Abstract
The Precision Medicine Initiative (PMI) has created considerable discussions about research participant issues including re-consent and how and when to incorporate the patient experience into clinical trials. Within the changing landscape of genetic and genomic research, the preferences of participants are lacking yet are needed to inform policy. With the growing use of biobanks intended to support studies, including the national research cohort proposed under the PMI, understanding participant preferences, including re-consent, is a pressing concern. The Participant Issues Project (PIP) addresses this gap, and here we present data on participant attitudes regarding re-consent and broad consent in research studies. PIP study participants came from the Northwest Cancer Genetics Registry and included cancer patients, relatives, and controls. Thirty telephone interviews were conducted and analyzed using content and thematic analysis. Results indicate that in some scenarios, re-consent is needed. Most participants agreed that re-consent was necessary when the study direction changed significantly or a child participant became an adult, but not if the genetic variant changed. Most participants’ willingness to participate in research would not be affected if the researcher or institution profited or if a broad consent form were used. Participants emphasized re-consent to provide information and control of the use of their data, now relevant for tailored treatment, while also prioritizing research as important. In the era of precision medicine, it is essential that policy makers consider participant preferences with regard to use of their materials and that participants understand genetic and genomic research and its harms and benefits as well as what broad consent entails, including privacy and re-identification risks.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The Precision Medicine Initiative (PMI) vision is that scientists, clinicians, social and behavioral investigators, and patients will collaborate to generate and use massive data networks that access, aggregate, integrate, and analyze information with the goal of providing precise health advice, diagnoses, and treatments for each individual (Hawgood et al. 2015). Precision medicine (PM) has already created several challenges for researchers as they consider conducting studies on large and existing cohorts (Overby and Tarczy-Hornoch 2013). For example, creating a million-person cohort, mostly from existing cohorts of study participants, is a goal of the PMI and will require many new research relationships to occur on a scale that we have not seen before. These new interactions will bring specific challenges, such as how best to obtain consent and for what purposes, how to involve and maintain very large numbers of participants and their data, including genomic data, and how to return results that are actionable to patients and providers (Alyass et al. 2015). We will need to apply both new and existing methods to solve these dilemmas to continue to build trust and participation among the current and future individuals that engage in this research agenda.
Genomic researchers and Institutional Review Board (IRB) professionals confront these complex PM challenges in the recruitment for and review of new and existing genomic studies, respectively. Questions about re-consent, return of research results, and identifiability continue to be debated within and between these two groups. This conversation will become more complex as the PMI national research cohort is assembled and other PM focused research and clinical trials are implemented. Researchers are divided on whether re-consent is needed for data sharing and on the nature and degree of risk of re-identification in genetic studies (Edwards et al. 2011). When IRB professionals were surveyed, they, too, were divided on when re-consent should occur and the level of risk to participants of re-identification (Lemke et al. 2010). A minority of both researchers and IRB members on genetic studies indicated that the chance of harm to participants or re-identification was unlikely, with more genetic researchers trusting that coded genetic data would deter re-identification (Edwards et al. 2012). In addition, while some advocate broad consent as a beneficial way to promote research (Petrini 2010; Haga and Beskow 2008), others question the ethics associated with broad consent (Hofmann 2009; Caulfield 2007; Arnason 2004). These findings indicate several key topics that are problematic for researchers and IRBs and that will be relevant to the efforts of the PMI. However, despite informed consent being a cornerstone of participant protections, the role of consent―particularly re-consent for longer running repositories and ongoing studies that were established prior to genome-wide association studies (GWAS) and now the sequencing era―is still largely unresolved (Tasse et al. 2010).
While the views of those who conduct and oversee research are crucial, the voice of research participants, whom both IRBs and researchers are charged to protect, is often not included in these debates. The biological samples and personal and family medical history of biobank and research participants will continue to be sought after for genomic studies, and as we enter the PM era, a greater emphasis will be placed on these individuals and their data. Information about participants’ views on issues related to participation in genetic and genomic studies, including consent, is needed to inform policies around these issues. We conducted qualitative interviews with cancer registry participants to assess their views toward key issues of consent, including the harms and benefits of broad consent, one of the most-invoked alternatives to re-consent.
