Abstract
Our recent study has demonstrated that hemoglobin (Hb) is present in cerebral neurons, and neuronal Hb is inducible after cerebral ischemia. In the present study, we examined the effects of intracerebral hemorrhage (ICH) on the messenger RNA (mRNA) levels of the α-globin (HbA) and the β-globin (HbB) components of Hb and Hb protein in the brain in vivo and in vitro. In vivo, male Sprague–Dawley rats received either a needle insertion (sham) or an infusion of autologous whole blood into the basal ganglia and were killed at different time points. In vitro, cultured rat brain cells were used for HbA, HbB, and Hb determination. Cultured neurons were exposed to 50 or 100 µM hemin for 24 h. Some neurons also were treated with deferoxamine, an iron chelator, or vehicle. Levels of HbA and HbB, Hb, and hemopexin, a transporter of heme, were measured. We found that HbA, HbB, and Hb are primarily expressed in neurons, with much lower expression in astrocytes and microglia. HbA, HbB, and Hb expression in the perihematomal zone was increased after ICH and Hb was localized in neurons and glia. Hemin increased HbA, HbB, and hemopexin mRNA levels in cultured neurons. Deferoxamine reduced hemin-induced neuronal Hb expression. ICH increased HbA and HbB expression in the brain, which may potentially serve to buffer the heme released during clot resolution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemoglobins are heme proteins present in all groups of organisms, even those without a bloodstream. They carry out different functions, including transport of oxygen between tissues, intracellular oxygen transport, and catalysis of redox reactions [1]. Mammalian hemoglobin (Hb) is a heterotetramer of two α-globin (HbA) and two β-globin (HbB) polypeptides, with a heme tightly bound to a pocket in each globin monomer [2]. Mammalian Hb has been traditionally thought to be exclusively present in erythrocytes circulating in blood. Recent studies have demonstrated that Hb is expressed in cerebral neurons, and neuronal Hb can be induced by cerebral ischemia and ischemic preconditioning [3–5].
ICH is a stroke subtype with high morbidity and mortality. After ICH, Hb is released from erythrocytes causing brain damage [6, 7]. Exogenous Hb can cause neuronal injury when injected into the brain [8, 9] or added to cultured cerebral cortical neurons [10, 11]. The effects of ICH on endogenous Hb expression (HbA or HbB) are unknown to date.
Heme is a structural component of Hb, which can be derived from exogenous Hb after ICH and transported into the cytoplasm of cells by binding to its transport protein hemopexin or haptoglobin [12]. Heme can be degraded into iron, carbon monoxide, and biliverdin by heme oxygenases. Hemin, an oxidized form of heme, has been shown to participate in the regulation of gene transcription and translation of Hb globin molecules and assembly of Hb [13, 14]. In the present study, we examined the change of endogenous Hb expression in the brain after ICH and the effects of hemin and iron on neuronal Hb.
Materials and Methods
Animal Preparation and Intracerebral Infusion
The University of Michigan Committee on the Use and Care of animals approved the protocols for these experiments. Adult male Sprague–Dawley rats (275–325 g; Charles River Laboratories, Portage, MI, USA) were used for this study. Rats were anesthetized with pentobarbital (40–50 mg/kg, i.p.). A polyethylene catheter (PE-50) was then inserted into the right femoral artery to monitor arterial blood pressure and blood gases and to obtain blood for intracerebral blood injection. Body temperature was maintained at 37.5ºC using a feedback-controlled heating pad. The animals were positioned in a stereotactic frame (Kopf Instruments, Tujunga, CA, USA), and a cranial burr hole (1 mm) was drilled. Autologous blood was infused into the right caudate nucleus through a 26-gauge needle at a rate of 10 μL/min using a microinfusion pump (Harvard Apparatus Inc., South Natick, MA, USA). The coordinates were 0.2 mm anterior and 3.5 mm lateral to the bregma and a depth of 5.5 mm. After intracerebral infusion, the needle was removed and the skin incision closed with suture.
Experimental Animal Groups
Rats received an intracerebral infusion of 100 μL autologous whole blood into the right basal ganglia. Sham rats had a needle insertion. In the first set, rats were killed at 1, 4, 24, or 72 h later (n = 5, each time point) and brains were sampled by real-time polymerase chain reaction (PCR). In the second set, rats were killed at 1, 3, 14, or 28 days later, and brains were used for immunohistochemistry (n = 3 each time point).
