Abstract
Emerging data suggest that exosomal microRNA (miRNA) may provide potential biomarkers in acute ischemic stroke. However, the effects of ischemia-reperfusion on total versus exosomal miRNA responses in circulating blood remain to be fully defined. Here, we quantified levels of miR-126 in whole serum versus exosomes extracted from serum and compared these temporal profiles against reperfusion and outcomes in a rat model of acute focal cerebral ischemia. First, in vitro experiments confirmed the vascular origin and changes in miR-126 in brain endothelial cultures subjected to oxygen-glucose deprivation. Then in vivo experiments were performed by inducing permanent or transient focal cerebral ischemia in rats, and total serum and exosomal miR-126 levels were quantified, along with measurements of infarction and neurological outcomes. Exosomal levels of miR-126 showed a transient reduction at 3 h post-ischemia that appeared to normalize back close to pre-ischemic baselines after 24 h. There were no detectable differences in exosomal miR-126 responses in permanent or transient ischemia. Serum miR-126 levels appeared to differ in permanent versus transient ischemia. Significant reductions in serum miR-126 were detected at 3 h after permanent ischemia but not transient ischemia. By 24 h, serum miR-126 levels were back close to baseline in both permanent and transient ischemia. Overall, there were no correlations between serum miR-126 and exosomal miR-126. This proof-of-concept study suggests that changes in serum miR-126 may be able to distinguish severe permanent ischemia from milder injury after transient ischemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
MicroRNAs (miRNAs) are endogenously expressed ∼22 nucleotides long, noncoding RNAs that control a wide spectrum of cellular function [1–3]. Although their mechanism of action is not yet completely understood, recent studies suggested that specific miRNAs could bind to target regions of certain genes to control their expression by either repression or activation of mRNA translation/transcription [4, 5]. A single miRNA can regulate thousands of downstream target genes and influence the entire gene networks and downstream protein synthesis [6–8]. It has been demonstrated that miRNAs play important roles in developmental and functional aspects of the central nervous system and in many neurological diseases [9, 10]. Therefore, miRNAs are potentially important candidates for stroke diagnosis and therapeutics since they will surely be involved in multiple pathways in the ischemic cascade [11].
In the context of stroke, miRNAs have been implicated in multiple pathogenic processes including atherosclerosis (miR-21, miR-126), hyperlipidemia (miR-33, miR-125a-5p), hypertension (miR-155), plaque rupture (miR-222, miR-210), blood brain barrier disruption (miR-15a), and caspase-mediated cell death (miR-497) [12]. Accordingly, an increasing number of exploratory studies have been performed to assess miRNAs isolated from blood of human stroke patients, and blood and brain tissue from animal stroke models [13–17]. Thus far, the cumulative data are complex, and both increased and decreased miRNA responses have been documented, so it has been challenging to separate stroke-specific profiles from those incurred as a general response to vascular dysfunction. More recently, miRNAs from exosomes have been explored as a potential specific response element in stroke since extracellular vesicles and their cargo can be regulated by multiple cells in the neurovascular unit [18]. However, in spite of this burgeoning interest, how specific miRNA responses in exosomes compare versus general responses in total blood after stroke remains to be fully defined. Therefore, in this proof-of-concept study, we explored miR-126 in exosomes and serum and compared these profiles with outcomes after severe permanent or mild transient focal cerebral ischemia in rats.
Materials and Methods
Brain Endothelial Cell Cultures
Human brain endothelial cells (CSC Systems, Kirkland, WA, USA) were grown as previously described on collagen-coated dishes [19]. Confluent cells were washed twice with PBS and then subjected to 3- or 6-h oxygen-glucose deprivation (OGD). At the end of OGD, culture media and cells were collected for lactate dehydrogenase assay (LDH, as a measure of cell death) or exosome isolation. All culture media contained no serum to avoid exogenous microvesicle contamination. Exosome isolation was performed as previously described [20]. Briefly, exosomes were collected from conditioned media after centrifuge at 300g, 10 min and 2000g, and 20 min sequentially to discard cell debris. The resultant supernatant went through detection with NanoSight LM10 nanoparticle characterization system (NanoSight) equipped with a blue laser (405 nm) illumination.