Materials and methods
Recruitment
The Northwest Cancer Genetics Registry (NWCGR) was created in 2010 to extend the involvement of participants in the Northwest Cancer Genetics Network, which was established in 1998 as one of seven population-based sites in the USA and funded by the National Cancer Institute (Anton-Culver et al. 2003). The NWCGR is composed of individuals with cancer and controls recruited from the Pacific Northwest region of the USA, primarily from Seattle and the surrounding Puget Sound region of Washington State. The population from this region is predominantly non-Hispanic white and tends to be well-educated and of higher socio-economic status. First-degree relatives of cancer cases were also recruited and come from a broader geographic area. When established in 2010, the registry included 81 % of the original cohort (n = 3539; 220 have refused and 594 of the original cohort are confirmed to be deceased based on the report from a relative or through a search of the US National Death Index conducted between prior to 2010) and includes cancer cases, relatives, and controls. The majority of participants in the registry self-reported as non-Hispanic white (89 %), Asian (3 %), Hispanic white (2 %), and Black (1 %), and 3 % self-reporting as American Indian, Pacific Islander, or other. Individuals with cancer (n = 1796) at baseline (cases) make up about half (51 % of 3539) of the registry and have a range of primary cancers. Most cancer participants have melanoma and skin cancer (43 %), thyroid (20 %), prostate (9 %), breast (8 %), and pancreatic (1 %) cancer, as well as a number of other less frequent cancer types. There is demographic and extensive family history information for all participants, including the 965 controls and 778 first-degree relatives. The average age of the active participants is 62.6 years; 61 % are female.
Target recruitment for the qualitative interviews was up to 40 total participants, or until saturation was achieved. The goal was to have equal numbers of men and women and cases, controls, and relatives in proportions reflecting the registry (approximately half cases and the other half with approximately equal numbers of first-degree relatives and controls). Additional individuals were also recruited to participate in pre- and pilot testing the study instrument (up to 35 in total). For the cases, skin, breast, prostate, and/or colorectal cancer were prioritized for selection for this study because they are among the most prevalent cancers in the USA and represent the views of a large stakeholder group involved in genetic studies. First-degree relatives and controls were included in the sample because their expectations and motivations for participating in research may differ from those of cancer cases. To meet our goal of up to 40 participants, plus up to an additional 35 participants for pre- and pilot testing of interview guides and study instruments, an initial list of 160 individuals (equal numbers of men and women and distributed across cases, control, and relative groups) who had responded to the most recent NWCGR survey (2 years prior to this project) were identified as eligible for the interviews. Due to the predominance of non-Hispanic whites in the sample, minority participants were overrepresented in this list of eligible participants.
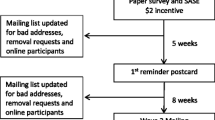
A letter, including a study consent and participation instructions, was mailed to the subset of eligible participants in batches reflecting the desired distribution of participants. Letters were sent beginning in late 2011 and continuing through the first part of 2012 inviting them to participate in interviews about consent for cancer genetic research. Interested participants were asked to call a toll-free line or send an email. A maximum of two follow-up letters were mailed at 2-week intervals. An initial interview guide was drafted through the process of expert consensus and drew upon a previous study that examined the attitudes of researchers and IRB members toward genetic research issues (Edwards et al. 2011). Six participants from NWCGR participated in pre- and pilot testing the interview protocol, which was then revised for clarity. The final interview protocol comprised questions concerning research relationships, re-consent, data repositories, and return of results in research focused on cancer genetics. Eighty potential participants identified as eligible were invited by mail to participate, and 30 were interviewed concerning re-consent issues; one interview was terminated prior to the re-consent section, four people were reported deceased, two refused, three were lost to follow-up (letters of invitation were returned as undeliverable), and 34 did not respond. After team review, idea saturation was considered achieved with these 31 participants. Each participant received a US$25 gift card. This study was approved by the IRBs of University of Washington, University of Georgia, Boston University, and Johns Hopkins University.