Cell Culture
Primary neuronal cultures were obtained from embryonic day-17 Sprague–Dawley rats (Charles River Laboratories, Portage, MI, USA). Cultures were prepared according to a previously described procedure with some modifications [15]. Briefly, cerebral cortex was dissected, stripped of meninges, and dissociated by a combination of 0.5% trypsin digestion and mechanical trituration. The dissociated cell suspensions were seeded onto poly-l-lysine precoated six-well plates in a density of 6 × 100,000/cm2. The cells were grown in neurobasal medium with 2% B27, 0.5 mM glutamine, and 1% antibiotic–antimycotic and maintained in a humidified incubator at 37ºC with 5% CO2. Half of the culture media was changed every 3–4 days. The neurons were used for experiments after 7 days.
Primary cultures of astrocytes and microglia were prepared from the brains of 1–3-day-old Sprague–Dawley rat pups [16] with some modifications. Cerebral cortex was isolated, meninges were removed, and the tissue was dissociated by trypsinization and plated on 75 mm2 flasks in glial medium (Dulbecco’s modified Eagle medium with 10% fetal calf serum, 0.5 mM glutamine and 2% antibiotic–antimycotic). The cells were kept at 37ºC with 5% CO2, and growth medium was changed every other day. Seven to 10 days after plating, the flasks were shaken at 200 rpm on a gyratory shaker for 1 h at 4ºC. After shaking, the flask-adherent cells were predominantly astrocytes, whereas the supernatant was composed of microglia and oligodendrocytes. The supernatant was plated onto 25-mm2 flasks and returned to the incubator. Thirty minutes later, the medium was replaced with microglia culture medium (Dulbecco’s modified Eagle medium with 10% fetal calf serum, 0.5 mM glutamine, and 2% antibiotic–antimycotic and 10 ng/mL macrophage colony-stimulating factor). The culture medium was changed every other day.
Treatment of the Cells
The in vitro studies were divided into three parts. In the first, primary cultured neurons, astrocytes and microglia were collected for real-time PCR and Western blot analysis. In the second part, neurons were treated with either vehicle or hemin (50 or 100 µM; Sigma, St. Louis, MO, USA). Cells were collected 24 h later for real-time PCR. In the third part, neurons were treated with hemin (50 µM) with or without deferoxamine (50 µM). Cells were analyzed by real-time PCR 24 h later.
Real-Time Quantitative Polymerase Chain Reaction
In the in vivo studies, rats were anesthetized and decapitated. The brains were quickly removed, and a 3-mm-thick coronal brain slice was cut approximately 4 mm from the frontal pole. The slice was separated into the ipsilateral and contralateral basal ganglia and then frozen in liquid nitrogen. In in vivo studies, the cell medium was removed, and plates were washed three times with phosphate-buffered saline (PBS). The cells were quickly scraped and collected by centrifugation at 4°C, then stored at −80°C.
Total RNA was extracted from the frozen brain tissue and cultured cells with Trizol reagent (Gibco BRL, Grand Island, NY, USA), and 1 μg RNA was digested with deoxyribonuclease I (DNaseI, amplification-grade, Gibco BRL Grand Island, NY, USA). Complimentary DNA was synthesized by reverse transcription mixing 1 μg of DNase I digested RNA (11 μL) with 14 μL reaction buffer (Perkin Elmer, Foster City, CA, USA) containing dNTP (dATP, dCTP, dGTP, and dTTP), 25 mmol/L MgCl2, 10× PCR buffer II, Random Hexamer Primer, RNase inhibitor, and MuMLV reverse transcriptase. The reaction was performed at 42°C for 30 min and terminated with a 5-min incubation at 99°C. Diethyl pyrocarbonate water (75 μL) was added to dilute the complimentary DNA to 100 μL, which was stored at −20°C for later use.
