Abstract
The link between obesity-induced systemic inflammation and decreased insulin signalling is well-known. It is also known that peripherally produced inflammatory cytokines can cross the blood-brain barrier, resulting in the release of neurotoxins that can ultimately lead to the demise of central nervous system integrity. A high-mesembrine Sceletium tortuosum extract was recently shown to possess cytoprotective and mild anti-inflammatory properties in monocytes and to target specific p450 enzymes to reduce adrenal glucocorticoid synthesis. This is significant since the aetiology of both obesity and diabetes is linked to inflammation and excess glucocorticoid production. Given the interlinked nature of glucocorticoid action and inflammation, central immunomodulatory effects of two Sceletium tortuosum extracts prepared by different extraction methods were investigated. Human astrocytes were pre-treated for 30 min, before exposure to Escherichia coli lipopolysaccharide for 23.5 h (in the presence of treatment). Cytotoxicity, mitotoxicity and cytokine responses (basally and in response to inflammatory stimulus) were assessed. In addition, total polyphenol content, antioxidant capacity and selected neural enzyme inhibition capacity were assessed for both extracts. The high-mesembrine Sceletium extract exerted cytoprotective and anti-inflammatory effects. In contrast, the high delta7-mesembrenone extract, rich in polyphenols, exhibited potent antioxidant effect, although with relatively higher risk of adverse effects with overdose. We conclude that both Sceletium tortuosum extracts may be employed as either a preventative supplement or complimentary treatment in the context of obesity and diabetes; however, current data also highlights the impact that extraction methods can have on plant product mechanism of action.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of diabetes worldwide is predicted to reach 366 million by 2030 [34]. The major focus of diabetes management is glycaemic control, which commences relatively late in the developmental time frame of the disease. In contrast, oxidative stress and chronic systemic inflammation are present much earlier and responsible for the development of widespread insulin resistance, ultimately resulting in the establishment of type 2 diabetes (T2D) [25].
In addition, peripheral inflammation is linked to cognitive decline, via crosstalk with neuroinflammatory processes. This has been confirmed by multiple studies, which have reported an increased risk of dementia associated with obesity [2, 15, 20]. This phenomenon has been termed “type 3 diabetes” (T3D) [19] and results from overlapping pathways of inflammation, oxidative stress and mitochondrial dysfunction, which form the basis of obesity, type 2 diabetes and neurodegeneration [23].
T3D results from peripheral inflammation, which triggers neuroinflammatory responses via gene expression profiling [32]. In addition, inflammation within the central nervous system is attributed to damage to the blood-brain barrier (BBB), resulting from migration of leukocytes into the central compartment. Compromised BBB integrity has been observed in conjunction with hippocampal-dependent cognitive decline in a rat model of diet-induced obesity [33].
Both inflammation and oxidative stress seldom occur in isolation and are characteristic of underlying pathology. The relationship between the two is often circular, with no determinable starting point: inflammation may cause oxidative stress in some settings, while in other cases, the converse occurs [4]. Relevant to the topic of diabetes, antioxidant treatment has been shown to attenuate the harmful effects of high-glucose exposure in vitro in a simulated blood-brain-barrier model [1].
The effectiveness of plant medicines with anti-inflammatory capacity in the context of chronic disease has also been the focus of many research groups for some time [18, 22]. One of these potential plant medicines, Sceletium tortuosum, was traditionally used by the Khoisan people of Southern Africa for pain relief [14, 21], but its commercial availability has significantly increased recently after reports suggesting that it may have anti-depressive and anxiolytic properties [11, 27].
A high-mesembrine Sceletium tortuosum extract was recently shown to possess cytoprotective and mild anti-inflammatory properties in the setting of acute inflammation in the peripheral compartment. In addition, it has also been shown to target specific enzymes in the adrenal cortical steroid synthesis pathway, to reduce glucocorticoid synthesis [30]. In the context of diabetes and obesity, this is significant since the aetiology of both conditions is linked to chronically elevated pro-inflammatory cytokine and glucocorticoid levels.
