Abstract
Female sex steroids, particularly estrogens, contribute to the sexually dimorphic response observed in cerebral ischemic outcome, with females being relatively protected compared to males. Using a mouse model of cardiac arrest and cardiopulmonary resuscitation, we previously demonstrated that estrogen neuroprotection is mediated in part by the estrogen receptor β, with no involvement of estrogen receptor α. In this study, we examined the neuroprotective effect of the novel estrogen receptor, G protein-coupled estrogen receptor 1 (GPER1/GPR30). Male mice administered with the GPR30 agonist G1 exhibited significantly reduced neuronal injury in the hippocampal CA1 region and striatum. The magnitude of neuroprotection observed in G1-treated mice was indistinguishable from estrogen-treated mice, implicating GPR30 in estrogen neuroprotection. Real-time quantitative RT-PCR indicates that G1 treatment increases expression of the neuroprotective ion channel, small-conductance calcium-activated potassium channel 2. We conclude that GPR30 agonists show promise in reducing brain injury following global cerebral ischemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebrovascular diseases resulting in cerebral ischemia, including stroke and cardiac arrest, are sexually dimorphic, with women experiencing relative protection compared to men [1]. The reduced incidence and improved outcome in women has been attributed to neuroprotection provided by the endogenous female sex steroids, in particular estrogen [2]. Consistent with this hypothesis, incidence of brain attack significantly increases following menopause in women and the sex difference is minimized [1, 3]. Similarly, female animals suffer smaller central nervous system (CNS) damage following experimental cerebral ischemia compared to age-matched male animals [4, 5]. Further, there is extensive evidence that estrogen is neuroprotective in experimental models using both male and female animals [2]. However, the clinical utility of estrogen therapy has become highly controversial due to several recent large clinical trials, such as Women’s Health Initiative, Heart and Estrogen/Progestin Replacement Study, and Women Estrogen Stroke Trial. These studies showed that hormone replacement therapy has negative effects on outcomes and incidence of cerebrovascular disease in postmenopausal women [6–8]. An alternative to estrogen treatment of postmenopausal women or men would be selective estrogen receptor modulators (SERMS), which exhibit neuroprotective activity without other pleiotropic effects of natural estrogens. Several synthetic and natural SERMS have been demonstrated to have neuroprotective effects in experimental models, including tamoxifen, genistein, and the estrogenic diphenylacrylamide, STX [9]. These SERMS appear to protect independent of estrogen receptors α and β [10].
G protein-coupled estrogen receptor 1 (GPER1/GPR30) is a recently identified G protein-coupled receptor that binds estrogen with high affinity and has been characterized as a putative membrane estrogen receptor. Activation of GPR30 can result in both rapid nongenomic signaling events and transcriptional regulation [11]. There is recent evidence that the neuroprotective effects of exogenously administered estrogen are mediated at least in part by GPR30 activation. However, it remains unclear whether activation of GPR30 is a viable alternative approach to neuroprotection following cerebral ischemia. G1, a recently identified selective agonist of GPR30 [12], protects against oxidative toxicity in vitro and in a mouse model of stoke [13, 14]. Estrogen (E2) and G1 have been demonstrated to have rapid effects of membrane excitability via interaction with membrane ion channels [15–17], likely contributing to their neuroprotective effects. We recently demonstrated that small-conductance calcium-activated potassium channel 2 (SK2) activation protects neurons from ischemic injury [18] and therefore have tested the hypothesis that GPR30 activation is neuroprotective via increased SK2 expression. Our results demonstrate for the first time that the GPR30 agonist G1 increases expression of SK2 channels and enhances neuronal survival following cardiac arrest and cardiopulmonary resuscitation (CA/CPR)-induced cerebral ischemia.