Real-time quantitative PCR was performed with SYBR green as a double-strand DNA specific dye using an Eppendorf Mastercycler EP Realplex (Eppendorf North America Inc., Westbury, NY, USA). The primers for rat hemoglobin α chain (HbA), β chain (HbB), and hemopexin were designed from known sequences of rat HbA-messenger RNA (mRNA) (GeneBank no. U29528), HbB-mRNA (GeneBank no. NM_033234), and hemopexin (GeneBank no. NM_053318) identified by PrimerQuest (Integrated DNA Technologies Inc., Coralville, IA, USA). The primers were as follows: rat HbA, 5′-TGATCC-ACTTCCT-TCTCTGCCCAA-3′ (forward primer) and 5′-ATCAGTTGCCCAAGTGCTTCTTGC-3′ (reverse primer); HbB, 5′-ATGGCCTGAAACACTTGGACAACC-3′ (forward primer) and 5′-TGGTGGCCCAAC-ACAATCACAATC-3′ (reverse primer); and hemopexin, 5′-AAATGGGACCAAGCCAGACTCAGA -3′ (forward primer) and 5′-TGTGATCCATGGTGGTAGCGTCAA -3′ (reverse primer). Primers for rat GAPDH, a housekeeping gene, served as a control. They were as follows: 5′-CCGTGCCAAGATGAAATTGGCTGT-3′ (forward) and 5′-TGTGCATATGTGCGTGTGTGTGTG-3′ (reverse). PCR reactions were run in triplicate on a 96-well plate with a total volume of 20 μL per well using 2.5× SYBR® Green universal master mix. Cycling condition were 2 min at 95°C, 30 s at 95°C, 30 s at 60°C, 1 min at 72°C, 40 cycles, and a melting-curve program (60–95°C with warming of 1.75°C per minute). The relative quantification analysis module was used to compare expression levels of a target gene. The expression levels were calculated using the ∆∆CT method [17]. Fold changes in gene expression of the target gene were equivalent to 2−∆∆CT. With this method, a value equal to 1 represents no change in relative expression between untreated (set to 1.0) and treated samples. We defined overexpression when 2−∆∆CT > 1 and underexpression when 2−∆∆CT < 1.
Western Blot Analysis
Cell medium was removed, and plates were washed three times with chilled PBS. The cells were quickly scraped and collected by centrifugation at 4°C, then stored at −80°C. Western blot analysis was performed as described previously [18]. Cell samples were sonicated with Western blot lysis buffer. Protein concentration was determined using a Bio-Rad protein assay kit (Hercules, CA, USA). A 15-μg portion of protein from each sample was separated by sodium dodecyl sulfate polyacrylamide gel electrophoresis and transferred to a hybond-C-pure nitrocellulose membrane (Amersham, Piscataway, NJ, USA). Membranes were blocked in Carnation nonfat milk and probed with the primary and secondary antibodies. Rabbit polyclonal anti-hemoglobin antibody was used at a 1:1,000 dilution (Cappel, MP Biomedicals Inc., OH, USA). Detection was accomplished with goat anti-rabbit IgG (Bio-Rad, Hercules, CA, USA; 1:2,500 dilution). The antigen–antibody complexes were observed with the ECL chemiluminescence system (Amersham, Piscataway, NJ, USA). Membranes were stripped and reprobed with antibody against β-actin (Sigma, St Louis, MO, USA; 1:6,000 dilution). The relative densities of bands were analyzed with the NIH Image (Version 1.61).
Immunofluorescent Double Labeling
Rats were reanesthetized with pentobarbital (60 mg/kg, i.p.) and underwent intracardiac perfusion with 4% paraformaldehyde in 0.1 M phosphate-buffered saline (pH 7.4). The brains were removed and kept in 4% paraformaldehyde overnight, followed by immersion in 30% sucrose for 3–4 days at 4°C. Specimens were then placed in embedding compound and sectioned (18-μm thickness) on a cryostat. Immunofluorescent double labeling was performed according to the method described previously [18]. The primary antibodies included rabbit anti-hemoglobin (Cappel, MP Biomedicals Inc., OH, USA; 1:100 dilution), mouse anti-glial fibrillary acid protein (GFAP; Chemicon International Inc. Temecula, CA, USA; 1:100 dilution), mouse anti-rat neuronal nuclei (NeuN; Chemicon International Inc., Temecula, CA, USA; 1:100 dilution), and mouse anti-rat CD11b (MRC OX42; Serotec, Oxford, UK; 1:100 dilution). Rhodamine-conjugated goat anti-rabbit antibody (Chemicon International Inc., Temecula, CA, USA; 1:100 dilution) and fluorescein isothiocyanate (FITC)-labeled horse anti-mouse antibody (Vector Laboratories, Burlingame, CA, USA; 1:100 dilution) were used as secondary antibodies. The double labeling was analyzed using a fluorescence microscope.
