Abstract
The translocator protein (18 kDa) (TSPO) is a mitochondrial transmembrane protein, which has brought attention as a neuroinflammatory biomarker. Positron emission tomography (PET) imaging studies have been done for several decades, since neuroinflammation has been implicated as an important pathophysiology of several common neurologic disorders. However, despite numerous previous studies with positive findings, its clinical significance is not yet clear. Various attempts to overcome the limitations are ongoing, in order to bring acceptance for use in clinics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, neuroinflammation has been suggested to play a major role in the development of multiple neurologic diseases. However, due to the complex mechanism and signaling cascade, yet, little is known about its distinct role in the generation and progression of various neurologic diseases. Moreover, the central nervous system (CNS) has a separate immune system compared with other organs, consists of several distinguishable factors. For example, the blood brain barrier functions as a mechanical barrier, protecting the brain from external pathogens or irritants. Also, there are dedicated immune cells in the nervous system, the microglial cells, which act as the primary defense mechanism of the CNS. Investigating the physiology of neuroinflammation has received remarkable interest for several decades, with numerous studies being conducted in various neurologic diseases.
The translocator protein (18 kDa) (TSPO) is a transmembrane protein known to mainly express in the mitochondria. It is generally involved in the regulation of cholesterol transport and the synthesis of steroid hormones [1]. In the CNS, TSPO is usually expressed in the microglia, along with astrocytes [2]. The expression of TSPO increases under the activation of glial cells, in response to neuron injury. For this reason, TSPO has been currently under investigation as the primary biomarker for neuroinflammation. Various radioligands targeting TSPO for positron emission tomography (PET) imaging have been developed, and have shown promising results in numerous human studies. In this article, we review the associated issues of applicating TSPO targeting radioligands as a PET imaging biomarker for neurodegenerative disorders.
Current Value of TSPO Imaging in Neurologic Diseases
Despite numerous previous studies, TSPO PET imaging is not yet widely applicated in the clinics. For Alzheimer’s disease (AD), TSPO imaging has been attempted since β-amyloid and hyperphosphorylated tau were known to induce neuroinflammation by activating microglia [3, 4]. However, it is controversial whether TSPO PET can identify significant differences between AD patients and normal controls. Some studies have reported increased binding of TSPO targeting radioligands in AD patients compared with normal controls, with positive correlation of TSPO targeting radioligand binding and clinical severity [5, 6]. However, some studies found no differences between AD patients and normal controls [7,8,9], and only weak or no correlation between TSPO and amyloid imaging [10, 11]. It is yet unclear whether neuroinflammation conducts an important role in the development of AD, or whether neuroinflammation takes part in the conversion of mild cognitive impairment to AD. It also lacks reproducibility of correlation between clinical performance factors and TSPO uptake. TSPO PET imaging needs further prospective trials to be conducted, before it may be used for diagnosis, prognosis, and risk stratification for AD.
There are several other studies that investigated neurodegenerative disorders other than AD. For dementia with Lewy bodies, one study demonstrated increased TSPO radioligand binding in the cortex and cerebellum [12]. Several other studies of patients with frontotemporal lobar dementia [13], corticobasal degeneration [14], and progressive supranulcear palsy [15] also described significant increased uptakes of TSPO radioligands, but results are quite preliminary and require further evaluation for clinical application. These studies were done with a small number of patients, and used reference tissue regions that are not free of TSPO binding. For multiple system atrophy, one study reported increased TSPO binding, while one study reported decreased TSPO binding after minocycline treatment [16, 17]. For Parkinson’s disease, one study reported no significant differences of TSPO radioligand binding of the patient group compared with the healthy control group [18]. Overall, there are not enough significant data of TSPO PET imaging for neurodegenerative disorders other than AD.
For ischemic stroke, several studies described increased TSPO radioligand binding in ischemic regions and peri-infarct regions of post-stroke patients [19,20,21]. However, TSPO radioligand binding has diverse spatial and temporal features in stroke patients. Binding peaks at 3–4 weeks after the ischemic event, and also increases in regions remote to the infarction, which is probably associated with Wallerian degeneration [20, 22]. The increased uptake in areas remote to the infarction area were reported to appear even weeks and months after the stroke event. Furthermore, it is yet uncertain whether the post-stroke neuroinflammation has a protective effect, or a proinflammatory effect, in relation to its temporal, regional characteristics. Future studies on TSPO PET imaging in stroke needs to focus on the temporal changes, remote region findings, and its clinical correlation to patients’ prognosis.