Data collection
Using a semi-structured interview guide containing four re-consent-related questions with follow-up probes, two broad consent questions, and one question related to effects of for-profit research, participants’ views were gathered via telephone interviews, a mode convenient to participants and one that encourages discussion of potentially sensitive topics (Novick 2008). The questions asked participants to consider three scenarios in which the research focus had changed from the original study to (1) a different but related health condition—e.g., a different type of cancer; (2) a different and unrelated health condition—e.g., depression; and (3) the same cancer but a different gene. In addition, participants were asked views about the re-consent of a child who has achieved his/her age of majority. Participants were queried about whether the researcher or research institution receiving money from a patent or a license would affect their willingness to participate in a study, the harms and benefits of broad consent, and whether its use would affect willingness to participate in research. For the re-consent-related questions, the subset of participants endorsing re-consent were also asked whether re-consent was mandatory or merely desirable. Both interviewers were trained in standard interview techniques, and interviews lasted 45–90 min. Study identification numbers were assigned to protect confidentiality. Interviews were recorded, transcribed, and de-identified. Transcriptions were checked for accuracy by a non-interviewer before coding commenced.
Data analysis
All transcripts were uploaded into qualitative analysis software Atlas.ti 7 for coding and content analysis (Graneheim and Lundman 2004). A code book incorporating both a priori and iterative themes was created through the process of expert consensus. Briefly, the interview discussion guide was used to first develop a provisional list of mainly descriptive codes. A code book was then developed by the study team, which refined and changed the provisional list of descriptive codes as new ideas were encountered in the reading of each interview transcript. Codes included unique descriptive and interpretive codes that applied to concepts used at least once by two or more of the participants, and could be used once to identify a single passage, or more than one code could be used within a passage depending on the complexity of the passage. Two coders coded content independently to determine the level of endorsement (agree, disagree, or neutral) about whether re-consent would be needed and why the level endorsement was indicated. To explore participant responses, additional thematic analysis of the coded data was performed (Vaismoradi et al. 2013), using the “why” part of the interview. Responses to these questions were grouped thematically. Where interpretive questions arose, the code book was revised to ensure analogous understanding of categories and the two coders re-coded. Inter-rater reliability of at least 90 % for all but one coding category (87 %) was achieved.
Results
Participant data indicating group (case, relative, control), type of cancer, age, gender, and race are included in Table 1. Greater than half the participants were cases and tended to be older and more likely to be female than the relative and control groups. None of the participants self-reported as Hispanic. There were no significant differences between participant demographics (e.g., gender, ethnicity, and case/relative/control) and thematic trends in responses.
The majority of participants endorsed re-consent when the study had changed to a different, but related, health condition (n = 22) and an unrelated health condition (n = 22). Most (n = 19) participants did not think re-consent was necessary when studying the same cancer but a different gene. Of the 22 participants who endorsed the need for re-consent for a different but related health condition, 14 indicated that re-consent should be mandatory and the remaining 7 indicated that it would be desirable, whereas 18 of the 22 who endorsed re-consent for an unrelated health condition indicated that it should be mandatory. Nearly all (n = 27) participants endorsed re-consent when a child achieved his/her age of majority, and the majority of those felt that this should be mandatory (n = 24). Most (n = 19) participants said broad consent would not affect the likelihood that they would participate in a research study; most (n = 18) felt that there were more benefits to using a broad consent than harms. Finally, the majority (n = 22) of participants would not be affected by the researcher or research institution making a profit. Tables 2 and 3 summarize the content analytic findings. Responses analyzed by themes are summarized below.
Re-consent provides the main opportunity for additional and updated study information
The most frequently occurring themes were the opportunity re-consent afforded in conveying updated study information to participants and in ensuring they were informed about the uses of their data (Table 4). The chance for participants to be made aware that their data and samples may be used for additional, follow-up, studies was often cited as a reason that participants would want to be re-consented. This finding held for all scenarios, including studies involving a different, but related, health condition; the same health condition but a different gene; and an unrelated health condition. As participant 27 explained:
“Well, I think it would be a good thing in terms of that way the participant knows that there’s additional research that can be coming out of the effort that they’ve put into this particular research project. It’s kind of something to…let the person know that… ‘Yeah, we’re looking at your data again and we’re looking at it from a different angle, or a different perspective.’”
