Abstract
Rodent animal models of stroke are widely used with brain ischemia inducible by various occlusion methods. Permanent or transient occlusion of the distal portion of the middle cerebral artery (MCAO) offers a reproducible model with low mortality rates, and it is the most likely model of choice for mid- and long-term studies to assess neurorepair or long-term effects of neuroprotective drugs. Therefore, a measurable and stable neurological assessment would be required to evaluate sensorimotor and cognitive deficits at short and long terms as suggested by the Stroke Therapy Academic Industry Roundtable preclinical recommendations. We review the usefulness of different tests used to measure functional outcome after distal MCAO in mice and further sustain these data with our own multilaboratories’ experience. Results show that several tests were suitable to detect neurological deterioration at short term. Grip strength and latency to move have shown some usefulness at long term, with important differences between strains, while less clear are the data for the corner test. Important strain differences in terms of infarct volume are also reported in this study. Statistical power analysis and sample size calculation of our data confirmed the value of grip strength and latency to move tests but suggest that larger sample size would be required. In conclusion, there are no robust data supporting the use of a specific behavior test to assess long-term functional outcome after distal MCAO in mice. This is an important limitation since translational basic research should provide data to help further clinical trial evaluation. New multicenter studies with larger sample size and specific mouse strains are needed to confirm the validity of tests, such as the corner, latency to move or grip strength.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is a leading cause of death and disability worldwide. According to the World Health Organization, it remains the second most important cause of mortality accounting for 6.15 million deaths each year and representing more than 10 % of the total death rate (http://www.who.int). Yet, the only approved treatments for stroke patients are reperfusion therapies with tPA (either intravenous or intra-arterial) and clot retrieval in certain patients with acute ischemic strokes [1]. In this context, the stroke research field faces the challenge to find new therapies for stroke patients that remain untreated and for all disabled stroke survivor. In this scenario, stroke repair therapies are getting positioned as best-candidate strategies to be offered to most stroke patients.
Experimental models of stroke have been developed since the early 1070s, but there is no single universal animal model for all human forms of stroke. For that reason, different species and surgical approaches are employed to mimic different clinical stroke situations and forms [2, 3] that researchers adapt to their field of interest. At the end, they are considered an important step in proof-of-concept therapeutic studies, and preclinical data obtained from those models are indispensable to support further clinical trial evaluation: a bench-to-bedside translation is required. Within the complexity of experimental studies, two major study endpoints are investigated: infarct reduction and improvement on neurological function. In fact, the last update of the Stroke Therapy Academic Industry Roundtable (STAIR) recommendations for preclinical studies includes the measurement of stroke outcome in behavioral studies at least 2 or 3 weeks or longer after the insult to demonstrate a sustained benefit of the tested treatment [4].
Several tests have been developed to assess neurological deficits and outcome in stroke models by evaluating motor, somatosensory, or cognitive functions [5–7]. The selection of appropriate tests should be decided accurately according to the animal species, stroke model, evaluation time, and expertise of the investigator. It is important to carefully plan the experimental approach and to select the most efficient, reliable, and valid tests for the specific purpose [8, 9]; not all tests are suitable for every stroke model. We want to focus our attention to functional testing in mouse models of stroke affecting the cerebral cortex, which are induced mainly by the distal occlusion of the middle cerebral artery (MCAO). Since mortality rates are very low, these are models of choice for many researchers investigating long-term effects of neuroprotection treatments or efficacy of neurorepair strategies.
We will review published data on functional outcome assessment in mouse stroke models induced by occlusion of the distal middle cerebral artery (MCA) and provide new results obtained in different laboratories, models, strains, and evaluation times. The question is whether long-term functional assessment is a valuable endpoint to determine deterioration and functional recovery, or whether we should admit that we are not ready for this evaluation in certain models of stroke.
Methods
Focal Cerebral Ischemia
All stroke models were performed in male young adult mice by occluding the distal part of the MCA accordingly to previous reported methods. Laboratory 1 applied permanent electrocoagulation and transient compression models as described by Morancho et al. [10]. Briefly, animals were anaesthetized with isofluorane via facemask (4 % for induction, 2 % for maintenance in air, and 79 % N2/21 % O2; Abbot Laboratories, Madrid, Spain). A small craniotomy in the left temporal bone was performed to expose the MCA and the distal portion of the artery was electrocoagulated (permanent model) or compressed with a 30-G needle for 60 min (transient MCAO).
Laboratory 2 applied thromboembolic stroke as described by Orset et al. [11]. Briefly, animals were deeply anesthetized with isoflurane 5 % and maintained with 2.5 % isoflurane in a 70/30 % mixture of NO2/O2. Mice were intubated and mechanically ventilated (ventilator NEMI Scientific Inc) at 180 breaths/min. The skin between the right eye and the right ear was incised, and the temporal muscle was retracted. A small craniotomy was performed, the dura was excised, and the MCA was exposed. A pipette was introduced into the lumen of the MCA and 1 μL of purified murine alpha-thrombin (0.75 UI) was pneumatically injected to induce the formation of a clot in situ.
