Abstract
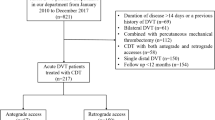
A recent national study in Japan indicated that 5.8 % of deep venous thrombosis (DVT) patients were treated using endovascular procedures, 83 % of which included catheter-directed thrombolysis (CDT). However, the details of these endovascular procedures and their outcomes have not yet been fully evaluated. Using DVT data from the EDO registry (EnDOvascular treatment registry) database, a total of 35 symptomatic iliac or femoral DVT patients who received endovascular treatment (54.3 % male, age 64.7 ± 15.1) were analyzed. The dominant patient risks were being bedridden (22.9 %) and May–Thurner syndrome (25.7 %). Approximately 77.1 % of patients were treated using an antegrade approach, and CDT and other endovascular procedures were performed in 82.9 and 57.1 % of patients, respectively. A periprocedural inferior vena cava (IVC) filter was used in 94.1 % of patients, which remained implanted in 37.1 and 20.0 % of patients after discharge and 6 months after hospitalization, respectively. After 6 months of treatment, 2.9 % of patients experienced a recurrence of DVT and 5.7 % suffered revascularization, but no patient had a recurrence of pulmonary embolism. Subjective symptoms improved in 80.0 % of patients, while 2.9 % of patients felt worse at 6 months after treatment. Postthrombotic syndrome-related symptoms were observed in seven patients (19.4 %), and edema was most frequently observed (71.4 %). The details of CDT procedures, such as approach site and the removal of the IVC filter, varied among hospitals. Despite improved symptoms, further procedural standardization and data collection should be conducted to reduce complications and improve outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
The standard therapy for deep venous thrombosis (DVT) consists of anticoagulants, compression therapy, and mobilization, which together decrease the risk of pulmonary embolism and the recurrence of DVT [1]. Despite the use of appropriate anticoagulants, residual thrombosis is associated with postthrombotic morbidity [2]. The early removal and resolution of the thrombus have been suggested as beneficial for the prevention of postthrombotic syndrome (PTS) [2–4]. A previous randomized controlled clinical trial has shown the efficacy of catheter-directed thrombolysis (CDT) in the prevention of PTS [3].
A recent Japanese national study indicated that 5.8 % of DVT patients were treated using endovascular procedures, 83 % of which included CDT [5]. However, the details of these procedures and their thrombolytic dosages were not reported. The approved dosages of thrombolytic drugs for CDT in Japan are significantly lower than those in other countries, as mentioned in the Japanese guidelines [1]. Furthermore, other catheter procedures such as ballooning and stenting have not been fully evaluated [6].
A multicenter prospective registry (EnDOvascular treatment registry in the Tokyo area: EDO registry) has been established to determine the real clinical practice of catheter therapy in specific situations (subclavian artery stenosis/occlusion, common femoral artery stenosis/occlusion, popliteal artery stenosis/occlusion, DVT, and acute limb ischemia). We analyzed the real-world clinical practice of endovascular treatment for DVT using the DVT data from the EDO registry database.
Methods
Data source
The EDO registry is an ongoing, prospective, multicenter registry designed to collect clinical backgrounds, procedural details, and clinical outcome data for consecutive complicated endovascular treatment patients with the following diseases: common femoral artery stenosis/occlusion, popliteal artery stenosis/occlusion, subclavian artery stenosis/occlusion, acute limb ischemia, and DVT. In this registry, 10 hospitals with cardiovascular centers within the metropolitan Tokyo area registered all consecutive endovascular procedures performed during the study period, including cases of failure, using an Internet-based interface. The use of these data in the present study was approved by the Institutional Ethics Committee of each hospital, and all subjects gave informed consent.
Study population and follow-up
A total of 324 patients were enrolled in this registry from November 2011 to October 2013. Among these patients, all consecutive symptomatic DVT patients who received endovascular treatment were analyzed in this study. Clinical outcomes and subjective symptoms at 6 months after treatment were evaluated by the doctors at each hospital.
Variables and definition
We examined the baseline characteristics of all patients and their previous histories with DVT. We also measured patient thigh and calf circumferences according to the methods of a previous report [7]. The severity of pulmonary embolism was assessed according to the Japanese Circulation Society guidelines [1]. Patient outcomes were evaluated by death, symptoms, and bleeding complications as assessed by the following The Global Use of Strategies to Open Occluded Arteries (GUSTO) criteria: severe, intracerebral hemorrhaging resulting in a substantial hemodynamic compromise requiring treatment; moderate, bleeding requiring a blood transfusion but not resulting in a hemodynamic compromise; mild, bleeding that does not meet the above criteria [8]. Recurrences of DVT and PE were defined as symptomatic events that met the classical definite diagnosis criteria, which meant confirmation by computed tomography and other imaging modalities [9].
