Abstract
Purpose
18F-fluorodeoxyglucose-positron emission tomography (FDG-PET) imaging is well known to have clinical significance in the initial staging and response evaluation of the many kinds of neoplasms. However, its role in the pediatric neuroblastoma is not clearly defined. In the present study, the clinical significance of FDG-PET/computed tomography (CT) in 123I- or 131I-metaiodobenzylguanidine (MIBG)-avid pediatric neuroblastoma was investigated.
Methods
Twenty patients with neuroblastoma who undertook pretreatment FDG PET/CT at our institute between 2008 and 2015 and showed MIBG avidity were retrospectively enrolled in the present study. Clinical information—including histopathology, and serum markers—and several PET parameters—including SUVmax of the primary lesion (Psuv), target-to-background ratio (TBR), metabolic tumor volume (MTV), and coefficient of variation (CV)—were analyzed. The prognostic effect of PET parameters was evaluated in terms of progression-free survival (PFS).
Results
Total 20 patients (4.5 ± 3.5 years) were divided as two groups by disease progression. Six patients (30.0 %) experienced disease progression and one patient (5.0 %) died during follow-up period. There were not statistically significant in age, stage, MYCN status, primary tumor size, serum lactate dehydrogenase (LDH), neuron-specific enolase (NSE), and ferritin level between two groups with progression or no progression. However, Psuv (p = 0.017), TBR (p = 0.09), MTV (p = 0.02), and CV (p = 0.036) showed significant differences between two groups. In univariate analysis, PFS was significantly associated with Psuv (p = 0.021) and TBR (p = 0.023).
Conclusions
FDG-PET parameters were significantly related with progression of neuroblastoma. FDG-PET/CT may have the potential as a valuable modality for evaluating prognosis in the patients with MIBG-avid pediatric neuroblastoma.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Neuroblastoma is the most common extracranial solid tumor of childhood age and the most frequent malignancy diagnosed during infancy [1]. It represents 8–10 % of all childhood malignancies and about 15 % of all mortalities of malignancy in children [2]. Five-year survival rate in children less than 1 year of age reported in European population is 91 %, whereas it is less than 60 % in older children [3]. One of the most important prognostic factors is the disease extent; thus, various imaging modalities are employed to stage the disease and subsequently to identify the extent of unresected tumor mass or to evaluate the effectiveness of therapy [4]. Some of the commonly used imaging modalities are plain radiography, ultrasonography, computed tomography (CT), magnetic resonance imaging (MRI), 123I- or 131I-metaiodobenzylguanidine (MIBG) scintigraphy, bone scintigraphy and positron emission tomography (PET) [4]. Conventional imaging with 123I- or 131I-MIBG is a well-established and standard method for staging of neuroblastoma with reported sensitivity and specificity of above 90 % [5–7]. As about 70 % of neuroblastoma only concentrates MIBG, however, there may be false-negative results associated with radioiodinated MIBG scan [8]. Therefore, due to these false-negative or false-positive issues, several studies have compared the MIBG scan with 18F-fluorodeoxyglucose (FDG)-PET. Some studies have reported that MIBG scan is superior to FDG-PET in the tumor evaluation, and others have shown opposite results. FDG-PET is well known as a very useful imaging modality in the clinical oncology field. Numerous studies have reported the clinical significance of FDG-PET in the diagnosis, treatment response, and prognosis evaluation of various kinds of tumors [9–11]. Especially, in the pediatric malignancies, the role of FDG-PET has also been reported in the several studies [12, 13]. However, its clinical role for neuroblastoma still remains less clear due to the paucity of published studies which have presented the significance of FDG-PET [14–16]. There are just a few studies which have investigated the prognostic evaluation of FDG-PET in neuroblastoma patients [17, 18]. However, no FDG-PET studies have been performed in patients with MIBG-avid neuroblastoma. It is well known that MIBG uptake of neuroblastoma is not related to tumor differentiation but the noradrenalin transporter system [18, 19]. However, it is not still clear why some of the neuroblastoma present less expression of noradrenaline transporter gene. Therefore, it may be worthy of investigating the value of FDG-PET under the same condition of MIBG uptake. We have performed this study to evaluate the prognostic value of pretreatment FDG-PET in patients with MIBG-avid neuroblastoma.
