Abstract
This study aims to investigate the association of human leukocyte antigen (HLA) class II genes and cytotoxic T lymphocyte-associated antigen-4 (CTLA-4) with autoimmune thyroid diseases in the Lebanese population. A total of 128 patients with autoimmune thyroid disease (55 with Graves’ disease (GD) and 73 with Hashimoto’s thyroiditis (HT)) were typed for HLA DQA1 (0301 and 0501) and DQB1 (0201, 0302, and 0303) and for 49A/G CTLA-4 using PCR-based sequence-specific priming methods. A total of 186 matched controls were typed for the same alleles and compared to the diseased population. Results showed no significant differences in HLA DQB1*0201 or DQB1*0301 allelic frequencies or CTLA-4 polymorphisms between patients and controls. For GD, there was a weak association with HLA DQB1*0302 [34.6% (19 of 55) vs. 21.5% (40 of 186), P = 0.048, odds ratio (OR) = 1.926, confidence interval (CI) = 0.999–3.715] and HLA DQB1*0302-DQA1*0501 haplotype [56.36% (31 of 55) vs. 40.8% (76 of 186), P = 0.042, OR = 1.870, CI = 1.018–3.433]. For HT, the frequencies of DQB1*0302-DQA1*0501 haplotype [28.8% (21of 73) vs. 14.5% (27 of 186), P = 0.008, OR = 2.378, CI = 1.241–4.558] and DQB1*0302-DQA1*0301 haplotype [60.2% (44 of 73) vs. 38.7% (72 of 186), P = 0.002, OR = 2.402, CI = 1.381–4.180] were significantly higher in patients. On the other hand, weak association was found between HT and DQA1*0301 allele [32.9% (24 of 73) vs. 20.9% (39 of 186), P = 0.044, OR = 1.846, CI = 1.011–3.373]. Findings show that DQB1*0302-DQA1*0501 and DQB1*0302-DQA1*0301 haplotypes may play a role in the pathogenesis of HT in the Lebanese population. For the 49A/G CTLA-4 polymorphism, no significant difference was found between patients and controls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autoimmune thyroid diseases (AITD) are the most prevalent autoimmune disorders. They affect up to 5% of the entire population (Szyper-Kravitz et al. 2005; Wang and Crapo 1997). AITD, including Graves’ disease (GD), atrophic myxedema, and Hashimoto’s thyroiditis (HT), encompass a number of conditions that have in common cellular and humoral immune that targets the thyroid gland. They are complex diseases in which susceptibility genes and environmental triggers act together to initiate autoimmune response against the thyroid gland (Weetman 1996). Although environmental agents are important for AITD to develop, studies have shown that almost 80% of its occurrence is due to genetic factors (Brix et al. 2001). Thus, models for the pathogenesis of AITD suggest that each subject has inherited tendency to autoimmunity and that environmental and hormonal factors lead to the development of the disease (Vaidya et al. 2002).
At least seven genes have been found to be associated with AITD, but their extent of association has been variable (Jacobson et al. 2008; Tomer 2010). Among these susceptibility genes, those which appear to be of a major importance are represented mainly by human leukocyte antigen (HLA) and the cytotoxic T lymphocyte-associated antigen-4 (CTLA-4) (Jacobson et al. 2008; Vaidya et al. 2002). The HLA system plays the biggest role in autoimmune disorders (Wiebolt et al. 2010). Disease association studies show that the nature and location of HLA polymorphisms are of major importance (Erlich et al. 1993). The CTLA-4 gene has been one of the most studied genes in relation to autoimmunity (Kavvoura et al. 2007). It is an important co-stimulatory molecule that participates in the interaction between T cells and antigen-presenting cells. CTLA-4 gene which suppresses T cell activation has raised the possibility that mutations altering CTLA-4 expression and/or function results in an exaggerated T cell activation and lead to the development of autoimmunity (Reiser and Stadecker 1996). An association between a common polymorphism at nucleotide 49(A/G) resulting in the substitution of an alanine for a threonine at codon 17 in the signal peptide of the CTLA-4 and AITDs has been reported across populations of different ethnic backgrounds such as Caucasians (Yanagawa et al. 1995), Japanese (Akamizu et al. 2000; Yanagawa et al. 1997), and Koreans (Park et al. 2000).