Given the illustrated benefits which relate to chronic diseases such as diabetes, and given Sceletium tortuosum’s known psychoactive nature, we hypothesised that the plant could potentially alleviate neuroinflammation and central oxidative stress associated with chronic disease.
The aims of the current study were therefore to determine the effects of two different Sceletium tortuosum extracts (varying in alkaloidal composition) on human astrocyte viability, both basally and in the presence of an acute pro-inflammatory stimulus (Escherichia coli lipopolysaccharide, LPS). Furthermore, differences in the functional capacity of these neuroimmune cells before and after pre-treatment with Sceletium tortuosum extracts were assessed in terms of their capacity for inflammatory cytokine secretion. To further elucidate the mechanisms of action by which different Sceletium extracts exert beneficial effects, their inhibition of selected neural enzymes was assessed. Antioxidant properties of extracts were assessed in terms of total polyphenol content and antioxidant capacity, as well as their effect on astrocyte mitochondrial reductive capacity.
Materials and methods
Extract preparation and characterisation
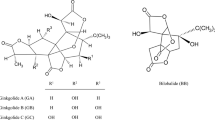
The relative composition of each extract can be seen in Fig. 1, with quantification of relative and total alkaloid content presented for comparison in Table 1. Extract A is an extract prepared from Sceletium tortuosum that was selectively propagated to achieve high-mesembrine content, while extract B was more intensively extracted using different solvents, to achieve particularly high levels of delta7-mesembrenone, which is usually contained in very low concentrations in Sceletium plants. Both extracts (batch numbers for extracts A and B: DV SCITRI:E 591/016 and DV SCDL7:E 525/016 respectively) were prepared by Verve Dynamics™ (Somerset West, South Africa) using proprietary methods and kindly donated by Mr. Richard Davies for the purposes of this study.
Cell culture
All cell culture experiments were conducted in triplicate and experiments were repeated a minimum of three times on separate occasions, as per convention for good laboratory practice in cell culture experiments.
Preparation of treatment media
A stock solution of each Sceletium extract was made (1 mg/ml extract A and 3.7 mg/ml extract B), by combining extract powder and pre-warmed serum-free media. The mixtures were vortexed for 2 min and subsequently sterile-filtered using a 0.22-μm syringe filter. From the filtered stock solutions, dilution series were performed.
The total alkaloidal content of extract B was matched to that of A. The high dose of extract A was used to represent a supra-physiological dose, while the lower dose has previously shown to be most beneficial in similar in vivo models [11].
A 2 mg/ml LPS (L4391, Sigma-Aldrich) stock solution was prepared in Hank’s Buffered Salt Solution (HBSS) and added to wells at a final concentration of 20 μg/ml for astrocyte inflammatory stimulation.
Cell propagation
Astrocytes (N7805-100, Life Technologies) of low passage (< 5) were thawed and cultured in complete Dulbecco’s modified eagle medium (DMEM), containing 10% FBS and 1% penicillin-streptomycin, and subsequently seeded into a 48-well culture plate at a density of 1 × 104 cells/well in serum-free DMEM, and incubated (37 °C, 5% CO2) for 24 h to fully adhere to the plate.
Sceletium extract treatment intervention
The supernatant was aspirated from each well, and the cell monolayer washed once with Dulbecco’s phosphate-buffered saline (DPBS) to remove remaining media residue. A 30-min pre-treatment period was then initiated, which involved the addition of the different dosages of each Sceletium extract to the respective wells. For this period, serum-free media was added to the control and LPS-control groups.
After the pre-incubation period, LPS was added to the LPS-control wells and LPS-Sceletium combination groups, to achieve a final LPS concentration of 20 μg/ml. The LPS vehicle was added to all control wells. The cells were incubated for a further 23.5 h. All experiments were performed at least three times, in duplicate.