Methods
Experimental Animals
All experimental protocols were approved by the Institutional Animal Care and Use Committee and conformed to the National Institutes of Health guidelines for the care and use of animals in research. To assess the effect of prolonged, controlled levels of hormones, E2 (12.6 μg) or G1 (1.8 mg), were administered via subcutaneous pellets (21-day continuous release pellets from Innovative Research of America, Toledo, OH) 1 week prior to arrest. We chose these doses based upon previous studies in our laboratory [19]. All cardiac arrest experiments utilizing vehicle, E2, or G1 were performed in a blinded randomized manner using male C57Bl/6 mice weighing 22–27 g, aged 6–9 weeks.
Cardiac Arrest
The experimental procedures were performed as previously described [20, 21], with minor modifications. Briefly, mice were anesthetized with isoflurane (3 %) via face mask. Temperature probes were placed into the left temporalis muscle and the rectum. Rectal temperature was controlled at 37 °C during surgery. For drug administration, the right jugular vein was cannulated with a PE-10 catheter. Electrocardiogram was monitored throughout the experimental procedures. Mice were endotracheally intubated with a 22 G intravenous catheter and mechanically ventilated (Minivent, Hugo Sachs Elektronik, March-Hugstetten, Germany). After a 10-min postsurgical stabilization period, pericranial temperature was raised to 38.5 °C using a circulating-water coil, which was placed around the head of the mice. CA was induced by intravenous injection of 50 μL cold 0.5 mol/L KCl and was confirmed by appearance of asystole on the electrocardiography monitor and no spontaneous breathing. Anesthesia was stopped and the endotracheal tube was disconnected from the ventilator. During CA, pericranial temperature was maintained at 38.5 ± 0.2 °C and body temperature was allowed to drop to 28 °C during CA. CPR was initiated 8 min after induction of CA by slow injection of 0.5 mL of epinephrine (8 μg), chest compressions (approximately 300/min), and ventilation with 100 % oxygen. As soon as return of spontaneous circulation (ROSC) was achieved, defined as electrocardiographic activity with visible cardiac contractions and rapid decreasing of pericranial temperature, chest compression was stopped. If ROSC could not be achieved within 2.5 min of CPR, resuscitation was stopped and the animal was excluded from the study. Body temperature was restored with a warming lamp during the recovery period. Twenty-five minutes after ROSC, temperature probes were removed, skin incisions were closed, and animals were weaned from the ventilator. Animals were extubated after confirmation of spontaneous ventilation/breathing, and mice were returned to their housing cage.
Health Assessment Score
Animals were assigned a score (0 being no deficit and 3 or 4 indicated impaired) for several parameters of overall health. These included consciousness, interaction, eye appearance, breathing, food/water intake, overall activity, and latency to move out of a 12-cm diameter field. Therefore, the total health assessment score is the sum of each behavior, with a range of 0–24 points. Assessments were performed on days 1, 2, and 3, and averaged sums for each day are reported.
Histological Analysis
Three days after CA/CPR, mice were deeply anesthetized with 3 % isoflurane and transcardially perfused and fixed with 10 % formalin as previously described [20, 22]. Brains were removed and embedded in paraffin, and 6-μm coronal sections were serially cut. The CA1 region of the hippocampus was analyzed, three levels (100 μm apart) beginning 1.5 mm caudal of bregma. Sections were stained with hematoxylin and eosin (H&E) for analysis of damaged neurons, determined by the presence of pink eosinophilic cytoplasm and dark pyknotic nuclei. All viable and nonviable neurons were counted for each microscopic field, and the percentage of nonviable neurons was calculated for the entire CA1 and striatum region (average of three levels/region). In order to analyze neuronal damage in the striatum, sections were stained with the neuronal-specific marker anti-NeuN antibody in addition to H&E [22]. The investigator was blinded to treatment before analyzing neuronal damage.