Venographic severity score
The extent of clot lysis was assessed using a scoring system previously developed by Yamada et al. [10]. All venographic images were read and scored independently by two trained observers blinded to the clinical data. The scores were calculated for nine venous segments: the upper, middle, and lower IVC; the common iliac vein; the external iliac vein; the common femoral vein; the proximal and distal portions of the femoral vein; and the popliteal vein. The scores were classified into seven categories according to the extent and form of the thrombus: 0 no thrombus; 1 thrombus extending over one-third of the length of the venous segment without occlusion; 2 thrombus extending over two-third of the length of the venous segment without occlusion; 3 thrombus extending along the entire length of the venous segment without occlusion; 4 thrombus extending over one-third of the length of the venous segment with occlusion; 5 thrombus extending over two-third of the length of the venous segment with occlusion; 6 thrombus extending the entire length of the venous segment with occlusion. The total scores before and after treatment were then calculated by adding the scores of the nine venous segments.
Statistical analysis
Continuous data were expressed as means ± standard deviations except for the D-dimer variables, which are summarized by medians and quartiles due to their positive skew and comparisons between groups were made using the t test or Mann–Whitney U test. Categorical data were compared between groups with χ 2 or Fisher’s exact tests. Statistical significance was inferred when p < 0.05. All statistical testing and data analysis were performed with SPSS version 17 (SPSS Inc., Chicago, IL, USA).
Results
A total of 35 patients were analyzed, 54.3 % of which were male, and their mean age was 64.7 years (Table 1). Aside from hypertension, no specific previous history or medications related with DVT were reported for any patient. Laboratory data showed significant high D-dimer levels and slightly elevated C-reacted protein levels.
All patients had an iliac or femoral vein thrombus, and ten patients (28.6 %) had an inferior vena cava thrombus. Table 2 showed the characteristics of DVT. The left side was predominantly (82.9 %) affected compared to the right side. Almost all patients presented edema and pain, but only one patient (2.8 %) was diagnosed with phlegmasia cerulea dolens. Considerable etiologies of DVT are listed (Table 2), but we could not identify dominant risks other than being bedridden and May–Thurner syndrome (22.9 and 25.7 %, respectively). Pulmonary embolism was detected in 31.4 % of patients, the severity of which was submassive in every patient. Pulmonary hypertension was observed in only two patients.
Catheterization therapy was performed in approximately three-fourth of the patients within 14 days (Table 3). An IVC filter was inserted in almost all (94.1 %) of the patients before EVT. The most common puncture site was the popliteal vein, but 28.6 % of the patients were treated via the femoral vein. Nine patients required an additional puncture, and two-third of patients was treated via an antegrade approach. The initial daily dosages of heparin and urokinase were 13645.2 ± 3764.3 IU and 413.3 ± 30.1 × 103 IU, respectively. During the procedure, approximately 60.6 ± 32.5 ml of contrast was employed.
Among catheter procedures, CDT and other endovascular procedures such as ballooning, aspiration, and stenting were performed in 82.9 and 57.1 % of patients, respectively. Urokinase was preferred for this purpose, and in 65.5 % of patients, thrombolysis was initiated in the catheterization room. A CDT catheter could not be placed in only one patient. During hospitalization, an average of 1.6 ± 0.8 endovascular procedures was performed, with 15 (42.9 %) patients requiring more than one procedure. Pulse-spray methods were used more frequently than was the continuous infusion method (69.0 vs 31.0 %). Intravascular ultrasound was used during the procedure in approximately one-third of the patients (34.3 %). Thigh and calf circumferences decreased after treatment (Fig. 1), and the average postvenographic severity score also significantly decreased, from 27.1 ± 11.0 to 8.1 ± 8.0 (Fig. 2) (p < 0.001). But in four patients, the venographic score before and after treatment did not differ. The improvement of the venographic score after treatment did not differ between the pulse-spray and continuous infusion methods (Fig. 3).
Table 4 displays the device size and details. Five patients need stent implantation, and the size of them varied. Regarding thrombus aspiration, a sheath was used in 41.7 % of the procedures. The size of the aspiration catheter quite varied.
The average duration of hospitalization was approximately 2 weeks (17.5 days) (Table 5). No deaths occurred during hospitalization, but one patient developed a DVT recurrence. Additional thrombus aspiration, ballooning, and stenting (but not CDT) were performed in this patient. Four complications occurred: three bleeding complications and one access site infection. One of three bleedings was severe bleeding, which resulted in inadequate anticoagulation and no improvement of venographic score.