Viability testing
Propidium iodide viability assay
A 1 mg/ml propidium iodide (PI) (P1304MP, Thermofisher Scientific) stock solution was prepared according to manufacturer’s instructions. For a 3 μM working solution, the stock solution was diluted 1:500 in PBS.
Following the 24-h treatment intervention, the supernatant was aspirated from each well. The cell monolayer was washed with DPBS before the cells were trypsinised, neutralised and centrifuged at 1500 rpm for 5 min at room temperature. The resulting supernatant was discarded, and each astrocyte pellet was resuspended 1 ml PI working solution. The samples were incubated at room temperature for 10 min in the dark before flow cytometric analysis on BD FACSAria II (with BD FACSDiva v8.1 Software). Live stained, dead stained and live unstained controls were included.
XTT viability assay
The XTT assay is a commonly used test method to indirectly measure cell viability, through assessment of mitochondrial reductive capacity. Following the 23.5-h incubation period, supernatant was removed from each well, centrifuged, aliquoted and stored at − 80 °C for subsequent batch analysis.
The astrocyte monolayer was washed twice with DPBS to remove residual Sceletium isolate treatment, following which XTT (X4626, Sigma Aldrich) solution (1 mg/ml) containing 0.5% phenazine methosulphate (P9625, Sigma-Aldrich) was added to each well, and a 4-h incubation period was initiated in a shaking incubator at 37 °C. Following incubation, optical densities were determined using a Universal Microplate Reader (Bio-Tek Instruments, Inc., EL800) and analysed using KCjunior for Windows Data Reduction Software (v1.41.3).
Cytokine measurement
Cell-free culture supernatant was analysed using a commercial magnetic bead panel assay (custom-designed Milliplex MAP Human Soluble Cytokine Receptor Panel, Merck Millipore) for concentrations of interleukin-6 (IL-6) and monocyte chemotactic protein-1 (MCP-1). The fluorescent signals were analysed with a Bio-Plex 200 instrument, in conjunction with Bio-Plex Manager 6.1 software. Cytokine responses were expressed as absolute concentrations in cell culture supernatant.
Quantification of cytokine concentrations was performed based on a standard curve, derived from linear dilution of the manufacturer-supplied cytokine standards. The detection limit was 0.9 pg/ml for IL-6 and 1.6 pg/ml for MCP-1.
Neural enzyme inhibition assay
Acetylcholinesterase (AChE) and tyrosinase inhibition was measured using a 96-microplate reader using established techniques [12, 17]. Appropriate controls, galantamine and kojic acid (known inhibitors of AChE and tyrosinase, respectively), were used for all analyses. Data were analysed using GraphPad to obtain IC50 values.
Assessment of antioxidant capacity and total phenolic content
Antioxidant capacity of both extracts was determined using the 2,2-diphenyl-1-picrylhydrazyl (DPPH) inhibition assay, which assesses radical scavenging capacity against DPPH radicals as previously described [9], with ascorbic acid as the reference standard. Total polyphenol content was determined by the Folin-Ciocalteu assay, using gallic acid as standard. Total polyphenol content was expressed as milligramme GAE (gallic acid equivalents) per milligramme of dried extract.
Statistical analysis
Results are presented as averages and standard error of the means (SEMs). Normality of data distribution was assessed, followed by non-parametric 2-way ANOVA and LSD post hoc tests. In cases where Levene’s test for homogeneity of variances rejected the null hypothesis, the Games-Howell test was used as a post hoc test (Statistica v.13.2). Differences were considered significant at p < 0.05.
Results
Neuroprotective effects
The PI exclusion assay illustrated a significant degree of cell death (fewer cells able to exclude the PI stain) in astrocytes after exposure to LPS (Fig. 2). While extract A afforded complete protection in a dose-dependent manner (Fig. 2a), extract B was not effective at any dose assessed (Fig. 2b). It is also of interest to note than while extract A did not affect cell viability in the absence of LPS, the highest dose of extract B appeared to be cytotoxic.