Rat Focal Ischemia Model
Adult male Wistar rats (260–280 g, Charles River Lab, Wilmington, USA) were subjected to focal cerebral ischemia using standard methods that have been previously described [21]. Briefly, rats were initially anesthetized with 1–2 % isoflurane by face mask. Rectal temperature was maintained at 37 °C ± 0.5 °C via a temperature-regulated heating pad. Regional cerebral blood flow was monitored using laser Doppler flowmetry (LDF) to ensure adequate focal ischemia. Animals that did not show a regional cerebral blood flow reduction to <30 % of pre-ischemia baseline levels were excluded. Rats were subjected to either transient (75 min, n = 27) and permanent (n = 27) middle cerebral artery occlusion by intraluminal occlusion of the right middle cerebral artery. Sham-operated animals (n = 5) underwent the same anesthesia and surgical procedures without arterial occlusion. All animal experiments were approved by the MGH Institutional Animal Care and Use Committee in accordance with the NIH Guide for the Care and Use of Laboratory Animals. Blood samples were obtained before ischemia and 3 and 24 h after ischemia. Fresh blood (1 mL) samples were immediately added to nonadditive tubes (BD Microtainer™, USA). After centrifugation (3000 rpm, 30mins, 4 °C), supernatant was collected as serum. Samples were stored at −80 °C until further processing. Total exosomes were isolated from serum using the Invitrogen™ total exosome isolation reagent (Applied Biosystems, Austin, TX, USA) according to manufacturer’s protocol. Neurological Severity Scores (mNSS) were assessed to evaluate the ischemic deficits at 24 h, and brains were removed to quantify infarction using standard tetrazolium chloride staining. To exclude possible confounding effects of brain swelling, an indirect method was used to calculate lesion volumes.
miRNA Quantification
Total RNA (with miRNA) was extracted from serum and serum-isolated exosomes using TaqMan™ miRNeasy Micro Kit (Applied Biosystems) according to the manufacturer’s protocol. The reverse transcription was performed using the TaqMan™ MiRNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA, USA). Real-time PCR was performed using 7500 Real-Time PCR System (Applied Biosystems). All reactions were run in triplicate. The primers of miR-126 (an endothelial marker) and miR-124a (a comparative neuronal marker) were purchased from Applied Biosystems. The 2−ΔΔCt method was used to determine the relative changes in gene expression. The relative expression level of miR-126 (ΔCt) was calculated by minus Ct value of U6 from Ct value of miR-126.
Statistical Analysis
Statistical analysis was performed by t test (infarct volume and mNSS), one-way ANOVA, and followed by Tukey post hoc tests (miR-126), and correlation analysis was performed using GraphPad Prism (version 6.0). P < 0.05 was considered statistically significant.
Results
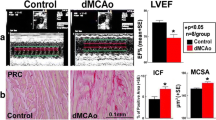
Brain endothelial cell miR-126 responses after oxygen-glucose deprivation
We selected miR-126 as our initial candidate reporter of neurovascular damage in stroke because it is specifically and highly expressed in endothelial cells and is known to be involved in the regulation of vascular integrity, endothelial function, and angiogenesis [22–24]. miR-126 was detectable in all exosomal preparations from our human brain endothelial cultures, confirming their endothelial cellular origins. Compared to DMEM normal controls, miR-126 levels were significantly reduced after oxygen-glucose deprivation (Fig. 1).
Infarction and neurological deficits after focal cerebral ischemia in rats
Twenty four of focal cerebral ischemia resulted in well-defined infarctions comprising cortical and subcortical areas of the middle cerebral artery distribution. As expected, infarct volumes were larger in permanent compared to transient ischemia (Fig. 2a). Correspondingly, neurological deficits were also more severe in permanent versus transient ischemia (Fig. 2b). Mortality in the transient ischemia group was 7.4 %, and mortality in the permanent ischemia group was 18.5 % (Fig. 2c). These two models therefore allowed us to ask how miR-126 responses may potentially differ according to stroke severity.
