Abstract
Cerebral ischemia leads to multifaceted injury to the brain. A polytherapeutic drug that can be administered immediately after reperfusion may increase protection to the brain by simultaneously targeting multiple deleterious cascades. This study evaluated efficacy of the combination of three clinically approved drugs: lamotrigine, minocycline, and lovastatin, using two mouse models: global and focal cerebral ischemia induced by transient occlusion of the common carotid arteries or the middle cerebral artery, respectively. In vitro, the combination drug, but not single drug, protected neurons against oxygen-glucose deprivation (OGD)-induced cell death. The combination drug simultaneously targeted cell apoptosis and DNA damage induced by ischemia. Besides acting on neurons, the combination drug suppressed inflammatory processes in microglia and brain endothelial cells induced by ischemia. In a transient global ischemia model, the combination drug, but not single drug, suppressed microglial activation and inflammatory cytokine production, and reduced neuronal damage. In a transient focal ischemia model, the combination drug, but not single drug, attenuated brain infarction, suppressed infiltration of peripheral neutrophils, and reduced neurological deficits following ischemic stroke. In summary, the combination drug confers a broad-spectrum protection against ischemia/reperfusion (I/R) injury and could be a promising approach for early neuroprotection after out-of-hospital cardiac arrest or ischemic stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral ischemia caused by disruption of blood supply to the brain is a leading cause of disability and death worldwide. Despite advanced interventions in cardiopulmonary resuscitation, many patients who experienced sudden cardiac arrest remain unconscious and suffer severe brain injury after successful return of spontaneous circulation (ROSC) [1]. Hospital-based therapeutic hypothermia is the only neuroprotective strategy recommended to treat cardiac arrest patients, but its therapeutic outcomes are controversial due to potential deleterious complications [2,3,4]. A new neuroprotective strategy that can be easily administered immediately after ROSC in the field might provide early neuroprotection after sudden cardiac arrest.
Postischemic brain injury is mediated through multifaceted processes. An ischemic insult induces several deleterious events, including cellular energy failure triggered by hypoperfusion, glutamate excitotoxicity, and acute inflammatory responses, leading to neuronal damage. Although reperfusion restores the blood supply, it causes secondary injury to the brain due to detrimental reactions induced by the re-oxygenation. Reperfusion following cerebral ischemia leads to exacerbated disruption of the blood-brain barrier (BBB) and marked influx of cytotoxic immune cells from the periphery [5, 6]. Due to the heterogeneity of postischemic brain injury, targeting an individual element in injury cascades has not been effective. An approach using drug combinations to target multiple pathways is likely to be more efficacious.
After reviewing several pharmacologic interventions tested in clinical or experimental settings, we decided to investigate the therapeutic potential of combining lamotrigine, minocycline, and lovastatin for the treatment of postischemic brain injury. These three Food and Drug Administration (FDA)-approved drugs are reported to have different mechanisms of actions. Lamotrigine, an antiepileptic drug, reduces excitotoxicity to neurons through blocking voltage-gated sodium channels to prevent an excessive release of glutamate. Lamotrigine is shown to exert neuroprotective effects in experimental models of cerebral ischemia [7, 8]. Minocycline is an antibiotic of the tetracycline family. The anti-inflammatory effect of minocycline contributes to improved neurological outcomes after ischemic stroke in animal and human studies [9]. Statin therapy is shown to improve patient outcomes after ischemic stroke in clinical studies through its action on vascular protection [10, 11]. Based on different mechanisms of actions, these three drugs might act on different cells involved in the progression of ischemia-induced brain injury, including neurons, microglia, and brain endothelial cells. In addition, minocycline and lamotrigine are commonly prescribed medications to treat epilepsy or infection, which are common poststroke complications as well [12,13,14]. Moreover, statin, an effective lipid-lowing drug, is one of the most commonly prescribed medications in the USA. Many patients at high risk for stroke might have already taken statins as daily medications. This increases the feasibility of repurposing statins to treat postischemic brain injury.
Many drugs exert pleiotropic effects in a dose-dependent manner. Although a high dose of single drug is reported to show multiple therapeutic effects, a high dose of drug administration might increase a risk of drug toxicity. We hypothesized that using a low dose of drug combinations to simultaneously target multiple mechanisms might be a safer approach to ensure protection against ischemia/reperfusion (I/R) injury and reduce the risk of toxicity with a high-dose drug administration.
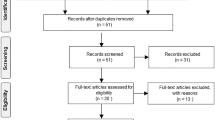
In this study, we showed that the combination drug provides superior protection to neurons over single drug against oxygen-glucose deprivation (OGD)-induced cell death. The combination drug acted on multiple injury cascades and cellular targets simultaneously, whereas single drug targets one injury cascade. We further evaluated therapeutic effects of the combination drug in animal models using a sub-effective dose of three drugs reported in previous studies [8, 15,16,17]. We used the mouse model of global ischemia induced by transient bilateral common carotid artery occlusion (BCCAO). The combination drug, but not single drug, administered at reperfusion suppressed acute neuroinflammation, microglial activation, and delayed neuronal damage in BCCAO mice. To gain more insights into effects of the combination drug to counter reperfusion injury, we utilized the mouse model of focal cerebral ischemia induced by intraluminal transient middle cerebral artery occlusion (tMCAO). The sub-effective dose of individual single drug failed to protect against brain infarction in intraluminal tMCAO mice. However, the combination drug, composed of the same sub-effective dose of three drugs, markedly reduced brain infarction and alleviated neurological deficits. The combination-drug treatment suppressed early-phase neuroinflammation and reduced infiltration of peripheral neutrophils after I/R. Taken together, these results demonstrate that a polytherapeutic combination drug that can be administered at the time of reperfusion confers protection against postischemic brain injury.
Materials and Methods
Animal
Adult C57BL/6 female mice (aged 12–16 weeks) and male mice (aged 8–12 weeks) used in studies were obtained from Jackson Laboratories (Bar Harbor, ME). All animals were treated in accordance with the National Institutes of Health (NIH) Guide for the Care and Use of Laboratory Animals. The animal protocols were approved by Purdue Animal Care and Use Committee, Purdue University. After reaching desired age and body weight for surgery, eligible animals were randomized and allocated to surgery and treatment groups blindly. Experimental data analyses and outcome assessment were performed by researchers blinded for group allocation.
Transient Global Cerebral Ischemia
Female C57BL/6 mice (18–22 g) were subjected to BCCAO surgery to induce transient global cerebral ischemia as previously reported [18,19,20,21]. The C57BL/6 strain is reported to be more susceptible to BCCAO-induced global ischemia than other strains due to poorly developed posterior communicating arteries [22, 23]. Anesthesia was induced with inhalation of 2% isoflurane in a mixture of air and oxygen (70:30) and maintained with 1.5% isoflurane during the surgery period. Rectal temperatures were maintained at 37 ± 0.5 °C with a heating pad (Harvard Apparatus, MA) and a heating lamp. Regional cerebral blood flow (rCBF) was measured using laser Doppler flowmetry (moorVMS-LDF2; Moor Instruments, Inc., Delaware). The fiber optic probes were fixed on the skull, 2 mm lateral and 1 mm caudal from the bregma. Changes in CBF were monitored before, during, and after BCCAO and were expressed as a percentage of the pre-ischemic value (baseline). The common carotid arteries were exposed via a neck incision and encircled with loose ligatures for later clamping. The BCCAO was induced by applying micro-serrefine clamps (Fine Science Tools, CA) to both common carotid arteries for 20 min, determined by our preliminary studies and as previously reported [20, 21, 23]. After releasing the clamps, the skin incision was closed using Reflex Wound Clips (Fine Science Tools, CA). The animals were maintained in recovery cages for 1 h until fully recovered from the surgery and anesthesia, where the ambient temperature was kept at 34–35 °C using a heating lamp and blanket. Sham-operated animals were treated as described above but without BCCAO. Only animals that exhibited more than 80% reduction of the mean CBF recorded from the right and left hemispheres during BCCAO were included in the study.