Anti-inflammatory outcome
The response of astrocytes to the extracts, both in the presence and absence of an inflammatory stimulus, was assessed in terms of two major pro-inflammatory cytokines associated with both neuroinflammation and systemic inflammation in chronic disease—IL-6 and MCP-1.
As expected, LPS exposure elicited significant cytokine responses for both IL-6 and MCP-1 (ANOVA main effect, p < 0.005 and p < 0.0005, respectively). This response was significantly inhibited by extract A, again in a dose-dependent manner, with the highest dose tested returning cytokine secretion to basal levels (Fig. 3a, b). In contrast, only the lower doses assessed for extract B prevented the IL-6 response significantly, with increasing doses suggesting a relatively more pro-inflammatory outcome (Fig. 3c). Similarly, the MCP-1 response indicated no benefit of extract B at any dose, while higher doses, in fact, elicited an inflammatory response similar in magnitude to the one seen after exposure to LPS (Fig. 3d).
Neural enzyme inhibition
The effects of the Sceletium extracts on two enzymes associated with neurodegeneration, namely tyrosinase and AChE, were assessed. Both extracts exhibited relatively mild inhibitory effects on these neural enzymes when compared to suitable controls (Fig. 4). Interestingly, while extract A exhibited a higher potency for inhibition of AChE than extract B (IC50 0.299 ± 0.34 vs IC50 0.983 ± 0.16 respectively), the opposite was observed for tyrosinase inhibition (IC50 – 1.621 ± 0.75 vs IC50 – 0.5908 ± 0.01 respectively). These results, which suggest as least some degree of neuroprotection—albeit perhaps via different pathways for the different extracts—were confirmed by ex vivo exposure of human astrocytes to an inflammatory stimulus.
Antioxidant outcome
To investigate whether differences in antioxidant capacity may explain the different effects reported for extract A vs B, antioxidant measures were also assessed. Indeed, the total phenolic content of extract B tested much higher than extract A (Fig. 5a). Similarly, while extract B compared favourably to the ascorbic acid control in terms of DPPH inhibition, extract A did not appear to have significant antioxidant activity in this context (Fig. 5b).
Assessment of antioxidant capacity of extract A and B. a Total polyphenol content of extracts A and B, expressed as gallic acid (GA) equivalents. b Antioxidant capacity of extracts A and B, compared to ascorbic acid. c Astrocyte mitochondrial reductive capacity following treatment with extract A. d Astrocyte mitochondrial reductive capacity following treatment with extract B. Data presented for (c) and (d) are from five experiments performed in triplicate
To put this result into a more physiologically relevant context, the LPS assay was again employed, but this time, mitochondrial functional capacity was assessed. While extract A did not affect this measure in the absence of LPS, extract B significantly compromised mitochondrial reductive capacity at the highest dose (Fig. 5c, d). In fact, this detrimental effect was similar in magnitude to the reduction in cell functional capacity after exposure to LPS. Neither extract could maintain mitochondrial function in the presence of LPS.
Discussion
The roles of glial cells in central nervous system (CNS) homeostasis maintenance and in the regulation of central innate immune responses are well-documented [29, 31, 35]. Astrocytes, which contribute 20–40% of all glial cells, respond vigorously to brain injury, releasing products that are capable of facilitating neuronal protection [16]. However, an excessive production of cytokines, chemokines and free radicals may result in functional impairment and neuronal decline [16].
In terms of the validity of the model employed, it was observed that under control conditions (i.e. at 100% viability), astrocytes expressed low levels of IL-6 and MCP-1. This is attributed to a normal physiological response to bi-products of functional metabolic processes in the body, as these cytokines are secreted as mediators of homeostasis maintenance [3]. With exposure to LPS, a significant upregulation of cytokine secretion was observed (fivefold and eightfold for IL-6 and MCP-1 respectively), validating sensitivity of the model to reflect an induced, acute inflammatory response.
