Abstract
Introduction
In contrast to information on the effects of organophosphate, pesticide, or environmental exposures, data on cholinergic crisis caused by pharmaceutical cholinesterase inhibitors are sparse. The present study aimed to describe the characteristics, demographics, and mortality of patients with cholinergic crisis caused by pharmaceutical cholinesterase inhibitors using a nationwide inpatient database in Japan.
Methods
We identified patients diagnosed with cholinergic crisis as a result of taking cholinesterase inhibitor medications in the Japanese Diagnosis Procedure Combination inpatient database from July 2010 to March 2016. We examined the patients’ characteristics, treatments, and mortality.
Results
A total of 235 patients with cholinergic crisis were identified during the 69-month study period. Forty-eight patients required mechanical ventilation (20.4%), and 15 patients died (6.4%) in hospital. The median lengths of hospital stay and intensive care unit stay were 15 days (interquartile range, 6–42) and 4 days (2–8), respectively. Approximately half of all hospitalized patients required catecholamines, atropine, or mechanical ventilation, while the other half did not require any of these treatments. Patients who required catecholamines, atropine, or mechanical ventilation were more likely to die and had longer hospital stays.
Conclusions
Cholinergic crisis caused by pharmaceutical cholinesterase inhibitors is a rare but potentially life-threatening condition. Patients who require mechanical ventilation and catecholamines or atropine have a poorer prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acetylcholinesterase terminates synaptic transmission through hydrolyzation of the neurotransmitter acetylcholine in brain synapses and neuromuscular junctions [1, 2]. Irreversible inhibition of acetylcholinesterase with organophosphorus compounds [1] leads to overstimulation of cholinergic receptors via excessive accumulation of acetylcholine, resulting in respiratory failure or even death [3]. Although reversible cholinesterase inhibitors are beneficial for the treatment of Alzheimer’s disease [4,5,6], myasthenia gravis [7], and neurogenic bladder [8, 9], they can still cause adverse cholinergic reactions. Excessive cholinesterase inhibition can cause cholinergic crisis, defined by symptoms including pupils ≤ 2 mm in diameter, fasciculations, heart rate ≤ 60 beats per minute, systolic blood pressure ≤ 80 mmHg, decreased consciousness (Glasgow Coma Scale < 15), excessive sweating, or poor air entry due to bronchorrhea and/or bronchospasm [10, 11].
Patients receiving pharmaceutical cholinesterase inhibitors rarely develop cholinergic crisis in clinical practice. However, relatively higher doses of distigmine bromide were prescribed for the treatment of neurogenic bladder in Japan compared with in other countries until 2010, and several case reports [12,13,14,15] and case series [16, 17] of cholinergic crisis associated with therapeutic doses of cholinesterase inhibitors have therefore been reported by Japanese doctors. However, to the best of our knowledge, there has been no large-scale study of the distribution of patient characteristics, and variations in treatments and outcomes among patients with cholinergic crisis caused by cholinesterase inhibitors.
The present study aimed to describe the patient characteristics, demographics, and mortality of cholinergic crisis caused by pharmaceutical cholinesterase inhibitors, using data from a nationwide database in Japan.
Materials and Methods
Data Source
We used information from the Japanese Diagnosis Procedure Combination inpatient database from July 2010 to March 2016. The database includes discharge abstracts and administrative claims data from more than 1200 acute-care hospitals and covers approximately 90% of all tertiary-care emergency hospitals in Japan. All academic hospitals are obliged to contribute to the database, while participation is voluntary for community hospitals. The diagnoses and procedure records in the Japanese Diagnosis Procedure Combination inpatient database have been validated previously [18]. The specificity of diagnoses exceeded 96%, and the sensitivity ranged from 50 to 80%. The specificity and sensitivity for procedures both exceeded 90% [18].
The database includes information on patients’ age, sex, body weight, body height, diagnoses, comorbidities at admission, complications after admission, procedures, prescriptions, intensive care unit (ICU) admission, and discharge status. Diagnoses, comorbidities, and complications were recorded according to the International Classification of Diseases, Tenth Revision (ICD-10) codes, with text data in Japanese. Barthel Index [19] and Japan Coma Scale (JCS) [20] at admission were also recorded. Barthel Index is a standardized scale for evaluating a patient’s self-care abilities. Scores are associated with performance of activities of daily living following discharge from hospital, with the total score ranging from 0 (complete dependence) to 100 (complete independence) [19]. JCS is used to describe the general level of consciousness, including measures of alert consciousness, dizziness, somnolence, and coma. JCS scores are well correlated with the Glasgow Coma Scale scores [20].
Patient Selection
We included patients who were diagnosed with cholinergic crisis, identified by ICD-10 code T44.0 (poisoning by drugs primarily affecting the autonomic nervous system, anticholinesterase agents) together with the text “cholinergic crisis” in Japanese.