Laboratory 3 applied electrocoagulation as described by Lubjuhn et al. [12]. Briefly, mice were anesthetized with tribromoethanol (2.5 %, 150 μl/10 g body weight, i.p.), and the temporal muscle was removed by electrical coagulation (Modell ICC 50, Erbe, Tübingen, Germany). Then, the stem of the dMCA was exposed through a burr hole and occluded by microbipolar coagulation (ERBE ICC50, Erbe).
C57BL/6, Balb/C, Swiss, and FVB strains were used as listed in Table 1 and a control group of sham-operated animals was included in some experimental groups (see Table 1) by performing all surgical manipulations except the occlusion of the artery. STAIR criteria [13] and NINDS RIGOR guidelines [www.ninds.nih.gov/funding/transparency_in_reporting_guidance.pdf] were followed. In this regard, cerebral blood flow was monitored in all models to ensure appropriate occlusion and reperfusion (if applicable), body temperature was maintained at 36.5–37.5 °C, performance of long-term behavioral testing, inclusion and exclusion criteria for blood flow rates were established, reporting negative data or describing in detail the statistical analysis. Other recommendations for preclinical studies, such as dose–response, therapeutic window, the use of multiple species were not followed since our study did not require it.
All experiments were performed in accordance with the French, Spanish, and German legislation and the European Communities Council guidelines for the care and use of laboratory animals. Approved consent was obtained from local Animal Care Committees.
Behavioral Testing
Neurological deterioration and functional outcome were assessed by different tests. Laboratory 1 conducted the corner test and the grip strength meter as described below. Laboratory 2 conducted the beam walk, rotarod, and corner tests as described below. Finally, laboratory 3 conducted the corner and latency to move tests as described below. Time points for functional testing are described in Table 1 according to the experimental group.
Some of these animals comprise the control group of current ongoing studies, in those cases behavioral tests were performed by an investigator blinded for the control and/or sham group.
Beam Walk
The beam walk test allows to measure complex motor coordination and balance performance in rodents. The procedure was adapted from Shelton et al. [14]. The beam (0.75 m × 1 cm), elevated 40 cm above the floor, had a black box with an opening at one end and an aversive stimulus (bright lamp) at the other end. The mouse was placed on the beam near the light source and the light was turned on. Four trials (maximum value, 120 s) were performed with a 1-min resting period. The latency (in seconds) to reach the black box was measured.
Rotarod
To assess motor coordination and balance alterations after MCAO, mice were subjected to accelerating rotarod from 4 to 40 rpm over 2 min (Letica LE8500, BIOSEB®, France) as previously described [15]. Three trials (maximum value, 120 s) were performed with a 1-min resting period. The latency (in seconds) to fall was recorded.
Corner
The corner test, used to assess sensorimotor and postural asymmetries after MCAO, was based on previous work [16]. The corner consisted of two boards (30 × 20 × 1 cm3) attached at a 30° angle with a small opening between the boards to encourage entry in the corner. Ten to twelve trials were performed and left and right turns were recorded. Laterality index was calculated as previously described [10] as: LI = (turns to the ipsilateral side − turns to the contralateral side)/total number of turns. A laterality index of 0 is scored by animals presenting total symmetry.
Grip Strength Meter
The grip strength meter allows the study of neuromuscular functions in rodents by determining the maximum force displayed by an animal (Harvard Apparatus). This test measures the maximum force displayed by the mouse forelimbs. To our knowledge, this is the first study evaluating the grip strength after dMCAO in mice. Briefly, animals are suspended by the tail and approached to the grid. Once the mouse grasped the center of the grid with both forelimbs, the animal was pulled backwards in the horizontal plane. The force applied to the grid was recorded as the peak tension and measured in grams. Six measures were acquired per time point and the mean force was obtained for statistical analysis.
Latency to Move
This test was performed as previously described [12]. Mice were placed on a plate and the time (in seconds) to move one full body length (about 7 cm) was recorded.
Infarct Volume
To assess differences on infarct extension in the different mice strains (C57BL/6, Balb/C, FVB, and Swiss-derived CD-1), laboratory 1 performed the permanent distal MCAO by electrocoagulation as explained above in separate cohorts of male animals (n = 4–5/strain). Briefly, 48 h after occlusion mice were transcardially perfused with cold saline, brains were removed, sliced in 1 mm sections, and stained by the triphenyltetrazolium chloride (TTC) method as reported [10]. Measurements of the ipsilateral and contralateral hemispheres of all slices were obtained as well as the area of the infarcted tissue (in white after TTC stain). Final infarct volume was corrected by edema, and results are given in cubic millimeters as described [10].