Transient Focal Cerebral Ischemia
Male C57BL/6 mice (23–27 g) were subjected to the MCAO to induce focal cerebral ischemia as previously reported [24, 25]. Mice were anesthetized, and body temperature was monitored and maintained, as described above. Regional CBF was monitored at the parietal bone, 3 mm lateral and 2 mm caudal to the bregma, using laser Doppler flowmetry as described above. The right common carotid artery (CCA) and the right external carotid artery (ECA) were exposed through a midline neck incision. The right ECA was further dissected distally and coagulated along with the terminal lingual and maxillary artery branches. The right CCA was temporarily clamped in order to make a minimal incision in the ECA stump. The drop of rCBF was recorded. A silicon-coated 6-0 nylon monofilament with a 0.21 ± 0.02 mm diameter (Doccol Corp., MA) was inserted through the ECA stump into the MCA to induce MCAO. The length of inserted suture from the ECA stump to the bifurcation of the MCA and anterior communicating artery (ACA) was ~9 mm. At 40 min after MCAO, the filament was withdrawn to re-establish right CBF. Poststroke surgery care was conducted as described above. We used two criteria to determine successful induction of focal cerebral ischemia: a reduction of right CBF ≥50% from CCA clamping to filament insertion and a decrease of right CBF ≥70% when the filament tip reached its target. Only animals that reached both criteria and exhibited a sustained reduction of CBF ≥70% during MCAO were included in the study [25, 26].
Laser Speckle Perfusion Imaging
The change of CBF resulting from BCCAO in global cerebral ischemia mice was monitored using a two-dimensional laser speckle perfusion imager (moorFLPI-2; Moor Instruments, Inc., Delaware). Briefly, the skulls of anesthetized mice were exposed and the CBF was measured immediately before the surgery, during the occlusion (5 and 15 min), and after reperfusion (5 and 10 min). CBF was analyzed by moorFLPI-2 software, and images were shown with arbitrary units in a 16-color palette.
Drugs and Treatments
Lamotrigine was obtained from R&D Systems, Inc., MN. Lovastatin hydroxyl acid was obtained from Cayman Chemical, MI. Minocycline was obtained from Sigma-Aldrich, MO. All compounds were dissolved in dimethyl sulfoxide (DMSO; Sigma-Aldrich, MO) and sterilized by passing the stock solution through a 0.22-μm filter. The prepared stock solutions were aliquoted and stored at −20 °C. The combination-drug preparation was freshly prepared before dosing by mixing the three stock solutions with the vehicle (0.9% saline containing 10% DMSO and 12.5% Solutol (Kolliphor® HS 15; Sigma-Aldrich, MO). The combination drug was administered intravenously through the tail vein or retro-orbital venous sinus. The dosage of the combination drug contained 10 mg/kg body weight lamotrigine, 20 mg/kg body weight lovastatin, and 10 mg/kg body weight minocycline. In the in vitro studies, minocycline at 20 μM, lovastatin at 10 μM, and lamotrigine at 100 μM were used.
Measurements of Brain Infarction in Focal Ischemia
Detection of brain infarct volume was performed by ex vivo triphenyltetrazolium chloride (TTC) staining 48 h after reperfusion as previously described [25]. Following sacrifice, 2-mm coronal brain sections were immediately stained with 1% TTC at 37 °C for 10 min. The stained sections were scanned, and the TTC-stained area (non-infarct area) in each section was measured and analyzed using Image J, NIH. The area of infarction was calculated by subtracting the non-infarct area of the ipsilateral side from the non-infarct area of the contralateral side to compensate for swelling in the ipsilateral side after I/R. The areas of infarction obtained from each section were summed and multiplied by thickness to obtain the total volume of brain infarction.
Brain Tissue Preparation and Histology
Mice were anesthetized and transcardiacally perfused with phosphate-buffered saline (PBS) followed by 4% paraformaldehyde (Sigma-Aldrich, MO). The brains were retrieved and postfixed in 4% paraformaldehyde at 4 °C overnight. Coronal brain blocks (2 mm thick) were cut and cryoprotected by sequentially immersing them into 6 and 30% sucrose-PBS (w/v) solution at 4 °C. Brain blocks were subsequently embedded and frozen in an optimal cutting temperature (OCT) compound (Tissue-Tek, Sakura). Serial frozen sections at 15 μm were cut using a cryostat (CM1950; Leica Biosystems, Inc., IL) and mounted on Superfrost Plus slides. Sectioned slides were stored at −20 °C until used for staining. For cresyl violet staining, slides were placed into 1:1 alcohol/chloroform overnight to reduce background fat staining. Slides were then rehydrated through 100, 95, 70, and 50% alcohol to distilled water. Slides were rinsed and stained with 0.1% cresyl violet for 6 min. After washing, slides were dehydrated through graduated alcohol, placed in xylene, and coverslipped. Bright-field images were acquired using a microscope (BX53; Olympus) equipped with a CCD camera (DP72; Olympus).
Immunohistochemistry
Frozen-sectioned slides were brought to room temperature (RT) for 1 h and washed with PBS. Slides were then incubated with a blocking solution (0.25% Triton X-100, 3% normal goat/horse serum in PBS) at RT for 1 h. Primary antibodies, rabbit anti-Iba1 (1:600; Wako), or mouse anti-NeuN (1:600; Chemi-Con) were diluted and incubated on slides at RT for 2 h. After washing with PBS, slides were incubated with secondary antibodies, goat anti-rabbit Alexa Fluor 546 or goat anti-mouse Alexa Fluor 488 (1:400; Invitrogen), at RT for 1 h. At the end of incubation, slides were washed with PBS and coverslipped with ProLong Gold anti-fade mountant with DAPI (Invitrogen). The edges of mounted coverslips were sealed with nail polish. Brain regions of interest were defined in relation to anatomical landmarks using a stereotaxic atlas (Franklin and Paxinos, 3rd edition, 2008) for guidance. Two to three sections from each mouse were stained (n = 5–6 mice per group). The Nuance FX multispectral imaging system and Nuance software (PerkinElmer) were used for image acquisition and analysis for NeuN-positive neurons. Images of Iba1-stained microglia were acquired using a FluoView FV10i confocal microscope (Olympus) and analyzed by Image J, NIH.
Neurological Function Assessment
Neurological function was evaluated using a six-point score as previously described [25, 27]. The assessment was performed at 24 and 48 h after reperfusion. The six-point scale used was score 0 = normal; score 1 = mild circling behavior with or without inconsistent rotation when picked up by the tail, <50% attempts to rotate to the contralateral side; score 2 = mild consistent circling, >50% attempts to rotate to contralateral side; score 3 = consistent strong and immediate circling, the mouse holds a rotation position for more than 1–2 s, with its nose almost reaching its tail; score 4 = severe rotation progressing into barreling, loss of walking or righting reflex; score 5 = comatose or moribund.
Cell Culture
Mouse brain endothelial cells (bEnd.3; American Type Culture Collection, Manassas, VA) were cultured in Dulbecco modified Eagle’s medium (DMEM; Life Technologies, CA) supplemented with 10% heat-inactivated fetal bovine serum (FBS) (Atlanta Biologicals, GA) containing 2 mM l-glutamine and 1× antibiotic/antimycotic in 5% CO2 at 37 °C. Immortalized mouse hippocampal neurons (HT22 cells) were a generous gift from Dr. David Schubert (Salk Institute, La Jolla, CA) [28]. The HT22 cells were maintained in DMEM supplemented with 10% FBS, 2 mM l-glutamine, 100 U/mL penicillin, and 100 μg/mL streptomycin in 5% CO2 at 37 °C. The HT22 cells were maintained at ≤50% confluency as suggested by Dr. David Schubert. The HT22 cells were differentiated in a Neurobasal medium (Life Technologies, CA) containing 2 mM l-glutamine and 1× N2 supplement (Life Technologies, CA) for 36–40 h before use as previously described [29,30,31]. The differentiated HT22 displayed apparent neurite outgrowth, which morphologically resembled more postmitotic neuronal characteristics than the undifferentiated cells (Supplemental Fig. 1A). Primary microglial cultures were generated from neonatal mice (days 1–2). The whole brain was harvested carefully with curved forceps, and the cerebellum was removed. After peeling off surface meninges, the cerebral cortex was dissected and homogenized with the glial cell enrichment culture medium, DMEM/F12 (50:50), containing 10% heat-inactivated FBS, 2 mM l-glutamine, and 1× antibiotic/antimycotic. The dissociated cortex was passed through 70-μm cell strainers with the culture medium. The cells were collected and plated in 75-cm2 poly-d-lysine precoated culture flasks replenished with a fresh culture medium. The culture medium was supplemented with 10 ng/mL GM-CSF on 5 days in vitro (DIV) and 10 DIV after plating. On 15 DIV, microglial cells were harvested from mixed glia culture by shaking the flasks at 300 rpm at 37 °C for 30 min. The purity of cultured microglial cells was examined using fluorescence-activated cell sorting (FACS) analysis, and ≥90% of cells were positive for CD11b expression.