Outcomes approximately 6 months after treatment are shown in Table 6. Subjective symptoms improved in 80 % of patients (71.4 %, markedly better; 8.6 %, mildly better). However, one patient (2.9 %) felt worse at 6 months after treatment. Lesion revascularization had to be targeted in 5.7 % of patients, and DVT recurred in one patient (2.9 %). Postthrombotic syndrome-related symptoms were observed in seven patients (19.4 %), of which edema was the most frequent. The IVC filter remained in 20 % of patients after 6 months.
The only patient with a recurrence of DVT was retrospectively analyzed. She was an 80-year-old female who had experienced a hip fracture before the occurrence of DVT. Because her DVT was limited in external iliac area, she was treated using CDT and anticoagulants without any complications. Her venographic score significantly improved (36–3), and her thigh and calf circumferences also improved (from 44.5 to 38.8 cm and from 36.5 to 29.5 cm, respectively) during hospitalization. CDT by the pulse-spray method was performed from the internal jugular vein, and the IVC filter had not been removed by 6 months after the procedure. Anticoagulants were continued for 6 months after initial treatment.
Discussion
Catheter therapy for DVT is occasionally indicated according to the Japanese guidelines and is considered useful for resolving a residual thrombus and reducing residual symptoms. However, few studies have examined how frequently and with what details these procedures are performed in clinical practice. This report describes the first multicenter study regarding the real clinical practices of catheter therapy for DVT in Japan.
Catheter therapy indication of DVT
The indication of catheter therapy for DVT is shown in the Japanese guidelines and considered as a Class 2b recommendation [1]. Only patients who had undergone catheter therapy for iliac or femoral venous thrombosis were analyzed in the present study. Iliac and femoral DVT is the most appropriate indication for catheter therapy according to previous studies [3]. We included more than 80 % iliofemoral DVT, which was slightly higher than in other countries but similar to previous CDT trials in Japan [3, 10]. PE was indicated in 31.4 % of the studied patients; this rate was higher than that of international data but lower than that of previous CDT data reported by Yamada et al. [3, 10]. The present patient inclusion rate was comparable to that of previous studies, but we included not only CDT patients but also those who underwent other endovascular procedures, such as ballooning and stenting, which may have led to patient selection differences.
Procedures
Approximately 77.1 % of the patients were treated via an antegrade approach. The Japanese guidelines also indicate an antegrade approach as preferred due to valve preservation concerns [1]. Puncture site differences may be due to the obstruction of popliteal vein; more than half of the studied patients had a venous thrombus in the popliteal vein, which was the most frequent puncture site. A previous report has indicated that half of iliofemoral DVT patients have an occluded popliteal vein [11]. An occluded popliteal vein may be punctured to perform CDT and other procedures, but some physicians may be unwilling to puncture an occluded vein. We could not conclude from the present results which was the best approach to perform endovascular procedures, but we determined the prevalence and frequencies of different approaches. Furthermore, it should be noted that the only patient in the present registry who experienced a recurrence of DVT was treated via a retrograde approach from the internal jugular vein.
Endovascular procedures other than CDT were performed in approximately 57.1 % of patients, including 5 (25 %) stent implantations. All of the patients in which stenting was conducted had May–Thurner syndrome. Many previous studies have indicated the efficacy of stent implantation in patients with May–Thurner syndrome [12–14]. One of five stents was occluded 6 months after treatment. Previous reports have indicated approximately 95 and 91–93 % patency at 6 months and 1 year after stent implantation, respectively [13, 14]. More patients and further long-term follow-ups must be assessed for comparison with previous reports, but the risk of stent occlusion should be noted. Furthermore, nine of the studied patients were diagnosed with May–Thurner syndrome, but only five of these patients received stent implants. Further work regarding the indication of stenting should be conducted by collecting clinical outcomes for consecutive patients diagnosed with May–Thurner syndrome.
Pulse-spray methods were preferred to continuous infusion in the present registry (69.0 vs 31.0 %). No previous studies have directly compared pulse-spray and continuous infusion methods. However, pulse-spray methods are generally considered to have several important merits over continuous infusion according to previous studies: (1) macerating the clot and increasing the contact area of the thrombus with the thrombolytic agent by penetrating intrathrombic injections, (2) increasing the rate of lysis by applying the concentrated agent, (3) minimizing the dilution of the thrombolytic agent, systemic effects, and effects of plasmin inhibitors in plasma due to the retention of the thrombolytic agent in the thrombus, (4) increasing the rate of lysis by simultaneously treating the entire thrombus, and (5) reducing the cost and potential bleeding problems associated with the use of thrombolytic agents [15, 16]. Furthermore, the efficacy of pulse-spray methods has been advocated in Japan, which may affect clinical practice [10]. Further study is necessary to directly compare pulse-spray and continuous infusion methods, but the present registry data suggest that pulse-spray methods are preferable.