Statistical Analysis
SPSS version 15.0 was used for statistical analysis. Significance between time points for normally distributed variables was assessed using the paired t test or repeated ANOVA followed by LSD post hoc when more than two measures were compared. Significance between time points for non-normally distributed variables was assessed using Friedman and Wilcoxon post hoc when more than two measures were compared. Differences between sham and MCAO animals were analyzed by the unpaired t test if normally distributed or Mann–Whitney U test if non-normally distributed. Values are expressed as mean ± SD. A p value of less than 0.05 was considered statistically significant. Ene 3.0 software (www.e-biometria.com/) was used to calculate statistical power of our results and sample size (setting the power at 80 % and level of significance, two sided, at 0.05).
Results
Short-Term Neurological Deterioration
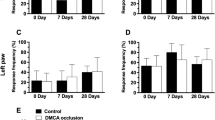
Three different methods to occlude the MCA and producing only cortical infarcts have been performed (electrocoagulation, compression, and thromboembolic) showing the value of several tests to recognize neurological deterioration early after ischemia (within the first 48 h) in Balb/c and C57BL/6 mice but not in Swiss and FVB strains, as summarized in Fig. 1a–d.
Bar graphs showing short- and long-term scores of different strains: grip strength (a), latency to move (b), beam balance (c), and corner (d). Electrocoagulation-induced permanent ischemia was performed in Balb/c, C57BL/6, and FVB strains while thromboembolic induction of cerebral ischemia was performed in Swiss mice. The day of the test after MCAO is indicated in the x-axis. Note that important differences are seen between strains and tests. Tests for repeated measures were applied for comparisons between time-points (repeated measures ANOVA followed by LSD or Friedman followed by Wilcoxon tests) whereas comparisons between sham and MCAO animals were analyzed by unpaired t test or Mann–Whitney U test. Bars represent mean ± SD; *p < 0.05
In this regard, forelimb force was altered in both Balb/c and C57BL/6 mice 24 h after electrocoagulation-induced permanent ischemia (p < 0.05, respectively) and in transient ischemia in C57BL/6 (p < 0.05). However, when comparing the ischemic and sham cohorts of C57BL/6 mice, only the compression model showed significant differences (p < 0.05) whereas differences with permanent occlusion did not reach significant difference (p > 0.05).
The corner test showed some asymmetry performance in different cohorts of Balb/c mice and C57BL/6 mice. In laboratory 1, two cohorts of Balb/c mice were subjected to permanent occlusion showing that laterality index was significantly altered 24 h compared with pre-ischemia in one cohort (p < 0.05) but not in the second one (p > 0.05). Contrary, at earlier time points (4 h), the two tested cohorts did not show differences (p > 0.05 in both cohorts). In laboratory 1, a cohort of C57BL/6 mice did not show asymmetry in the corner test at 24 h neither in the permanent nor in the transient model, while in laboratory 3 asymmetry was reached 48 h after permanent ischemia in two different cohorts (p < 0.05, respectively).
Latency to move one body length showed clear motor deficit 24 and 48 h after ischemia (p < 0.05 for both time points) as represented in Fig. 1b. Corner test was useless to show short-term neurological deterioration for FVB and Swiss cohorts as well as beam walk and rotarod for the Swiss cohort since non significant differences were found when compared with pre-ischemia scores or to sham animals (see Fig. 1c, d).
Mid- and Long-Term Neurological Outcome Assessments
Latency to move, grip strength and corner test were useful to show neurological deficits at mid- and long terms (1 or 2 weeks) in some strains (see Fig. 1a–d).
In summary, corner test performed after electrocoagulation-induced permanent ischemia in two cohorts of Balb/c showed differences in one cohort at 1 week (p < 0.05) but not at 2 weeks (p > 0.05) while no differences were observed in the other group of animals (p > 0.05). Similar data were obtained for Swiss mice after thromboembolic occlusion since asymmetry preference was detected at 1 week (p < 0.05) and a tendency at 2 weeks (p = 0.095). Contrary, FVB and C57BL/6 cohorts of permanently occluded mice by electrocoagulation did not show mid- or long-term asymmetry as seen in Fig. 1d.
Forelimb force was significantly reduced 1 and 2 weeks after permanent ischemia in Balb/c mice (p < 0.05, respectively; see Fig. 1a). Similarly, motor deficits were still present at 1 week when evaluated with the latency to move test after permanent occlusion in C57BL/6 (p < 0.05); data from longer time points or other strains are not available (Fig. 1b).
Finally, beam balance and rotarod test could not detect neurological deficits 1 week after thromboembolic occlusion in Swiss mice when compared with pre-ischemia or sham animals, as well as grip strength in FVB mice up to 3 weeks after permanent occlusion (see Fig. 1a, c).