Materials and Methods
Patients
Sixty-five patients who pathologically diagnosed as neuroblastoma or ganglioneuroblastoma and performed FDG-PET/CT at our institute from January 2008 to December 2015 were retrospectively reviewed. The 20 patients who have done initial diagnostic workup including pretreatment FDG-PET/CT at our institute and shown MIBG avidity were included in the present study. MIBG avidity was defined when the tumor showed MIBG uptake above blood pool in MIBG scintigraphy. For the analysis, clinical information including age, sex, histopathology, stage, serum lactate dehydrogenase (LDH), neuron-specific enolase (NSE), ferritin, primary tumor size, bone marrow involvement, and several PET parameters including SUVmax of the primary lesion (Psuv), target-to-background ratio (TBR), metabolic tumor volume (MTV), and coefficient of variation (CV) were investigated. This study was approved by the institutional review board of our hospital, and the need for written informed consent was waived.
FDG-PET/CT Imaging Protocol
All patients were given FDG-PET scans using a Siemens PET scanner (Biograph 40 True-point; Siemens, Knoxville, TN, USA). After fasting for at least 6 h, 18F-FDG of 5.18 MBq/kg (0.14 mCi/kg) was administered intravenously and the image acquisition was started at 60 min after the injection. Serum glucose levels were less than 150 mg/dL at the time of administration of FDG in all patients. A prior CT scan was obtained during shallow breathing from the skull base to the proximal thigh by using a low-dose CT protocol for the purpose of attenuation correction. The consecutive emission scan was acquired after the CT scans in three-dimensional mode at each bed position (2.5 min/bed, 21.6-cm increments). PET images were corrected for attenuation and reconstructed onto a matrix of 128 × 128 using the three-dimensional ordered-subsets expectation maximization algorithm (2 iterations, 21 subsets, 7-mm post-smoothing).
FDG-PET Data Analysis
All PET images were reviewed by the experienced nuclear medicine physician using commercial imaging software (Syngo.via, VA 30; Siemens Healthcare, Erlangen, Germany). To evaluate FDG uptake of neuroblastoma, spherical volume of interests (VOIs) were drawn for the primary tumor for each patient. In each VOI, the maximum standardized uptake value (SUVmax) was measured and the SUVmax of the primary tumor was calculated. To analyze target-to-background ratio (TBR), a background mean SUV was measured in the normal liver parenchyma. A spherical VOI with 3.0 cm radius was placed in the right inferior hepatic lobe (segment 5/6) avoiding large vessels such as the portal vein (Fig. 1). In patients with hepatic invasion or metastasis, the VOI was drawn in a hepatic location where metastatic lesions were not detected by other imaging modalities such as CT or MRI. Based on these metabolic values, parameters for analysis of FDG-PET/CT were calculated; the SUVmax of the primary tumor (Psuv), the uptake ratio of Psuv to mean SUV of normal liver (TBR), and metabolic tumor volume (MTV). MTV was calculated on SUV threshold 2.5 using Syngo.via software. In addition, coefficient of variation (CV) that has been reported to predict therapy response and prognosis in other cancers was chosen for intratumoral FDG heterogeneity (IFH) analysis. The CV is an intuitive and feasible parameter as against complexity of other statistics-based heterogeneity parameters. The CV was defined as the ratio of the standard deviation (SD) of the SUVmax to the SUVmean within the automatically delineated tumor volume calculated using SUV threshold 2.5.
Statistical Analysis
To evaluate a difference of clinical factors and FDG-PET parameters between two groups by progression, Mann–Whitney U test and Chi-square test were used. For the prognostic evaluation of clinical factors and FDG-PET parameters, progression-free survival (PFS) was chosen as end point. PFS was defined as the time from diagnosis to first evidence of progression or relapse. Data were censored if the patients were alive and free of progression during the follow-up period. Optimal thresholds of continuous variables for distinguishing low and high risk in Kaplan-Meier analysis were determined with receiver operating characteristics (ROC) curves analysis. Kaplan-Meier method was used to calculate cumulative PFS according to FDG-PET parameters. Univariate regression analysis using the log-rank test was used to assess the value of all the prognostic factors for the prediction of PFS. A p value of less than 0.05 was considered statistically significant and all analysis was performed using SPSS software for Windows (version 22.0; IBM SPSS, Somers, NY, USA).