Even participants who were inclined to participate in additional studies using their data would want to be notified of any new uses of their data.
Participants own their own data and should control or know how data are used
Several participants endorsing re-consent indicated that they expected control of their personal data and felt that this would be facilitated by the re-consent process. For different, but related, health conditions, four participants cited data control and ownership as reasons re-consent was mandatory. For an unrelated health condition, six participants indicated that re-consent was mandatory, also for data control and ownership. However, for a study of the same cancer but a different gene, only one participant indicated that re-consent was mandatory, again because of data control issues.
Generally, when issues concerning the control of personal data were involved, attitudes were firm, even among participants who were inclined to participate in follow-up studies. Participant 4 explained:
“Because each participant is in charge of his or her own body and how it’s used…I think you need to know what kind of research your data is being used for…I probably would say sure go ahead and use it for whatever the second or third thing was, but I wouldn’t want it to just happen without me knowing what was happening with my tissue or blood or whatever it was.”
The nature or extent of the study change determines the need for re-consent
Although being informed was a concern of participants in general, the nature of the changes in study direction was crucial when participants considered whether re-consent was required in specific scenarios. Most participants believed re-consent was needed when the study changed, either to a related health condition or to an unrelated health condition, but not when the study was the same cancer but a different gene. Moving the study away from cancer to an unrelated health condition caused the most concern, with the majority of participants stating that re-consent should be required in those cases. Participant 25 explained:
“Because it’s completely different. It’s not related to the same reason that people agreed to be a participant.”
However, when the study would be for the same cancer but a different gene, participant consensus was that re-consent was not required. Several participants felt that “genetics” implicitly covered all research involving genes. Participant 16 stated:
“I would think genetics is a big umbrella over a lot of little genetic-type things. And therefore that big umbrella covers everything underneath it.”
Participant 4 also indicated that consent for this sort of study change could be assumed:
“Moving from one gene to another—to me—doesn’t seem to be a violation of what you originally agreed to do.”
Minors should be re-consented upon achieving their majority
Participants were nearly unanimous in their endorsement of the need for re-consent when a child became old enough to decide for herself/himself. Participant 21 stated:
“At that point, the child is no longer a child, he’s an adult—at least in the eyes of the law he is. And at that point, he can make—he should make—his own decisions.”
This respect for an adult person’s autonomy was a common theme in the majority of participant responses. Participant 17 explained:
“Because then it’s not in the parents’ hands any more, and they [the child] need to be able to make up their own minds about what they want to do.”
Most participants accept researchers making a profit
The majority of respondents indicated that their willingness to participate in research would not be affected by the researcher or institution profiting from a patent or a license. Participant 24 said:
“More power to you. If you can come up with something and get a patent on it, why would I be deserving of any of that money? I just gave my opinion. I didn’t do any of the research. I didn’t do any of the hard work that it takes to do that.”
Most participants had very down-to-earth views of the financial aspects of research. Participant 26 stated:
“I understand it’s a business world out there, and research institutions need to generate revenue as well.”
However, a minority of participants was wary of money being involved at all (participant 9: “it’s not a money making thing”). Participant 3 explained:
“If it was a big pharma and they’re doing this research to come up with a cure, and then, I don’t know, there’s something about getting money off the research—I think everything should be like Dr. Salk. He gave the polio vaccination to the world.”
Most participants have practical views of broad consent
The use of broad consent might be one way to expedite additional research on already-collected genetic samples. The final two questions in the protocol asked participants to imagine the potential harms and benefits of broad consent and to offer their opinions on whether their willingness to participate in research would be affected by this type of consent. The majority of participants felt that the benefits of broad consent outweighed the harms, emphasizing practicality and the importance of research in their responses but not mentioning individual-level benefits. Participant 30 stated:
“To me, the good far outweighs any potential—I just don’t see the harm in there. So I think that’s fine, I mean it would make so much sense just to do that, and say, ‘You know, this really is what we’re looking at, but you need to understand that if you sign this, it could be used for other things. If you have a problem with that, you don’t want to sign it.”