Statistical Analysis
All data in this study are presented as mean ± SD. Data were analyzed with Student’s t test, analysis of variance, Kruskal–Wallis test, or Mann–Whitney U rank test. Statistical significance was set at 0.05.
Results
Physiological variables including blood pH, PaO2, PaCO2, glucose, hematocrit, and mean arterial blood pressure were controlled in normal ranges (blood pH, 7.35–7.45; PaO2, 80–120 mmHg; PaCO2, 35–45 mmHg; blood glucose level, 80–135 mg/dL; hematocrit, 35–45%; mean arterial blood pressure, 80–120 mmHg).
Hb Was Primarily Expressed in Neurons
Quantitative real-time PCR analysis revealed that the levels of mRNA for both HbA and HbB were higher in primary neurons compared to in primary astrocytes and microglia (p < 0.05, Mann–Whitney U rank test, Fig. 1a, b). Western blot analysis showed two Hb band clusters at approximately 10 and 30 kDa. Hb protein levels were markedly lower in primary cultured astrocytes and microglia compared to the neurons (Fig. 1c).
Relative expression of HbA (a) and HbB (b) mRNA in primary cultured cerebral neurons, astrocytes, and microglia. Value are expressed as mean ± SD; *p < 0.05 versus the other groups. c Western blot analysis showing Hb levels in primary cultured cerebral neurons (lanes 1–3), astrocytes (lane 4–6), and microglia (lane 7–9). Rat Hb was used as a positive control (P). Value are expressed as mean ± SD. # p < 0.01; *p < 0.05 versus the other groups
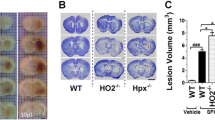
ICH-Induced Hb Expression in Brain
Quantitative real-time PCR showed that HbA mRNA expression in the ipsilateral basal ganglia was increased and reached a peak at 4 h after ICH (Fig. 2a). HbB mRNA expression in the ipsilateral basal ganglia also peaked at 4 h and remained at slightly higher levels 24 h after ICH (Fig. 2b). There was a 14.5 ± 6.2-fold increase in HbA mRNA and 93.7 ± 71.3-fold increase in HbB mRNA in the ipsilateral basal ganglia at 4 h after ICH compared to sham-operated rats (p < 0.05, Fig. 2c, d).
Relative expression in HbA (a) and HbB (b) mRNA in the ipsilateral basal ganglia at 1, 4, 24, or 72 h after ICH. Value are expressed as mean ± SD; *p < 0.05 versus 1 h after ICH. Relative expression in HbA (c) and HbB (d) mRNA in the ipsilateral basal ganglia at 4 h after ICH. Value are expressed as mean ± SD; *p < 0.05 versus sham
Using immunohistochemistry, we found Hb-positive cells in the brains of both sham-operated and ICH rats. The negative control without primary antibody showed no immunoreactive signals. Double-labeling showed that approximately 61 ± 9% NeuN-positive cells, 53 ± 10% GFAP-positive cells, and 7 ± 2% OX42-positive cells were Hb positive in the perihematomal area 3 days after ICH (Fig. 3). In contrast, 36 ± 3% NeuN positive cells, 12 ± 3% GFAP-positive cells, and 6 ± 1% OX42-positive cells were Hb positive in the sham animals.
Hemin Induced Neuronal HbA and HbB Upregulation
To further investigate the mechanism of ICH-induced Hb expression, primary cultured neurons were treated with either hemin (50 or 100 µM) or vehicle for 24 h. Quantitative real-time PCR showed a 44 ± 21- and 61 ± 12-fold increase in HbA mRNA compared to the control after treatment with 50 or 100 µM hemin, respectively (p < 0.05, Fig. 4a). HbB mRNA expression was also increased by 3.2 ± 0.7 and 2.8 ± 0.3 times, respectively (p < 0.05, Fig. 4b).
Hemin Increased Hemopexin mRNA Expression
Hemopexin is a transporter of heme. To determine the effect of hemin on hemopexin expression, neurons were exposed to hemin or vehicle for 24 h. Cells were then collected for real-time PCR. We found 3.6- and 4.6-fold increases of hemopexin mRNA after treatment with 50 and 100 µM hemin, respectively (p < 0.05, Fig. 4c).