When considering effects elicited by the two Sceletium tortuosum extracts assessed, clear differences were evident. While astrocyte viability was not affected under basal conditions by either dose of extract A, the highest dose of the delta7-mesembrenone-rich extract B decreased cell viability by 20%. The decrease in viability was similar in magnitude to the effect of bacterial LPS exposure. While the latter is an expected response due to significant cellular stress caused by a major inflammatory stimulus [6], the effect of extract B indicated undesired cell death. Potential reasons for this result were investigated in the context of anti-inflammatory and antioxidant mechanisms.
Firstly, in the context of inflammation, it is important to note that extract A clearly limited endotoxin-induced cytokine production to levels that were not significantly different from control conditions. This indicates a potential mechanism behind the previously observed cytoprotective effects of extract A [5]. However, the same effects were not seen in response to extract B treatment, and it appeared that in the presence of an inflammatory stressor, the higher doses of this extract contributed to cytotoxicity, although not in an additive manner.
Assessment of neural enzyme inhibition by the extracts shed more light on the differences between the high-mesembrine versus the high-delta7-mesembrenone extracts. In terms of AChE inhibition, although relatively mildly when compared to galantamine, extract A had a higher potency than extract B. A major modulator of peripheral inflammation is the cholinergic pathway, which involves suppression of innate immune responses by acetylcholine. This mechanism inhibits cytokine release by peripheral leukocytes [13]. In the CNS, inhibitors of AChE have been shown to enhance the cholinergic anti-inflammatory pathway [13].
Previous in vitro studies have shown that acetylcholine pre-treatment inhibited LPS-induced cytokine release by microglia [26]. Accordingly, AChE inhibitors have shown to limit astrocyte activation and cytokine production [13]. This further supports our interpretation that extract A, which is high in mesembrine, acts as a mild anti-inflammatory agent.
It was observed that while extract A exerted only mild inhibitory effects in tyrosinase activity, extract B acts as a potent inhibitor of this enzyme, matching the effects of kojic acid at higher doses. This effect suggests that extract B is more antioxidant in nature, in comparison to extract A. Tyrosinase is a copper-containing polyphenol oxidase (i.e. forms part of the reactive oxygen species group), which plays a vital role in melanin pigment formation [17]. Previously, tyrosinase was associated with Parkinson’s disease [10]. Therefore, inhibition of this enzyme may be beneficial in the prevention of neurodegeneration.
The antioxidant nature of extract B is further confirmed by assessing its total phenolic content, which was 20-fold higher than that of extract A. In addition, the DPPH inhibition assay indicated that extract B had a similar antioxidant capacity to that of ascorbic acid, a well-documented antioxidant agent [1]. However, it has been reported that antioxidants in high doses may lose their beneficial, radical scavenging properties, and may act as pro-oxidants, causing further cellular damage [7].
Taken together, this suggests that the 20% reduction in cell viability in response to high-dose extract B exposure can probably be attributed to antioxidant overload-associated cellular damage. This interpretation is in line with the dose-dependent upregulated inflammatory response of the astrocytes exposed to extract B which may have been the result of reactive gliosis in response to oxidative damage.
It was important to assess mitochondrial reductive capacity as an indication of overall cell functionality in the setting of Sceletium tortuosum treatment. Mitochondrial dysfunction represents an important link between metabolic syndrome and neurodegeneration, and oxidative stress has been well reported in patients with neurodegeneration, obesity and T2D, as well as in rodent models of all of these conditions [8]. Mitotoxicity is an important trigger for inflammation [28], resulting in the secretion of cytokines.
Our results indicate that while extract A had no effect on mitochondrial reductive capacity in either the presence or absence of inflammatory stimulus, treatment with extract B improved this capacity in basal conditions. In line with the indicated antioxidant properties of extract B, it was noted that a significant loss of mitochondrial function occurred with exposure to the highest dose of this extract, again indicative of antioxidant overload. Bacterial LPS exposure caused significant mitotoxicity, which was not corrected by the addition of either Sceletium extract, indicating that treatment with this natural product may be more beneficial in settings of low-grade inflammation, such as chronic disease, rather than in an acute bout of high-grade inflammation.