Oxygen-Glucose Deprivation
OGD was performed by placing cultured cells in a 37 °C incubator housed in an anaerobic chamber as previously described with some modifications [32, 33]. In brief, cells were washed twice and incubated with predeoxygenated glucose-free Hank’s balanced salt solution (HBSS). The cells were then placed into an anaerobic incubator chamber (Galaxy 170R equipped with O2 control sensor; Eppendorf, NY), which was saturated with 95% N2/5% CO2 for 16–18 h. The level of O2 was maintained ≤1% through continuous flushing of N2. The OGD was terminated by removing HBSS, replenishing with a warmed culture medium, and placing cells in a normoxic incubator chamber (95% air/5% CO2). This latter step was referred to as re-oxygenation.
FACS Analysis of Apoptotic and Necrotic Cell Death
The differentiated HT22 neurons were subjected to a 45-min OGD stimulus followed by re-oxygenation for 6 h with or without drug incubation. Annexin V + propidium iodide (PI) staining was performed to detect apoptotic and necrotic cell death as previously described [34]. Cells were harvested, washed with PBS, and re-suspended in 200 μL of annexin V-binding buffer (BioLegend, CA). Cells were then incubated with annexin V-APC and PI for 10 min at room temperature in the dark and immediately analyzed by FACS analysis. Flow cytometry analysis was performed by flow cytometry (FACSVerse; BD Biosciences, CA). A minimum of 10,000 events were collected per sample. For fluorescence microscopy analysis, cells were stained with annexin V-FITC, PI, and Hoechst 3342. The Leica DMI6000B fluorescence inverted microscope and Leica Application Suite software system were used for image acquisition. The annexin V+/PI− cells were considered as early apoptotic cells whereas the annexin V+/PI+ cells were considered as necrotic and late apoptotic cells.
Immunocytochemistry
Primary microglial cells were seeded on poly-d-lysine-coated coverslips and subjected to OGD stimulus for 1.5 h followed by 6 h of re-oxygenation. Cells were then fixed in 2% paraformaldehyde for 15 min and then washed with PBS. Cells were permeabilized with 0.3% Triton X-100 for 10 min and blocked with 3% normal goat serum at RT for 30 min. After blocking, cells were incubated with primary antibodies, mouse anti-phospho-H2A.X Ser139 (Abcam, MA) or rabbit anti-TNF-α (IHC World, MD) at RT for 1 h. After washing with PBS, cells were incubated with Alexa Fluor 594-conjugated goat anti-mouse or anti-rabbit antibody (Life Technologies; 1:600) at RT for 1 h. Cells were stained with Hoechst 3342 for 15 min and then washed with PBS. Coverslips were mounted with the ProLong Gold anti-fade mountant (Life Technologies, CA). Confocal images were acquired on the FluoView FV10i confocal microscope with a ×60 objective using the FV10iO software (Olympus) and analyzed using ImageJ (NIH).
Brain Mononuclear Cell Isolation and FACS Analysis
Mice were perfused with ice-cold PBS transcardiacally. The brain was harvested immediately, and the meninges were removed. The brains harvested from MCAO mice were separated into two hemispheres: ipsilateral hemisphere and contralateral hemisphere. The brains were homogenized with HBSS buffer and passed through a 70-μm nylon cell strainer to obtained single-cell suspensions. To remove myelin and debris, cells were resuspended in 70/30% Percoll and then centrifuged at 1000×g for 25 min at RT. The cells at the interface of 70/30% Percoll were collected, washed with PBS, and incubated with an antibody cocktail containing anti-CD45 (30-F11; BioLegend), anti-CD11b (M1/70; BioLegend), and anti-Ly6G (1A8; BioLegend). After staining, cells were subjected to FACS analysis (FACSVerse; BD Biosciences, CA). A minimum of 20,000 events were collected per sample. Brain mononuclear cells isolated from BCCAO mice were incubated with an antibody cocktail containing anti-CD45 (30-F11; BioLegend), anti-CD11b (M1/70; BioLegend), and anti-CD86 (GL-1; BioLegend) to identify and detect microglial activation [35].
Quantitative Real-Time PCR Analysis In Vivo and In Vitro
Total RNAs were extracted using the RNeasy RNA Isolation Kit (Qiagen) according to the manufacturer’s instruction. cDNAs were prepared by reverse transcription from 1 μg of total RNAs using the High-Capacity cDNA Reverse Transcription Kit with random primers (Life Technologies, CA). Quantitative real-time PCR was performed using TaqMan gene expression probes and PCR Master Mix (Applied Biosystems; Life Technologies, CA). Quantitative RT-PCR was carried out using StepOnePlus (Applied Biosystems; Life Technologies, CA). β-Actin and peptidylprolyl isomerase A (PPIA) were used as internal controls.
Statistical Analysis
Data are presented as means ± SEM. Comparisons between two groups were determined using the paired Student’s t test, whereas comparisons among multiple groups were done by one-way ANOVA followed by Bonferroni’s post hoc multiple comparison test. The statistical analysis was performed using GraphPad Prism 5 (GraphPad). Statistical significance was determined with p values <0.05. For categorized neurological scores, differences between two groups were determined using the chi-square test (SPSS Statistics, version 23; IBM).
Results
Combination Drug, but Not Single Drug, Protects Neurons from Ischemia-Induced Cell Death
In this study, we compared the neuroprotective effect of single-drug treatment of minocycline, lovastatin, or lamotrigine with that of combinations of the three drugs. We subjected differentiated HT22 hippocampal neurons to OGD for 45 min following re-oxygenation for 6 h in the presence or absence of different drug treatments. Cell survival was determined by combined PI and annexin V staining to identify ischemia-induced necrotic or apoptotic cell death (Supplemental Fig. 1B). We used a flow cytometer to further quantify different cell populations (Fig. 1a). Compared to vehicle control, cells treated with the combination drug showed significant viable cells identified as the PI/annexin V double-negative cell populations (53.6 ± 2.4 of vehicle treated; 76.4 ± 3.1 of combo drug treated; Fig. 1b). The single-drug treatment of minocycline, lovastatin, or lamotrigine did not rescue neurons from cell death induced by ischemia compared to the combination-drug treatment (Fig. 1a, b). These results demonstrate that the combination drug exerts superior neuroprotection than each drug individually. To identify how these three drugs interact against ischemic cascades, we further analyzed annexin V-stained cells, which represented cells undergoing apoptosis. We found a reduction of apoptotic cells in the treatment with minocycline alone. These results indicate that minocycline contributes to the action of the combination drug to suppress ischemia-induced cell apoptosis. Early DNA damage is the characteristics of cellular injury induced by ischemia. Compared to vehicle control, cells treated with the combination drug showed a significant reduction of DNA double-strand breaks revealed by the phosphorylation of histone H2AX (Fig. 1d, e). Unlike suppressing ischemia-induced cell apoptosis, minocycline could not suppress ischemia-induced DNA damage, whereas lamotrigine significantly suppressed DNA damage as the combination drug did. Lamotrigine contributed to the action of the combination drug to reduce DNA damage and subsequent cell death after ischemia. The results demonstrate that a single drug cannot efficiently block multiple cellular injury cascades induced by ischemia. The combination drug showed the potential to act on multiple injury cascades simultaneously and exerted superior neuroprotection than a single drug.