Hemin-Induced Hb Expression was Partly Mediated by Iron
To test the effect of iron on hemin-induced Hb expression, primary cultured neurons were treated with or without an iron chelator, deferoxamine. Real-time PCR demonstrated that deferoxamine had no significant effects on HbA and HbB mRNA expression under control conditions (1.05 ± 0.23-fold to HbA mRNA in the control, p > 0.05; 1.11 ± 0.45-fold to HbB mRNA in the control, p > 0.05). However, hemin-induced HbA and HbB mRNA expressions were decreased by deferoxamine (Fig. 5a, b).
Discussion
The main findings of this study are that: (1) HbA and HbB are mainly expressed in cultured neurons, with much lower expression in cultured astrocytes and microglia; (2) HbA and HbB mRNA levels in the basal ganglia are increased after ICH and Hb is localized in neurons and glia; (3) neuronal HbA and HbB mRNA expression is upregulated by hemin; (4) hemopexin mRNA levels in cultured neurons are also upregulated by hemin; and (5) deferoxamine reduces hemin-induced HbA and HbB mRNA upregulation in neurons. These results indicate that ICH increases Hb expression in neurons and glia and that heme and iron may be important factors for ICH-induced Hb expression. The function of the increased HbA and HbB expression after ICH is still uncertain, but it may serve to bind heme that is taken up into cells during clot resolution.
Mammalian Hb has been traditionally thought to be exclusively present in the cells of erythroid lineage and involved solely in oxygen transport. This common perception of Hb has been challenged by recent studies, where the expression of Hb and the mRNAs for its globin constituents have been reported in a variety of nonhematopoietic tissues and cell lines. Liu et al. [19] found that β-globin gene is induced by the treatment of lipopolysaccharide and interferon-γ in murine macrophages. Nishi et al. [20] demonstrated that Hb is expressed by mesangial cells in the kidney. Newton et al. [21] also reported the expression of Hb in alveolar epithelial type II cells of the lung. In addition, Hb has also been found in other sites of the brain, including hippocampus, cerebellum, and pituitary [19, 22–26]. In this study, we provide evidence of HbA and HbB expression as well as Hb protein in rat neurons and glia.
Our previous studies have demonstrated that neuronal Hb is inducible after cerebral ischemia or ischemic preconditioning [5]. In the present study, we found Hb-positive cells in the perihematomal area after ICH. Double labeling identified Hb-positive cells in the perihematomal area as neurons and glia. Hb in neurons and glia could be endogenous or derived from red blood cell lysis. To further confirm endogenous expression of Hb in the brain after ICH, quantitative real-time PCR was performed. We found local synthesis of HbA and HbB mRNA within neurons and glia has a role in ICH-induced endogenous Hb expression. The strong cytoplasmic expression of Hb in vivo (as opposed to surface staining) and the recapitulation of heme-product stimulated Hb gene induction in vitro also strongly support local synthesis of Hb gene products in ICH.
The biological function of endogenous Hb in the brain remains to be elucidated, but exogenous Hb is deleterious to the brain [7]. Exposure of neocortical neurons to Hb produces widespread and concentration-dependent cell death [10], and Hb can cause cytotoxicity in rat cerebral cortical neurons [11]. Our previous studies have shown that intracerebral injection of Hb and its degradation products, including heme, induce brain injury [9]. Endogenous Hb has been shown to have a role in oxygen transport and nitric oxide [1]. It is possible that extracellular Hb activates deleterious cellular pathways, while intracellular Hb is protective. Future studies should determine the role of endogenous HbA and HbB in brain injury after ICH.
Heme is a structural component of hemoglobin. After ICH, heme is released from the hemoglobin. Extracellular heme can be transported into the cytoplasm of cells by binding to its transport protein hemopexin or heptoglobin [12]. Previous studies have shown that heme regulates the expression of α- and β-globin via transcriptional factor Bach 1 in erythroid cells [27, 28]. Hemin, the ferric chloride salt of heme, has also been shown to regulate gene expression of Hb and neuroglobin [13, 14, 29]. In this study, we found that neuronal HbA and HbB mRNA levels were markedly upregulated by hemin. Hemin also significantly increased hemopexin mRNA levels. These results suggest that ICH-induced Hb upregulation may be related to hemin. In addition, HbA mRNA levels were decreased after the treatment of thrombin, whereas HbB mRNA levels were increased compared to the controls, suggesting that α- and β-globin may have a different expression pattern.