Power Analysis and Sample Size Calculation
A posterior analysis of the statistical power of our results was performed in order to assess the value of the obtained results and to determine the minimal sample size required in future studies based on our data (see Table 2). The analysis indicates strong power for grip strength in C57BL/6 and Balb/c mice for short-term assessments and at long-term in Balb/c mice (C57BL/6 was not tested). The sample size required would be between five and seven animals as indicated in Table 2. Similar power was obtained for latency to move test in C57BL/6 mice at both short- and long-term assessments (sample size required between 4 and 15 animals). The corner test power analysis showed larger variability between strains and time points of assessment. Here, the results seem to indicate that larger sample sizes would be needed especially for long-term assessment (between 6 and >100). A detailed analysis, cohort by cohort, for corner test, grip strength, and latency to move is described in Table 2.
Strain Differences
Behavioral evaluation of Swiss and FVB mice clearly showed difficulties to demonstrate neurological deterioration at both short and long terms. As summarized in Table 3, tests performed acutely after ischemia could not show worsening when measuring force, asymmetry, motor activity, or sensory functions when compared with pre-ischemia capacities or compared with non-ischemic animals in those strains. Only Swiss mice showed a transient asymmetry in the corner test 1 week after ischemia (p < 0.05 versus pre-ischemia), though this was not sustained at later time points (see Fig. 1d). In this sense, Balb/c mice showed a similar pattern since acute (24 h, p < 0.05) and mid-term (1 week, p < 0.05) asymmetry preference were detected compared with pre-ischemia values (see Fig. 1d) but not at 2 weeks. Contrary, C57BL/6 mice showed significant asymmetry scores only in the acute phase at 2 days (p < 0.05 versus pre-ischemia) but not at 7 days (p > 0.05 versus pre-ischemia). Overall, a large variability was seen in all strains for corner test. FVB mice failed to show reduced forelimb force while Balb/C and C57BL/6 mice did show reduced force as summarized in Table 3.
Sample size calculations indicate that, due to a very low statistical power, a large number of mice would be needed for FVB (from 40 to >100 individuals) and Swiss strain (from 15 to >100 individuals) to assess neurological deterioration at any time point.
Regarding infarct volume, enormous differences were observed among strains as shown in Fig. 2. Balb/c mice presented the largest and less variable infarct volumes (54 ± 6.5) while FVB displayed the smallest volumes (22.6 ± 10.4). C57BL/6 mice and CD-1 (Swiss-derived strain) presented intermediate infarct volumes, 29.4 ± 11.3 and 36.1 ± 6.8, respectively.
Discussion
Our results show the usefulness of several tests to measure early neurological deterioration after ischemic stroke in mice affecting the cerebral cortex, but no robust data support the use of a specific test to assess mid- or long-term functional outcomes. Our results also show important differences between strains to consider when designing our research protocols. We will discuss how our results are supported by other authors and question whether long-term measurements of functional outcome should be considered as relevant endpoints in neuroprotection and neurorepair experimental studies using mouse models of cortical infarction.
Good neurological outcome and functional independence are the major indicators of recovery for stroke survivors regardless of residual signs of brain damage in neuroimage studies during the follow-up. To this end, clinicians can assess stroke severity, neurological deterioration, disabilities, or long-term functional outcome by using quite simple neurological scales, such as National Institute of Health Stroke Scale (NIHSS) and the modified Rankin Scale [17] which have become the main endpoints in human clinical trials. Possibly for that reason, stroke researchers and clinicians expect to obtain similar information, in a bedside-back-to-bench viewpoint, from experimental animal models of stroke. In this sense, many tests have been developed, from simple neurological scales to more complex tests measuring anxiety, learning and memory, balance, postural reflexes, or sensory awareness among others. The reality is that over 20 tests have been validated in animal models of stroke [5, 6, 9], but there is no consensus for using one single test for one single model and each researcher has to try with several tests in its experimental conditions as summarized in Table 4. At the same time, failed experiments (or more exactly negative results) are difficult to publish, introducing a bias of nonpublished data and somehow hiding to other researchers valuable information about what did not work for others.
The usefulness of cognitive and behavioral assessment in experimental stroke research has been a theme of debate in the last decades. In general, tests used to measure functional recovery in rats appear to be less useful in murine stroke models. For example, a quite simple neurological score that works in proximal [18–20] and distal [21, 22] occlusions of the MCA at different time points is also useful in mice for proximal occlusion models affecting the striatum [23, 24] but not for distal occlusions [25, 26], indicating important differences between rodent species and the importance of infarct location.
In the present study, we provide data obtained from different laboratories with proved experience in animal models of stroke by inducing MCA occlusion by three different models (electrocoagulation, compression and thromboembolic), including also negative results. All the tests are known to evaluate somatosensory, motor function, or a combination of both which are totally or partially affected by the resulting cortical infarctions of the performed models as published by the different laboratories [10–12].