It is becoming increasingly important that a standardised composition of the relevant compounds in phytopharmaceutical supplements must be established, from a consumer point of view, as well as for regulatory purposes. However, due to the diversity of compounds present in most plants, coupled with varying extraction methods, quality control and standardisation of the pharmacologically active constituents of plant-based supplements is generally not achieved [21, 24].
This study highlights the importance of extraction methods’ effects on extract composition and overall properties. While extract A is a less-refined Sceletium tortuosum extract, it appears to exert more beneficial effects at a broad range of doses, which is promising in the setting of chronic disease. Although extract B does possess properties that may assist in prevention of chronic disease-associated neurodegeneration, where oxidative stress is both an etiological and comorbid factor, its highly refined nature resulted in a much more potent antioxidant product, which needs to be carefully administered at specific, low doses to achieve desired effects whilst also minimising undesired pro-oxidant damage.
Conclusion
In conclusion, from current data, it is clear that the extracts tested have a potential in the preventative medicine niche, specifically in terms of limiting inflammation and/or oxidative stress to achieve a rate-limiting effect on chronic disease development. However, the effects of Sceletium extracts and/or its isolated pure alkaloids on endocrine-immune interaction need to be further elucidated, to enable optimisation of the use of this indigenous product in the setting of chronic lifestyle diseases such as type 2 and type 3 diabetes.
Abbreviations
- ANOVA:
-
Analysis of variance
- AChE:
-
Acetylcholinesterase
- BBB:
-
Blood-brain barrier
- CNS:
-
Central nervous system
- DMEM:
-
Dulbecco’s modified eagle’s medium
- DPBS:
-
Dulbecco’s phosphate-buffered saline
- DPPH:
-
1,1-Diphenyl-2-picrylhydrazyl
- FBS:
-
Foetal bovine serum
- HBSS:
-
Hank’s balanced salt solution
- HPLC:
-
High-performance liquid chromatography
- IFN-γ:
-
Interferon-gamma
- IL-6:
-
Interleukin-6
- LPS:
-
Lipopolysaccharide
- MAO-A:
-
Monoamine oxidase A
- MCP-1:
-
Monocyte chemotactic protein-1
- PBS:
-
Phosphate-buffered saline
- PI:
-
Propidium iodide
- ROS:
-
Reactive oxygen species
- RPM:
-
Revolutions per minute
- SEM:
-
Standard error of the mean
- T2D:
-
Type 2 diabetes
- T3D:
-
Type 3 diabetes
References
Allen CL, Bayraktutan U (2009) Antioxidants attenuate hyperglycaemia-mediated brain endothelial cell dysfunction and blood-brain barrier hyperpermeability. Diabetes Obes Metab 11:480–490. https://doi.org/10.1111/j.1463-1326.2008.00987.x
Anstey KJ, Cherbuin N, Budge M, Young J (2011) Body mass index in midlife and late-life as a risk factor for dementia: a meta-analysis of prospective studies. Obes Rev 12:426–437. https://doi.org/10.1111/j.1467-789X.2010.00825.x
Balkwill FR, Burke F (1989) The cytokine network. Immunol Today 10:299–304. https://doi.org/10.1016/0167-5699(89)90085-6
Belanger M, Magistretti PJ (2009) The role of astroglia in neuroprotection. Dialogues Clin Neurosci 11:281–296. https://doi.org/10.1038/nrn1722
Bennett AC, Smith C (2018) Immunomodulatory effects of Sceletium tortuosum (Trimesemine™) elucidated in vitro: implications for chronic disease. J Ethnopharmacol 214:134–140. https://doi.org/10.1016/j.jep.2017.12.020