Patient Backgrounds and Treatments
For this study, we analyzed patient age (years), sex, body mass index (BMI) (kg/m2), Barthel Index, JCS, comorbidities at admission, and concomitant diseases. Age was categorized into 0–19, 20–39, 40–59, 60–69, 70–79, 80–89, or ≥ 90 years; BMI was categorized into < 18.5, 18.5–22.9, 23–24.9, 25–29.9, or ≥ 30 [21]; Barthel Index was categorized into 0–50, 55–90, and 95–100 [22]. Comorbidities at admission included myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatologic disease, peptic ulcer disease, mild liver disease, diabetes without chronic complications, diabetes with chronic complications, hemiplegia or paraplegia, renal disease, any malignancy including leukemia and lymphoma, metastatic solid tumor, myasthenia gravis, neurogenic bladder, and benign prostatic hypertrophy. ICD-10 codes A41.9 and A49.9 were taken to denote concomitant sepsis and ICD-10 code J69 to denote aspiration pneumonia.
Treatments included use of catecholamines (dopamine, dobutamine, noradrenaline, and adrenaline), use of atropine, hemodialysis, and mechanical ventilation.
Outcomes
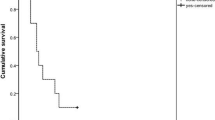
The main outcome of interest was in-hospital mortality. The secondary outcome was length of hospital stay (days).
Statistical Analyses
We hypothesized that patients with cholinergic crisis who needed circulatory or respiratory support were more likely to die. We therefore divided the patients into those who did not receive catecholamines, atropine, or mechanical ventilation; those who received catecholamines or atropine (without mechanical ventilation); and those who received mechanical ventilation (with or without catecholamines or atropine). We then compared the mortality and the mean length of stay among the three groups of patients receiving different treatments using Fisher’s exact and Kruskal–Wallis tests, respectively. These analyses were performed using IBM SPSS version 23.0 (IBM Corp., Armonk, NY, USA) and STATA/MP 14.2 (StataCorp, College Station, TX, USA).
Results
Among a total of approximately 40 million inpatients during the 69-month study period, we identified 235 patients with cholinergic crisis. Patient characteristics are shown in Table 1. Patients aged ≥ 70 years accounted for > 72% of all eligible patients. The average (standard deviation) ages and median (interquartile range) ages of all patients were 74 (16) and 79 (68–84) years, respectively. The overall proportion of males was 49%. About half of the patients showed alert consciousness at admission. The proportions of patients with neurogenic bladder or benign prostatic hypertrophy, myasthenia gravis, and dementia were 23, 10, and 12%, respectively. There was no in-hospital mortality among patients with comorbid myasthenia gravis. Sepsis and aspiration pneumonia occurred concomitantly in 15 (6%) patients and 38 (16%) patients, respectively.
Patient outcomes and treatments are shown in Table 2. The overall in-hospital mortality was 6.4% and the median length of hospital stay was 15 days. Thirty-four patients were admitted to the ICU. The proportion of patients who received mechanical ventilation, catecholamines, and atropine were 20, 20, and 42%, respectively. The median (interquartile range) durations of mechanical ventilation and ICU stay in patients who needed those interventions were 4.5 (2–17) and 4 (2–8) days, respectively.
Approximately half of all hospitalized patients required catecholamines, atropine, or mechanical ventilation, while the other half did not require any of these treatments. In-hospital mortalities were 2% in patients who did not receive catecholamines, atropine, or mechanical ventilation, 8% in those who received catecholamines or atropine (without mechanical ventilation), and 15% in those who received mechanical ventilation (with or without catecholamines or atropine), with a significant difference among the three groups (p = 0.007) (Fisher’s exact tests; Table 3). The mean length of stay differed significantly among the three groups (p ≤ 0.001) (Kruskal–Wallis test; Table 4).
Discussion
We identified 235 patients with cholinergic crisis following administration of cholinesterase inhibitor medications in a Japanese nationwide inpatient database, during an observation period of 5 years and 9 months. Overall in-hospital mortality was about 6%; however, about half of all the patients received catecholamines, atropine, or mechanical ventilation, and these patients had higher in-hospital mortality.
Patients in cholinergic crisis present with a combination of typical symptoms, which can thus discriminate cholinergic crisis from other diseases. However, differential diagnosis may be difficult in the early phase of the disease. Most clinicians may never have experienced cholinergic crisis, and some patients with cholinergic crisis may therefore initially have been treated for other conditions, such as pneumonia. Clinicians may only have diagnosed cholinergic crisis after noting the excessive decrease in serum cholinesterase levels several days after admission. This delayed diagnosis may have resulted in treatment opportunities being missed. Although the specificity of a recorded diagnosis of cholinergic crisis in the database was considered to be high, the sensitivity may be low, because a physician’s awareness of the disease may be limited and the condition may thus have been underreported in the database.