Clinical experience suggests that thyroid disease is also common in the Lebanese population, but no studies have described the prevalence of thyroid dysfunction in the general population and the association of HLA class II genes and CTLA-4 polymorphism with AITD patients. In this study, we analyzed 186 healthy Lebanese subjects and 128 AITD patients to evaluate the association of the HLA genotypes of DQA1 (0301 and 0501), DQB1 (0201, 0302, and 0303), as well as 49A/G CTLA-4 polymorphism with AITD.
Materials and methods
Sample design
Taking into consideration that Lebanon is a small country with a small population, a total of 1,156 Lebanese adult subjects aging more than 18 years were recruited from different regions, ethnicities, and religious communities proportionally to their distribution in the country. In every region, one village or district was chosen to make a randomly selected sample using population and electoral register. A total of 219 subjects (18.9%) were not available or refused to participate in the study. On the other hand, 162 subjects (14%) reported history of goiter, thyroid diseases, or use of thyroid medication and were excluded from the study. Information about the remaining 775 subjects (67%) (617 females, 158 males) was collected on age, sex, and family history of AITD. Examination of the neck for goiter was also conducted. Serum was frozen for analysis of thyroid antibodies and thyroid-stimulating hormone (TSH). Subjects diagnosed with goiter or who were positive for antimicrosomal and/or antithyroglobulin antibodies or with abnormal TSH value were excluded. A total of 186 subjects (132 females, 54 males) with normal findings were randomly chosen. DNA was extracted from the obtained blood samples and typed for HLA DQA1 (0301 and 0501) and DQB1 (0201, 0302, and 0303) and for 49A/G CTLA-4 polymorphism.
On the other hand, 128 Lebanese patients with AITD (55 with GD and 73 with HT), aged between 13 and 68 years (mean age of 42 years), were recruited from the University Hospital of Hotel-Dieu de France in Beirut, between March 2005 and November 2005. Similar to controls, patients were from different regions and religious backgrounds. GD was diagnosed on the basis of clinical and laboratory evidence of thyrotoxicosis, palpable diffuse goiter, and absence of other causes of thyrotoxicosis such as multinodular goiter. Thyrotoxicosis was identified according to TSH blood levels (TSH <0.1 mIU/l) (De Groot 2005). In addition, most patients had one or more of the following: exophthalmos, positive anti-TSH receptors antibodies, and diffuse isotope distribution on radionuclide scanning. HT was defined by thyroid peroxidase antibody (TPO Ab) >200 UI/ml (Slatosky et al. 2000). HLA DQA1 (0301 and 0501), DQB1 (0201, 0302 and 0303), and 49A/G CTLA-4 polymorphism analyses were performed in all patients and compared to controls.
Analysis of the HLA-DR haplotypes was not performed in this study, since the allocated budget was not sufficient. The study received ethical approval from local ethics committee, and written informed consent was obtained from every participant.
Laboratory methods
TSH was measured with a chemiluminescence immunometric assay (DPC, Immulite, Los Angeles, CA, USA). The normal reference range for the test was 0.4–4 μIU/ml, but we chose 0.1 mIU/l for the lower normal value instead of the laboratory reference range because values between 0.1 and 0.39 mIU/l are generally considered clinically insignificant using this sensitive TSH assay (Hollowell et al. 2002). So, hyperthyroidism (clinically significant and subclinical) was defined for TSH <0.1 mIU/l, and hypothyroidism (clinically significant and subclinical) was defined for TSH >4 mIU/l.
TPO Ab, antithyroid antibodies, and Tg antibodies were all measured using a chemiluminescence immunometric assay (DPC, Immulite, Los Angeles, CA, USA). Each test was considered positive if TPO Ab >30 UI/ml, antithyroid antibodies >9 IU/ml, or Tg antibodies >40 mIU/l. The size of the thyroid gland was determined by inspection and palpation using the WHO 1960 and 1994 palpation criteria (Perez et al. 1960; WHO/UNICEF/ICCIDD 1994).