When re-consent scenarios were discussed, a couple of participants raised the possibility of broad consent unprompted by suggesting that the potential to move beyond the initial study should be included in the original consent. Participant 23 said:
“They could just go ahead and put something at the very beginning of the studies saying that, ‘Look, we may not only use this information, but do you agree also—could we also use this information in a related fashion’ to each participant at the beginning of taking the data…Just do it to begin with and save everybody a whole bunch of time.”
Only a minority of participants expressed doubt as to the benefits for participants when researchers were allowed latitude in decision-making. Participant 12 explained:
“I’d say that that is way too open-ended, and people could run it up the flag pole and see who’s willing to sign it, but…I would become suspicious that the benefit mainly was on their [the researchers’] side, not mine.”
By contrast, the majority of respondents stated that their willingness to participate would not be affected by broad consent, including most of those who enumerated harms or expressed wariness. Some participants talked about their “belief” in the research and wanting to ensure that research endeavors continued. Participant 20 stated:
“I don’t think it would be anything but good…because I believe in the research.”
Potential harms of genetic research are not easily identified
Several participants had difficulty imagining the harms of genetic research in their responses to the question concerning whether re-consent should be required for a follow-up study involving the same cancer but a different gene and in the discussion of harms and benefits of broad consent in genetic research. Even when specifically prompted, participants exhibited difficulty imagining the harms of genetic research, particularly on an individual level. According to participant 18:
“They’re not going to do anything more to him [the participant], and they can’t do anything much for him or to him, once they have it.”
Participant 21 explained:
“I can’t imagine. It’s not like the samples then jump back and give you something. So, I don’t know what the harm could be. At least I don’t see it.”
Discussion
Current debates on the risks and benefits of re-consent for genomic research have one side arguing that re-consent for additional data usage should occur whenever possible and the other side contending that minimal risk studies should not require re-consent, particularly in light of the amount of resources re-consent would consume and the chance that this additional effort would deter new projects, including reduced participation (Trinidad et al. 2011; Forsberg et al. 2011). This study is one of only a few to consider the views of participants on re-consent in genetic studies. These findings are timely and can help inform the debate around several issues that have arisen in discussions around PM, particularly with regard to issues of consent.
Participants exhibited a high level of consensus and clarity regarding which instances should require re-consent. For different, but related, health conditions, most participants felt that re-consent was a “good thing,” and of those, over half indicated re-consent should be mandatory. For an unrelated health condition, a majority felt that re-consent was mandatory. This finding bears out recent research that emphasizes the importance of consent for additional uses of participant data (Willison et al. 2007). In addition, the majority of participants stated that it should be mandatory that children who become adults be re-consented. This mirrors the views of researchers who argue that the genetic data of children should not be shared (e.g., via biobanks) unless they are contacted and consented as adults (Gurwitz et al. 2009). These findings have important implications when assembling the proposed national PM research cohort from existing cohorts and data and indicate that when the research direction has changed, e.g., from cancer to another disease, the majority of participants felt that re-consent is needed.
Most participants agreed that re-consent was not required when a study’s focus moved from one gene to another but the disease remained the same, but did not offer much detail in describing why changing genes seemed negligible. In addition, although several participants were concerned with controlling their data, we found that most participants were unable to view harms as personally relevant within a genetic context (e.g., identifiability). This positive view of genetics is in keeping with attitudes reported in other studies (Henderson et al. 2008). Further research is needed to understand this important issue, particularly as de-identifying data may not protect participants’ (re)identifiability sufficiently (Colditz 2009; El Emam et al. 2011). A recent high-profile study used computational tools and Internet searches to re-identify members of the general population who had contributed to publicly available recreational genetic genealogy databases; it took a single person only 3–7 h to re-identify each pedigree (Gymrek et al. 2013). This finding raised concern, particularly as whole exome and whole genome sequencing becomes the standard in human genetic studies. However, it is not known how participants feel about this issue and whether this potential risk is outweighed by the perceived benefits of participating in research (Trinidad et al. 2010). It has been suggested that a genetic study that promises the confidentiality of genetic data may, through that assurance to participants, invalidate their informed consent (Lunshof et al. 2008). Researchers and IRBs may need to pay increased attention to the use of the term “de-identified,” and (re)consent material might need to be more explicit regarding the limits of de-identification and risk of re-identification.