Quantitative Reverse Transcriptase PCR
For quantitative PCR measurement of small-conductance calcium-activated potassium (SK2 and SK3) channel transcripts, hippocampi were harvested 7 days after implantation of G1 (or vehicle) pellets. Total RNA was isolated using the RNAqueous-4 PCR kit (Ambion, Austin, TX, USA) as per manufacturer’s instructions. Briefly, approximately, 1–3 mg of tissue was lysed in lysis buffer and total RNA was isolated and eluted from a column with 50 μL RNase-free elution buffer and further treated with Turbo DNase (Ambion, Austin, TX, USA). First-strand cDNA was reverse transcribed from 500 ng total RNA with High Capacity cDNA archive Kit (Applied Biosystems, Foster City, CA, USA). Real-time PCR reactions using SYBR green PCR kit were performed on ABI Prism 7000 sequence detection system in triplicate using 50 ng cDNA. Primers used to detect SK2 and SK3 were synthesized by Invitrogen. The housekeeping gene 18S was also assayed for each sample using 5 ng of cDNA. Cycle parameters used were 50 °C for 2 min, 95 °C for 10 min followed by 40 cycles of 95 °C for 15 s and 60 °C for 1 min. Expression levels were calculated as the ratio of the target gene to 18S.
Preparation of Hippocampal Slices and Electrophysiology
Mice (6–9 weeks of age) were sedated with isoflurane (2 %) and then perfused through the left ventricle with ice-cold artificial cerebrospinal fluid solution (in millimolar) 125 NaCl, 2.5 KCl, 2 CaCl2, 1 MgCl2, 1.25 NaH2PO4, 25 NaHCO3, and 10 glucose saturated with 95 % O2/5 % CO2 gas to obtain pH 7.35. After decapitation, the hippocampus was removed and transverse slices 300-μm thick were cut with a vibratome (Leica VT 1000S, Nussloch, Germany). CA1 neurons were visualized with a microscope (Leica DMLFS). Recording pipettes were fabricated from standard-wall borosilicate glass with a resistance of 2–4 MΩ. Pipettes were filled with intracellular solution containing (in millimolar): 135 K-gluconate, 8 NaCl, 1 MgCl2, 10 HEPES, 4 Mg-ATP, 0.3 Na2-GTP, and 0.05 EGTA, pH 7.3. Whole-cell voltage-clamp currents were recorded with a MultiClamp 700A amplifier (Axon Instruments, Foster City, CA) and acquired using pCLAMP10 (Axon Instruments). To record apamin-sensitive tail currents, CA1 neurons were held at −60 mV and depolarized to 20 mV for 100 ms followed by a return to −55 mV. Access resistance was stable at <25 MΩ and was 80 % compensated. Current traces in the presence of 100 nM apamin were subtracted from control traces and fitted with a single exponential to determine decay kinetics, and current amplitude was analyzed from subtracted traces of each cell.
Statistical Analysis
All data are presented as mean ± SEM. Neuroscores and body weight were compared for treatment group and time point using two-way analysis of variance (ANOVA). Histological damage in the hippocampus was compared using one-way ANOVA followed by Newman–Keuls multiple comparison test to determine the source of variance. Histological data from striatum did not pass Shapiro–Wilk normality tests and thus Kruskal–Wallis test was used followed by Dunn’s multiple comparison test. Student’s t test was used to compare SK mRNA expression and apamin-sensitive current amplitudes. P values less than 0.05 are considered significant.
Results
Male C57Bl/6 mice were subjected to 8-min CA/CPR and neuronal injury in the striatum, and hippocampal CA1 brain structures were analyzed. Immediate asystolic cardiac arrest was observed in all mice following injection of KCl. All mice were resuscitated successfully within the CPR time window of 2.5 min. CPR duration, epinephrine dose, and body weight were not different between groups (Table 1). A health assessment score was measured each day for the 3 days of survival, being greatest (poorest health) on the first day and slowly improving. Mice subjected to E2 treatment showed improved recovery compared to vehicle and G1 (Fig. 1a), reaching significance on day 3 after CA/CPR (vehicle versus E2, P < 0.05). Body weight decreased by 10–24 % during the 3-day observation period and did not differ between treatment groups (Fig. 1b).