PCR amplification and analysis
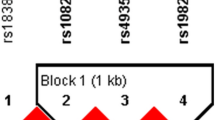
HLA class II genotyping was carried out by PCR amplification with sequence-specific primers followed by restriction fragment length polymorphism (RFLP) and according to analyses reported in the literature (Olerup et al. 1993). 49A/G CTLA-4 polymorphism was analyzed by PCR-RFLP as previously described (Kinjo et al. 2002).
Statistical analysis
Data analysis was performed with SPSS software 13.0 (copyright SPSS, Inc., 1989–2004). Yates' chi-square test was used when necessary. In reference to previously reported data on HLA class II association with AITD, the results in this study were considered significant (with expected frequency of more than 5) with uncorrected P value <0.05. Odds ratio with 95% confidence intervals were calculated as well.
The mean and standard error of the mean for TSH were calculated from logarithmic transformed values. Kolmogorov–Smirnov test was used to assess normality. The median 2.5 and 97.5 percentiles were calculated to generate possible reference limits for TSH from the reference population.
Results
Our reference population included 186 people (132 females, 54 males) aged between 18 and 65 years old (mean age 44.5 ± 12.9 years). We also studied 128 patients with AITD aged between 13 and 68 years old: 73 patients with HT (68 females, 5 males, mean age 44.6 ± 13.4 years) and 55 patients with GD (41 females, 14 males, mean age 40.6 ± 11.4 years). Twenty-six patients had one or more autoimmune diseases associated with their thyroid disease, type 1 diabetes being the most frequent.
Graves’ disease and Hashimoto’s thyroiditis
Allelic distribution of HLA DQA1 and DQB1 genes
The frequencies of DQA1 and DQB1 alleles were compared between the 55 GD patients, 73 HT patients, and 186 controls (Table 1 in the “Appendix”). There were no significant differences for the frequency of DQA1 alleles between GD patients and controls. A weak association was found between GD and HLADQB1*0302 allele [34.6% (19 of 55) vs. 21.5% (40 of 186), P = 0.048, odds ratio (OR) = 1.926, confidence interval (CI) = 0.999–3.715]. Although the frequency of DQA1*0301 was significantly higher in HT patients than in controls, the lower range of the confidence interval is barely greater than 1 which reflects weak association [32.9% (24 of 73) vs. 20.9% (39 of 186), P = 0.044, OR = 1.846, CI = 1.011–3.373]. For the DQB1 alleles, there were no significant differences between HT patients and controls (P > 0.05).
Haplotypes of DQA1*0501 and DQB1
The allelic frequencies in GD patients, HT patients, and controls were also analyzed for the haplotypes of DQB1-DQA1*0501. Weak association was found between GD patients and the allelic frequency of the haplotype DQB1*302-DQA1*0501 [GD patients 56.36% (31of 55) vs. 40.8% (76 of 186), P = 0.042, OR = 1.870, CI = 1.018–3.433]. On the other hand, this haplotype was significantly higher in HT patients than in the controls having more than twice the odds of disease occurrence [28.8% (21of 73) vs. 14.5% (27 of 186), P = 0.008, OR = 2.378, CI = 1.241–4.558]. Also, the allelic frequency of the haplotype DQB1*302-DQA1*0301 was significantly higher in HT patients than in controls [60.2% (44 of 73) vs. 38.7% (72 of 186), P = 0.002, OR = 2.402, CI = 1.381–4.180].
Polymorphism of CTLA-4
The prevalence of 49A/G CTLA-4 polymorphism was compared between each patient group and control group. No difference was found in the distribution of the A or G alleles, nor did the AA, AG, or GG genotypes differ between patients and controls (Table 2 in the “Appendix”).