Combination drug, but not single drug, protects neurons from I/R-induced cell death in vitro. a The combination drug protected HT22 neurons against I/R injury in vitro. Differentiated HT22 neurons were subjected to OGD for 45 min co-treated with vehicle, the combination drug, or each drug individually. HT22 neurons cultured at normoxia condition were used as normal control. After OGD, the cells were incubated with the normal culture medium and returned to normoxia condition as re-oxygenation. At 6 h after re-oxygenation, PI/annexin V-stained HT22 neurons were analyzed using FACS analysis. The cell necrosis and apoptosis were identified as PI+/annexin V+ and PI−/annexin V+, respectively, as shown. b The percentage of viable cells (PI−/annexin V−) was measured. Data presented are from eight independent experiments for the vehicle and combination drug and from three independent experiments for the individual drug. **p < 0.01, ***p < 0.001, by one-way ANOVA with Bonferroni’s post hoc multiple comparison test. c The percentage of cell apoptosis (PI−/annexin V+) was measured. Data presented are from eight independent experiments for the vehicle and combination drug and from three independent experiments for the individual drug. *p < 0.05, ***p < 0.001, by one-way ANOVA with Bonferroni’s post hoc multiple comparison test. d Immunostaining of phospho-H2AX (pH2AX) as a marker of DNA double-strand breaks in neurons treated with vehicle, combination drug, or each drug individually. Data are representative confocal images from three independent experiments. Arrows indicate uniformly pH2AX-postitive cell nuclei. Hoechst 3342-stained cell nuclei are depicted in blue. Scale bar, 20 μm. e The percentage of pH2AX-positive cells in each treatment group was measured. Data presented are from three independent experiments. **p < 0.01, ***p < 0.001, by one-way ANOVA with Bonferroni’s post hoc multiple comparison test
Combination Drug Suppresses Ischemia-Induced Activation of Microglia and Inflammation in Endothelial Cells
After acute ischemic insult, resident microglia are rapidly activated and considered to be the main source of most brain-derived inflammatory mediators that are cytotoxic to injured neurons. We challenged primary cultured mouse microglia with OGD following re-oxygenation. We found significant induction of TNF-α in microglial cells in response to OGD. Importantly, the combination drug effectively inhibited OGD-induced TNF-α expression (Fig. 2a, b). Minocycline treatment alone contributed to the action of the combination drug to suppress microglial activation after OGD and re-oxygenation. These results suggest that in addition to rescuing neurons from cell death, the combination-drug treatment suppresses microglial activation induced by ischemia. Pro-inflammatory cytokines, such as TNF-α, released by activated microglia plays a critical role in BBB damage and subsequent peripheral cell infiltrations after I/R. We stimulated brain endothelial cells with TNF-α and examined protective effects of the combination drug versus single-drug treatment. The expression of matrix metalloproteinase-9 (MMP9) was induced by TNF-α stimulation within brain endothelial cells. The combination drug significantly inhibited the TNF-α-induced expression of MMP9 (Fig. 2c). Minocycline or lamotrigine did not show effects on MMP9 production, whereas lovastatin alone suppressed TNF-α-induced MMP9 production similar to what the combination drug did. Taken together, our results suggest that these three drugs act additively against I/R injury to the brain through targeting different ischemic injury cascades and cells involved in the progression of I/R injury, including neurons, microglia, and brain endothelial cells. The combination drug confers a broader spectrum of protection to the brain than a single drug.
Combination drug suppresses inflammation in microglia and brain endothelial cells. Primary cultured microglial cells were subjected to OGD for 1 h followed by re-oxygenation for another 6 h. The vehicle, combination drug, or each individual drug was applied at the beginning of re-oxygenation. The microglial cells cultured under normoxia condition were used as normal control. a Immunostaining of intracellular TNF-α in microglial cells at 6 h after re-oxygenation. Data are representative confocal images from three independent experiments. Arrows indicate activated microglial cells showing increased intracellular TNF-α. Arrowheads indicate resting microglial cells. Cell nuclei are visualized by Hoechst 3342 staining. Scale bar, 20 μm. b The percentage of TNF-α-positive cells in each treatment group was measured. Data presented are from three independent experiments. ***p < 0.001, by one-way ANOVA with Bonferroni’s post hoc multiple comparison test. c The brain endothelial (bEnd.3) cells were pretreated with vehicle, combination drug, or individual drug (minocycline, lovastatin, or lamotrigine), respectively for 1 h followed by TNF-α (50 ng/mL) stimulation for 24 h. The mRNA expression of MMP9 was analyzed using qPCR. Data presented are from four independent experiments. *p < 0.05, **p < 0.01, by one-way ANOVA with Bonferroni’s post hoc multiple comparison test
Combination Drug, but Not Single Drug Treatment Alleviates Delayed Neuronal Death After Transient Global Ischemia
To further investigate the translational potential of the combination-drug treatment, we conducted BCCAO in mice to induce transient global ischemia, which mimics lack of blood supply to the brain induced by sudden cardiac arrest. We administered the combination drug or single drug during reperfusion. Changes of CBF were monitored using laser speckle contrast imaging (Supplemental Fig. 2A). We also used laser Doppler flowmetry to monitor CBF changes temporally and observed that the CBF returned to baseline 10 min following the onset of reperfusion (Supplemental Fig. 2B). The rapid return of CBF after transient BCCAO mimics successful ROSC following cardiac arrest and indicates a risk of reperfusion injury in the brain. We administered drug treatment at reperfusion and at 24 and 48 h after reperfusion. A similar reduction of CBF was confirmed among different treatment groups (Supplemental Fig. 2C). We did not observe significant changes of body weight in mice when three drugs were co-administered (Supplemental Fig. 2D). These results suggest that these three drugs might not be intolerant of each other. We assessed neuronal damage 72 h after reperfusion, the phase in which delayed neuronal death is manifested clinically [36,37,38,39]. The pyramidal neurons in the hippocampal CA1 sector from combination drug-treated mice were significantly protected against transient global ischemia compared to pyramidal neurons in vehicle- or each single drug-treated mice (Fig. 3a, b). NeuN immunostaining to detect neurons showed a more dispersed cell layer with fewer neurons in vehicle-treated mice, compared to a more intact cell layer exhibited in combination drug-treated mice. Moreover, neither single-drug treatment restored the fully intact cell layer in the hippocampal CA1 sector (Fig. 3c). These results demonstrate that the combination drug exerts superior protective effects on hippocampal neurons after transient global ischemia than single drug individually.
Combination drug, but not single drug, treated at the time of reperfusion suppresses delayed neuronal death in BCCAO mice. a C57BL/6 female mice subjected to transient BCCAO were treated with vehicle, combination drug, or single drug individually at reperfusion, 24 and 48 h following reperfusion. At 72 h after reperfusion, brain tissues were prepared and stained with cresyl violet. Representative images of cresyl violet staining of the hippocampus are shown. N = 7–10 mice/group. Arrows indicate healthy neurons. Arrowheads indicate damaged/dead neurons with shrunken cell bodies. Scale bar, 20 μm. b The percentage of damaged pyramidal neurons in medial CA1 sector in each treatment group was measured. N = 7–10 mice/group. *p < 0.05, ***p < 0.001 by one-way ANOVA with Bonferroni’s post hoc multiple comparison test. c Immunostaining of NeuN for neurons showed reduced neuronal loss in combination drug-treated mice. N = 5–6 mice/group for sham, vehicle, and the combination-drug treatment groups. N = 4 mice/group for single-drug treatment groups. DAPI stained for the cell nucleus. Scale bar, 40 μm. MIN minocycline, LVN lovastatin, LAM lamotrigine
Combination Drug, but Not Single Drug Treatment Suppresses Acute Neuroinflammation After Transient Global Ischemia
As we observed the combination drug suppressed ischemia-induced activation of microglia in vitro, we examined whether the combination-drug treatment suppressed activation of microglia in vivo using Iba1 immunostaining. Transient global ischemia significantly increased microglial Iba1 expression in vehicle-treated mice (Fig. 4a). The microglia displayed hyperactive status, showing enlarged soma and shortened and highly branched processes (Fig. 4b). The combination-drug, but not individual single-drug, treatment markedly suppressed microglial Iba1 expression. Microglia from combination drug-treated mice exhibited ramified morphology with fewer and long-branching processes, indicative of a relatively resting phenotype. In addition to microglial activation, we examined the induction of pro-inflammatory mediators in the brain following transient global ischemia. The expression levels of TNF-α and Ccl2 were strongly induced, as early as 6 h after reperfusion. The combination drug administered at reperfusion significantly suppressed acute induction of inflammatory mediators in the brain, whereas single-drug treatment could not effectively suppress acute neuroinflammation following transient global ischemia (Fig. 4c). To confirm suppressive effects of the combination drug on acute microglial activation, we measured surface expression of maturation marker CD86 on microglia isolated from the ischemic brain at 6 h after reperfusion. The expression of CD86 on CD45IntCD11b+ microglia was significantly reduced in the combination drug-treated mice compared to that in vehicle-treated controls (Fig. 4d). Taken together, these results demonstrate that the combination drug administered at reperfusion acts effectively to suppress neuroinflammation following transient global ischemia.