Thromboaspiration is used to decrease the dose of the thrombolytic agent and increase the speed of thrombus removal [11]. Aspiration is frequently performed in patients with acute limb ischemia; but in DVT patients, reports about the effects of aspiration are limited and often involve combination with CDT [17]. Thromboaspiration was performed in 34.3 % of the studied patients. In approximately half of patients, thromboaspirations were performed via sheaths, half of which were smaller than 6Fr in size. A previous study mentioned that aspiration had several disadvantages, such as its requirement of a large vascular sheath and its potential to decrease hemoglobin levels [17]. A smaller aspiration catheter may be less useful than a larger one. Furthermore, manual aspiration is the only method permitted in Japan. The real effectiveness of smaller sheath manual aspiration should be carefully considered.
Outcomes
Several measures of patient outcomes after catheter therapy for DVT were considered. We used venographic severity scores and physical findings such as thigh and calf circumferences, which were used in a previous study [10]. We could, therefore, compare our results to those of previous work. The venographic severity scores before and after the procedure were comparable with those of previous data. Hospitalization duration and 6-month outcomes, including complications, were also comparable to those observed in previous studies. However, the usage of IVC filters in comparison with that of previous reports should be given particular attention. Of the studied patients, 37.1 and 20.0 % still had an IVC filter implanted after discharge and 6 months after hospitalization, respectively, and a previous study indicated an IVC filter implantation rate of approximately 40 % in Japan [5]. The Clinical Practice Guidelines of the Society for Vascular Surgery and the American Venous Forum recommend against routine use of IVC filters (permanent or temporary) in conjunction with catheter-directed pharmacologic thrombolysis of the iliofemoral venous segments, indicating no need to insert an IVC filter even in periprocedural situations. Below 1.0 % periprocedural pulmonary embolism was not to be paid attention. Furthermore, it should be noted that the only studied patient with a recurrence of DVT possessed an IVC filter at 6 months after implantation. Further data are required, but the results suggest that IVC filters should not be used routinely during endovascular therapy.
Limitations
This study is the first to examine the real clinical practices of endovascular therapy for DVT patients. Nevertheless, we should mention several of its limitations. First, because the present work was a cohort study to reveal the clinical practices of endovascular therapy for DVT, we did not obtain data for DVT patients who were not treated by catheter therapy. However, we did not intend to compare patient characteristics between non-catheter and catheter therapy groups in this study. We instead aimed to determine the real clinical practice of catheter procedures for DVT, because only 5.8 % of DVT patents are treated by endovascular treatment. Second, we could not obtain the real postthrombotic syndrome incidence after endovascular therapy. Instead, we were only able to analyze the typical symptoms related with postthrombotic syndrome. Because many studies have already shown the effectiveness of CDT and other procedures, the present study only focused on obtaining information regarding its clinical practice. Third, our dataset is insufficiently large to reach conclusions regarding patient outcome and other clinical implications. As previously mentioned, the endovascular treatment of DVT is not frequently used in Japan. Further collection of registry data is required to obtain information on a greater number of patients.
Conclusion
This study represents the first analysis of multicenter data regarding endovascular therapy for DVT patients. CDT was shown to be a safe and effective therapy, especially for improving symptoms. An IVC filter was used in almost all (94.1 %) of the patients, and an average of 1.6 procedures was required during hospitalization. Details of the procedures, including approach site, devices, and removal of the IVC filter, varied among hospitals and were different from those of previous studies. Although endovascular treatment of DVT improved the symptoms of patients in the present registry, further standardization of procedures and data collection is required to reduce complications and improve outcomes.
References
JCS Joint Working Group. Guidelines for the diagnosis, treatment and prevention of pulmonary thromboembolism and deep vein thrombosis (jcs 2009). Circ J. 2011;75:1258–81.
Comerota AJ, Grewal N, Martinez JT, Chen JT, Disalle R, Andrews L, Sepanski D, Assi Z. Postthrombotic morbidity correlates with residual thrombus following catheter-directed thrombolysis for iliofemoral deep vein thrombosis. J Vasc Surg. 2012;55:768–73.
Enden T, Haig Y, Klow NE, Slagsvold CE, Sandvik L, Ghanima W, Hafsahl G, Holme PA, Holmen LO, Njaastad AM, Sandbaek G, Sandset PM. Long-term outcome after additional catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis (the cavent study): a randomised controlled trial. Lancet. 2012;379:31–8.
