Abstract
Objectives
Mindfulness-based stress reduction (MBSR) enhances short-term psychological health in clinical and non-clinical samples, whereas studies examining long-term effects are scarce. This study examined whether the effects of a 7-week MBSR programme on mental health persisted at 2- and 4-year follow-up and explored possible mechanisms of effect.
Methods
In a two-site randomised controlled trial, 288 medical and psychology students were allocated to an MBSR intervention (n = 144) or a no-treatment control group (n = 144). During the 4-year follow-up period, the MBSR group was offered 90-min booster sessions semi-annually. The primary outcome measures were mental distress (General Health Questionnaire (GHQ)) and subjective well-being (SWB); these were measured at baseline (T0) and post-intervention follow-up at 1 month (T1), 2 years (T1) and again at 4 years (T3). Secondary outcomes included coping, mindfulness and meditation practice.
Results
At 4-year follow-up, the MBSR group showed significantly better scores on mental distress, mindfulness, avoidance coping and problem-focused coping (Cohen’s d = 0.23–0.42). Meditation practice positively predicted long-term mindfulness scores. Short-term effects in mindfulness scores mediated long-term intervention effects in mental distress and coping. However, reversed mediation was also observed (i.e. changes in outcome mediating long-term mindfulness scores), and this indicates that initial changes in outcome and mindfulness are intrinsically intertwined and may both influence long-term effects. Small post-intervention effects on well-being and seeking social support did not persist at follow-up.
Conclusions
MBSR fostered enduring effects on mental distress and coping in medical and psychology students 4 years post-intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mindfulness involves the coalescence of present-moment attention and a particular set of attitudes including acceptance, equanimity, kindness and tolerance (Grossman 2015). Mindfulness has been conceptualised as a natural disposition that can be enhanced through practise (Baer 2011). Mindfulness practice aims to increase awareness of habitual patterns of thought, emotion and behaviour. This awareness may enhance emotion regulation and adaptive coping, strengthen self-insight and value clarification and, conversely, decrease negative cognitive and emotional reactivity (Brown et al. 2007; Shapiro et al. 2006; Teasdale et al. 2000). The assumption that these benefits exert a potentially life-long impact on mental health and well-being (Kabat-Zinn 2005) is addressed in the current study of long-term effects of mindfulness training.
In both clinical and non-clinical samples, such as those including healthcare professionals and trainees, mindfulness-based interventions (MBIs) have demonstrated multidimensional short-term health benefits, such as increased well-being and reduced depression, anxiety and burnout (Burton et al. 2016; Gotink et al. 2015; Goyal et al. 2014; Khoury et al. 2015). Further, increased mindfulness improves the way in which people regulate negative affect and stress. Laboratory studies have shown increases in willingness to experience aversive stimuli and decreases in the intensity and negative valence of emotional responses towards stressors, following brief mindfulness exercises (Arch and Craske 2006). Similarly, short-term MBI trials have shown increases in approach coping and decreases in avoidance coping in both clinical and non-clinical samples (Berghmans et al. 2012; Cousin and Crane 2016; Witek-Janusek et al. 2008).
To date, few studies have sought to determine whether such short-term health benefits endure. Some reviews indicated that reductions in depression and anxiety persisted, albeit with a follow-up period of only 3–6 months (Goyal et al. 2014; Hofmann et al. 2010). In non-clinical samples (e.g. students), a few mindfulness studies involving 1-year follow-up periods showed persistent effects on positive psychological outcomes, such as relaxation, empathy and mindfulness (Amutio et al. 2015; Malarkey et al. 2013; Shapiro et al. 2011), but not stress-related outcomes. In clinical samples, some randomised controlled trials (RCTs) have demonstrated persistent MBI effects on mental distress and coping over 2 years (Chien and Thompson 2014; Henderson et al. 2012; Meadows et al. 2014). However, one review (de Vibe et al. 2017) indicated a general decay of effects over 1–2 years, and this was supported by subsequent studies (Fjorback et al. 2013; Henderson et al. 2012; Shapiro et al. 2011). Unfortunately, the interpretation of promising long-term (i.e. 3–4 years) effects of mindfulness-based stress reduction (MBSR) for people with fibromyalgia, chronic pain or anxiety symptoms (Grossman et al. 2007; Kabat-Zinn et al. 1987; Miller et al. 1995) is limited by the use of uncontrolled study designs. Therefore, it is unsurprising that most reviews (Bohlmeijer et al. 2010; Khoury et al. 2013) have suggested a need for longitudinal studies to further the field. Accordingly, the present study aimed to contribute to the fulfilment of this need.