Combination drug treated at the time of reperfusion suppresses microglial activation and acute neuroinflammation in BCCAO mice. a Representative confocal images of Iba1-postitive microglia in the hippocampus of mice that received vehicle, combination drug, or each drug individually. N = 5–6 mice/group for sham, vehicle, and the combination-drug treatment groups. N = 4 mice/group for single-drug treatment groups. DAPI stains for cell nuclei (blue). Scale bar, 20 μm. b Representative confocal images of single microglial cell from Iba1-stained tissue sections presented in a. MIN minocycline, LVN lovastatin, LAM lamotrigine. c Effects of vehicle, the combination drug, or individual single drug on acute neuroinflammation. The mRNA levels of pro-inflammatory cytokine, TNF-α, or chemokine, Ccl2, in postischemic brains were measured at 6 h after reperfusion. N = 7–11 mice/group. **p < 0.01, by one-way ANOVA with Bonferroni’s post hoc multiple comparison test. d Mononuclear cells were isolated from postischemic brains 6 h after reperfusion and subjected to FACS analysis to identify subsets of immune cells using antibodies against CD45, CD11b, and CD86. Brain-resident microglial cells were gated as CD45IntCD11b+ cell population. Identified CD45IntCD11b+ microglia were analyzed to examine the expression of surface marker, CD86, as the indication of activation status. The proportion of CD86+ microglial cells were determined. N = 4 mice/group. **p < 0.01, ***p < 0.001, by one-way ANOVA with Bonferroni’s post hoc multiple comparison test. Post hoc statistical power, 0.84
Combination Drug, but Not Single Drug Treatment Reduces Brain Infarction in Intraluminal tMCAO Mice
Recently, the endovascular thrombectomy, which removes occluding clots mechanically using stent-retriever devices, has shown promising therapeutic effects on large-vessel ischemic stroke [40, 41]. With higher rates of recanalization, the rapid increase of CBF after thrombectomy resembles ROSC after cardiac arrest and may increase a risk of reperfusion injury. We tested the translation potential of combination drug combined with endovascular thrombectomy for the treatment of ischemic stroke. Using an intraluminal tMCAO mouse model which mimics the endovascular thrombectomy in ischemic stroke, we administered the combination drug or each individual drug after the onset of reperfusion [42]. The physiological parameters for intraluminal tMCAO mice are listed in Supplemental Table 1, which shows no differences among different treatment groups. We evaluated whether a low dose of single drug exerts protective effects against brain damage. We measured the size of brain infarction on TTC-stained brain slices at 48 h after reperfusion. When administered at a low dose, neither minocycline, lovastatin, nor lamotrigine showed protective effects to the brain in intraluminal tMCAO mice. The brain infarct volume was comparable in size to that of vehicle-treated mice (Fig. 5a, b). However, when a low dose of three drugs was co-administered together, the infarct volume of ischemic brain was significantly reduced (31.42 ± 3.11 combo drug vs. 68.33 ± 4.31 vehicle; Fig. 5c, d). In addition, the combination-drug treatment alleviated neurological deficits induced by I/R in intraluminal tMCAO mice (Fig. 5e). These results demonstrate that the combination drug effectively attenuates postischemic brain injury and preserves neurological function compared to individual single drug. Similar to transient global ischemia, neuroinflammation plays a critical role in the pathophysiology of ischemic stroke and promotes progression of brain infarction [43]. We examined whether the combination-drug treatment inhibits production of pro-inflammatory mediators in the ischemic brain at an early phase (24 h post injury). Our results show that pro-inflammatory cytokines and chemokines, including TNF-α, IL-1β, and Ccl2, were upregulated in the ipsilateral hemisphere of vehicle-treated mice after intraluminal tMCAO. The combination-drug treatment significantly reduced production of pro-inflammatory mediators. These results suggest that a reduction of neuroinflammation mediated by the combination drug might contribute to its protective effect on ischemic stroke.
Combination drug, but not single drug, reduces brain infarction in intraluminal tMCAO mice. C57BL/6 male mice subjected to transient MCAO were treated with vehicle or each drug individually after reperfusion. At 48 h after reperfusion, the postischemic brains were examined using TTC staining. a Representative images of TTC-stained brains from mice that received different treatments. N = 8 mice/group. Dotted lines indicate the infarct area (white). The infract volume is listed for the individual brain. The brain tissue from mice that received sham surgical operation is shown as control, showing no brain infarction. b Volume of brain infarct in vehicle- or single drug-treated mice. N = 8 mice/group. N.S. no significance; by one-way ANOVA with Bonferroni’s post hoc multiple comparison test. c Five representative images of TTC-stained brains from vehicle- or combination drug-treated mice. N = 14 mice/group. Dotted line indicates the infarct area (white). The volume of brain infarct is listed for the individual brain. d Volume of brain infarct in vehicle- or combination drug-treated mice. N = 14 mice/group. ***p < 0.001, by Student’s t test. e Neurological scores were determined in vehicle- or combination drug-treated mice at 48 h after intraluminal tMCAO. N = 14 mice/group. a p < 0.0001, by chi-square test. **p < 0.01, by Student’s t test. f RNA was extracted from the ipsilateral and contralateral hemispheres of intraluminal tMCAO mice at 24 h after reperfusion. The expression of TNF-α, IL-1β, and Ccl2 mRNA was determined using qPCR. The relative expression level in the ipsilateral hemisphere was compared to the level in the contralateral hemisphere within an individual mouse. N = 5–7 mice/group. *p < 0.05, **p < 0.01, ***p < 0.001, by one-way ANOVA with Bonferroni’s post hoc multiple comparison test
Combination Drug Treatment Reduces Infiltration of Neutrophils in Intraluminal tMCAO Mice
Postischemic inflammation is critical for infiltration of cytotoxic immune cells from the periphery. We observed that the combination drug effectively suppresses neuroinflammation in the ischemic brain and inhibits inflammation-induced MMP9 production in brain endothelial cells. To further characterize effects of the combination drug on infiltration of peripheral immune cells into the brain, we isolated whole leukocyte populations in the ischemic brain. The vehicle-treated mice showed a significant increase in CD45hiCD11b+-infiltrating leukocytes in the ipsilateral compared to the contralateral hemisphere (Fig. 6a, upper panel, b). Infiltrating leukocytes were not significantly decreased in the ipsilateral hemisphere of combination drug-treated mice. However, within the CD45hiCD11b+-infiltrating leukocyte population, a significant reduction of neutrophils, characterized as CD45hiCD11b+Ly6G+ cells, was observed in the ipsilateral hemisphere of combination drug-treated mice (4.3 ± 0.8% combo drug vs. 11.1 ± 3.1% vehicle; Fig. 6a, lower panel, c). These results indicate that the combination drug might more effectively inhibit the influx of neutrophils into the brain following transient focal ischemia.
Combination-drug treatment suppresses brain-derived inflammatory cytokines and infiltration of neutrophils after intraluminal tMCAO. C57BL/6 male mice subjected to transient MCAO treated with vehicle or the combination drug after reperfusion. a The mononuclear cells isolated from the brains were stained with antibodies against CD45, CD11b, and Ly6G. Representative plots of infiltrating CD45hiCD11b+ leukocytes identified from ipsilateral and contralateral hemispheres at 48 h after reperfusion are shown (upper panel). N = 8 mice/group. The CD45IntCD11b+ brain-resident microglial cells were separately gated as microglia (MG). The CD45hiCD11b+Ly6G+ neutrophils were identified and are shown in the bottom panel. Ipsi. ipsilateral, Cont. contralateral. The proportion of CD45hiCD11b+-infiltrating cells (b) and CD45hiCD11b+Ly6G+ neutrophils (c) were determined. N = 8 mice/group. **p < 0.01, ***p < 0.001, N.S. no significance, one-way ANOVA with Bonferroni’s post hoc multiple comparison test
Discussion
In this study, we demonstrate that a combination drug composed of three FDA-approved drugs (minocycline, lovastatin, and lamotrigine) protects neurons from cell death induced by OGD. The combination drug showed superior neuroprotection over single drug individually. We further dissected the ischemic injury cascade targeted by the combination drug. The effect of the combination drug on suppressing cell apoptosis is mediated through actions of minocycline. However, lamotrigine, but not minocycline, contributed to suppress OGD-induced DNA damage. These results demonstrate that the combination drug simultaneously targets multiple ischemic injury cascades, whereas single drug inhibits one injury cascade.