Effect of G1 and estrogen on general health outcome. a Quantification of general health score 1–3 days after recovery from CA/CPR. Health assessment is a 24-point scale with 0 corresponding to no impairment. Intact male mice were implanted with E2 or G1 7 days prior to CA/CPR. b Quantification of body weight 1–3 days after recovery from CA/CPR. Intact male mice were implanted with E2 or G1 7 days prior to CA/CPR. Data are presented as mean ± SEM. *P < 0.05, compared to vehicle
Histopathology
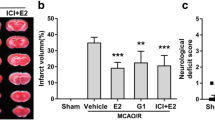
H&E staining was used to assess neuronal injury. Male mice treated with 17β-estradiol (12.6 μg) pellets 7 days prior to CA/CPR had significantly less neuronal damage in CA1 (Fig. 2) and striatum (Fig. 3) compared to vehicle-treated mice, consistent with our previously published results [25]. Hippocampal CA1 neuronal cell death decreased from 56.8 ± 9.7 % (n = 18) in vehicle-treated male mice to 24.7 ± 4.6 % (n = 9, P < 0.05) in E2-treated mice. Similarly, in striatum, E2-treated mice had reduced neuronal damage, 93.7 ± 9.7 % (n = 18) versus vehicle 77.1 ± 7.9 % (n = 9, P < 0.05). We tested the ability of the selective GPR30 agonist G1 to protect neurons against CA/CPR-induced damage. Using the same experimental protocol, we observed that G1 (1.8 mg) provides significant neuroprotection to CA1 neurons (Fig. 2) and striatal neurons (Fig. 3). Hippocampal CA1 neuronal cell death decreased from 56.8 ± 9.7 % (n = 18) in vehicle-treated male mice to 27.4 ± 5.7 % (n = 18, P < 0.05) in G1-treated mice. Similarly, in striatum, G1-treated mice had reduced neuronal damage, 93.7 ± 9.7 % (n = 18) in vehicle versus 81.9 ± 5.8 % (n = 9, P < 0.05).
G1 and E2 decrease hippocampal CA1 neuronal injury following CA/CPR. a Representative photomicrographs of hippocampal CA1 neurons from vehicle-treated (top), G1-treated (middle), and E2-treated (bottom) mice 3 days after CA/CPR. Intact male mice were implanted with E2 or G1 7 days prior to CA/CPR. Damaged neurons identified by presence of pink eosinophilic cytoplasm and dark pyknotic nucleus. b Quantification of ischemic neurons in the CA1 region of hippocampus 3 days after CA/CPR. Data are presented as mean ± SEM. *P < 0.05, compared to vehicle
G1 and E2 decrease neuronal injury in striatum following CA/CPR. a Representative photomicrographs of hippocampal CA1 neurons from vehicle-treated (top), G1-treated (middle), and E2-treated (bottom) mice 3 days after CA/CPR. Intact male mice were implanted with E2 or G1 7 days prior to CA/CPR. b Quantification of ischemic neurons in the striatum 3 days after CA/CPR. Data are presented as mean ± SEM. *P < 0.05, compared to vehicle
SK2 expression
To determine the effect of G1 treatment on the expression of small-conductance calcium-activated potassium channels (SK2 and SK3), quantitative real-time RT-PCR was performed from hippocampus and striatum from mice treated with vehicle or G1 pellets for 7 days. Male mice treated with G1 pellets for 7 days had significantly increased expression of SK2 channels in hippocampus and striatum (Fig. 4a) relative to mice treated with vehicle pellet for 7 days, increasing by 260 ± 50 % (n = 3, P < 0.05) in hippocampus and by 200 ± 23 % (n = 3, P < 0.05) in striatum. In contrast, G1 had no effect on the expression of SK3 channels in either hippocampus or striatum (Fig. 4b). To confirm G1-induced increase in SK2 expression, whole-cell voltage-clamp recordings were performed in hippocampal slices from mice treated with G1 pellets or placebo pellets. We have previously demonstrated that SK2 channels underlie the apamin-sensitive component of the tail current in CA1 neurons (Fig. 4c) [23]. Figure 4d demonstrates that mice implanted with G1 for 7 days exhibited significantly larger apamin-sensitive tail currents recorded 100 ms after repolarization (244.5 ± 53.5, n = 8) relative to placebo-implanted controls (73.3 ± 8.3, n = 4, P < 0.05). G1 treatment did not alter the decay kinetics of the apamin-sensitive SK2 currents (G1, 326.2 ± 37 ms; placebo, 303 ± 50.1 ms).