Results
Patients’ Characteristics
The demographic and clinical characteristics of patients are summarized in Table 1. Of a total of 20 patients (mean age, 4.5 ± 3.5 years; age range, 1 month to 14 years; male:female ratio = 1.5:1), 6 patients (30 %) experienced disease progression and 1 patient (5 %) died during follow-up period. Survival time was defined as the time from the day of the first diagnosis with pathologic result to the day of detection of disease progression (or death) or to the day of the last follow-up visit at our medical center. The disease progression was defined as ≥20 % increase in the size of known tumor based on the Response Evaluation Criteria In Solid Tumor (RECIST) or detection of newly developmental metastases on follow-up imaging examinations such as CT or MRI after initial pathologic diagnosis. The patients were divided into two groups depending on either the presence of disease progression into progression or no progression. There were not statistically significant differences in age, stage, MYCN gene status, primary tumor size, serum NSE, LDH and ferritin level between two different groups with disease progression or non-progression. However, FDG-PET parameters including Psuv, TBR, MTV, and CV did show significant differences between the two groups (p = 0.017, 0.09, 0.02, and 0.036). The Psuv (11.5 ± 8.9 vs 5.4 ± 2.7), TBR (9.1 ± 5.9 vs 5.3 ± 2.9), MTV (174.5 ± 129.9 vs 98.01 ± 126.7), and CV (0.34 ± 0.20 vs 0.13 ± 0.1) values in the disease progression group were remarkably higher compared with the non-progression group and statistically significant.
Prognostic Evaluation of FDG-PET Parameters
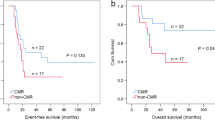
Data on progression were available for six patients with a median PFS of 22.33 ± 16.54 months. The selected cutoff values of Psuv, TBR, MTV, and CV for prognostic analysis were 7.78, 5.54, 33.46, and 0.11 respectively. Psuv (p = 0.021) and TBR (p = 0.023) among four FDG-PET parameters were predictive for PFS in univariate analysis using log-rank test. Although MTV showed a significant trend, it was not significant (p = 0.074). CV was not statistically significant (p = 0.111). Survival curves for low- and high-risk subgroups determined by optimal cutoff are depicted in Fig. 2. The corresponding thresholds with p values for dichotomized variables are given in Table 2. The same way was applied to clinical factors including age, sex, stage, serum NSE and ferritin levels, but there was not significant. However, the primary tumor size and LDH which are well known as representative prognostic factors of pediatric neuroblastoma showed a significant trend (p < 0.1), though statistically insignificant.
Discussion
In this study, we investigated the prognostic value of diagnostic FDG-PET/CT before any treatment in MIBG-avid pediatric neuroblastoma. Psuv and TBR among FDG-PET parameters were predictive for progression. These results suggest that FDG-PET may be a useful and potential predicator for disease progression or recurrence in pediatric neuroblastoma patients.
Evaluation of prognosis is of great importance so that the clinician properly figures out a patient and decides the effective treatment regimen. FDG PET is well known as a useful predictive study in many malignant tumors such as lymphoma, lung cancer, breast cancer, and so on [20–22]. However, for pediatric neuroblastoma, there are only a few reports that have evaluated the prognostic significance of FDG PET [17, 18]. Many studies have reported that MIBG scintigraphy is the most sensitive and specific method for staging and response evaluation in neuroblastoma [23, 24]. Therefore, the radioiodine-labeled MIBG scan has been used in the diagnosis and response evaluation and considered as the “gold standard” in the staging of neuroblastoma for several decades. Even several studies have reported that radioiodine-labeled MIBG scintigraphy is superior to FDG-PET in the assessment of stage IV neuroblastomas because of the better detection of bone or bone marrow metastases [15, 17]. However, there are several limitations associated with the use of radiolabeled MIBG in the diagnostic workup of pediatric neuroblastoma that present false-positive or false-negative findings [15]. Moreover, this technique requires correlation with morphological imaging modalities in most of the cases and also involves patient preparation precautions [25].