Tissue and functional outcomes after severe permanent versus mild transient focal cerebral ischemia. a Significant difference in infarction volume between transient (tMCAO) and permanent (pMCAO) ischemia groups. *p < 0.05. b Significant difference in modified neurological scores (mNSS) between transient (tMCAO) and permanent (pMCAO) ischemia groups. *p < 0.05. c Mortality in tMCAO and pMCAO groups
miR-126 profiles in transient versus permanent focal cerebral ischemia
Delta-CT values indicated that measurable levels of miR-126 were obtained for exosome and serum samples across all groups (Fig. 3a, b). Sham samples showed no change in miR-126 levels. Compared to levels before ischemic onset, both transient and permanent ischemia samples showed a rapid and significant reduction in exosomal miR-126 at 3 h (Fig. 3c). This response appeared to be temporary, and by 24 h, exosomal miR-126 levels mostly renormalized close to pre-ischemia baseline levels (Fig. 3c).
MiR-126 levels in exosomes and whole serum after transient and permanent ischemia. a Expression levels of exosomal miR-126 (delta-CT values) before and after ischemia. b Expression levels of serum miR-126 (delta-CT values) before and after ischemia. c Log-10 fold changes of exosomal miR-126 levels versus pre-ischemia baselines. Compared with baseline levels, both transient and permanent ischemia samples showed a rapid significant reduction in exosomal miR-126 at 3 h (p < 0.05). Both transient and permanent ischemia showed significant difference in exosomal miR-126 between 3 and 24 h after ischemia. *p < 0.05. d Log-10 fold changes of serum miR-126 levels versus pre-ischemia baselines. There was significant difference of serum miR-126 levels between transient and permanent ischemia at 3 h. *p < 0.05
Next, we examined miR-126 levels in the whole serum. Compared to exosomes, serum responses may not be as sensitive, and no clear effects of cerebral ischemia were detectable for either permanent or transient ischemia, except for the early 3-h samples from the permanent ischemia group. Compared with the baseline levels of miR-126 before ischemia, permanent ischemia significantly decreased serum miR-126 levels at 3 h (Fig. 3d). In contrast, no significant changes in serum miR-126 were observed after milder injury induced by transient ischemia (Fig. 3d). By 24 h, all serum miR-126 levels appeared to renormalize back close to baseline (Fig. 3d).
Overall, there were no correlations between exosome and serum miR-126 levels across all groups (Fig. 4). When comparing against outcomes, serum levels of miR-126 appeared to be significantly correlated with infarction volumes at 3 h (Table 1). But, no other correlations were detected for 24 h or for exosomal miR-126 at any timepoint (Table 1).
As an additional control, we also attempted to measure levels of miR-124, a known neuronal marker. Within the sensitivity limits of our system, we were unable to detect miR-124 in any of our serum or exosomal samples post-ischemia (data not shown).
Discussion
Finding biomarkers in stroke are important because these indices may provide quantitative endpoints to assess stroke evolution, measure therapeutic response, and potentially separate responders from nonresponders in clinical trials [25]. Recently, the pursuit of stroke biomarkers has begun to focus on miRNAs. MiRNAs comprise a subset of noncoding RNAs that may play a role in stroke pathophysiology [26], and because they can be released into extracellular space, microRNAs may also reflect the status of stroke-injured tissue. In this study, we used a combination of endothelial cell cultures and in vivo rat focal ischemia models to assess the hypothesis that circulating levels of the vascular miRNA miR-126 may be correlated with infarction severity and ischemia-reperfusion over time. During hyperacute stroke (3 h after ischemia), exosomal miR-126 levels significantly decreased in both transient and permanent ischemia, whereas serum miR-126 levels decreased only in permanent ischemia. In contrast, at 3 h after ischemia, serum miR-126 levels, not exosomal miR-126 levels, showed significant difference between transient and permanent ischemia. Our results indicated that whereas exosomal miR-126 levels may be more sensitive than serum miR-126 levels, changes in miR-126 in whole serum may distinguish severe injury after permanent focal ischemia from milder injury after transient focal ischemia. Furthermore, serum miR-126 levels at 3 h may also be correlated with infarction volumes at 24 h. These initial results provide proof-of-concept that circulating levels of miR-126 may potentially provide insight into the severity of tissue damage and status of ischemia-reperfusion after acute stroke.