G1 increases expression of small-conductance calcium-activated potassium channel, SK2. a Quantification of SK2 mRNA in the hippocampus and striatum of vehicle- and G1-treated male mice. b Quantification of SK3 mRNA in the hippocampus and striatum of vehicle- and G1-treated male mice. Relative SK2 and SK3 mRNA was assessed using quantitative real-time RT-PCR from each brain region normalized to 18S RNA. Hippocampal and striatal RNA was collected 7 days after implantation of male mice with vehicle or G1. c Representative whole-cell recording from placebo-treated WT mouse of the apamin-sensitive current. d Quantification of apamin-sensitive current amplitude in CA1 neurons recorded from G1- and placebo-treated control mice
Discussion
The results of this study indicate that activation of GPR30 using chronic administration of G1 protects hippocampal and striatal neurons from ischemic damage from CA/CPR. The level of neuroprotection is similar to that observed with administration of the natural estrogen E2. These findings are of clinical significance as GPR30 activation offers a novel alternative to hormone replacement for the treatment of cerebral ischemia. An increase in SK2 expression was also observed with G1 administration and may contribute to protection in neurons.
Natural estrogens (E2) have been shown to be neuroprotective in the hippocampus and striatum when administered chronically prior to arrest or as an acute dose after resuscitation [24, 25]. A variety of mechanisms have been implicated in E2-mediated neuroprotection. Our previous study demonstrated that the ERβ agonist diarylpropionitrile (DPN) partially mimicked the effect of E2, providing significant protection following CA/CPR. In contrast, the ERα agonist propyl pyrazole triol provided no neuroprotection [26]. The magnitude of DPN effects appeared smaller than E2, leading us to hypothesize that alternative ER signaling may contribute to E2 neuroprotection. In addition, we recently demonstrated that the GPR30 agonist G1 reduces infarct volume in the cortex and striatum following experimental stroke [19]. Our present data indicate that chronic pretreatment with G1 is also protective in cardiac arrest-induced global ischemia. Our data are consistent with a recent report, demonstrating that acute administration of G1 directly into the brain immediately following reperfusion in a vessel occlusion model of global ischemia provided protection in CA1 neurons [27]. The mechanism for G1-mediated neuroprotection remains to be elucidated. G1 couples to pertussis-toxin-sensitive G proteins and activates multiple signaling pathways including Src, MAPK,, and ERK. Transcriptional regulation through activation of GPR30 has also been reported [28]. There is recent evidence that GPR30 signaling is mediated in part through an interaction with ERα [11, 28]. Interestingly, G1 and E2 protect to similar extent in our study, implying interacting mechanisms. However, this is purely circumstantial and further studies are needed to explore the interplay between ERs and GPR30 in estrogen neuroprotection.