Recently, several studies have reported that FDG-PET scan was especially useful in patients with tumors that showed less MIBG uptake [15]. There are several reports showing importance of FDG-PET scan in neuroblastoma which MIBG scan failed to detect the lesions [26, 27]. Generally, poorly differentiated malignancy tends to show higher FDG uptake than the well-differentiated tumors [28]. It is just as well in the case of neuroblastoma. Poorly differentiated neuroblastoma presents high FDG uptake compared to differentiated neuroblastoma and ganglioneuroblastoma [18]. Contrary to this, MIBG uptake of neuroblastoma is not related to tumor differentiation but the noradrenalin transporter system [17–19]. That is, MIBG uptake does not suggest tumor differentiation and hence it is difficult to show prognostic value. Eventually, it is concluded that FDG uptake of neuroblastoma reflects better tumor aggressiveness than MIBG uptake and has much relevance to prognosis of patient. Nevertheless, MIBG avidity that has a role as a tumor-specific tracer in neuroblastoma is an important factor that cannot be ignored. To evaluate the prognostic value of pretreatment FDG-PET in those patients with neuroblastoma having a similar degree of MIBG uptake, we have performed this study.
Our data showed that parameters from FDG PET were predictive in the prognosis evaluation of neuroblastoma. Psuv and TBR, which are representative parameters of FDG-PET, were significant prognostic factors for predicting PFS beyond other conventional clinical prognostic factors. Although MTV showed a significant trend, it was statistically insignificant. These results correspond with previously noted findings in other malignant tumors. Numerous studies have reported that FDG-PET parameters such as SUVmax, MTV, and TBR were predictive to PFS or overall survival (OS) in various malignant tumors [29, 30]. We have also analyzed CV, which is one of representative parameters of intratumoral FDG heterogeneity (IFH). It is a well-known fact that FDG uptake pattern within a tumor is not homogenous, and several studies have reported that IFH has the potential as a new biomarker of prognosis [31, 32]. In this study, however, CV was not significant. This result may be due to a small number of subjects, and so further study with more patients is needed. Actually, clinical values such as age, primary tumor size, MYCN, and serum markers are already well-known prognostic factors in pediatric neuroblastoma. In this study, the values did not present significant meaning because of a small number of patients, except for primary tumor size and serum LDH which showed significant trends. Nevertheless, however, in the way that FDG-PET parameters were predictive for PFS in this small subject group, parameters of diagnostic FDG-PET before any treatment may have potential as prognostic factors in pediatric neuroblastoma. In our study, Psuv and TBR were significant to predict prognosis compared with other FDG-PET parameters which did not show statistical significance. Figure 3 is a representative case which shows high MTV and IFH, but relatively low Psuv. The Psuv in this case was lower than a optimal threshold for distinguishing low and high risk in Kaplan-Meier analysis (Psuv 6.3, threshold 7.78), and both MTV and CV were over the thresholds (MTV 147.5, threshold 33.46; CV 0.26, threshold 0.11). This patient did not show disease progression during the follow-up period.
The representative case showing the predictive value of the SUVmax of primary tumor (Psuv) compared to metabolic tumor volume (MTV), and coefficient of variation (CV). The patient showed low Psuv (6.3, threshold 7.78), high MTV (147.5, threshold 33.46) and high CV (0.26, threshold 0.11) based on the optimal thresholds. This patient is under observation without any evidence of disease progression
There are several limitations to our study. First, it was not a prospectively designed study, but a retrospective study from a single center with a relatively small population. Thus, there is a possibility of selection bias. Secondly, the number of patients with initial diagnostic FDG-PET scans was too low, which may cause deviation of significance in statistical analysis. Thirdly, due to the small number of patients, we could not perform the multivariate analysis and also compare the difference of the FDG PET parameters according to the stage or histopathology. A multicenter prospective study would be needed to validate the clinical significance of FDG PET.
In summary, the present study demonstrates that some parameters from pretreatment FDG-PET were significant for predicting PFS in patients with MIBG-avid neuroblastoma. FDG-PET may have the potential to suggest prognostic information in pediatric neuroblastoma.
References
Mullassery D, Dominici C, Jesudason EC, McDowell HP, Losty PD. Neuroblastoma: contemporary management. Arch Dis Child. 2009;94:177–85.
Colon NC, Chung DH. Neuroblastoma. Adv Pediatr. 2011;58:297–311.
Gatta G, Botta L, Rossi S, Aareleid T, Bielska-Lasota M, Clavel J, et al. Childhood cancer survival in Europe 1999–2007: results of EUROCARE-5-a population-based study. Lancet Oncol. 2014;15:35–47.