Although our results suggest intriguing differences in miR-126 response in permanent versus transient ischemia, the underlying pathomechanisms remain unclear. The downregulation of miR-126 in permanent focal ischemia may be consistent with previous studies, where miR-126 has been associated with vascular pathologies. Hypoxia is known to decrease miR-126 both in vitro and in vivo [14, 27]. Pilot studies in stroke patients suggest that circulating miR-126 levels may be downregulated up to 24 weeks post-stroke [28]. Furthermore, miR-126 has also been associated with the progression of type 2 diabetes, hypertension, and atherosclerosis [29–31]. In contrast, our data demonstrate that after transient ischemia, miR-126 is positively correlated with infarct size and reperfusion, which may be associated with an inflammatory response [32, 33]. Hence, downstream inflammatory targets of miR-126 may be especially relevant for reperfusion injury. MiR-126 is known to suppress vascular cell adhesion molecule-1 and C-X-C motif chemokine 12, and it may also inhibit vascular endothelial growth factor signaling by repressing Spred-1 and PI3-kinase pathways [31, 34–36]. Taken together, our findings may be consistent with the overall idea that miR-126 responses contribute to the balance between beneficial and detrimental effects of reperfusion. Further investigations into the mechanistic role of miR-126 or other miRNAs in ischemia and reperfusion injury will be useful [32].
For this initial study, we decided to focus on a vascular signal because the cerebral endothelial system should be the major contributor in circulating signals in the blood [37, 38]. However, the blood-brain barrier leakage occurs after stroke, so central signals may also leak into the circulation. We attempted to look for miR-124, which is thought to be the most abundant miRNA in the brain [39]. Its expression increases on neuronal differentiation and reaches maximal levels in mature neurons. Previous studies suggested that after focal cerebral ischemia in rats, miR-124a in subventricular regions becomes significantly reduced [40]. But, effects on circulating miR-124 have not been confirmed. In the present study, we also tried to detect circulating miR-124 based on the possibility that it may leak through a compromised blood-brain barrier. However, within the sensitivity limits of our system, we were unable to detect significant levels of miR-124 in serum of exosomal samples. Future studies to systematically map out other central vs peripheral miRNA signals should be warranted.
Although our initial data here may also point to interesting correlations between total serum miR-126 and infarct outcomes, the differences between exosome and nonexosome compartments remain to be clarified. miRNAs may be stable in the circulation which supports their potential use as disease biomarkers [41]. In part, this stability is thought to be mediated via exosomes that may represent an encapsulation and delivery system that protects miRNAs from external RNases. Several studies have supported this idea of functional miRNA transfer by exosomes and observed the uptake of exosomal miRNAs into cells in vitro [42–45]. Circulating miR-126 should be mostly derived from endothelial cells, which may also be the main source of circulating exosomes. One study showed that endothelial miR-126 shuttled by exosomes is biologically active in target cells and modulates adhesive and migratory abilities of leukemia cells [46]. Hence, the differential of exosomal miR-126 may also indicate its potential role in connecting cerebral ischemic pathophysiology with systemic responses in other cell types and organs. However, we were unable to find any correlations between serum and exosomal miR-126 levels in our study, so further investigations will be needed to define how these signals are sorted between compartments.