At least three large studies have evaluated a battery of sensorimotor and cognitive tests after distal MCAO including sham and ischemic animals [12, 27, 28]. Gerlai and colleagues [27] induced transient focal cerebral ischemia (45 min) in C57BL/6 males, confirming the cortical lesions by MRI, and performed rotarod, hanging wire, horizontal surface approach, spontaneous t maze, and eye closure tests 3 weeks after MCAO or sham operation. Their results showed significant differences between all sensorimotor and sensory test but not in cognitive test (t maze). However, these authors did not study how mice scored over time comparing pre-ischemia with different time points post-ischemia. Freret and colleagues [28] used a stroke model of permanent distal MCA occlusion in Swiss males to monitor animals’ behavior several days/weeks before and after stroke or sham surgery. Their results were contundent: sensorimotor performances were not significantly altered when assessed with the corner, cylinder, pole, accelerated rotarod, chimney, or staircase tests neither mnesic performances in the passive avoidance test and in the Morris water maze could not reveal learning and memory deficits. Only the adhesive removal indicated a clear contralateral deficit (increased time to contact and to remove the tape) early after ischemia and during the study period (3 weeks) correlating with infarct volume only at 3 weeks. Significant differences were also seen when comparing ischemic versus sham mice. More recently, Lubjhun and colleagues performed functional testing in C57BL/6 males also after permanent occlusion by electrocoagulation [12] identifying the latency to move as a suitable test to assess motor deficits at short and long terms (up to 2 weeks). In the same study, corner and handedness tests showed differences at short term (day 1 or 2) with pre-ischemia scores and sham animals and both Catwalk and DigiGait systems detected shorter time of paw contact with walking surface in ischemic animals (day 1 or 2) versus sham animals.
In the present study, we have found that short-term evaluation of neurological deterioration is feasible in C57BL/6 mice and Balb/c mice by corner, grip strength meter, and latency to move tests when comparing pre- versus post-ischemia scores but showing large variability between animals. In this regard grip strength meter has been used to assess neurological deficit in rats[29] and mice [30] subjected to proximal occlusions of the MCA showing deficits after ischemia at mid- and long terms but not when compared with sham animals. To our knowledge, this is the first study evaluating the grip strength test after distal MCAO in mice. The latency to move test time was found to be elevated in previous studies 2 weeks after proximal [31] or distal [12] occlusion of the MCA in mice, but other studies have reported no changes after ischemia [32]. However, no systematic use of these two tests has been found in the literature and further studies are needed to confirm its value at long term. Regarding the asymmetry preferences detected by the corner test we have found consistent asymmetric turning preference one week after ischemia but our data also suggest that spontaneous recovery occurs at longer time points, probably by compensatory strategies, large variability between animals and lack of sensitivity of some strains. Other investigations performing similar models of ischemia have reported usefulness only during the first days after ischemia [10, 12, 33, 34] or no differences in the turning preference at any time point [29, 35, 36]. Some of these studies found similar results for the cylinder test [29, 35, 36].
Other tests, such as freezing time [37], adhesive tap removal [35], the pasta matrix reaching test [35], tongue protrusion [36], global motor activity [11], eye closure [27], wire hang [27], and elevated body swing [34] have shown short- and/or long-term sensitivities to neurological deficits in cortical lesions only in isolated studies, while others have failed even shortly after ischemia, such as the chimney [28], the passive avoidance [28], or the Morris water maze [38] (this last one showing some cognitive deficits only at long term). In our study, Swiss mice were evaluated by the beam walk and rotarod tests (latency times) showing no differences between pre- versus post-ischemia values nor between sham versus ischemic animals at any of the time points. In this sense, other authors have found similar results for the rotarod test [25, 28, 36] while others have reported slight differences in the beam balance tests (slip steps) at long term between treatment groups after MCAO, although no data are reported regarding pre-ischemia values or sham animals [34]. Our study only reports one single negative result in Swiss mice in terms of the uselessness of beam balance and rotarod tests, but it supports these other previous studies in FVB or C57BL/6 mice.
Finally, our study has been pointless to assess neurological deterioration in FVB mice by the corner or grip strength tests either at short- or long-term measurements. Similar results were obtained with this strain in another study where accelerating rotarod, tongue, corner test, and cylinder test were tested before and after ischemia induced by common carotid artery ligation and electrocoagulation of the distal MCA [36]. The authors report that no functional deficits compared with baseline performance could be found in limb-use asymmetry, corner turning test, or rotarod performance, and only acute (1 day) motor dysfunction of the tongue occurred in WT FVB mice. Contrary, mice knockout for thrombospondin-1/2 maintained minor motor deficits when compared with WT mice at 3 and 4 weeks [36]. The strain differences found in our study and described by other authors are probably the consequence of genetic variations that among others, cause differences on collateral morphometrics thus affecting collateral circulation and collateral remodeling after obstruction as demonstrated in 15 inbred mouse strains [39]. The cited study shows that these differences are major contributors to variability in infarct volume after permanent distal MCAO; unfortunately, authors do not perform behavioral studies. Other studies have also shown important differences in infarct volumes after performing the same occlusion method in different mouse strains [40, 41]. These studies show a 3-fold increase in Balb/c versus FVB or 2-fold increase versus C57BL/6 in infarct volume, with obvious different patterns for cortical infarct distribution. Similar data have been obtained in the present study by using the electrocoagulation model since Balb/c presented a 2.5-fold change on infarct volume when compared with FVB or 1.8-fold change compared with C57BL/6. This might explain the difficulties for measuring neurological deterioration in FVB mice and the strain differences described here and in the literature.