Liu W, Zheng J, Li Q. Application of imaging modalities for evaluating neuroblastoma. J Pediatr Endocrinol Metab. 2013;26:1015–20.
Biermann M, Schwarzlmuller T, Fasmer KE, Reitan BC, Johnsen B, Rosendahl K. Is there a role for PET-CT and SPECT-CT in pediatric oncology? Acta Radiol. 2013;54:1037–45.
Mueller WP, Coppenrath E, Pfluger T. Nuclear medicine and multimodality imaging of pediatric neuroblastoma. Pediatr Radiol. 2013;43:418–27.
Jacobson AF, Deng H, Lombard J, Lessig HJ, Black RR. 123I-meta-iodobenzylguanidine scintigraphy for the detection of neuroblastoma and pheochromocytoma: results of a meta-analysis. J Clin Endocrinol Metab. 2010;95:2596–606.
Ley S, Ley-Zaporozhan J, Gunther P, Deubzer HE, Witt O, Schenk JP. Neuroblastoma imaging. RoFo : Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 2011;183:217–25.
Avril S, Muzic RF, Plecha D, Traughber BJ, Vinayak S, Avril N. 18F-FDG PET/CT for monitoring of treatment response in breast cancer. J Nucl Med. 2016;57:34S–9.
Liao S, Penney BC, Wroblewski K, Zhang H, Simon CA, Kampalath R, et al. Prognostic value of metabolic tumor burden on 18F-FDG PET in nonsurgical patients with non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2012;39:27–38.
Etchebehere E, Macapinlac HA. The role of 18F-FDG PET/CT in diagnosis and staging of musculoskeletal soft tissue sarcomas. Clin Transl Imaging. 2015;3:111–21.
Uslu L, Donig J, Link M, Rosenberg J, Quon A, Daldrup-Link HE. Value of 18F-FDG PET and PET/CT for evaluation of pediatric malignancies. J Nucl Med. 2015;56:274–86.
Sioka C. The utility of FDG PET in diagnosis and follow-up of lymphoma in childhood. Eur J Pediatr. 2013;172:733–8.
Choi YJ, Hwang HS, Kim HJ, Jeong YH, Cho A, Lee JH, et al. 18F-FDG PET as a single imaging modality in pediatric neuroblastoma: comparison with abdomen CT and bone scintigraphy. Ann Nucl Med. 2014;28:304–13.
Sharp SE, Shulkin BL, Gelfand MJ, Salisbury S, Furman WL. 123I-MIBG scintigraphy and 18F-FDG PET in neuroblastoma. J Nucl Med. 2009;50:1237–43.
Dhull VS, Sharma P, Patel C, Kundu P, Agarwala S, Bakhshi S, et al. Diagnostic value of 18F-FDG PET/CT in paediatric neuroblastoma: comparison with 131I-MIBG scintigraphy. Nucl Med Commun. 2015;36:1007–13.
Papathanasiou ND, Gaze MN, Sullivan K, Aldridge M, Waddington W, Almuhaideb A, et al. 18F-FDG PET/CT and 123I-metaiodobenzylguanidine imaging in high-risk neuroblastoma: diagnostic comparison and survival analysis. J Nucl Med. 2011;52:519–25.
Lee JW, Cho A, Yun M, Lee JD, Lyu CJ, Kang WJ. Prognostic value of pretreatment FDG PET in pediatric neuroblastoma. Eur J Radiol. 2015;84:2633–9.
Lode HN, Bruchelt G, Seitz G, Gebhardt S, Gekeler V, Niethammer D, et al. Reverse transcriptase-polymerase chain reaction (RT-PCR) analysis of monoamine transporters in neuroblastoma cell lines: correlations to meta-iodobenzylguanidine (MIBG) uptake and tyrosine hydroxylase gene expression. Eur J Cancer. 1995;31:586–90.
Itti E, Lin C, Dupuis J, Paone G, Capacchione D, Rahmouni A, et al. Prognostic value of interim 18F-FDG PET in patients with diffuse large B-Cell lymphoma: SUV-based assessment at 4 cycles of chemotherapy. J Nucl Med. 2009;50:527–33.
Pandit N, Gonen M, Krug L, Larson SM. Prognostic value of [18F] FDG-PET imaging in small cell lung cancer. Eur J Nucl Med Mol Imaging. 2003;30:78–84.