The importance of re-consent in conveying updated information was expressed by those who said re-consent should almost always occur but also by those who felt it needed to occur in some instances (e.g., a different health condition) but not in others (e.g., same cancer but different gene). If the re-consent process is the only option for participants to receive additional information, then it makes sense that participants would think it mandatory to be re-consented even if they are inclined to participate in the new study. However, re-consent may not be the ideal vehicle to address this expectation. This issue will need increased attention as we move towards PM given that the ultimate goal is to tailor treatments and medical care based largely on genomic information.
Most participants focused on the benefits of broad consent. Participants usually offered only positive statements concerning broad consent, including something that humankind generally might experience in the future (e.g., through scientific advances to improve health) or researchers particularly might have (e.g., through research being made easier). Regarding harms, participants expressed concerns over control of personal data, particularly knowing how their data were being used. These findings are similar to other studies which found that participants did not want genetic information shared publicly without consent and expressed an interest in receiving information and being involved in decisions regarding their own data (Trinidad et al. 2010; McGuire et al. 2008). This is also consistent with two recent studies among US (Platt et al. 2014) and UK adults (Kelly et al. 2015) which found that research subjects favored broad consent if they were provided with sufficient information about the use of the data. Participants exhibited a practical view of research, and most would not be affected by the researcher or institution making a profit. This agrees with a study in which biobank registrants emphasized that commercialization was acceptable with ethical controls to ensure a just use of data (Steinsbekk et al. 2013).
There remains a discussion concerning the use of broad consent (Helgesson 2012). Informed consent issues in the USA are evolving in response to new issues arising from genetic and genomic research, including placing more emphasis on using consent as a vehicle to address potential issues in advance or at the start of a study (e.g., return of individual research results) (Simon et al. 2012). The issue is complex: approaches need to meet participant needs and expectations as well as researchers’ ethical obligations (Knoppers and Lévesque 2011) when no standardized guidelines exist for individual research studies in general and biobanks in particular (Bledsoe et al. 2012). Some argue that for existing biobanked data, re-consent may be impractical and possibly unnecessary if appropriate safeguards are in place regarding de-identification, limiting access to bona fide researchers, ensuring that any additional data uses do not contradict the original consent and that the risk to privacy or harm from breach of privacy is low (Bathe and McGuire 2009).
Proponents of broad consent for biobank research argue that what makes consent informed in the use of broad consent is not that all, or even most, types of future research and their potential harms and benefits can be predicted, but rather, that potential participants (i.e., biobank registrants) understand what broad consent means (Helgesson 2012). This focus on genetic and genomic research consent that emphasizes participant understanding of potential risks and benefits, such as identifiability, is not a new concept or concern (Annas 2001), but recent events demonstrating the potential ease of re-identification may breathe new life into the debate. Understanding explicitly where participant concerns lie is critical to informing the conversation.
Limitations
The main limitation is the lack of generalizability beyond this cohort, which was composed largely of older, non-Hispanic white adults with a history of cancer. Thus, these data were used to inform a survey among a more representative respondent base. While Ewing et al. have shown a significant difference between non-Hispanic whites and African Americans in acceptance of broad consent, we were limited by sample size and unable to stratify by case status or other demographic characteristics (Ewing et al. 2015). Second, the flow of the questions may have affected participant responses. For example, participants were asked to envision the harms and benefits of a broad consent form immediately after being asked if their participation in research would be affected by the researcher or the institution profiting from a patent or license. Consequently, a minority of participants focused on the commercial aspect in their discussion of harms. Finally, questions concerning whether participants would be affected by certain elements (i.e., researcher profiting, use of a broad consent) assessed intention and not actual action.