Strijkers RHW, Grommes J, Arnoldussen CWKP, de Graaf R, ten Cate AJ, Wittens CHA. Ultrasound-accelerated catheter-directed thrombolysis in acute iliofemoral deep venous thrombosis. J Vasc Surg Venous Lymphat Disord. 2013;1:225–30.
Nakamura M, Miyata T, Ozeki Y, Takayama M, Komori K, Yamada N, Origasa H, Satokawa H, Maeda H, Tanabe N, Unno N, Shibuya T, Tanemoto K, Kondo K, Kojima T. Current venous thromboembolism management and outcomes in japan. Circ J. 2014;78:708–17.
Enden T, Klow NE, Sandvik L, Slagsvold CE, Ghanima W, Hafsahl G, Holme PA, Holmen LO, Njaastad AM, Sandbaek G, Sandset PM. Catheter-directed thrombolysis vs anticoagulant therapy alone in deep vein thrombosis: results of an open randomized, controlled trial reporting on short-term patency. J Thromb Haemost. 2009;7:1268–75.
Shi HJ, Huang YH, Shen T, Xu Q. Percutaneous mechanical thrombectomy combined with catheter-directed thrombolysis in the treatment of symptomatic lower extremity deep venous thrombosis. Eur J Radiol. 2009;71:350–5.
Kahn SR, Partsch H, Vedantham S, Prandoni P, Kearon C. Definition of post-thrombotic syndrome of the leg for use in clinical investigations: a recommendation for standardization. J Thromb Haemost. 2009;7:879–83.
Heit JA, Mohr DN, Silverstein MD, Petterson TM, O’Fallon WM, Melton LJ 3rd. Predictors of recurrence after deep vein thrombosis and pulmonary embolism: a population-based cohort study. Arch Intern Med. 2000;160:761–8.
Yamada N, Ishikura K, Ota S, Tsuji A, Nakamura M, Ito M, Isaka N, Nakano T. Pulse-spray pharmacomechanical thrombolysis for proximal deep vein thrombosis. Eur J Vasc Endovasc Surg. 2006;31:204–11.
Oguzkurt L, Ozkan U, Gulcan O, Koca N, Gur S. Endovascular treatment of acute and subacute iliofemoral deep venous thrombosis by using manual aspiration thrombectomy: long-term results of 139 patients in a single center. Diagn Interv Radiol. 2012;18:410–6.
Budnur SC, Singh B, Mahadevappa NC, Reddy B, Nanjappa MC. Endovascular treatment of iliac vein compression syndrome (may-thurner). Cardiovasc Interv Ther. 2013;28:101–5.
Liu Z, Gao N, Shen L, Yang J, Zhu Y, Li Z, Si Y. Endovascular treatment for symptomatic iliac vein compression syndrome: a prospective consecutive series of 48 patients. Ann Vasc Surg. 2014;28:695–704.
Xue GH, Huang XZ, Ye M, Liang W, Zhang H, Zhang JW, Zhang BG. Catheter-directed thrombolysis and stenting in the treatment of iliac vein compression syndrome with acute iliofemoral deep vein thrombosis: outcome and follow-up. Ann Vasc Surg. 2014;28:957–63.
Chang R, Cannon RO 3rd, Chen CC, Doppman JL, Shawker TH, Mayo DJ, Wood B, Horne MK 3rd. Daily catheter-directed single dosing of t-pa in treatment of acute deep venous thrombosis of the lower extremity. J Vasc Interv Radiol. 2001;12:247–52.
Vedantham S, Vesely TM, Parti N, Darcy M, Hovsepian DM, Picus D. Lower extremity venous thrombolysis with adjunctive mechanical thrombectomy. J Vasc Interv Radiol. 2002;13:1001–8.
Rigatelli G, Cardaioli P, Roncon L, Giordan M, Milan T, Zonzin P. Combined percutaneous aspiration thrombectomy and rheolytic thrombectomy in massive subacute vena cava thrombosis with ivc filter occlusion. J Endovasc Ther. 2006;13:373–6.
Acknowledgments
We would like to extend our profound gratitude to Norihiro Yamada, Yoshinori Nagashima, Tetsuo Yamanaka, and Yuichi Suzuki for correcting our data and improving our discussions.
Conflict of interest
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Mizuno, A., Anzai, H., Utsunomiya, M. et al. Real clinical practice of catheter therapy for deep venous thrombosis: periprocedural and 6-month outcomes from the EDO registry. Cardiovasc Interv and Ther 30, 251–259 (2015). https://doi.org/10.1007/s12928-014-0314-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-014-0314-0