Discussion
AITD are complex diseases in which susceptibility genes, mainly HLA genes, have been identified to initiate the autoimmune response against the thyroid gland in complex with environmental triggers (Kavvoura et al. 2007). There are at least two hypotheses concerning the existence of an association between an allele and a disease: (1) the allele itself is the genetic variant causing an increased risk for the disease and (2) the allele itself is not causing the disease but rather a gene in linkage disequilibrium with it. In our study, we focused on analyzing the association of HLA DQA1 and DQB with AITD in the Lebanese population. To our knowledge, this is the first report to test the association between HLA alleles and AITD in our population. For GD, we observed weak association with HLA DQB1*0302. In agreement with other studies, no association was found between HLA DQB1*0201 and HLA DQB1*0303 and GD (Zamani et al. 2000; Chen et al. 2000) (Table 1 in the “Appendix”). Also, weak association was found between GD and DQB1*0302-DQA1*0501 haplotype, where the confidence interval was barely greater than one (P = 0.042, OR = 1.870, CI = 1.018–3.433). Studies suggest that susceptibility to GD associated with inheritance of a specific HLA class II gene is mainly due to the influence of HLA molecule–thyroid-stimulating hormone receptor peptide complex on the T cell. Several studies have reported the association of GD with DQA1*05 where it was considered a susceptibility marker for GD. Indeed DQA1*05 has been associated with GD in Latvians and Brazilians (Marga et al. 2001; Maciel et al. 2001). However, it was not found to be associated with GD in the Greek population (Philippou et al. 2001) or in African-American patients (Yanagawa and De Groot 1996; Ofosu et al. 1996). In our study, no association was found between DQA1*05 and GD patients (Table 1 in the “Appendix”). Taken together, these data suggest that neither one of the studied alleles is susceptible to GD in the Lebanese patients. As suggested by Chen et al. (2000), the discordance of the results among different studies may be due to the complex interaction of HLA molecules with environmental factors, to initiate the pathogenic process of the disease.
We also studied the distribution of HLA DQAl and DQB alleles in patients with HT to analyze the HLA-linked genetic factors for HT in the Lebanese population. In contrast to the results of the study done by Wan et al. (1995) on 71 Japanese patients with HT, our findings revealed weak association between HT and HLA DQA1*0301. Our results also revealed no relation between HT and DQB1*303 or DQB1*0201 (Table 1 in the “Appendix”). These findings are almost similar to the study done by Hunt et al. (2001) on 77 UK patients that showed only a weak relation between HT and DQB1*303. Data on HLA haplotypes and their association with HT have been less definitive than those on GD (Vaidya et al. 2002). In addition, there are no consistency between the different studies reported on HLA association with HT, such as HLA-DQw7 in English Caucasians (Tandon et al. 1991), HLA-DRB1*0405 in Greek population (Kokaraki et al. 2009), HLA-DRw53 in Japanese (Honda et al. 1989), and HLA-DR9 in Chinese (Hawkins et al. 1987). In our study, when the frequencies of HLA DQB1-DQA1 were compared between patients and controls, positive association was found with the haplotypes DQB1*0302-DQA1*0501 (P = 0.008, OR = 2.378, CI = 1.241–4.558) and DQB1*0302-DQA1*0301 (P = 0.002, OR = 2.402, CI = 1.381–4.180). Although the mentioned haplotypes where found to be significantly associated with HT, neither one of the alleles were directly related to the disease. This agrees with what was previously mentioned by Petrone et al. (2001) that the HLA-linked factor is more complex than a one-locus model and that the combination of alleles could lead to increasing the risk of disease incidence.
CTLA-4 polymorphisms have been widely examined for their associations with AITD. In this study, we analyzed the 49A/G CTLA-4 polymorphism in a sample of Lebanese patients as well. Our findings reveal no association between CTLA-4 and the discussed AITDs. Also, no difference was found in the distribution of the A and G alleles, nor did the AA, AG, or GG genotypes differ between patients and controls (Table 2 in the “Appendix”). Our findings in this respect are similar to that reported on studies done on small samples of Tunisian and Japanese populations (Maalej et al. 2001; Sakai et al. 2001). In the available literature, studies on the polymorphism of CTLA4 exon1 A49G have shown conflicting results. Indeed, some studies disagree with our findings and suggest significant associations with GD and HT for both 49A/G and CT60G/A (Chistiakov and Turakulov 2003; Kavvoura et al. 2007; Furugaki et al. 2004) while others suggest that CTLA4 leads to the production of thyroid autoantibodies but it does not contribute to AITD (Tomer et al. 2001).