Iron is another important component for Hb synthesis. Iron can be released from heme by heme oxygenase (HO). Two isoforms of HO have been identified in the brain. HO-1 is expressed in a very low level in the brain under normal condition. It is rapidly induced in glia cells after ICH [30]. HO-2 is constitutively expressed in neurons in the brain [31]. Our previous studies have shown that iron concentration in the brain can reach very high levels, and non-heme iron is not cleared from the brain within 4 weeks [30]. In the present study, we found that deferoxamine had no significant effects on HbA and HbB mRNA expression under the normal condition. Hemin-induced expression of HbA and HbB mRNA was decreased by deferoxamine, an iron chelator, suggesting that iron is involved in the regulation of hemin-induced Hb expression. However, the inhibitory effect of deferoxamine was incomplete, indicating that factors other than iron may participate in the regulation of hemin-induced Hb expression.
The upregulation of HbA and HbB mRNA expression by hemin suggests a mechanism by which the production of the globin molecules in neurons is coordinated with heme synthesis. In erythroid cells, heme regulates the levels of several proteins involved in Hb synthesis, including HbA and HbB [27, 28], and it is tempting to speculate that a similar feedback mechanism occurs in neurons. In the setting of ICH, the upregulation in HbA and HbB in neurons may serve to buffer heme taken up into those cells as the hematoma resolves.
In conclusion, endogenous HbA and HbB expression is increased in the brain after ICH, which may be related to heme and iron stimulation. Endogenous neuronal hemoglobin has been found in rodent and human brain, and its function is still not clear [4, 5, 32]. It is important to understand the mechanisms behind alpha- and/or beta-globin-induced protective effects since they may lead to expedited strategies to treating ICH, cerebral ischemia, and Parkinson’s disease by attenuating iron toxicity and oxidative brain injury [4, 5, 32].
References
Hardison R (1998) Hemoglobins from bacteria to man: evolution of different patterns of gene expression. J Exp Biol 201(Pt 8):1099–1117
Poyart C, Wajcman H, Kister J (1992) Molecular adaptation of hemoglobin function in mammals. Respir Physiol 90(1):3–17
Schelshorn DW, Schneider A, Kuschinsky W, Weber D, Kruger C, Dittgen T et al (2009) Expression of hemoglobin in rodent neurons. JCereb Blood Flow Metab 29(3):585–595
Richter F, Meurers BH, Zhu C, Medvedeva VP, Chesselet MF (2009) Neurons express hemoglobin alpha- and beta-chains in rat and human brains. J Comp Neurol 515(5):538–547
He Y, Hua Y, Liu W, Hu H, Keep RF, Xi G (2009) Effects of cerebral ischemia on neuronal hemoglobin. J Cereb Blood Flow Metab 29(3):596–605
Xi G, Keep RF, Hoff JT (1998) Erythrocytes and delayed brain edema formation following intracerebral hemorrhage in rats. J Neurosurg 89(6):991–996
Xi G, Keep RF, Hoff JT (2006) Mechanisms of brain injury after intracerebral haemorrhage. Lancet Neurol 5(1):53–63
Sadrzadeh SM, Anderson DK, Panter SS, Hallaway PE, Eaton JW (1987) Hemoglobin potentiates central nervous system damage. J Clin Invest 79(2):662–664
Huang FP, Xi G, Keep RF, Hua Y, Nemoianu A, Hoff JT (2002) Brain edema after experimental intracerebral hemorrhage: role of hemoglobin degradation products. J Neurosurg 96(2):287–293
Regan RF, Panter SS (1993) Neurotoxicity of hemoglobin in cortical cell culture. Neurosci Lett 153(2):219–222
Wang X, Mori T, Sumii T, Lo EH (2002) Hemoglobin-induced cytotoxicity in rat cerebral cortical neurons: caspase activation and oxidative stress. Stroke 33(7):1882–1888
Wagner KR, Sharp FR, Ardizzone TD, Lu A, Clark JF (2003) Heme and iron metabolism: role in cerebral hemorrhage. J Cereb Blood Flow Metab 23(6):629–652
Rutherford TR, Clegg JB, Weatherall DJ (1979) K562 human leukaemic cells synthesise embryonic haemoglobin in response to haemin. Nature 280(5718):164–165