Considering all these data, we could ask ourselves what we should expect from a good behavioral test. Whether to show differences between ischemic and non-ischemic animals or to show differences between pre- versus post-ischemia values or we should only focus on improvement after post-ischemia scores? This unsolved question acquires more complexity when we introduce groups of treatment: what is truly relevant in terms of neurological status, to score better at one time point than vehicle-treated animals or to improve more over time than vehicle-treated animals? Should we forget about pre-ischemia scores since neurological improvement in humans is often defined as improvement in the baseline (post-stroke) NIHSS scores? Should be move to other designs and ask how much a given treatment can accelerate spontaneous recovery? Again, nowadays no consensus has been established for preclinical studies and we can probably answer “yes” to all these questions supported by a large number of studies. In this sense, our results show that most consistent and positive results have been found been assessing differences, between pre- and post-ischemia scores while differences between sham and ischemic animals (in those cohorts with sham-control groups) or between early post-ischemia with late post-ischemia scores, do not exist or have been weak. We believe that the distal occlusion model in mice is certainly a valid model of stroke to study mechanisms of cell death and recovery but perhaps we are not ready to ask for improvement on long- term functional outcome when we see that mice in these particular models show spontaneous recovery after a few days with minimal mortality incidence. We wonder if the currently available behavioral tests should only be applied to assess impairment of the neurological status or to determine long-term side effects of a given treatment. Importantly, STAIR recommendations, among others, include long-term behavioral testing and the development of neurological impairment of a given severity as inclusion criteria whereas RIGOR guidelines include the calculation of sample sizes/power calculation and the robustness and reproducibility of the observed results. The data presented here suggest that only some behavioral tests could accomplish these requirements if the model of choice is the distal occlusion of the MCA in mouse.
In conclusion, several tests have shown their usefulness in measuring neurological deterioration in mice acutely after cerebral ischemia induced by distal occlusion of the cerebral artery, but no robust data are currently available supporting the value of a single behavioral test to measure neurological deficits at mid- and long terms. Some tests such as the corner test, adhesive tape removal, latency to move, freezing time or grip strength meter have demonstrated signs of usefulness at long-term evaluations in sparse publications but data are still missing to confirm that these methods are sufficient to prove efficacy and safety in our preclinical studies; no systematic use of a specific test can be found in the literature. Our results support the potential value of the grip strength meter and latency to move tests; less clear are our results on the corner test.
However, some limitations arise from this study, such as a the incomplete time point profile for all tests and mouse strain responses in relation to the ischemic lesion in terms of infarct volume and topographic distribution. We propose that a multicenter study with larger sample sizes and multiple strains, perhaps including neuroimaging monitoring, is needed to validate our observations and others findings to establish a valid behavioral test for distal MCAO in mice.
References
Molina CA. Reperfusion therapies for acute ischemic stroke: current pharmacological and mechanical approaches. Stroke. 2011;42:S16–9.
Howells DW, Porritt MJ, Rewell SS, O’Collins V, Sena ES, van der Worp HB, Traystman RJ, Macleod MR. Different strokes for different folks: the rich diversity of animal models of focal cerebral ischemia. J Cereb Blood Flow Metab. 2010;30:1412–31.
Lo EH. Experimental models, neurovascular mechanisms and translational issues in stroke research. Br J Pharmacol. 2008;153:S396–405.
Fisher M, Feuerstein G, Howells DW, Hurn PD, Kent TA, Savitz SI, Lo EH. STAIR Group. Update of the stroke therapy academic industry roundtable preclinical recommendations. Stroke. 2009;40:2244–50.
DeVries AC, Nelson RJ, Traystman RJ, Hurn PD. Cognitive and behavioral assessment in experimental stroke research: will it prove useful? Neurosci Biobehav Rev. 2001;25:325–42.
Schallert T. Behavioral tests for preclinical intervention assessment. NeuroRx. 2006;3:497–504.
Zarruk JG, Garcia-Yebenes I, Romera VG, Ballesteros I, Moraga A, Cuartero MI, Hurtado O, Sobrado M, Pradillo JM, Fernandez-Lopez D, Serena J, Castillo-Melendez M, Moro MA, Lizasoain I. Neurological tests for functional outcome assessment in rodent models of ischaemic stroke. Rev Neurol. 2011;53:607–18.