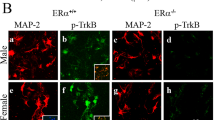
Interestingly, the study by Lebesgue and coworkers reported an increase in hippocampal CA1 excitability in response to acute G1 administration [27]. However, it is likely that the neuroprotective mechanisms engaged in our study are different, due to the different timing of administration. Our prolonged administration is likely to engage transcriptional mechanisms as well as acute signaling events. Indeed, our quantitative real-time PCR data and patch-clamp recordings indicate enhanced SK2 channel expression following 1 week of G1 administration. Such an increase is expected to dampen, rather than enhance excitability [18, 29]. We recently demonstrated that increased expression or activity of SK2 decreases hippocampal CA1 neuronal injury following CA/CPR [18]. Thus, increased SK2 expression may contribute to G1 protection by dampening ischemia-induced hyperexcitability and minimizing excitotoxicity. We performed PCR on the closely related ion channel SK3 in order to demonstrate specificity. Our observation that G1 increases SK2 expression without having an effect on SK3 enhances our confidence that GPR30 regulation of SK2 is a specific mechanism of neuroprotection. In addition, we previously demonstrated that estrogen interaction with ERα regulates SK3 expression. Therefore, our current data further indicate a separate signaling pathway for G1 interaction with SK2, having no effect on SK3.
Interestingly, in our current study, we observed improved sensorimotor health in E2-treated mice, while G1 had no effect on these outcomes. We attribute this to estrogen’s pleiotropic effects, which improve the overall health of the animal, having large effects that are important to ischemic outcome of several organs. This is particularly relevant in our mouse cardiac arrest model, which mimics the clinical condition and exposes the entire organism to hypoxia/ischemia. Indeed, we have demonstrated that estrogen minimizes renal injury following CA/CPR, likely contributing to the overall benefit observed in estrogen-treated mice in the current study [14]. It remains unclear whether G1 protects kidney. Nonetheless, we interpret the improved health of the animal observed following E2 treatment to be a result of E2 protection of peripheral organ damage following CA/CPR, resulting in an overall healthy animal. Therefore, our data indicate that further study of the effects of GPR30 activation on non-CNS organs after cardiac arrest is needed.
Conclusion
Chronic treatment of male mice with the GPR30 agonist G1 decreases CA/CPR-induced neuronal injury to a similar extent as estrogen treatment. Our data further implicate transcriptional regulation of specific ion channels responsible for dampening hyperexcitability following ischemia. Therefore, novel nonfeminizing ligands of GPR30 represent a new approach to neuroprotection following global cerebral ischemia.
References
Roger VL, et al. Heart disease and stroke statistics—2012 update: A report from the American Heart Association. Circulation. 2012;125(1):e2–220.
McCullough LD, Hurn PD. Estrogen and ischemic neuroprotection: An integrated view. Trends Endocrinol Metab. 2003;14(5):228–35.
Reeves MJ, et al. Sex differences in stroke: Epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7(10):915–26.
Appelros P, Stegmayr B, Terent A. A review on sex differences in stroke treatment and outcome. Acta Neurol Scand. 2010;121:359–69.
Alkayed NJ, et al. Gender-linked brain injury in experimental stroke. Stroke. 1998;29(1):159–65.
Renoux C, Suissa S. Hormone therapy administration in postmenopausal women and risk of stroke. Womens Health (Lond Engl). 2011;7(3):355–61.
Anderson GL, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: The Women’s Health Initiative randomized controlled trial. JAMA. 2004;291(14):1701–12.
Billeci AM, et al. Hormone replacement therapy and stroke. Curr Vasc Pharmacol. 2008;6(2):112–23.
Hoffman GE, et al. Ovarian steroid modulation of seizure severity and hippocampal cell death after kainic acid treatment. Exp Neurol. 2003;182(1):124–34.
Abdelhamid R, et al. Benzothiophene selective estrogen receptor modulators provide neuroprotection by a novel GPR30-dependent mechanism. ACS Chem Neurosci. 2011;2(5):256–68.
Prossnitz ER, Barton M. The G-protein-coupled estrogen receptor GPER in health and disease. Nat Rev Endocrinol. 2011;7(12):715–26.
Bologa CG, et al. Virtual and biomolecular screening converge on a selective agonist for GPR30. Nat Chem Biol. 2006;2(4):207–12.