Blanco AM, Valles SL, Pascual M, Guerri C (2005) Involvement of TLR4/type I IL-1 receptor signaling in the induction of inflammatory mediators and cell death induced by ethanol in cultured astrocytes. J Immunol 175:6893–6899. https://doi.org/10.4049/jimmunol.175.10.6893
Burkitt M (2001) Too much of a good thing? Nat Biotechnol 19:811–812. https://doi.org/10.1136/vr.f2845
Carvalho C, Cardoso S, Correia SC, Santos RX, Santos MS, Baldeiras I, Oliveira CR, Moreira PI (2012) Metabolic alterations induced by sucrose intake and Alzheimer’s disease promote similar brain mitochondrial abnormalities. Diabetes 61:1234–1242. https://doi.org/10.2337/db11-1186
Cásedas G, Les F, Gómez-Serranillos MP, Smith C, López V (2017) Anthocyanin profile, antioxidant activity and enzyme inhibiting properties of blueberry and cranberry juices: a comparative study. Food Funct 8:4187–4193. https://doi.org/10.1039/c7fo01205e
Chen YS, Liou HC, Chan CF (2013) Tyrosinase inhibitory effect and antioxidative activities of fermented and ethanol extracts of Rhodiola rosea and Lonicera japonica. Sci World J 2013:1–5. https://doi.org/10.1155/2013/612739
Coetzee DD, López V, Smith C (2016) High-mesembrine Sceletium extract (Trimesemine™) is a monoamine releasing agent, rather than only a selective serotonin reuptake inhibitor. J Ethnopharmacol 177:111–116. https://doi.org/10.1016/j.jep.2015.11.034
Ellman GL, Courtney KD, Andres V, Featherstone RM (1961) A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem Pharmacol 7:88–95. https://doi.org/10.1016/0006-2952(61)90145-9
Gnatek Y, Zimmerman G, Goll Y, Najami N, Soreq H, Friedman A (2012) Acetylcholinesterase loosens the brain’s cholinergic anti-inflammatory response and promotes epileptogenesis. Front Mol Neurosci 5:1–10. https://doi.org/10.3389/fnmol.2012.00066
Harvey AL, Young LC, Viljoen AM, Gericke NP (2011) Pharmacological actions of the South African medicinal and functional food plant Sceletium tortuosum and its principal alkaloids. J Ethnopharmacol 137:1124–1129. https://doi.org/10.1016/j.jep.2011.07.035
Hassing LB, Dahl AK, Pedersen NL, Johansson B (2010) Overweight in midlife is related to lower cognitive function 30 years later: a prospective study with longitudinal assessments. Dement Geriatr Cogn Disord 29:543–552. https://doi.org/10.1159/000314874
Kaushal V, Dye R, Pakavathkumar P, Foveau B, Flores J, Hyman B, Ghetti B, Koller BH, LeBlanc AC (2015) Neuronal NLRP1 inflammasome activation of Caspase-1 coordinately regulates inflammatory interleukin-1-beta production and axonal degeneration-associated Caspase-6 activation. Cell Death Differ 22:1676–1686. https://doi.org/10.1038/cdd.2015.16
Kim YJ, Uyama H (2005) Tyrosinase inhibitors from natural and synthetic sources: structure, inhibition mechanism and perspective for the future. Cell Mol Life Sci 62:1707–1723. https://doi.org/10.1007/s00018-005-5054-y
Ku SK, Kwak S, Kim Y, Bae JS (2014) Aspalathin and Nothofagin from rooibos (Aspalathus linearis) inhibits high glucose-induced inflammation in vitro and in vivo. Inflammation 38:445–455. https://doi.org/10.1007/s10753-014-0049-1
De La Monte SM (2008) Alzheimer’s disease is type 3 diabetes—evidence reviewed. J Diabetes Sci Technol 2:1101–1113. https://doi.org/10.1177/193229680800200619
Nepal B, Brown LJ, Anstey KJ (2014) Rising midlife obesity will worsen future prevalence of dementia. PLoS One 9:1–5. https://doi.org/10.1371/journal.pone.0099305
Patnala S, Kanfer I (2013) Chemotaxonomic studies of mesembrine-type alkaloids in Sceletium plant species. S Afr J Sci 109:5–9. https://doi.org/10.1590/sajs.2013/882