In conclusion, the clinical impact and usefulness of TSPO PET imaging is still uncertain. Further studies with larger number of patients are needed in most neurologic disorders.
Nucleotide Polymorphism of the TSPO Gene
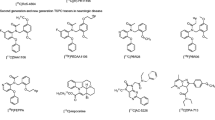
Human application of several second-generation TSPO-binding radioligands, such as 11C-PBR28, 18F-PBR06, 18F-FEPPA, 11C-DAA1106, 11C-DPA713, and 18FPBR111, have revealed substantial variation in binding affinity among normal population. The radioligands bind to the brain as three different clusters, the high-affinity binders (HAB), the low-affinity binders (LAB), and the mixed-affinity binders (MAB). This is due to a variation caused by a common polymorphism (rs6971) in the TSPO gene, which leads to a single amino-acid substitution (Ala147Thr) [23]. Alanine 147 is suggested to contribute to maintaining the helical structure of the transmembrane domain of the TSPO protein. However, the amino acid substitution to Threonine 147 introduces a substantial conformational change, which alters the tertiary structure of TSPO, eventually altering the binding region of TSPO targeting radioligands [24, 25]. The ratio of polymorphism rs6971 among normal subjects depends on ethnicity, in which ~ 70% of the Caucasian is HABs. However, there are no current data on the Korean population. Due to this polymorphism, patients undergoing TSPO PET imaging has to undergo genotyping to know the existence of individual amino-acid substitution, before PET imaging. Recently developed TSPO-binding radioligands such as 18F-FEBMP and 18F-GE-180 are less affected by the polymorphism, but requires further validation [26, 27]. Not only does this polymorphism affect the binding of TSPO targeting radioligands but also it has been suggested that it affects the phenotype of patients. Previous studies have reported that Ala147Thr substitution may affect the hypothalamus-pituitary-adrenal axis regulation, resulting in an increased association with bipolar disorders or panic disorders [28, 29]. In conclusion, a genotyping test is necessary in current TSPO PET imaging studies, for the determination of radioligand binding affinity to different cluster population, and its association with clinical phenotypes.
Methodological Issues of TSPO Radioligand Quantification
Quantification of TSPO-binding radioligands has encountered several challenges. One factor comes from the difficulty of obtaining the accurate measurement of free plasma concentrations. For 11C-PK11195, which is the first generation TSPO radioligand, the fraction of radioligands bound to blood cells are unstable, and also are affected by plasma proteins that are upregulated in reaction to peripheral inflammatory events [30]. This difficulty of obtaining accurate free plasma concentration also applies to several other second-generation TSPO radioligands [31]. Additionally, there exists an irreversible TSPO-binding component in the endothelial cells of venous sinuses, arteries, and the blood brain barrier of the brain [32]. This results in the need for an additional consideration of the presence of an irreversible component, during kinetic modeling. Another obstacle is selecting the reference region for kinetic modeling. Since microglia is distributed in the whole brain, TSPO is also expressed correspondingly. Moreover, normal TSPO expression levels of respective brain regions are yet unknown.
To overcome these problems, several measurement methods have been proposed. First is to use the volume of distribution (VT). However, an accurate measurement of the VT is dependent on the arterial plasma input function, which may be complicated as previously discussed. Second, measuring the standardized uptake value (SUV) at a certain time interval, but which is also sensitive to blood flow. Finally, the distribution volume ratio (DVR) or standardized uptake value ratio (SUVR) may be used by employing a pseudo-reference region, but also has a limitation that the uptake ratio of the pseudo-reference region is hard to know [31, 33, 34].
Conclusion
Multiple previous studies have suggested the value of TSPO PET imaging for the past few decades. However, it has not been widely accepted in clinics, since it is yet challenging to quantify the uptake of TSPO expression. As a consequence, several clinical studies have shown inconclusive or conflicting results. Despite the shortcomings, TSPO PET imaging still has the potential to be applicated in various neurologic diseases. Moreover, recently developed TSPO radioligands have shown promising in vitro results with high signal-to-noise ratio [35]. Prospective longitudinal human studies are needed, that may clarify the role of TSPO PET imaging in neurologic disorders.