Conclusions
There were specific scenarios in which the majority of participants felt re-consent was needed (e.g., a significantly different study and the re-consent of a minor achieving majority) and other scenarios where it was not needed (e.g., same disease focus but interrogating a different gene). Among participants in favor of re-consent, it was primarily as a vehicle to get information about the project or to control their data. Results from this study suggest that participants do not interpret harms and benefits in the same way as researchers and IRBs do. Defining the limits of de-identification, so as not to overstate privacy guarantees or “anonymity,” might be particularly important. In order to support research that adheres to scientific research standards, such as reproducibility and mandated data sharing, consent should assume that data may be made public (Ioannidis 2013). However, we currently do not know whether explicitly describing re-identification would cause it to be a significant participant concern. Because most indicated that their willingness to participate in a study would not be affected by the use of broad consent, future research might assess what safeguards biobanks and long-running studies should have in place in order to respect participants’ willingness to abrogate research-related decisions via broad consent (Sheehan 2011). As we move towards PM and consider the use of existing samples and data to populate a new national research cohort, it may be necessary to develop a process that includes all stakeholder feedback about circumstances that would trigger re-consent. Exploring these issues in more detail will help ensure that protections and scientific endeavors are of the highest standard and meet the goals of the PMI, while also respecting participants’ needs as expressed by the participants themselves.
References
Alyass A, Turcotte M, Meyre D (2015) From big data analysis to personalized medicine for all: challenges and opportunities. BMC Med Genomics 8:33
Annas GJ (2001) Reforming informed consent to genetic research. JAMA 286(18):2326–2328
Anton-Culver H, Ziogas A, Bowen D et al (2003) The Cancer Genetics Network: recruitment results and pilot studies. Community Genet 6(3):171–177
Arnason V (2004) Coding and consent: moral challenges of the database project in Iceland. Bioethics 18:27–49
Bathe OF, McGuire AL (2009) The ethical use of existing samples for genome research. Genet Med 11(10):712–715
Bledsoe MJ, Grizzle WE, Clark BJ, Zeps N (2012) Practical implementation issues and challenges for biobanks in the return of individual research results. Genet Med 14(4):478–483
Caulfield T (2007) Biobanks and blanket consent: the proper place of the public good and public perception rationales. King Law J 18:209–226
Colditz GA (2009) Constraints on data sharing: experience from the nurses' health study. Epidemiology 20(2):169–171
Edwards KL, Lemke AA, Trinidad SB et al (2011) Attitudes toward genetic research review: results from a survey of human genetics researchers. Public Health Genomics 14(6):337–345
Edwards KL, Lemke AA, Trinidad SB et al (2012) Genetics researchers' and IRB professionals' attitudes toward genetic research review: a comparative analysis. Genet Med 14(2):236–242
El Emam K, Jonker E, Arbuckle L, Malin B (2011) A systematic review of re-identification attacks on health data. PLoS One 6(12), e28071
Ewing AT, Bollinger E, Tetteyfio E et al (2015) Demographic differences in willingness to provide broad and narrow consent for biobank research. Biopreserv Biobank 13:98–106
Forsberg JS, Hansson MG, Eriksson S (2011) The risks and benefits of re-consent. Science 332(6027):306
Graneheim UH, Lundman B (2004) Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today 24(2):105–112
Gurwitz D, Fortier I, Lunshof JE, Knoppers BM (2009) Research ethics. Children and population biobanks. Science 325(5942):818–819
Gymrek M, McGuire AL, Golan D, Halperin E, Erlich Y (2013) Identifying personal genomes by surname inference. Science 339(6117):321–324
Haga SB, Beskow LM (2008) Ethical, legal, and social implications of biobanks for genetic research. Adv Genet 60:505–544
Hawgood S, Hook-Barnard IG, O’Brien TC, Yamamoto KR (2015) Precision medicine: beyond the inflection point. Sci Transl Med 7:300.PS17
Helgesson G (2012) In defense of broad consent. Camb Q Healthc Ethics 21(1):40–50