García-Bonilla L, Rosell A, Torregrosa G, Salom JB, Alborch E, Gutiérrez M, Díez-Tejedor E, Martínez-Murillo R, Agulla J, Ramos-Cabrer P, Castillo J, Gasull T, Montaner J. Recommendations guide for experimental animal models in stroke research. Neurologia. 2011;26:105–10.
Brooks SP, Dunnett SB. Tests to assess motor phenotype in mice: a user’s guide. Nat Rev Neurosci. 2009;10:519–29.
Morancho A, García-Bonilla L, Barceló V, Giralt D, Campos-Martorell M, Garcia S, Montaner J, Rosell A. A new method for focal transient cerebral ischemia by distal compression of the middle cerebral artery. Neuropathol Appl Neurobiol. 2012; (in press)
Orset C, Macrez R, Young AR, Panthou D, Angles-Cano E, Maubert E, Agin V, Vivien D. Mouse model of in situ thromboembolic stroke and reperfusion. Stroke. 2007;38:2771–8.
Lubjuhn J, Gastens A, von Wilpert G, Bargiotas P, Herrmann O, Murikinati S, Rabie T, Marti HH, Amende I, Hampton TG, Schwaninger M. Functional testing in a mouse stroke model induced by occlusion of the distal middle cerebral artery. J Neurosci Methods. 2009;184:95–103.
STAIR. Recommendations for standards regarding preclinical neuroprotective and restorative drug development. Stroke. 1999;12:2752–8.
Shelton SB, Pettigrew B, Hermann AD, Zhou W, Sullivan PM, Crutcher KA, Strauss KI. A simple, efficient tool for assessment of mice after unilateral cortex injury. J Neurosci Methods. 2008;168:431–42.
Bouët V, Freret T, Toutain J, Divoux D, Boulouard M, Schumann-Bard P. Sensorimotor and cognitive deficits after transient middle cerebral artery occlusion in the mouse. Exp Neurol. 2007;203:555–67.
Zhang L, Chen J, Li Y, Zhang ZG, Chopp M. Quantitative measurement of motor and somatosensory impairments mild (30 min) and severe (2 h) transient middle cerebral artery occlusion in rats. J Neurol Sci. 2000;74:141–6.
Kasner SE. Clinical interpretation and use of stroke scales. Lancet Neurol. 2006;5:603–12.
Guluma KZ, Lapchak PA. Comparison of the post-embolization effects of tissue-plasminogen activator and simvastatin on neurological outcome in a clinically relevant rat model of acute ischemic stroke. Brain Res. 2010;1354:206–16.
Morris DC, Chopp M, Zhang L, Lu M, Zhang ZG. Thymosin beta4 improves functional neurological outcome in a rat model of embolic stroke. Neuroscience. 2010;169:674–82.
Schäbitz WR, Sommer C, Zoder W, Kiessling M, Schwaninger M, Schwab S. Intravenous brain-derived neurotrophic factor reduces infarct size and counterregulates Bax and Bcl-2 expression after temporary focal cerebral ischemia. Stroke. 2000;31:2212–7.
Gutiérrez-Fernández M, Rodríguez-Frutos B, Alvarez-Grech J, Vallejo-Cremades MT, Expósito-Alcaide M, Merino J, Roda JM, Díez-Tejedor E. Functional recovery after hematic administration of allogenic mesenchymal stem cells in acute ischemic stroke in rats. Neuroscience. 2011;175:394–405.
McGill JK, Gallagher L, Carswell HV, Irving EA, Dominiczak AF, Macrae IM. Impaired functional recovery after stroke in the stroke-prone spontaneously hypertensive rat. Stroke. 2005;36:135–41.
Hayakawa K, Pham LD, Katusic ZS, Arai K, Lo EH. Astrocytic high-mobility group box 1 promotes endothelial progenitor cell-mediated neurovascular remodeling during stroke recovery. Proc Natl Acad Sci USA. 2012;109:7505–10.
Chen J, Zacharek A, Zhang C, Jiang H, Li Y, Roberts C, Lu M, Kapke A, Chopp M. Endothelial nitric oxide synthase regulates brain-derived neurotrophic factor expression and neurogenesis after stroke in mice. J Neurosci. 2005;25:2366–75.
Guo Q, Wang G, Liu X, Namura S. Effects of gemfibrozil on outcome after permanent middle cerebral artery occlusion in mice. Brain Res. 2009;1279:121–30.
García-Yébenes I, Sobrado M, Zarruk JG, Castellanos M, Pérez de la Ossa N, Dávalos A, Serena J, Lizasoain I, Moro MA. A mouse model of hemorrhagic transformation by delayed tissue plasminogen activator administration after in situ thromboembolic stroke. Stroke. 2011;42:196–203.
Gerlai R, Thibodeaux H, Palmer JT, van Lookeren Campagne M, Van Bruggen N. Transient focal cerebral ischemia induces sensorimotor deficits in mice. Behav Brain Res. 2000;108:63–71.