Buck A, Schirrmeister H, Kühn T, Shen C, Kalker T, Kotzerke J, et al. FDG uptake in breast cancer: correlation with biological and clinical prognostic parameters. Eur J Nucl Med Mol Imaging. 2002;29:1317–23.
Matthay KK, Shulkin B, Ladenstein R, Michon J, Giammarile F, Lewington V, et al. Criteria for evaluation of disease extent by (123)I-metaiodobenzylguanidine scans in neuroblastoma: a report for the international neuroblastoma risk group (INRG) task force. Br J Cancer. 2010;102:1319–26.
Yanik GA, Parisi MT, Shulkin BL, Naranjo A, Kreissman SG, London WB, et al. Semiquantitative mIBG scoring as a prognostic indicator in patients with stage 4 neuroblastoma: a report from the children’s oncology group. J Nucl Med. 2013;54:541–8.
Taggart D, Dubois S, Matthay KK. Radiolabeled metaiodobenzylguanidine for imaging and therapy of neuroblastoma. Q J Nucl Med Mol Imaging. 2008;52:403–18.
Piccardo A, Lopci E, Conte M, Foppiani L, Garaventa A, Cabria M, et al. PET/CT imaging in neuroblastoma. Q J Nucl Med Mol Imaging. 2013;57:29–39.
Koopmans KP, Neels ON, Kema IP, Elsinga PH, Links TP, de Vries EG, et al. Molecular imaging in neuroendocrine tumors: molecular uptake mechanisms and clinical results. Crit Rev Oncol Hematol. 2009;71:199–213.
de Geus-Oei L-F, van Krieken JHJ, Aliredjo RP, Krabbe PF, Frielink C, Verhagen AF, et al. Biological correlates of FDG uptake in non-small cell lung cancer. Lung Cancer. 2007;55:79–87.
Im H-J, Pak K, Cheon GJ, Kang KW, Kim S-J, Kim I-J, et al. Prognostic value of volumetric parameters of 18F-FDG PET in non-small-cell lung cancer: a meta-analysis. Eur J Nucl Med Mol Imaging. 2015;42:241–51.
Lee JW, Kang CM, Choi HJ, Lee WJ, Song SY, Lee J-H, et al. Prognostic value of metabolic tumor volume and total lesion glycolysis on preoperative 18F-FDG PET/CT in patients with pancreatic cancer. J Nucl Med. 2014;55:898–904.
Lee M, Lee H, Cheon GJ, Kim HS, Chung HH, Kim J-W, et al. Prognostic value of preoperative intratumoral FDG uptake heterogeneity in patients with epithelial ovarian cancer. Eur Radiol. 2016; doi:10.1007/s00330-016-4368-5.
Hyun SH, Kim HS, Choi SH, Choi DW, Lee JK, Lee KH, et al. Intratumoral heterogeneity of 18F-FDG uptake predicts survival in patients with pancreatic ductal adenocarcinoma. Eur J Nucl Med Mol Imaging. 2016;43:1461–8.
Acknowledgments
Seo Young Kang, Muhammad Kashif Rahim, Yong-il Kim, Gi Jeong Cheon, Hyoung Jin Kang, Hee Young Shin, Keon Wook Kang, June-Key Chung, E. Edmund Kim, and Dong Soo Lee declare that this manuscript has not been published or presented elsewhere in part or in entirety, and is not under consideration by another journal. This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number : HI14C1072).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Seo Young Kang, Muhammad Kashif Rahim, Yong-il Kim, Gi Jeong Cheon, Hyoung Jin Kang, Hee Young Shin, Keon Wook Kang, June-Key Chung, E. Edmund Kim, and Dong Soo Lee declare that they have no conflict of interest.
Ethical Statement
All procedures followed were performed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013. The study design and exemption of informed consent were approved by the Institutional Review Board of Seoul National University Hospital (IRB No. 1407-148-597).
Rights and permissions
About this article
Cite this article
Kang, S.Y., Rahim, M.K., Kim, Yi. et al. Clinical Significance of Pretreatment FDG PET/CT in MIBG-Avid Pediatric Neuroblastoma. Nucl Med Mol Imaging 51, 154–160 (2017). https://doi.org/10.1007/s13139-016-0451-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-016-0451-8