Henderson G, Garrett J, Bussey-Jones J, Moloney ME, Blumenthal C, Corbie-Smith G (2008) Great expectations: views of genetic research participants regarding current and future genetic studies. Genet Med 10(3):193–200
Hofmann B (2009) Broadening consent - and diluting ethics? J Med Ethics 35:125–129
Ioannidis JP (2013) Informed consent, big data, and the oxymoron of research that is not research. Am J Bioeth 13(4):40–42
Kelly SE, Spector TD, Cherkas LF et al (2015) Evaluating the consent preferences of UK research volunteers for genetic and clinical studies. PLoS ONE 10:e0118027
Knoppers BM, Lévesque E (2011) Introduction: return of research results: how should research results be handled? J Law Med Ethics 39(4):574–576
Lemke AA, Trinidad SB, Edwards KL, Starks H, Wiesner GL (2010) Attitudes toward genetic research review: results from a national survey of professionals involved in human subjects protection. J Empir Res Hum Res Ethics 5(1):83–91
Lunshof JE, Chadwick R, Vorhaus DB, Church GM (2008) From genetic privacy to open consent. Nat Rev Genet 9(5):406–411
McGuire AL, Hamilton JA, Lunstroth R, McCullough LB, Goldman A (2008) DNA data sharing: research participants' perspectives. Genet Med 10(1):46–53
Novick G (2008) Is there a bias against telephone interviews in qualitative research? Res Nurs Health 31(4):391–398
Overby CA, Tarczy-Hornoch (2013) Personalized medicine: challenges and opportunities for translational bioinformatics. Per Med 10:453–462
Petrini C (2010) "Broad" consent, exceptions to consent and the question of using biological samples for research purposes different from the initial collection purpose. Soc Sci Med 70:217–220
Platt J, Bollinger J, Dvoskin R et al (2014) Public preferences regarding informed concent models for participation in population-based genomic research. Genet Med 16:11–18
Sheehan M (2011) Can broad consent be informed consent? Public Health Ethics 4(3):226–235
Simon C, Shinkunas LA, Brandt D, Williams JK (2012) Individual genetic and genomic research results and the tradition of informed consent: exploring US review board guidance. J Med Ethics 38(7):417–422
Steinsbekk KS, Ursin LO, Skolbekken JA, Solberg B (2013) We're not in it for the money-lay people's moral intuitions on commercial use of 'their' biobank. Med Health Care Philos 16(2):151–162
Tasse AM, Budin-Ljosne I, Knoppers BM, Harris JR (2010) Retrospective access to data: the ENGAGE consent experience. Eur J Hum Genet 18(7):741–745
Trinidad SB, Fullerton SM, Bares JM, Jarvik GP, Larson EB, Burke W (2010) Genomic research and wide data sharing: views of prospective participants. Genet Med 12(8):486–495
Trinidad SB, Fullerton SM, Ludman EJ, Jarvik GP, Larson EB, Burke W (2011) Research practice and participant preferences: the growing gulf. Science 331(6015):287–288
Vaismoradi M, Turunen H, Bondas T (2013) Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci 15(3):398–405
Willison DJ, Schwartz L, Abelson J et al (2007) Alternatives to project-specific consent for access to personal information for health research: what is the opinion of the Canadian public? J Am Med Inform Assoc 14(6):706–712
Acknowledgments
This study involved multiple collaborators, including our valued colleagues enrolled in the Northwest Cancer Genetics Registry for their ongoing participation in and contribution to cancer research; the University of Washington (UW) Department of Epidemiology, the Institute for Public Health Genetics, and the Department of Biomedical Informatics and Medical Education; Boston University, Department of Community Health Sciences; University of Georgia, Department of Communication Studies; Johns Hopkins University, Genetics and Public Policy Center; the National Coalition for Health Professional Education in Genetics; and the University of California, Irvine. The authors also wish to also acknowledge and thank Nirupama Schridhar, Katherine W. Snapinn, Joan Scott, and David Kaufmann for their work contributing to the earlier stages of this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was funded by the National Cancer Institute (grant 1R01CA149051-01A1; KL Edwards, PI.)
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional research boards and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Edwards, K.L., Korngiebel, D.M., Pfeifer, L. et al. Participant views on consent in cancer genetics research: preparing for the precision medicine era. J Community Genet 7, 133–143 (2016). https://doi.org/10.1007/s12687-015-0259-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12687-015-0259-8