Few years back, an association between 49A/G CTLA-4 polymorphism and a small group of Lebanese patients with GD was reported. The authors investigated the polymorphism in 34 patients and in 38 healthy controls and concluded that the G allele was associated with the disease (Nakkash-Chmaisse et al. 2004). As compared to our study, the sample size was much smaller. Moreover, the 95% confidence interval for the odds ratio for the association between the G allele frequency and GD had a lower limit of 1.0, which indicates a weak association.
In conclusion, our results suggest that the haplotypes DQB1*0302-DQA1*0501 and DQB1*0302-DQA1*0301 may play a role in the pathogenesis of HT in the Lebanese population. On the other hand, weak association was found between HLA DQB1*0302, DQA1*0501, and DQA1*0301 alleles and AITD whereas no significant difference was found between patients and controls regarding the 49A/G CTLA-4 polymorphism.
AITDs are the most common autoimmune disorders in which studies are slowly progressing toward the identification of their susceptibility genes. This hopefully will help us fully understand the underlying mechanism which in turn will light the way for some new therapeutic interventions.
References
Akamizu T, Sale MM, Rich SS, Hiratani H, Noh JY, Kanamoto N, Saijo M, Miyamoto Y, Saito Y, Nakao K, Bowden DW (2000) Association of autoimmune thyroid disease with microsatellite markers for the thyrotropin receptor gene and CTLA-4 in Japanese patients. Thyroid 10:851–858
Brix TH, Kyvik KO, Christensen K, Hegedus L (2001) Evidence for a major role of heredity in Graves’ disease: a population-based study of two Danish twin cohorts. J Clin Endocrinol Metab 86:930–934
Chen QY, Nadell D, Zhang XY, Kukreja A, Huang YJ, Wise J, Svec F, Richards R, Friday KE, Vargas A, Gomez R, Chalew S, Lan MS, Tomer Y, Maclaren NK (2000) The human leukocyte antigen HLA DRB3*020/DQA1*0501 haplotype is associated with Graves’ disease in African Americans. J Clin Endocrinol Metab 85:1545–1549
Chistiakov DA, Turakulov RI (2003) CTLA-4 and its role in autoimmune thyroid disease. J Mol Endocrinol 31:21–36
De Groot LJ (2005) Diagnosis and treatment of Graves’ disease. In: The thyroid and its diseases. www.thyroidmanager.org/Chapter11/11-frame.htm. Accessed 4 Oct 2011
Erlich H, Bugawan T, Begovich A, Scharf S (1993) Analysis of HLA class II polymorphism using polymerase chain reaction. Arch Pathol Lab Med 117:482–485
Furugaki K, Shirasawa S, Ishikawa N, Ito K, Ito K, Kubota S, Kuma K, Tamai H, Akamizu T, Hiratani H, Tanaka M, Sasazuki T (2004) Association of the T-cell regulatory gene CTLA4 with Graves’ disease and autoimmune thyroid disease in the Japanese. J Hum Genet 49:166–168
Hawkins BR, Lam KS, Ma JT, Wang C, Yeung RT (1987) Strong association between HLA DRw9 and Hashimoto's thyroiditis in southern Chinese. Acta Endocrinol (Copenh) 114:543–546
Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, Braverman LE (2002) Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 87:489–499
Honda K, Tamai H, Morita T, Kuma K, Nishimura Y, Sasazuki T (1989) Hashimoto's thyroiditis and HLA in Japanese. J Clin Endocrinol Metab 69:1268–1273