Besides acting on neurons, the combination drug targeted different cells involved in the progression of postischemic brain injury. The combination drug suppressed the activation of microglia in response to OGD. The effect is mediated through actions of minocycline to suppress microglial TNF-α production. The combination drug inhibited TNF-α-induced production of MMP9 in brain endothelial cells. This effect of the combination drug is contributed by actions of lovastatin. In contrast to single drug affecting one or two cellular targets, the combination drug acts on multiple cellular targets. Collectively, our results demonstrate that these three drugs act additively to confer a broader spectrum of protection to the brain against multifaceted brain injury after ischemia.
Many drugs exert multiple therapeutic effects with a high dose of drug administration, such as minocycline. However, a high concentration of minocycline treatment may not be completely beneficial and it might exacerbate neurotoxicity after ischemia [16]. A clinical trial using minocycline to treat amyotrophic lateral sclerosis also reports a worsened outcome with a long-term and high-dose treatment regimen [44]. In this study, we used a low dose of minocycline reported as non-cytotoxic in previous studies [45, 46]. Interestingly, we observed that a non-cytotoxic dose of minocycline failed to reduce DNA damage and seemed to increase necrotic cells in neuron cultures challenged with OGD. The co-treatment of lovastatin and lamotrigine counteracted this adverse effect of minocycline. The dose of lamotrigine we used was reported as an IC50 value of lamotrigine to inhibit an excitatory postsynaptic current in brain slice cultures [47]. Besides minocycline, statins exert beneficial outcomes in ischemic stroke associated with high-dose treatment regimens and some adverse effects of high-dose statin treatment are reported [48, 49]. The effects of lovastatin on cultured neurons are controversial in the literature. Lovastatin was shown to protect rat hippocampal neurons from kainate injury [50]. However, it was also reported to cause alteration of microtubules and induce cell death in cultured rat hippocampal neurons, at a similar dose we used in this study [51]. These differences of lovastatin effects might be dose and model dependent. In our model of OGD-induced neuron cell death, we did not observe lovastatin-suppressing cell apoptosis or DNA damage in neurons following OGD. On the other hand, we observed lovastatin-inhibiting TNF-α-induced MMP9 production in brain endothelial cells. Future studies using primary cultured cortical or hippocampal neurons are warranted to further dissecting specific molecular targets of the combination drug and defining an optimal dose of lovastatin for injured neurons after ischemia.
We further examined therapeutic effects of the combination drug versus individual single drug in two animal models. We used a sub-effective dose of three drugs reported in previous studies [8, 15,16,17]. We selected lamotrigine at a dose of 10 mg/kg reported showing minimal protection to the rat brains after transient focal ischemia. Although different high doses of statins were used to test therapeutic effects on animal models of cerebral ischemia, lovastatin at a dose of 20 mg/kg was reported to potentiate antiepileptic effects of lamotrigine against seizures in mice [52]. We selected this dose of lovastatin in our drug combinations. Minocycline was used at different high doses to test in different animal models. It was reported to be well tolerated in humans up to a dose of 10 mg/kg in a dosing-finding study to test minocycline in combination of tissue plasminogen activator [53]. We selected minocycline at a dose of 10 mg/kg in our drug combinations. When compared to single-drug treatment individually, the combination drug showed superior protective effects on hippocampal neurons following transient global ischemia. Moreover, the combination drug, but not single drug, reduced brain infarction after transient focal ischemia.
Microglial cells are highly susceptible to energy failure and sensitive to local changes in CBF [54, 55]. Activated microglia produce inflammatory mediators that are cytotoxic to injured neurons [56,57,58]. We observed an acute activation of microglia following I/R (6 h after reperfusion) in BCCAO mice, which is temporally associated with induction of TNF-α expression in the brain. Microglia isolated from mice that received the combination-drug treatment exhibited less activated phenotype. The inhibitory effect of the combination drug on microglial activation correlates with its suppression on TNF-α induction. In addition, activated microglia produce chemokines that recruit peripheral immune cells into the brain. Among infiltrating peripheral immune cells, neutrophil is widely suggested to contribute to brain tissue damage [59,60,61]. Neutrophils follow a gradient of chemokines produced by the injured tissue and transmigrate through endothelial cells, by which they acquire cytotoxic activation [62]. With treatment of the combination drug which could suppress microglial activation, we observed a significant reduction of neutrophil infiltration in the later phase after I/R in intraluminal tMCAO mice.
Early neuroprotection using prehospital hypothermia after ROSC shows exciting results in some animal and clinical studies. However, some meta-analyses also report controversial results, including an increased risk of mortality [3, 63,64,65,66]. The combination drug might provide an alternative neuroprotective strategy that can be easily administered immediately after ROSC in the field after out-of-hospital cardiac arrest. In acute ischemic stroke, the capability to salvage brain tissue at risk declines rapidly with time. Prehospital delivery of tPA within the “golden hour” or of other neuroprotective agents as early as possible after the onset of ischemia is one promising therapeutic strategy [67, 68]. The ideal prehospital neuroprotective agents should be easy to administer in the ambulance and with low risks of intracranial hemorrhage. The combination drug demonstrates its potential to be given in a prehospital setting in the ambulance.
In conclusion, this study demonstrates the value of a rational approach using FDA-approved drugs in a new combination way to show polytherapeutic effects for the treatment of postischemic brain injury. In the past, many new compounds effective in preclinical models failed in human trials due to unexpected toxic effects. Minocycline, lamotrigine, and lovastatin have been used for a long time to treat different patient populations with infection, epilepsy, or hypercholesterolemia. The combination drug can be potentially used as an early neuroprotective strategy to treat the postischemic brain injury.
References
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–e360. doi:10.1161/CIR.0000000000000350.
Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, et al. Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. N Engl J Med. 2013;369(23):2197–206. doi:10.1056/NEJMoa1310519.
Haugk M, Testori C, Sterz F, Uranitsch M, Holzer M, Behringer W, et al. Relationship between time to target temperature and outcome in patients treated with therapeutic hypothermia after cardiac arrest. Crit Care. 2011;15(2):R101. doi:10.1186/cc10116.
MacLaren R, Gallagher J, Shin J, Varnado S, Nguyen L. Assessment of adverse events and predictors of neurological recovery after therapeutic hypothermia. Ann Pharmacother. 2014;48(1):17–25. doi:10.1177/1060028013511228.
Iadecola C, Anrather J. The immunology of stroke: from mechanisms to translation. Nat Med. 2011;17(7):796–808. doi:10.1038/nm.2399.
Moskowitz MA, Lo EH, Iadecola C. The science of stroke: mechanisms in search of treatments. Neuron. 2010;67(2):181–98. doi:10.1016/j.neuron.2010.07.002.
Papazisis G, Kallaras K, Kaiki-Astara A, Pourzitaki C, Tzachanis D, Dagklis T, et al. Neuroprotection by lamotrigine in a rat model of neonatal hypoxic-ischaemic encephalopathy. Int J Neuropsychopharmacol. 2008;11(3):321–9. doi:10.1017/S1461145707008012.
Smith SE, Meldrum BS. Cerebroprotective effect of lamotrigine after focal ischemia in rats. Stroke. 1995;26(1):117–21. discussion 21-2
Fagan SC, Cronic LE, Hess DC. Minocycline development for acute ischemic stroke. Transl Stroke Res. 2011;2(2):202–8. doi:10.1007/s12975-011-0072-6.
Ni Chroinin D, Asplund K, Asberg S, Callaly E, Cuadrado-Godia E, Diez-Tejedor E, et al. Statin therapy and outcome after ischemic stroke: systematic review and meta-analysis of observational studies and randomized trials. Stroke. 2013;44(2):448–56. doi:10.1161/STROKEAHA.112.668277.
Antoniades C, Bakogiannis C, Leeson P, Guzik TJ, Zhang MH, Tousoulis D, et al. Rapid, direct effects of statin treatment on arterial redox state and nitric oxide bioavailability in human atherosclerosis via tetrahydrobiopterin-mediated endothelial nitric oxide synthase coupling. Circulation. 2011;124(3):335–45. doi:10.1161/CIRCULATIONAHA.110.985150.
Lokk J, Delbari A. Management of depression in elderly stroke patients. Neuropsychiatr Dis Treat. 2010;6:539–49. doi:10.2147/NDT.S7637.
Silverman IE, Restrepo L, Mathews GC. Poststroke seizures. Arch Neurol. 2002;59(2):195–201.