Taken together, our findings here suggest that specific responses in circulating miR-126 within total serum and exosomes may provide quantitative profiles that correlate with infarction severity and ischemia-reperfusion. However, there are still several caveats in this proof-of-concept study. First, further studies are needed to define the source for our miR-126 responses. Our brain endothelial culture data are consistent with our in vivo rat stroke model data, but it remains possible that many other nonvascular cell types may also be involved. Second, within the limits of this initial study, we cannot precisely determine the effects of the central versus systemic responses. Blood-brain barrier leakage is a key part of ischemia-reperfusion injury. How various miRNA signals from brain interact with those from other organs and circulating blood cells remains to be rigorously investigated. Third, we only focus on acute timepoints in this initial study. It is possible that the miR-126 profiles will continue to evolve over time. How circulating miR-126 responses correspond to long-term reperfusion and neurological outcomes will have to be determined in future studies. Fourth, our in vivo experiments were performed in healthy young male rats. How miR-126 mechanisms are modified in aged or female rats with stroke comorbidities such as hypertension or diabetes will have to be considered as well. This may be especially important since miR-126 has been implicated in various mechanisms of diabetes, hypertension, and atherosclerosis. Fifth, we only focus on a single miRNA endpoint. Although our initial focus on miR-126 may be reasonable since it is known to reflect vascular integrity, it is likely that many other miRNAs will be modulated in ischemia-reperfusion. Future studies will be required to carefully assess the network response and potentially identify an integrated miRNA signature for stroke. Finally, the primary goal of this study was to assess circulating miR-126 responses as potential biomarkers in stroke. However, beyond a role as a surrogate reporter of pathophysiology, increasing evidence now points to the possibility of using or targeting miRNAs as a therapeutic approach as well [47]. It should be interesting to ask whether modulating miR-126 and its attendant exosomal carrier systems may be exploited for novel treatment strategies.
In conclusion, this proof-of-concept study using cell culture models of oxygen-glucose deprivation and rat models of focal cerebral ischemia suggests that although changes in exosomal miR-126 levels in blood may be more sensitive to cerebral ischemia (i.e., able to respond to both mild and severe ischemia), total serum miR-126 may be more specific to the severity of ischemia (i.e., responds only to severe ischemia). However, we were unable to find clear relationships between exosomal miR-126 and serum responses, so the mechanisms of how miR-126 is sorted and compartmentalized after release from damaged vasculature remain to be defined. MiRNA is now known to comprise critical mediators in CNS function and disease [48]. Further investigations are warranted to assess how exosomal versus total microRNA responses participate in stroke pathophysiology.
References
Ambros V. The functions of animal microRNAs. Nature. 2004;431(7006):350–5.
Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116(2):281–97.
Grishok A, Pasquinelli AE, Conte D, Li N, Parrish S, Ha I, et al. Genes and mechanisms related to RNA interference regulate expression of the small temporal RNAs that control C. elegans developmental timing. Cell. 2001;106(1):23–34.
Duursma AM, Kedde M, Schrier M, le Sage C, Agami R. miR-148 targets human DNMT3b protein coding region. Rna. 2008;14(5):872–7.
Place RF, Li LC, Pookot D, Noonan EJ, Dahiya R. MicroRNA-373 induces expression of genes with complementary promoter sequences. Proc Natl Acad Sci U S A. 2008;105(5):1608–13.
Lewis BP, Shih IH, Jones-Rhoades MW, Bartel DP, Burge CB. Prediction of mammalian microRNA targets. Cell. 2003;115(7):787–98.
Miska EA, Alvarez-Saavedra E, Townsend M, Yoshii A, Sestan N, Rakic P, et al. Microarray analysis of microRNA expression in the developing mammalian brain. Genome Biol. 2004;5(9):R68.
Lai M, Macleod M. MicroRNA--taking regulation of protein synthesis to another level. Cerebrovasc Dis. 2005;20(1):49–50. discussion.
Fiore R, Siegel G, Schratt G. MicroRNA function in neuronal development, plasticity and disease. Biochim Biophys Acta. 2008;1779(8):471–8.
Christensen M, Schratt GM. microRNA involvement in developmental and functional aspects of the nervous system and in neurological diseases. Neurosci Lett. 2009;466(2):55–62.
Vemuganti R. The microRNAs and stroke: no need to be coded to be counted. Transl Stroke Res. 2010;1(3):158–60.
Rink C, Khanna S. MicroRNA in ischemic stroke etiology and pathology. Physiol Genomics. 2011;43(10):521–8.
Sorensen SS, Nygaard AB, Nielsen MY, Jensen K, Christensen T. miRNA expression profiles in cerebrospinal fluid and blood of patients with acute ischemic stroke. Transl Stroke Res. 2014;5(6):711–8.
Dharap A, Bowen K, Place R, Li LC, Vemuganti R. Transient focal ischemia induces extensive temporal changes in rat cerebral microRNAome. J Cereb Blood Flow Metab. 2009;29(4):675–87.