Hunt PJ, Marshall SE, Weetman AP, Bunce M, Bell JI, Wass JA, Welsh KI (2001) Histocompatibility leucocyte antigens and closely linked immunomodulatory genes in autoimmune thyroid disease. Clin Endocrinol (Oxf) 55:491–499
Jacobson E, Huber A, Tomer Y (2008) The HLA gene complex in thyroid autoimmunity: from epidemiology to etiology. J Autoimmun 30:58–62
Kavvoura FK, Akamizu T, Awata T, Ban Y, Chistiakov DA, Frydecka I, Ghaderi A, Gough SC, Hiromatsu Y, Ploski R, Wang PW, Ban Y, Bednarczuk T, Chistiakova EI, Chojm M, Heward JM, Hiratani H, Juo SH, Karabon L, Katayama S, Kurihara S, Liu RT, Miyake I, Omrani GH, Pawlak E, Taniyama M, Tozaki T, Ioannidis JP (2007) Cytotoxic T-lymphocyte associated antigen 4 gene polymorphisms and autoimmune thyroid disease: a meta-analysis. J Clin Endocrinol Metab 92:3162–3170
Kinjo Y, Takasu N, Komiya I, Tomoyose T, Takara M, Kouki T, Shimajiri Y, Yabiku K, Yoshimura H (2002) Remission of Graves' hyperthyroidism and A/G polymorphism at position 49 in exon 1 of cytotoxic T lymphocyte-associated molecule-4 gene. J Clin Endocrinol Metab 87:2593–2596
Kokaraki G, Daniilidis M, Yiangou M, Arsenakis M, Karyotis N, Tsilipakou M, Fleva A, Gerofotis A, Karadani N, Yovos JG (2009) Major histocompatibility complex class II (DRB1*, DQA1*, and DQB1*) and DRB1*04 subtypes’ associations of Hashimoto’s thyroiditis in a Greek population. Tissue Antigens 73:199–205
Maalej A, Bougacha N, Rebai A, Bellassouad M, Ayadi-Makni F, Abid M, Jouida J, Makni H, Ayadi H (2001) Lack of linkage and association between autoimmune thyroid diseases and the CTLA-4 gene in a large Tunisian family. Hum Immunol 62:1245–1250
Maciel LM, Rodrigues SS, Dibbern RS, Navarro PA, Donadi EA (2001) Association of the HLA-DRB1*0301 and HLA-DQA1*0501 alleles with Graves' disease in a population representing the gene contribution from several ethnic backgrounds. Thyroid 11:31–35
Marga M, Denisova A, Sochnev A, Pirags V, Farid NR (2001) Two HLA DRB 1 alleles confer independent genetic susceptibility to Graves disease: relevance of cross-population studies. Am J Med Genet 102:188–191
Nakkash-Chmaisse H, Makki RF, Abdelhamid E, Fakhoury H, Salti NN, Salti I (2004) CTLA-4 gene polymorphism and its association with Graves' disease in the Lebanese population. Eur J Immunogenet 31:141–143
Ofosu MH, Dunston G, Henry L, Ware D, Cheatham W, Brembridge A, Brown C, Alarif L (1996) HLA-DQ3 is associated with Graves' disease in African-Americans. Immunol Invest 25:103–110
Olerup O, Aldener A, Fogdell A (1993) HLA-DQB1 and -DQA1 typing by PCR amplification with sequence-specific primers (PCR-SSP) in 2 hours. Tissue Antigens 41:119–134
Park YJ, Chung HK, Park DJ, Kim WB, Kim SW, Koh JJ, Cho BY (2000) Polymorphism in the promoter and exon 1 of the cytotoxic T lymphocyte antigen-4 gene associated with autoimmune thyroid disease in Koreans. Thyroid 10:453–459
Perez C, Scrimshaw NS, Munoz JA (1960) Technique of endemic goitre surveys. In: Endemic goiter, Geneva. Monogr Ser World Health Organ. WHO, Geneva, pp 369–383
Petrone A, Giorgi G, Mesturino CA, Capizzi M, Cascino I, Nistico L, Osborn J, Di Mario U, Buzzetti R (2001) Association of DRB1*04-DQB1*0301 haplotype and lack of association of two polymorphic sites at CTLA-4 gene with Hashimoto's thyroiditis in an Italian population. Thyroid 11:171–175