References
Papadopoulos V, Baraldi M, Guilarte TR, et al. Translocator protein (18 kDa): new nomenclature for the peripheral-type benzodiazepine receptor based on its structure and molecular function. Trends Pharmacol Sci. 2006;27:402–9.
Casellas P, Galiegue S, Basile AS. Peripheral benzodiazepine receptors and mitochondrial function. Neurochem Int. 2002;40:475–86.
Maezawa I, Zimin PI, Wulff H, Jin LW. Amyloid-beta protein oligomer at low nanomolar concentrations activates microglia and induces microglial neurotoxicity. J Biol Chem. 2011;286:3693–706.
Morales I, Jimenez JM, Mancilla M, Maccioni RB. Tau oligomers and fibrils induce activation of microglial cells. J Alzheimers Dis. 2013;37:849–56.
Edison P, Archer HA, Gerhard A, et al. Microglia, amyloid, and cognition in Alzheimer’s disease: an [11C](R)PK11195-PET and [11C]PIB-PET study. Neurobiol Dis. 2008;32:412–9.
Yokokura M, Mori N, Yagi S, et al. In vivo changes in microglial activation and amyloid deposits in brain regions with hypometabolism in Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2011;38:343–51.
Wiley CA, Lopresti BJ, Venneti S, et al. Carbon 11-labeled Pittsburgh compound B and carbon 11-labeled (R)-PK11195 positron emission tomographic imaging in Alzheimer disease. Arch Neurol. 2009;66:60–7.
Schuitemaker A, Kropholler MA, Boellaard R, et al. Microglial activation in Alzheimer’s disease: an (R)-[11C]PK11195 positron emission tomography study. Neurobiol Aging. 2013;34:128–36.
Stefaniak J, O’Brien J. Imaging of neuroinflammation in dementia: a review. J Neurol Neurosurg Psychiatry. 2016;87:21–8.
Carter SF, Scholl M, Almkvist O, et al. Evidence for astrocytosis in prodromal Alzheimer disease provided by 11C-deuterium-L-deprenyl: a multitracer PET paradigm combining 11C-Pittsburgh compound B and 18F-FDG. J Nucl Med. 2012;53:37–46.
Kreisl WC, Lyoo CH, McGwier M, et al. In vivo radioligand binding to translocator protein correlates with severity of Alzheimer’s disease. Brain. 2013;136:2228–38.
Iannaccone S, Cerami C, Alessio M, et al. In vivo microglia activation in very early dementia with Lewy bodies, comparison with Parkinson’s disease. Parkinsonism Relat Disord. 2013;19:47–52.
Cagnin A, Rossor M, Sampson EL, et al. In vivo detection of microglial activation in frontotemporal dementia. Ann Neurol. 2004;56:894–7.
Gerhard A, Watts J, Trender-Gerhard I, et al. In vivo imaging of microglial activation with [11C](R)-PK11195 PET in corticobasal degeneration. Mov Disord. 2004;19:1221–6.
Gerhard A, Trender-Gerhard I, Turkheimer F, et al. In vivo imaging of microglial activation with [11C](R)-PK11195 PET in progressive supranuclear palsy. Mov Disord. 2006;21:89–93.
Gerhard A, Banati RB, Goerres GB, et al. [11C](R)-PK11195 PET imaging of microglial activation in multiple system atrophy. Neurology. 2003;61:686–9.
Dodel R, Spottke A, Gerhard A, et al. Minocycline 1-year therapy in multiple-system-atrophy: effect on clinical symptoms and [11C] (R)-PK11195 PET (MEMSA-trial). Mov Disord. 2010;25:97–107.
Koshimori Y, Ko JH, Mizrahi R, et al. Imaging striatal microglial activation in patients with Parkinson’s disease. PLoS One. 2015;10:e0138721.
Gulyas B, Toth M, Schain M, et al. Evolution of microglial activation in ischaemic core and peri-infarct regions after stroke: a PET study with the TSPO molecular imaging biomarker [11C]vinpocetine. J Neurol Sci. 2012;320:110–7.