Westendorp WF, Nederkoorn PJ, Vermeij JD, Dijkgraaf MG, van de Beek D. Post-stroke infection: a systematic review and meta-analysis. BMC Neurol. 2011;11:110. doi:10.1186/1471-2377-11-110.
Han H, Qian Q, Yu Y, Zhao D, Sun G. Lamotrigine attenuates cerebral ischemia-induced cognitive impairment and decreases beta-amyloid and phosphorylated tau in the hippocampus in rats. Neuroreport. 2015;26(12):723–7. doi:10.1097/WNR.0000000000000424.
Matsukawa N, Yasuhara T, Hara K, Xu L, Maki M, Yu G, et al. Therapeutic targets and limits of minocycline neuroprotection in experimental ischemic stroke. BMC Neurosci. 2009;10:126. doi:10.1186/1471-2202-10-126.
Potey C, Ouk T, Petrault O, Petrault M, Berezowski V, Salleron J, et al. Early treatment with atorvastatin exerts parenchymal and vascular protective effects in experimental cerebral ischaemia. Br J Pharmacol. 2015;172(21):5188–98. doi:10.1111/bph.13285.
Murakami K, Kondo T, Kawase M, Chan PH. The development of a new mouse model of global ischemia: focus on the relationships between ischemia duration, anesthesia, cerebral vasculature, and neuronal injury following global ischemia in mice. Brain Res. 1998;780(2):304–10.
Walker EJ, Rosenberg GA. TIMP-3 and MMP-3 contribute to delayed inflammation and hippocampal neuronal death following global ischemia. Exp Neurol. 2009;216(1):122–31. doi:10.1016/j.expneurol.2008.11.022.
Yoshioka H, Niizuma K, Katsu M, Okami N, Sakata H, Kim GS, et al. NADPH oxidase mediates striatal neuronal injury after transient global cerebral ischemia. J Cereb Blood Flow Metab. 2011;31(3):868–80. doi:10.1038/jcbfm.2010.166.
Zhen G, Dore S. Optimized protocol to reduce variable outcomes for the bilateral common carotid artery occlusion model in mice. J Neurosci Methods. 2007;166(1):73–80. doi:10.1016/j.jneumeth.2007.06.029.
Wellons JC 3rd, Sheng H, Laskowitz DT, Mackensen GB, Pearlstein RD, Warner DS. A comparison of strain-related susceptibility in two murine recovery models of global cerebral ischemia. Brain Res. 2000;868(1):14–21.
Yang G, Kitagawa K, Matsushita K, Mabuchi T, Yagita Y, Yanagihara T, et al. C57BL/6 strain is most susceptible to cerebral ischemia following bilateral common carotid occlusion among seven mouse strains: selective neuronal death in the murine transient forebrain ischemia. Brain Res. 1997;752(1–2):209–18.
Longa EZ, Weinstein PR, Carlson S, Cummins R. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke. 1989;20(1):84–91.
Kuo PC, Scofield BA, Yu IC, Chang FL, Ganea D, Yen JH. Interferon-beta modulates inflammatory response in cerebral ischemia. J Am Heart Assoc. 2016;5(1) doi:10.1161/JAHA.115.002610.
Kunze R, Urrutia A, Hoffmann A, Liu H, Helluy X, Pham M, et al. Dimethyl fumarate attenuates cerebral edema formation by protecting the blood-brain barrier integrity. Exp Neurol. 2015;266:99–111. doi:10.1016/j.expneurol.2015.02.022.
Liu DZ, Xie KQ, Ji XQ, Ye Y, Jiang CL, Zhu XZ. Neuroprotective effect of paeoniflorin on cerebral ischemic rat by activating adenosine A1 receptor in a manner different from its classical agonists. Br J Pharmacol. 2005;146(4):604–11. doi:10.1038/sj.bjp.0706335.
Li Y, Maher P, Schubert D. A role for 12-lipoxygenase in nerve cell death caused by glutathione depletion. Neuron. 1997;19(2):453–63.
Suo Z, Wu M, Citron BA, Palazzo RE, Festoff BW. Rapid tau aggregation and delayed hippocampal neuronal death induced by persistent thrombin signaling. J Biol Chem. 2003;278(39):37681–9. doi:10.1074/jbc.M301406200.
Liu J, Li L, Suo WZ. HT22 hippocampal neuronal cell line possesses functional cholinergic properties. Life Sci. 2009;84(9–10):267–71. doi:10.1016/j.lfs.2008.12.008.
He M, Liu J, Cheng S, Xing Y, Suo WZ. Differentiation renders susceptibility to excitotoxicity in HT22 neurons. Neural Regen Res. 2013;8(14):1297–306. doi:10.3969/j.issn.1673-5374.2013.14.006.
Goldberg MP, Choi DW. Combined oxygen and glucose deprivation in cortical cell culture: calcium-dependent and calcium-independent mechanisms of neuronal injury. J Neurosci. 1993;13(8):3510–24.
Sasaki T, Takemori H, Yagita Y, Terasaki Y, Uebi T, Horike N, et al. SIK2 is a key regulator for neuronal survival after ischemia via TORC1-CREB. Neuron. 2011;69(1):106–19. doi:10.1016/j.neuron.2010.12.004.
Kang Y, Tiziani S, Park G, Kaul M, Paternostro G. Cellular protection using Flt3 and PI3Kalpha inhibitors demonstrates multiple mechanisms of oxidative glutamate toxicity. Nat Commun. 2014;5:3672. doi:10.1038/ncomms4672.
Ponomarev ED, Shriver LP, Dittel BN. CD40 expression by microglial cells is required for their completion of a two-step activation process during central nervous system autoimmune inflammation. J Immunol. 2006;176(3):1402–10.
Chalkias A, Xanthos T. Post-cardiac arrest brain injury: pathophysiology and treatment. J Neurol Sci. 2012;315(1–2):1–8. doi:10.1016/j.jns.2011.12.007.
Horn M, Schlote W. Delayed neuronal death and delayed neuronal recovery in the human brain following global ischemia. Acta Neuropathol. 1992;85(1):79–87.
Nagao K. Therapeutic hypothermia following resuscitation. Curr Opin Crit Care. 2012;18(3):239–45. doi:10.1097/MCC.0b013e3283523f4a.
Petito CK, Feldmann E, Pulsinelli WA, Plum F. Delayed hippocampal damage in humans following cardiorespiratory arrest. Neurology. 1987;37(8):1281–6.
Badhiwala JH, Nassiri F, Alhazzani W, Selim MH, Farrokhyar F, Spears J, et al. Endovascular thrombectomy for acute ischemic stroke: a meta-analysis. JAMA. 2015;314(17):1832–43. doi:10.1001/jama.2015.13767.
Campbell BC, Donnan GA, Lees KR, Hacke W, Khatri P, Hill MD, et al. Endovascular stent thrombectomy: the new standard of care for large vessel ischaemic stroke. Lancet Neurol. 2015;14(8):846–54. doi:10.1016/S1474-4422(15)00140-4.
Sutherland BA, Neuhaus AA, Couch Y, Balami JS, DeLuca GC, Hadley G, et al. The transient intraluminal filament middle cerebral artery occlusion model as a model of endovascular thrombectomy in stroke. J Cereb Blood Flow Metab. 2016;36(2):363–9. doi:10.1177/0271678X15606722.
Amantea D, Micieli G, Tassorelli C, Cuartero MI, Ballesteros I, Certo M, et al. Rational modulation of the innate immune system for neuroprotection in ischemic stroke. Front Neurosci. 2015;9:147. doi:10.3389/fnins.2015.00147.
Gordon PH, Moore DH, Miller RG, Florence JM, Verheijde JL, Doorish C, et al. Efficacy of minocycline in patients with amyotrophic lateral sclerosis: a phase III randomised trial. Lancet Neurol. 2007;6(12):1045–53. doi:10.1016/S1474-4422(07)70270-3.
Kernt M, Hirneiss C, Neubauer AS, Kampik A. Minocycline is cytoprotective in human corneal endothelial cells and induces anti-apoptotic B-cell CLL/lymphoma 2 (Bcl-2) and X-linked inhibitor of apoptosis (XIAP). Br J Ophthalmol. 2010;94(7):940–6. doi:10.1136/bjo.2009.165092.