Selvamani A, Williams MH, Miranda RC, Sohrabji F. Circulating miRNA profiles provide a biomarker for severity of stroke outcomes associated with age and sex in a rat model. Clin Sci (Lond). 2014;127(2):77–89.
Sepramaniam S, Tan JR, Tan KS, DeSilva DA, Tavintharan S, Woon FP, et al. Circulating microRNAs as biomarkers of acute stroke. Int J Mol Sci. 2014;15(1):1418–32.
Chevillet JR, Lee I, Briggs HA, He Y, Wang K. Issues and prospects of microRNA-based biomarkers in blood and other body fluids. Molecules. 2014;19(5):6080–105.
Smalheiser NR. Do Neural Cells Communicate with Endothelial Cells via Secretory Exosomes and Microvesicles? Cardiovasc Psychiatry Neurol. 2009;2009:383086.
Wu L, Walas S, Leung W, Sykes DB, Wu J, Lo EH, et al. Neuregulin1-beta decreases IL-1beta-induced neutrophil adhesion to human brain microvascular endothelial cells. Transl Stroke Res. 2015;6(2):116–24.
Balaj L, Lessard R, Dai L, Cho YJ, Pomeroy SL, Breakefield XO, et al. Tumour microvesicles contain retrotransposon elements and amplified oncogene sequences. Nat Commun. 2011;2:180.
Asahi M, Asahi K, Jung JC, del Zoppo GJ, Fini ME, Lo EH. Role for matrix metalloproteinase 9 after focal cerebral ischemia: effects of gene knockout and enzyme inhibition with BB-94. J Cereb Blood Flow Metab. 2000;20(12):1681–9.
Wang S, Aurora AB, Johnson BA, Qi X, McAnally J, Hill JA, et al. The endothelial-specific microRNA miR-126 governs vascular integrity and angiogenesis. Dev Cell. 2008;15(2):261–71.
Wu F, Yang Z, Li G. Role of specific microRNAs for endothelial function and angiogenesis. Biochem Biophys Res Commun. 2009;386(4):549–53.
van Solingen C, Seghers L, Bijkerk R, Duijs JM, Roeten MK, van Oeveren-Rietdijk AM, et al. Antagomir-mediated silencing of endothelial cell specific microRNA-126 impairs ischemia-induced angiogenesis. J Cell Mol Med. 2009;13(8A):1577–85.
Foerch C, Montaner J, Furie KL, Ning MM, Lo EH. Invited article: searching for oracles? Blood biomarkers in acute stroke. Neurology. 2009;73(5):393–9.
Vemuganti R. All’s well that transcribes well: non-coding RNAs and post-stroke brain damage. Neurochem Int. 2013;63(5):438–49.
Ye P, Liu J, He F, Xu W, Yao K. Hypoxia-induced deregulation of miR-126 and its regulative effect on VEGF and MMP-9 expression. Int J Med Sci. 2014;11(1):17–23.
Long G, Wang F, Li H, Yin Z, Sandip C, Lou Y, et al. Circulating miR-30a, miR-126 and let-7b as biomarker for ischemic stroke in humans. BMC Neurol. 2013;13:178.
Kontaraki JE, Marketou ME, Zacharis EA, Parthenakis FI, Vardas PE. MicroRNA-9 and microRNA-126 expression levels in patients with essential hypertension: potential markers of target-organ damage. J Am Soc Hypertens. 2014;8(6):368–75.
Zampetaki A, Kiechl S, Drozdov I, Willeit P, Mayr U, Prokopi M, et al. Plasma microRNA profiling reveals loss of endothelial miR-126 and other microRNAs in type 2 diabetes. Circ Res. 2010;107(6):810–7.
Wei Y, Nazari-Jahantigh M, Neth P, Weber C, Schober A. MicroRNA-126, −145, and −155: a therapeutic triad in atherosclerosis? Arterioscler Thromb Vasc Biol. 2013;33(3):449–54.
Di Y, Lei Y, Yu F, Changfeng F, Song W, Xuming M. MicroRNAs expression and function in cerebral ischemia reperfusion injury. J Mol Neurosci. 2014;53(2):242–50.