Freret T, Bouet V, Leconte C, Roussel S, Chazalviel L, Divoux D, Schumann-Bard P, Boulouard M. Behavioral deficits after distal focal cerebral ischemia in mice: usefulness of adhesive removal test. Behav Neurosci. 2009;123:224–30.
Ruscher K, Erickson A, Kuric E, Inácio AR, Wieloch T. Effects of chronic Clozapine administration on apolipoprotein D levels and on functional recovery following experimental stroke. Brain Res. 2010;1321:152–63.
Ferrara A, El Bejaoui S, Seyen S, Tirelli E, Plumier JC. The usefulness of operant conditioning procedures to assess long-lasting deficits following transient focal ischemia in mice. Behav Brain Res. 2009;28(205):525–34.
Hattori K, Lee H, Hurn PD, Crain BJ, Traystman RJ, DeVries AC. Cognitive deficits after focal cerebral ischemia in mice. Stroke. 2000;31:1939–44.
Craft TK, Glasper ER, McCullough L, Zhang N, Sugo N, Otsuka T, Hurn PD, DeVries AC. Social interaction improves experimental stroke outcome. Stroke. 2005;36:2006–11.
Liesz A, Sun L, Zhou W, Schwarting S, Mracsko E, Zorn M, Bauer H, Sommer C, Veltkamp R. FTY720 reduces post-ischemic brain lymphocyte influx but does not improve outcome in permanent murine cerebral ischemia. PLoS One. 2011;6:e21312.
Wang X, Mao X, Xie L, Sun F, Greenberg DA, Jin K. Conditional depletion of neurogenesis inhibits long-term recovery after experimental stroke in mice. PLoS One. 2012;7:e38932.
Tennant KA, Jones TA. Sensorimotor behavioral effects of endothelin-1 induced small cortical infarcts in C57BL/6 mice. J Neurosci Methods. 2009;181:18–26.
Liauw J, Hoang S, Choi M, Eroglu C, Choi M, Sun GH, Percy M, Wildman-Tobriner B, Bliss T, Guzman RG, Barres BA, Steinberg GK. Thrombospondins 1 and 2 are necessary for synaptic plasticity and functional recovery after stroke. J Cereb Blood Flow Metab. 2008;28:1722–32.
Macrez R, Obiang P, Gauberti M, Roussel B, Baron A, Parcq J, Cassé F, Hommet Y, Orset C, Agin V, Bezin L, Berrocoso TG, Petersen KU, Montaner J, Maubert E, Vivien D, Ali C. Antibodies preventing the interaction of tissue-type plasminogen activator with N-methyl-d-aspartate receptors reduce stroke damages and extend the therapeutic window of thrombolysis. Stroke. 2011;42:2315–22.
Guégan C, Braudeau J, Couriaud C, Dietz GP, Lacombe P, Bähr M, Nosten-Bertrand M, Onténiente B. PTD-XIAP protects against cerebral ischemia by anti-apoptotic and transcriptional regulatory mechanisms. Neurobiol Dis. 2006;22:177–86.
Zhang H, Prabhakar P, Sealock R, Faber JE. Wide genetic variation in the native pial collateral circulation is a major determinant of variation in severity of stroke. J Cereb Blood Flow Metab. 2010;30:923–34.
Majid A, He YY, Gidday JM, Kaplan SS, Gonzales ER, Park TS, Fenstermacher JD, Wei L, Choi DW, Hsu CY. Differences in vulnerability to permanent focal cerebral ischemia among 3 common mouse strains. Stroke. 2000;31:2707–14.
Koistinaho M, Malm TM, Kettunen MI, Goldsteins G, Starckx S, Kauppinen RA, Opdenakker G, Koistinaho J. Minocycline protects against permanent cerebral ischemia in wild type but not in matrix metalloprotease-9-deficient mice. J Cereb Blood Flow Metab. 2005;25:460–7.
Acknowledgments
A.R. is supported by the Miguel Servet program (CP09/00265) from the Spanish Ministry of Health (Instituto de Salud Carlos III). V.A., C.A. and D.V. works are supported by INSERM, French Ministry of Research and Technology, and Regional Council of Lower Normandy. The research leading to these results has received funding from the European Union’s Seventh Framework Program (FP7/2007-2013) under grant agreements No. 201024 and 202213 (European Stroke Network), the Spanish Ministry of Health (Instituto de Salud Carlos III, grant agreement No. PI10/00694, and RETICS program, RENEVAS network), and the ERANET-NEURON program from the Ministerio de Economía y Competitividad (grant agreement No. 2011-1352).
Conflict of Interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosell, A., Agin, V., Rahman, M. et al. Distal Occlusion of the Middle Cerebral Artery in Mice: Are We Ready to Assess Long-Term Functional Outcome?. Transl. Stroke Res. 4, 297–307 (2013). https://doi.org/10.1007/s12975-012-0234-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-012-0234-1