Fibach E, Kollia P, Schechter AN, Noguchi CT, Rodgers GP (1995) Hemin-induced acceleration of hemoglobin production in immature cultured erythroid cells: preferential enhancement of fetal hemoglobin. Blood 85(10):2967–2974
Jiang Y, Wu J, Hua Y, Keep RF, Xiang J, Hoff JT et al (2002) Thrombin-receptor activation and thrombin-induced brain tolerance. J Cereb Blood Flow Metab 22(4):404–410
McCarthy KD, de Vellis J (1980) Preparation of separate astroglial and oligodendroglial cell cultures from rat cerebral tissue. J Cell Biol 85(3):890–902
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25(4):402–408
Xi G, Keep RF, Hua Y, Xiang J, Hoff JT (1999) Attenuation of thrombin-induced brain edema by cerebral thrombin preconditioning. Stroke 30(6):1247–1255
Liu L, Zeng M, Stamler JS (1999) Hemoglobin induction in mouse macrophages. Proc Natl Acad Sci USA 96(12):6643–6647
Nishi H, Inagi R, Kato H, Tanemoto M, Kojima I, Son D et al (2008) Hemoglobin is expressed by mesangial cells and reduces oxidant stress. J Am Soc Nephrol 19(8):1500–1508
Newton DA, Rao KM, Dluhy RA, Baatz JE (2006) Hemoglobin is expressed by alveolar epithelial cells. J Biol Chem 281(9):5668–5676
Ohyagi Y, Yamada T, Goto I (1994) Hemoglobin as a novel protein developmentally regulated in neurons. Brain Res 635(1–2):323–327
Blalock EM, Chen KC, Sharrow K, Herman JP, Porter NM, Foster TC et al (2003) Gene microarrays in hippocampal aging: statistical profiling identifies novel processes correlated with cognitive impairment. J Neurosci 23(9):3807–3819
Slemmon JR, Hughes CM, Campbell GA, Flood DG (1994) Increased levels of hemoglobin-derived and other peptides in Alzheimer's disease cerebellum. J Neurosci 14(4):2225–2235
Wu CW, Liao PC, Yu L, Wang ST, Chen ST, Wu CM et al (2004) Hemoglobin promotes Abeta oligomer formation and localizes in neurons and amyloid deposits. Neurobiol Dis 17(3):367–377
Leffers H, Navarro VM, Nielsen JE, Mayen A, Pinilla L, Dalgaard M et al (2006) Increased expression of alpha- and beta-globin mRNAs at the pituitary following exposure to estrogen during the critical period of neonatal sex differentiation in the rat. J Steroid Biochem Mol Biol 99(1):33–43
Tahara T, Sun J, Igarashi K, Taketani S (2004) Heme-dependent up-regulation of the alpha-globin gene expression by transcriptional repressor Bach1 in erythroid cells. Biochem Biophys Res Commun 324(1):77–85
Tahara T, Sun J, Nakanishi K, Yamamoto M, Mori H, Saito T et al (2004) Heme positively regulates the expression of beta-globin at the locus control region via the transcriptional factor Bach1 in erythroid cells. J Biol Chem 279(7):5480–5487
Zhu Y, Sun Y, Jin K, Greenberg DA (2002) Hemin induces neuroglobin expression in neural cells. Blood 100(7):2494–2498
Wu J, Hua Y, Keep RF, Nakamura T, Hoff JT, Xi G (2003) Iron and iron-handling proteins in the brain after intracerebral hemorrhage. Stroke 34(12):2964–2969
Vincent SR, Das S, Maines MD (1994) Brain heme oxygenase isoenzymes and nitric oxide synthase are co-localized in select neurons. Neuroscience 63(1):223–231
Biagioli M, Pinto M, Cesselli D, Zaninello M, Lazarevic D, Roncaglia P et al (2009) Unexpected expression of alpha- and beta-globin in mesencephalic dopaminergic neurons and glial cells. Proc Natl Acad Sci USA 106(36):15454–15459
Acknowledgments
This study was supported by grants NS-017760, NS-039866, NS-047245 NS-052510, and NS-057539 from the National Institutes of Health (NIH) and 0755717Z and 0840016N from American Heart Association (AHA). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH and AHA. MMW is supported by NS-062816 and NS-054724.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
He, Y., Hua, Y., Lee, JY. et al. Brain Alpha- and Beta-Globin Expression after Intracerebral Hemorrhage. Transl. Stroke Res. 1, 48–56 (2010). https://doi.org/10.1007/s12975-009-0004-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-009-0004-x