Petersen KS, Smith C (2016) Ageing-associated oxidative stress and inflammation are alleviated by products from grapes. Oxidative Med Cell Longev 2016:1–12. https://doi.org/10.1155/2016/6236309
Pugazhenthi S, Qin L, Reddy PH (2017) Common neurodegenerative pathways in obesity, diabetes, and Alzheimer’s disease. Biochim Biophys Acta - Mol Basis Dis 1863:1037–1045. https://doi.org/10.1016/j.bbadis.2016.04.017
Shikanga EA, Viljoen AM, Combrinck S, Marston A, Gericke N (2012) The chemotypic variation of Sceletium tortuosum alkaloids and commercial product formulations. Biochem Syst Ecol 44:364–373. https://doi.org/10.1016/j.bse.2012.06.025
Shoelson SE, Lee J, Goldfine AB (2006) Inflammation and insulin resistance. J Clin Invest 116:1793–1801. https://doi.org/10.1172/JCI29069.and
Shytle RD, Mori T, Townsend K, Vendrame M, Sun N, Zeng J, Ehrhart J, Silver AA, Sanberg PR, Tan J (2004) Cholinergic modulation of microglial activation by α7 nicotinic receptors. J Neurochem 89:337–343. https://doi.org/10.1046/j.1471-4159.2004.02347.x
Smith C (2011) The effects of Sceletium tortuosum in an in vivo model of psychological stress. J Ethnopharmacol 133:31–36. https://doi.org/10.1016/j.jep.2010.08.058
Sorbara MT, Girardin SE (2011) Mitochondrial ROS fuel the inflammasome. Cell Res 21:558–560. https://doi.org/10.1038/cr.2011.20
Streit WJ, Mrak RE, Griffin WST (2004) Microglia and neuroinflammation: a pathological perspective. J Neuroinflammation 1:1–4. https://doi.org/10.1186/1742-2094-1-14
Swart AC, Smith C (2016) Modulation of glucocorticoid, mineralocorticoid and androgen production in H295 cells by Trimesemine, a mesembrine-rich Sceletium extract. J Ethnopharmacol 177:35–45. https://doi.org/10.1016/j.jep.2015.11.033
Szelényi J (2001) Cytokines and the central nervous system. Brain Res Bull 54:329–338. https://doi.org/10.1016/S0361-9230(01)00428-2
Thomson CA, McColl A, Cavanagh J, Graham GJ (2014) Peripheral inflammation is associated with remote global gene expression changes in the brain. J Neuroinflammation 11:73. https://doi.org/10.1186/1742-2094-11-73
Tucsek Z, Toth P, Tarantini S, Sosnowska D, Gautam T, Warrington JP, Giles CB, Wren JD, Koller A, Ballabh P, Sonntag WE, Ungvari Z, Csiszar A (2014) Aging exacerbates obesity-induced cerebromicrovascular rarefaction, neurovascular uncoupling, and cognitive decline in mice. Journals Gerontol A Biol Sci Med Sci 2014 69:1339–1352. doi: https://doi.org/10.1093/gerona/glu080
Wild S, Roglic G, Green A, Sicree R, Hilary K (2004) Global prevalence of diabetes: estimates for the year 2000 and projection for 2030. Diabetes Care 27:1047–1053. https://doi.org/10.2337/diacare.27.5.1047
Wrona D (2006) Neural-immune interactions: an integrative view of the bidirectional relationship between the brain and immune systems. J Neuroimmunol 172:38–58. https://doi.org/10.1016/j.jneuroim.2005.10.017
Acknowledgements
We would like to acknowledge the South African National Research Foundation (NRF) for the funding, and Verve Dynamics for the preparation and kind donation of the extracts used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bennett, A., Van Camp, A., López, V. et al. Sceletium tortuosum may delay chronic disease progression via alkaloid-dependent antioxidant or anti-inflammatory action. J Physiol Biochem 74, 539–547 (2018). https://doi.org/10.1007/s13105-018-0620-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13105-018-0620-6