Philippou G, Krimitzas A, Kaltsas G, Anastasiou E, Souvatzoglou A, Alevizaki M (2001) HLA DQA1*0501 and DRB1*0301 antigens do not independently convey susceptibility to Graves' disease. J Endocrinol Invest 24:88–91
Reiser H, Stadecker MJ (1996) Costimulatory B7 molecules in the pathogenesis of infectious and autoimmune diseases. N Engl J Med 335:1369–1377
Sakai K, Shirasawa S, Ishikawa N, Ito K, Tamai H, Kuma K, Akamizu T, Tanimura M, Furugaki K, Yamamoto K, Sasazuki T (2001) Identification of susceptibility loci for autoimmune thyroid disease to 5q31–q33 and Hashimoto’s thyroiditis to 8q23–q24 by multipoint affected sib-pair linkage analysis in Japanese. Hum Mol Genet 10:1379–1386
Slatosky J, Shipton B, Wahba H (2000) Thyroiditis: differential diagnosis and management. Am Fam Physician 61(1047–1052):1054
Szyper-Kravitz M, Marai I, Shoenfeld Y (2005) Coexistence of thyroid autoimmunity with other autoimmune diseases: friend or foe? Additional aspects on the mosaic of autoimmunity. Autoimmunity 38:247–255
Tandon N, Zhang L, Weetman AP (1991) HLA associations with Hashimoto's thyroiditis. Clin Endocrinol (Oxf) 34:383–386
Tomer Y (2010) Genetic susceptibility to autoimmune thyroid disease: past, present, and future. Thyroid 20:715–725, Review
Tomer Y, Greenberg DA, Barbesino G, Concepcion E, Davies TF (2001) CTLA-4 and not CD28 is a susceptibility gene for thyroid autoantibody production. J Clin Endocrinol Metab 86:1687–1693
Vaidya B, Taylor P, Pearce S (2002) The genetics of autoimmune thyroid disease. J Clin Endocrinol Metab 87(12):5385–5397
Wan XL, Kimura A, Dong RP, Honda K, Tamai H, Sasazuki T (1995) HLA-A and -DRB4 genes in controlling the susceptibility to Hashimoto's thyroiditis. Hum Immunol 42:131–136
Wang C, Crapo LM (1997) The epidemiology of thyroid disease and implications for screening. Endocrinol Metab Clin North Am 26:189
Weetman AP (1996) Chronic autoimmune thyroiditis. In: Braverman LE, Utiger RD (eds) Werner and Ingbar’s the thyroid. Lippincott-Raven, Philadelphia, pp 738–748
WHO/UNICEF/ICCIDD (1994) Indicators for assessing iodine deficiency disorders and their control through salt iodization. WHO/NUT/94.6. WHO, Geneva
Wiebolt J, Koeleman BP, van Haeften TW (2010) Endocrine autoimmune disease: genetics become complex. Eur J Clin Invest 40:1144–1155
Yanagawa T, De Groot LJ (1996) HLA class II associations in African-American female patients with Graves’ disease. Thyroid 6:37–39
Yanagawa T, Hidaka Y, Guimaraes V, Soliman M, De Groot LJ (1995) CTLA-4 gene polymorphism associated with Graves' disease in a Caucasian population. J Clin Endocrinol Metab 80:41–45
Yanagawa T, Taniyama M, Enomoto S, Gomi K, Maruyama H, Ban Y, Saruta T (1997) CTLA4 gene polymorphism confers susceptibility to Graves' disease in Japanese. Thyroid 7:843–846
Zamani M, Spaepen M, Bex M, Bouillon R, Cassiman JJ (2000) Primary role of the HLA class II DRB1*0301 allele in Graves disease. Am J Med Genet 95:432–437
Acknowledgments
We thank the Lebanese Council for financial support.
Conflict of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Farra, C., Awwad, J., Fadlallah, A. et al. Genetics of autoimmune thyroid disease in the Lebanese population. J Community Genet 3, 259–264 (2012). https://doi.org/10.1007/s12687-012-0085-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12687-012-0085-1