There were 6167 cases of myasthenia gravis in Japan in 2003 [23]. Our study identified 24 patients with cholinergic crisis and myasthenia gravis during the 69-month study period, all of whom survived. A previous retrospective review of 2154 myasthenia gravis patients with 267 episodes of crisis found that myasthenic crisis was the most common (258/267, 96.6%), while nine patients had cholinergic crisis (3.4%) [17]. Myasthenia gravis patients tend to be younger and are well recognized to be at risk of cholinergic crisis, suggesting that the sensitivity of cholinergic crisis diagnosis may be higher among myasthenia gravis patients.
In our study, more than 70% of patients were aged 70 years or older, because patients with dementia, benign prostatic hypertrophy, and neurogenic bladder are generally older. Benign prostatic hypertrophy only occurs in men, but dementia and myasthenia gravis are more likely to occur in women [24], and the overall proportions of males and females were almost identical.
According to previous studies, distigmine bromide was considered as the main cause of cholinergic crisis in Japan [12,13,14,15]; however, the proportions of patients with comorbid neurogenic bladder (16.6%) or benign prostatic hypertrophy (8.9%) were relatively low. Unlike myasthenia gravis, it is possible that these diseases may have been underreported because the clinicians discontinued cholinesterase inhibitors prescribed in outpatient clinics when cholinergic crisis was suspected. The inpatient database does not include information on treatments in outpatient clinics before admission.
A previous small study showed three in-hospital deaths among 16 patients with cholinergic crisis with cholinesterase inhibitor medications [15]. Our study identified 15 in-hospital deaths among 235 patients, including seven of 48 patients with mechanical ventilation. Our study also showed that patients who required mechanical ventilation, catecholamines, or atropine were more likely to die in hospital.
Previous reports of acute organophosphate poisoning for accidental ingestion or attempted suicide revealed that 40% of patients received mechanical ventilation, with a mean duration of 7 days, and in-hospital mortality ranged from 15 to 25% [1, 11, 25]. These figures were relatively high compared with the present study. However, the differences in disease severity and mortality may be explained by the different inhibitory mechanisms induced by organophosphorus compounds and cholinesterase inhibitor medications [1, 2].
This study had some limitations. First, the database did not contain information on each component used in the diagnostic criteria of cholinergic crisis, including symptoms, vital signs, physical findings, and laboratory data. Furthermore, there was no information about blood levels of drugs or serum cholinesterase activity. The lack of this information means that we may not have captured all patients with cholinergic crisis. Second, we did not take into account the nature of the exposure (therapeutic dose, accidental overdose, or intentional ingestion for attempted suicide) due to lack of data. Third, we did not take account of the amount of atropine used for treatment. Last, the database did not include information on the results of Tensilon tests, which may help to distinguish myasthenic crisis from cholinergic crisis among patients with myasthenia gravis [19, 26].
Conclusions
Cholinergic crisis caused by pharmaceutical cholinesterase inhibitors is a rare but potentially life-threatening condition. Patients who require mechanical ventilation and catecholamines or atropine have a poorer prognosis.
References
Gorecki L, Korabecny J, Musilek K, Nepovimova E, Malinak D, Kucera T, et al. Progress in acetylcholinesterase reactivators and in the treatment of organophosphorus intoxication: a patent review (2006-2016). Expert Opin Ther Pat. 2017;27(9):971–85.
Lushington GH, Guo JX, Hurley MM. Acetylcholinesterase: molecular modeling with the whole toolkit. Curr Top Med Chem. 2006;6(1):57–73.
Marrs TC. Organophosphate poisoning. Pharmacol Ther. 1993;58(1):51–66.
Korabecny J, Andrs M, Nepovimova E, Dolezal R, Babkova K, Horova A, et al. 7-Methoxytacrine-p-anisidine hybrids as novel dual binding site acetylcholinesterase inhibitors for Alzheimer’s disease treatment. Molecules. 2015;20(12):22084–101.
Nepovimova E, Korabecny J, Dolezal R, Babkova K, Ondrejicek A, Jun D, et al. Tacrine-trolox hybrids: a novel class of centrally active, nonhepatotoxic multi-target-directed ligands exerting anticholinesterase and antioxidant activities with low in vivo toxicity. J Med Chem. 2015;58(22):8985–9003.
Alonso D, Dorronsoro I, Rubio L, Muñoz P, García-Palomero E, del Monte M, et al. Donepezil-tacrine hybrid related derivatives as new dual binding site inhibitors of AChE. Bioorg Med Chem. 2005;13(24):6588–97.