Thiel A, Radlinska BA, Paquette C, et al. The temporal dynamics of poststroke neuroinflammation: a longitudinal diffusion tensor imaging-guided PET study with 11C-PK11195 in acute subcortical stroke. J Nucl Med. 2010;51:1404–12.
Gulyas B, Toth M, Vas A, et al. Visualising neuroinflammation in post-stroke patients: a comparative PET study with the TSPO molecular imaging biomarkers [11C]PK11195 and [11C]vinpocetine. Curr Radiopharm. 2012;5:19–28.
Block F, Dihne M, Loos M. Inflammation in areas of remote changes following focal brain lesion. Prog Neurobiol. 2005;75:342–65.
Owen DR, Yeo AJ, Gunn RN, et al. An 18-kDa translocator protein (TSPO) polymorphism explains differences in binding affinity of the PET radioligand PBR28. J Cereb Blood Flow Metab. 2012;32:1–5.
Murail S, Robert JC, Coic YM, et al. Secondary and tertiary structures of the transmembrane domains of the translocator protein TSPO determined by NMR. Stabilization of the TSPO tertiary fold upon ligand binding. Biochim Biophys Acta. 1778;2008:1375–81.
Li F, Liu J, Zheng Y, et al. Crystal structures of translocator protein (TSPO) and mutant mimic of a human polymorphism. Science. 2015;347:555–8.
Tiwari AK, Ji B, Yui J, et al. [18F]FEBMP: positron emission tomography imaging of TSPO in a model of neuroinflammation in rats, and in vitro autoradiograms of the human brain. Theranostics. 2015;5:961–9.
Fan Z, Calsolaro V, Atkinson RA, et al. Flutriciclamide (18F-GE180) PET: first-in-human PET study of novel third-generation in vivo marker of human translocator protein. J Nucl Med. 2016;57:1753–9.
Colasanti A, Owen DR, Grozeva D, et al. Bipolar disorder is associated with the rs6971 polymorphism in the gene encoding 18 kDa translocator protein (TSPO). Psychoneuroendocrinology. 2013;38:2826–9.
Nakamura K, Yamada K, Iwayama Y, et al. Evidence that variation in the peripheral benzodiazepine receptor (PBR) gene influences susceptibility to panic disorder. Am J Med Genet B Neuropsychiatr Genet. 2006;141B:222–6.
Lockhart A, Davis B, Matthews JC, et al. The peripheral benzodiazepine receptor ligand PK11195 binds with high affinity to the acute phase reactant alpha1-acid glycoprotein: implications for the use of the ligand as a CNS inflammatory marker. Nucl Med Biol. 2003;30:199–206.
Turkheimer FE, Rizzo G, Bloomfield PS, et al. The methodology of TSPO imaging with positron emission tomography. Biochem Soc Trans. 2015;43:586–92.
Rizzo G, Veronese M, Tonietto M, et al. Kinetic modeling without accounting for the vascular component impairs the quantification of [11C]PBR28 brain PET data. J Cereb Blood Flow Metab. 2014;34:1060–9.
Owen DR, Guo Q, Rabiner EA, Gunn RN. The impact of the rs6971 polymorphism in TSPO for quantification and study design. Clin Transl Imaging 2015;3:417–22.
Lyoo CH, Ikawa M, Liow JS, et al. Cerebellum can serve as a pseudo-reference region in Alzheimer disease to detect neuroinflammation measured with PET radioligand binding to translocator protein. J Nucl Med. 2015;56:701–6.
Moon BS, Kim BS, Park C, et al. [18F]Fluoromethyl-PBR28 as a potential radiotracer for TSPO: preclinical comparison with [11C]PBR28 in a rat model of neuroinflammation. Bioconjug Chem. 2014;25:442–50.
Funding
This work was supported by a grant from the Basic Science Research Program through the National Research Foundation of Korea (NRF) (grant no. 2016R1D1A1A02937028).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
This work was supported by a grant from the Basic Science Research Program through the National Research Foundation of Korea (NRF) (no. 2016R1D1A1A02937028).
Ethical Approval
This article does not contain any studies with human participants or animals performed by the author.
Informed consent
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Song, Y.S. Perspectives in TSPO PET Imaging for Neurologic Diseases. Nucl Med Mol Imaging 53, 382–385 (2019). https://doi.org/10.1007/s13139-019-00620-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-019-00620-y