Xing C, Levchenko T, Guo S, Stins M, Torchilin VP, Lo EH. Delivering minocycline into brain endothelial cells with liposome-based technology. J Cereb Blood Flow Metab. 2012;32(6):983–8. doi:10.1038/jcbfm.2012.48.
Lee CY, Fu WM, Chen CC, Su MJ, Liou HH. Lamotrigine inhibits postsynaptic AMPA receptor and glutamate release in the dentate gyrus. Epilepsia. 2008;49(5):888–97. doi:10.1111/j.1528-1167.2007.01526.x.
Flint AC, Kamel H, Navi BB, Rao VA, Faigeles BS, Conell C, et al. Statin use during ischemic stroke hospitalization is strongly associated with improved poststroke survival. Stroke. 2012;43(1):147–54. doi:10.1161/STROKEAHA.111.627729.
Selim MH, Molina CA. High-dose statin for every stroke: the good, the bad, and the unknown. Stroke. 2012;43(7):1996–7. doi:10.1161/STROKEAHA.111.648832.
He X, Jenner AM, Ong WY, Farooqui AA, Patel SC. Lovastatin modulates increased cholesterol and oxysterol levels and has a neuroprotective effect on rat hippocampal neurons after kainate injury. J Neuropathol Exp Neurol. 2006;65(7):652–63. doi:10.1097/01.jnen.0000225906.82428.69.
Meske V, Albert F, Richter D, Schwarze J, Ohm TG. Blockade of HMG-CoA reductase activity causes changes in microtubule-stabilizing protein tau via suppression of geranylgeranylpyrophosphate formation: implications for Alzheimer’s disease. Eur J Neurosci. 2003;17(1):93–102.
Russo E, di Donato Paola E, Gareri P, Siniscalchi A, Labate A, Gallelli L, et al. Pharmacodynamic potentiation of antiepileptic drugs’ effects by some HMG-CoA reductase inhibitors against audiogenic seizures in DBA/2 mice. Pharmacol Res. 2013;70(1):1–12. doi:10.1016/j.phrs.2012.12.002.
Fagan SC, Waller JL, Nichols FT, Edwards DJ, Pettigrew LC, Clark WM, et al. Minocycline to improve neurologic outcome in stroke (MINOS): a dose-finding study. Stroke. 2010;41(10):2283–7. doi:10.1161/STROKEAHA.110.582601.
Gimeno-Bayon J, Lopez-Lopez A, Rodriguez MJ, Mahy N. Glucose pathways adaptation supports acquisition of activated microglia phenotype. J Neurosci Res. 2014;92(6):723–31. doi:10.1002/jnr.23356.
Masuda T, Croom D, Hida H, Kirov SA. Capillary blood flow around microglial somata determines dynamics of microglial processes in ischemic conditions. Glia. 2011;59(11):1744–53. doi:10.1002/glia.21220.
Clausen BH, Lambertsen KL, Babcock AA, Holm TH, Dagnaes-Hansen F, Finsen B. Interleukin-1beta and tumor necrosis factor-alpha are expressed by different subsets of microglia and macrophages after ischemic stroke in mice. J Neuroinflammation. 2008;5:46. doi:10.1186/1742-2094-5-46.
Denes A, Vidyasagar R, Feng J, Narvainen J, McColl BW, Kauppinen RA, et al. Proliferating resident microglia after focal cerebral ischaemia in mice. J Cereb Blood Flow Metab. 2007;27(12):1941–53. doi:10.1038/sj.jcbfm.9600495.
Benakis C, Garcia-Bonilla L, Iadecola C, Anrather J. The role of microglia and myeloid immune cells in acute cerebral ischemia. Front Cell Neurosci. 2014;8:461. doi:10.3389/fncel.2014.00461.
Garcia-Bonilla L, Moore JM, Racchumi G, Zhou P, Butler JM, Iadecola C, et al. Inducible nitric oxide synthase in neutrophils and endothelium contributes to ischemic brain injury in mice. J Immunol. 2014;193(5):2531–7. doi:10.4049/jimmunol.1400918.
Stowe AM, Adair-Kirk TL, Gonzales ER, Perez RS, Shah AR, Park TS, et al. Neutrophil elastase and neurovascular injury following focal stroke and reperfusion. Neurobiol Dis. 2009;35(1):82–90. doi:10.1016/j.nbd.2009.04.006.
Gelderblom M, Weymar A, Bernreuther C, Velden J, Arunachalam P, Steinbach K, et al. Neutralization of the IL-17 axis diminishes neutrophil invasion and protects from ischemic stroke. Blood. 2012;120(18):3793–802. doi:10.1182/blood-2012-02-412726.
Allen C, Thornton P, Denes A, McColl BW, Pierozynski A, Monestier M, et al. Neutrophil cerebrovascular transmigration triggers rapid neurotoxicity through release of proteases associated with decondensed DNA. J Immunol. 2012;189(1):381–92. doi:10.4049/jimmunol.1200409.
Maynard C, Longstreth WT Jr, Nichol G, Hallstrom A, Kudenchuk PJ, Rea T, et al. Effect of prehospital induction of mild hypothermia on 3-month neurological status and 1-year survival among adults with cardiac arrest: long-term follow-up of a randomized, clinical trial. J Am Heart Assoc. 2015;4(3):e001693. doi:10.1161/JAHA.114.001693.
Zhao D, Abella BS, Beiser DG, Alvarado JP, Wang H, Hamann KJ, et al. Intra-arrest cooling with delayed reperfusion yields higher survival than earlier normothermic resuscitation in a mouse model of cardiac arrest. Resuscitation. 2008;77(2):242–9. doi:10.1016/j.resuscitation.2007.10.015.
Diao M, Huang F, Guan J, Zhang Z, Xiao Y, Shan Y, et al. Prehospital therapeutic hypothermia after cardiac arrest: a systematic review and meta-analysis of randomized controlled trials. Resuscitation. 2013;84(8):1021–8. doi:10.1016/j.resuscitation.2013.02.003.
Scolletta S, Taccone FS, Nordberg P, Donadello K, Vincent JL, Castren M. Intra-arrest hypothermia during cardiac arrest: a systematic review. Crit Care. 2012;16(2):R41. doi:10.1186/cc11235.
Audebert HJ, Saver JL, Starkman S, Lees KR, Endres M. Prehospital stroke care: new prospects for treatment and clinical research. Neurology. 2013;81(5):501–8. doi:10.1212/WNL.0b013e31829e0fdd.
Ebinger M, Winter B, Wendt M, Weber JE, Waldschmidt C, Rozanski M, et al. Effect of the use of ambulance-based thrombolysis on time to thrombolysis in acute ischemic stroke: a randomized clinical trial. JAMA. 2014;311(16):1622–31. doi:10.1001/jama.2014.2850.
Acknowledgments
The authors thank Barbara A. Scofield for the skilled technical assistance. The authors thank Gregory Wemhoff, PhD for the important intellectual comment to the manuscript.
Author information
Authors and Affiliations
Contributions
I-C. Y. contributed to the overall study design, conceived the study, contributed to the research data, and wrote and edited the manuscript. P-C. K. contributed to the research data of transient focal ischemia mouse model, analyzed the data, and wrote and edited the manuscript. J-H. Y. contributed to the design of experiments and discussion, and reviewed and edited the manuscript. H. C. P. contributed to the research data of in vitro experiments and analyzed the data. E. T. C. contributed to research data of histology/immunohistochemistry staining and analyzed the data. B. C. H-G. and R. D. S. contributed to the discussion and reviewed and edited the manuscript. F-L. C. contributed to the overall study design, conceived the study, contributed to the discussion, and reviewed and edited the manuscript.
Corresponding authors
Ethics declarations
Sources of Funding
This work was financially supported by the IU Foundation, Lutheran Foundation, and Steel Dynamics Foundation. J-H. Yen was supported by the American Heart Association (AHA; 12SDG8170005).
Disclosures
The authors declare that the research was conducted in the absence of any financial relationships that could be constructed as a potential conflict of interest.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. This article does not contain any studies with human participants performed by any of the authors.
Electronic supplementary material
.
ESM 1
(PDF 329 kb)
Rights and permissions
About this article
Cite this article
Yu, IC., Kuo, PC., Yen, JH. et al. A Combination of Three Repurposed Drugs Administered at Reperfusion as a Promising Therapy for Postischemic Brain Injury. Transl. Stroke Res. 8, 560–577 (2017). https://doi.org/10.1007/s12975-017-0543-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-017-0543-5