Komloova M, Musilek K, Dolezal M, Gunn-Moore F, Kuca K. Structure-activity relationship of quaternary acetylcholinesterase inhibitors—outlook for early myasthenia gravis treatment. Curr Med Chem. 2010;17(17):1810–24.
Sugaya K, Onaga T, Nishijima S, et al. Relationship between serum cholinesterase level and urinary bladder activity in patients with or without overactive bladder and/or neurogenic bladder. Biomed Res. 2007;28(6):287–94.
Sugimoto K, Akiyama T, Shimizu N, Matsumura N, Hashimoto M, Minami T, et al. Acotiamide hydrochloride hydrate added to combination treatment with an alpha-blocker and a cholinergic drug improved the QOL of women with acute urinary retention: case series. Res Rep Urol. 2017;9:141–3.
Hetherington KA, Losek JD. Myasthenia gravis: myasthenia vs. cholinergic crisis. Pediatr Emerg Care. 2005;21(8):546–8. quiz 549–51
Abedin MJ, Sayeed AA, Basher A, Maude RJ, Hoque G, Faiz MA. Open-label randomized clinical trial of atropine bolus injection versus incremental boluses plus infusion for organophosphate poisoning in Bangladesh. J Med Toxicol. 2012;8(2):108–17.
Hameed A, Charles TJ. Cholinergic crisis following treatment of postoperative urinary retention with distigmine bromide. Br J Clin Pract. 1994;48(2):103–4.
Yamanaka S, Fujita I, Murota T, Kawakita M, Matsuda T. Cholinergic crisis following administration of distigmine bromide: a case report. Hinyokika Kiyo. 2002;48(1):21–3. Japanese
Tadara R, Kobayashi M, Nakamura N, et al. Patients confined in bed for an extended period and developing cholinergic crisis following administration of distigmine bromide: report of 3 cases. Nihon Naika Gakkai Zasshi. 1998;87(8):1566–7. Japanese
Kobayashi K, Sekiguchi H, Sato N, Hirose Y. Bowel obstruction-induced cholinergic crisis with progressive respiratory failure following distigmine bromide treatment. Chudoku Kenkyu. 2016;29(1):26–9. Japanese
Takahashi M, Ubukata S, Sato E, Shoji M, Morikawa N, Watanabe H, et al. Acute respiratory failure associated with cholinergic crisis: report of five cases and review of the literature. Nihon Kokyuki Gakkai Zasshi. 2011;49(12):877–84. Japanese
Huang X, Liu WB, Men LN, Feng HY, Li Y, Luo CM, et al. Clinical features of myasthenia gravis in southern China: a retrospective review of 2,154 cases over 22 years. Neurol Sci. 2013;34(6):911–7.
Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol. 2017;27:476–82.
Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:56–61.
Shigematsu K, Nakano H, Watanabe Y. The eye response test alone is sufficient to predict stroke outcome—reintroduction of Japan Coma Scale: a cohort study. BMJ Open. 2013;3(4):e002736.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation presented at: the World Health Organization; June 3–5, 1997; Geneva, Switzerland. Publication WHO/NUT/NCD/98.1.
Wade DT, Collin C. The Barthel ADL index: a standard measure of physical disability? Int Disabil Stud. 1988;10(2):64–7.
Ohta A, Nagai M, Nishina M, Shibazaki S, Ishijima H, Izumida M. Age at the onset of intractable disease: based on a clinical database for patients receiving financial aid for treatment. Nihon Koshu Eisei Zasshi. 2007;54(1):3–14. Japanese
Kalb B, Matell G, Pirskanen R, Lambe M. Epidemiology of myasthenia gravis: a population-based study in Stockholm, Sweden. Neuroepidemiology. 2002;21:221–5.
Tsao TC, Juang YC, Lan RS, et al. Respiratory failure of acute organophosphate and carbamate poisoning. Chest. 1990;98(3):631–6.
Berrih-Aknin S, Frenkian-Cuvelier M, Eymard B. Diagnostic and clinical classification of autoimmune myasthenia gravis. J Autoimmun. 2014;48–49:143–8.
Funding
This work was supported by grants from the Ministry of Health, Labour and Welfare of Japan (H29-Policy-Designated-009 and H29-ICT-Genral-004); the Ministry of Education, Culture, Sports, Science and Technology of Japan (17H04141); and the Japan Agency for Medical Research and Development (AMED).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ohbe, H., Jo, T., Matsui, H. et al. Cholinergic Crisis Caused by Cholinesterase Inhibitors: a Retrospective Nationwide Database Study. J. Med. Toxicol. 14, 237–241 (2018). https://doi.org/10.1007/s13181-018-0669-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13181-018-0669-1