science content of medical school curricula. Institute of Medicine, Washington DC
US Department of Health and Human Services (2000) Healthy people 2010. US Department of Health and Human Services, Washington DC
Sanson-Fisher RW, Girgis A, Boyes A et al (2000) The unmet supportive care needs of patients with cancer. Cancer 88:225–236
Hack TF, Degner LF, Parker P (2005) The communication goals and needs of cancer patients; a review. Psycho-Oncology 14:831–845
Butow PN, Brown RF, Cogar S, Tattersall MHN, Dunn SM (2002) Oncologists’ reactions to cancer patients verbal cues. Psycho-Oncology 11:47–58
Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP (2000) SPIKES—a six step protocol for delivering bad news: application to the patient with cancer. Oncologist 5:302–311
Eggly S, Penner L, Albrecht T et al (2006) Discussing bad news in the outpatient oncology clinic: rethinking current communication guidelines. J Clin Oncol 24:716–719
Costantini A, Baile WF, Lenzi R et al (2009) Overcoming cultural barriers to giving bad news: feasibility to promote truth-telling to cancer patients. J Cancer Educ 24:180–185
Dikici MF, Yaris F, Cubukcu M (2009) Teaching medical students how to break bad news: a Turkish experience. J Cancer Educ 24:246–248
Tavakol M, Murphy R, Torabi S (2008) Educating doctors about breaking bad news: an Iranian perspective. J Cancer Educ 23:260–263
Brown RF, Butow PN, Butt DG, Moore AR, Tattersall MHN (2004) Developing ethical strategies to assist oncologists in seeking informed consent to cancer clinical trials. Soc Sci Med 58:379–390
Back AL, Arnold RM (2006) Discussing prognosis: “How much do you want to know?” Talking to patients who do not want information or who are ambivalent. J Clin Oncol 24:4214–4217
Back AL, Arnold RM (2006) Discussing prognosis: “How much do you want to know?” Talking to patients who are prepared for explicit information. J Clin Oncol 24:4209–4213
Back AL, Arnold RM, Baile WF et al (2007) Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med 167:453–460
Fallowfield L, Jenkins V, Farewell V, Saul J, Duffy A, Eves R (2002) Efficacy of a cancer research UK communication skills training model for oncologists: a randomised controlled trial. Lancet 359:650–656
Fallowfield L, Jenkins V, Farewell V, Solis-Trapala I (2003) Enduring impact of communication skills training: results of a 12-month follow-up. Br J Cancer 89:1445–1449
Razavi D, Merckaert I, Marchal S et al (2003) How to optimize physicians’ communication skills in cancer care: results of a randomized study assessing the usefulness of posttraining consolidation workshops. J Clin Oncol 21:3141–3149
Brown RF, Bylund CL, Lubrano di Ciccone B, Diamond C, Eddington J, Kissane D (2010) Patient centered communication skills training for oncologists: describing the content and efficacy of training. Commun Educ 59:236–249
Brown RF, Bylund CL (2008) Communication skills training: describing a new conceptual model. Acad Med 83:37–44
Cegala DJ, Broz SL (2002) Physician communication skills training; a review of the theoretical backgrounds, objectives and skills. Med Educ 36:1004–1016
Back AL, Arnold RM, Baile WF, Tulsky JA, Fryer-Edwards K (2009) What makes education in communication transformative? J Cancer Educ 24:160–162
Kurtz S, Silverman J, Draper J (1998) Teaching and learning communication skills in medicine. Radcliffe Medical Press Ltd, Abingdon
Lane C, Rollnick S (2007) The use of simulated patients and role-play in communication skills training: a review of the literature to August 2005. Patient Educ Couns 67:13–20
Hafferty FW (1998) Beyond curriculum reform: confronting medicine’s hidden curriculum. Acad Med 73:403–407
Browning DM, Meyer EC, Truog RD, Solomon MZ (2007) Difficult conversations in health care: cultivating relational learning to address the hidden curriculum. Acad Med 82:905–913
Bylund CL, Brown RF, Lubrano di Ciccone B et al (2008) Training faculty to facilitate communication skills training: development and evaluation of a workshop. Patient Educ Couns 70:430–436
Bylund CL, Brown RF, Lubrano di Ciccone B, Diamond C, Eddington J, Kissane D (2009) Assessing facilitator competence in a comprehensive communication skills training programme. Med Educ 43:342–349
Back AL, Arnold RM, Tulsky JA, Baile WF, Fryer-Edwards KA (2003) Teaching communication skills to medical oncology fellows. J Clin Oncol 21:2433–2436
Kirkpatrick DL (1967) Evaluation of training. In: Craig R, Bittlel I (eds) Training and development handbook. McGraw Hill, New York
Konopasek L, Rosenbaum M, Encandela J, Cole-Kelly K (2010) Evaluating communication skills training courses. In: Kissane DW, Bultz BD, Butow PN, Finlay IG (eds) Handbook of communication in oncology and palliative care. Oxford University Press, Oxford, pp 683–693
Bylund CL, Brown RF, Gugeun JA, Diamond C, Bianculli J, Kissane DW (2010) The implementation and assessment of a comprehensive communication skills training curriculum for oncologists. Psycho-Oncology 19:583–593
Bylund CL, Brown R, Lubrano di Ciccone B, Konopasek L (2010) Facilitating skills practice in communication role play sessions: essential elements and training facilitators. In: Kissane DW, Bultz BD, Butow PN, Finlay IG (eds) Handbook of communication in oncology and palliative care. Oxford University Press, Oxford, pp 597–606
Brown RF, Butow P, Boyle F, Tattersall MHN (2007) Seeking informed consent to cancer clinical trials: evaluating the efficacy of communication skills training. Psycho-Oncology 16:507–516
Hulsman RL, Ros WJG, Winnubst JAM, Bensing JM (2002) The effectiveness of a computer-assisted instruction programme on communication skills of medical specialists in oncology. Med Educ 36:125–134
Delvaux N, Merckaert I, Marchal S et al (2005) Physicians’ communication with a cancer patient and a relative: a randomized study assessing the efficacy of consolidation workshops. Cancer 103:2397–2411
Shilling V, Jenkins V, Fallowfield L (2003) Factors affecting patient and clinician satisfaction with the clinical consultation: can communication skills training for clinicians improve satisfaction? Psycho-Oncology 12:599–611
Lienard A, Merckaert I, Libert Y et al (2006) Factors that influence cancer patients’ anxiety following a medical consultation: impact of a communication skills training programme for physicians. Ann Oncol 17:1450–1458
Lienard A, Merckaert I, Libert Y et al (2008) Factors that influence cancer patients’ and relatives’ anxiety following a three-person medical consultation: impact of a communication skills training program for physicians. Psycho-Oncology 17:488–496
Merckaert I, Libert Y, Delvaux N et al (2008) Factors influencing physicians’ detection of cancer patients’ and relatives’ distress: can a communication skills training program improve physicians’ detection? Psycho-Oncology 17:260–269
Rosenzweig M, Clifton M, Arnold R (2007) Development of communication skills workshop for oncology advanced practice nursing students. J Cancer Educ 22:149–153
Acknowledgments
This study was funded by Arthur Vining Davis Foundation, Josiah H. Macy, Jr. Foundations, and Kenneth B. Schwartz Center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bylund, C.L., Brown, R.F., Bialer, P.A. et al. Developing and Implementing an Advanced Communication Training Program in Oncology at a Comprehensive Cancer Center. J Canc Educ 26, 604–611 (2011). https://doi.org/10.1007/s13187-011-0226-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-011-0226-y