Weiss JB, Eisenhardt SU, Stark GB, Bode C, Moser M, Grundmann S. MicroRNAs in ischemia-reperfusion injury. Am J Cardiovasc Dis. 2012;2(3):237–47.
Harris TA, Yamakuchi M, Ferlito M, Mendell JT, Lowenstein CJ. MicroRNA-126 regulates endothelial expression of vascular cell adhesion molecule 1. Proc Natl Acad Sci U S A. 2008;105(5):1516–21.
Fish JE, Santoro MM, Morton SU, Yu S, Yeh RF, Wythe JD, et al. miR-126 regulates angiogenic signaling and vascular integrity. Dev Cell. 2008;15(2):272–84.
Meng S, Cao JT, Zhang B, Zhou Q, Shen CX, Wang CQ. Downregulation of microRNA-126 in endothelial progenitor cells from diabetes patients, impairs their functional properties, via target gene Spred-1. J Mol Cell Cardiol. 2012;53(1):64–72.
Ning M, Sarracino DA, Kho AT, Guo S, Lee SR, Krastins B, et al. Proteomic temporal profile of human brain endothelium after oxidative stress. Stroke. 2011;42(1):37–43.
Guo S, Lo EH. Dysfunctional cell-cell signaling in the neurovascular unit as a paradigm for central nervous system disease. Stroke. 2009;40(3 Suppl):S4–7.
Weng H, Shen C, Hirokawa G, Ji X, Takahashi R, Shimada K, et al. Plasma miR-124 as a biomarker for cerebral infarction. Biomed Res. 2011;32(2):135–41.
Liu XS, Chopp M, Zhang RL, Tao T, Wang XL, Kassis H, et al. MicroRNA profiling in subventricular zone after stroke: MiR-124a regulates proliferation of neural progenitor cells through Notch signaling pathway. PLoS One. 2011;6(8), e23461.
Egea V, Schober A, Weber C. Circulating miRNAs: messengers on the move in cardiovascular disease. Thromb Haemost. 2012;108(4):590–1.
Valadi H, Ekstrom K, Bossios A, Sjostrand M, Lee JJ, Lotvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9(6):654–9.
Stoorvogel W. Functional transfer of microRNA by exosomes. Blood. 2012;119(3):646–8.
Montecalvo A, Larregina AT, Shufesky WJ, Stolz DB, Sullivan ML, Karlsson JM, et al. Mechanism of transfer of functional microRNAs between mouse dendritic cells via exosomes. Blood. 2012;119(3):756–66.
Skog J, Wurdinger T, van Rijn S, Meijer DH, Gainche L, Sena-Esteves M, et al. Glioblastoma microvesicles transport RNA and proteins that promote tumour growth and provide diagnostic biomarkers. Nat Cell Biol. 2008;10(12):1470–6.
Taverna S, Amodeo V, Saieva L, Russo A, Giallombardo M, De Leo G, et al. Exosomal shuttling of miR-126 in endothelial cells modulates adhesive and migratory abilities of chronic myelogenous leukemia cells. Mol Cancer. 2014;13:169.
Janssen HL, Reesink HW, Lawitz EJ, Zeuzem S, Rodriguez-Torres M, Patel K, et al. Treatment of HCV infection by targeting microRNA. N Engl J Med. 2013;368(18):1685–94.
Zhang ZG, Chopp M. Promoting brain remodeling to aid in stroke recovery. Trends Mol Med. 2015;21(9):543–8.
Acknowledgments
Thanks to Drs. Xandra Breakefield and Balaj Leonora for expert advice on exosomes.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval
All animal experiments were approved by the MGH Institutional Animal Care and Use Committee in accordance with the NIH Guide for the Care and Use of Laboratory Animals. This article does not contain any studies with human participants performed by any of the authors.
Conflict of interest
None.
Funding
Supported in part by grants from NIH and National Natural Science Foundation of China.
Rights and permissions
About this article
Cite this article
Chen, F., Du, Y., Esposito, E. et al. Effects of Focal Cerebral Ischemia on Exosomal Versus Serum miR126. Transl. Stroke Res. 6, 478–484 (2015). https://doi.org/10.1007/s12975-015-0429-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-015-0429-3