Liu SB, et al. Neuroprotective effects of oestrogen against oxidative toxicity through activation of G-protein-coupled receptor 30 receptor. Clin Exp Pharmacol Physiol. 2011;38(9):577–85.
Hutchens MP, et al. Estrogen Is renoprotective via a nonreceptor-dependent mechanism after cardiac arrest in vivo. Anesthesiology. 2010.
Wu WW, Adelman JP, Maylie J. Ovarian hormone deficiency reduces intrinsic excitability and abolishes acute estrogen sensitivity in hippocampal CA1 pyramidal neurons. J Neurosci. 2011;31(7):2638–48.
Zhang C, Kelly MJ, Ronnekleiv OK. 17Beta-estradiol rapidly increases K(ATP) activity in GnRH via a protein kinase signaling pathway. Endocrinology. 2010;151(9):4477–84.
Zadran S, et al. 17-Beta-estradiol increases neuronal excitability through MAP kinase-induced calpain activation. Proc Natl Acad Sci U S A. 2009;106(51):21936–41.
Allen D, et al. SK2 channels are neuroprotective for ischemia-induced neuronal cell death. Journal of Cerebral Blood Flow & Metabolism. 2011.
Zhang B, et al. Estradiol and G1 reduce infarct size and improve immunosuppression after experimental stroke. J Immunol. 2010;184(8):4087–94.
Kofler J, et al. Histopathological and behavioral characterization of a novel model of cardiac arrest and cardiopulmonary resuscitation in mice. J Neurosci Methods. 2004;136(1):33–44.
Kelley MH, et al. Ischemic insult to cerebellar Purkinje cells causes diminished GABAA receptor function and allopregnanolone neuroprotection is associated with GABAA receptor stabilization. J Neurochem. 2008;107(3):668–78.
Nakano T, et al. Testosterone exacerbates neuronal damage following cardiac arrest and cardiopulmonary resuscitation in mouse. Brain Res. 2010;1357:124–30.
Bond CT, et al. Small conductance Ca2+-activated K+ channel knock-out mice reveal the identity of calcium-dependent afterhyperpolarization currents. J Neurosci. 2004;24(23):5301–6.
Miller NR, et al. Estrogen can act via estrogen receptor alpha and beta to protect hippocampal neurons against global ischemia-induced cell death. Endocrinology. 2005;146(7):3070–9.
Noppens RR, et al. Dose-dependent neuroprotection by 17beta-estradiol after cardiac arrest and cardiopulmonary resuscitation. Crit Care Med. 2005;33(7):1595–602.
Noppens RR, et al. Estradiol after cardiac arrest and cardiopulmonary resuscitation is neuroprotective and mediated through estrogen receptor-beta. J Cereb Blood Flow Metab. 2009;29(2):277–86.
Lebesgue D, et al. Acute administration of non-classical estrogen receptor agonists attenuates ischemia-induced hippocampal neuron loss in middle-aged female rats. PLoS One. 2010;5(1):e8642.
Notas G, et al. Interplay of estrogen receptors and GPR30 for the regulation of early membrane initiated transcriptional effects: A pharmacological approach. Steroids. 2011.
Ngo-Anh TJ, et al. SK channels and NMDA receptors form a Ca2+-mediated feedback loop in dendritic spines. Nat Neurosci. 2005;8(5):642–9.
Acknowledgments
This work was supported by NIH R01NS058792, RO1NS046072, and RO1NR03521. This work was also supported by a Walter S. and Lucienne Driskill Foundation grant.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kosaka, Y., Quillinan, N., Bond, C.T. et al. GPER1/GPR30 Activation Improves Neuronal Survival Following Global Cerebral Ischemia Induced by Cardiac Arrest in Mice. Transl. Stroke Res. 3, 500–507 (2012). https://doi.org/10.1007/s12975-012-0211-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-012-0211-8