Another gap in current knowledge involves the question as to whether any of the enduring health benefits of mindfulness interventions are attributable to enhancement of mindfulness skills. A recent meta-analysis (Gu et al. 2015) showed moderate but consistent evidence for mindfulness as a mediator of the effects of MBIs on psychological health. Another review (van der Velden et al. 2015) found that, in two of three studies, mindfulness mediated the effect of mindfulness-based cognitive therapy (MBCT). The establishment of a timeline, whereby a change in the mediator temporally precedes a change in the outcome, is a key criterion for drawing inferences about causal mechanisms (Kazdin 2007). Most studies have failed to establish a timeline, because of the use of a pre-post intervention design, whereby the presumed mediator (i.e. mindfulness) and outcome (i.e. mental health) are assessed simultaneously (Gu et al. 2015). Those that established a timeline (Baer et al. 2012; Bergen-Cico et al. 2013; Snippe et al. 2015) reported that changes in dispositional mindfulness assessed during an 8-week MBSR intervention mediated post-intervention effects on mental health. However, this research was limited by the short duration of their study periods (2 months). Thus far, only one study (Kuyken et al. 2010) has used a longer timeline (15 months) and reported that pre-post changes in mindfulness and self-compassion were significant mediators of the long-term effects of MBCT on depressive symptoms. By including a 48-month follow-up period with an intermediate 4-month assessment, the present study aims to further the field regarding possible long-term mechanisms of change.
Finally, questions remain regarding the role of meditation practice in obtaining the beneficial effects of MBIs. In influential mindfulness approaches, such as MBSR and MBCT, meditation and mindfulness practice within and between sessions represent an essential programme component. However, reviews of short-term outcome studies range from indicating a positive relationship between meditation practice and outcome (Gotink et al. 2015), to failing to detect or remaining inconclusive about such a relationship (de Vibe et al. 2017; Eberth and Sedlmeier 2012; Vettese et al. 2009).
In summary, the present study aimed to increase our knowledge regarding the long-term effects of MBIs and possible causal relationships between mindfulness training, negative and positive mental health dimensions and long-term use of coping strategies. To accomplish this, we used longitudinal data from a two-centre RCT examining the efficacy of a 7-week MBSR intervention for medicine and psychology students (de Vibe et al. 2013). The 1-month post-treatment results demonstrated that the intervention decreased mental distress and increased SWB and the non-reactivity mindfulness facet, and that meditation practice predicted levels of mental distress and dispositional mindfulness (de Vibe et al. 2013). Moreover, intervention effects were observed for both approach and avoidance coping strategies (Halland et al. 2015).
In the current study, we examined the intervention’s long-term impact on mental distress and SWB, which were primary outcomes, and on dispositional mindfulness and coping, which were secondary outcomes. In addition, we studied mechanisms of change, notably dispositional mindfulness as a mediator of long-term effects, as well as the role of mindfulness meditation practice (i.e. frequency and duration) as a predictor of long-term intervention effects.
Method
Participants
Of the 704 eligible first- and second-year medical and clinical psychology students from two Norwegian universities, 288 (mean age 24 years; 219 women; 176 medical students and 112 psychology students) participated in the study during 2009 and 2010, with 144 allocated to the MBSR intervention group and 144 to the no-treatment control group.
Procedures
All students continued their academic studies as scheduled. The investigators were blind to the group allocation, as a technician who was not otherwise involved in the study ran a computer randomisation programme and concealed allocation until baseline measurements had been collected. Data were collected at baseline and 1 month and 2 and 4 years after the intervention (T0, T1, T2 and T3, respectively). At each data collection, students received a book voucher of $50 in value for their participation. Details regarding the procedure, power analyses and baseline characteristics are described elsewhere (de Vibe et al. 2013). The study protocol is available on Clinicaltrials.gov (NCT00892138).
Programme Description
Interviews with medical students in the design phase of the project revealed that the time commitment of the original MBSR programme (Kabat-Zinn 2005) was perceived too extensive due to busy study schedules, hence representing a barrier to participation. Thus, the MBSR programme was modified in duration (reduced from 8 to 7 weeks) and intensity (reduced from 2.5-h sessions to 1.5-h sessions and from 45 to 20–30 min of recommended home-based MBSR practice). A full day of mindfulness practice in week 7 was retained. The intervention is described in de Vibe et al. (2013). During the 4-year follow-up period, students in the intervention group were invited to participate in optional 1.5-h mindfulness booster sessions biannually, consisting of mindfulness practice (i.e. sitting or walking meditation, body scan, yoga) and group dialogue. The 7-week MBSR programme and the booster sessions were held at the university campus outside normal lecture hours.
Measures
The 12-item General Health Questionnaire (GHQ) was used to assess general levels of mental distress experienced during the preceding 2 weeks (Goldberg and Williams 1988). The four response categories included 0 (more than usual), 1 (the same as usual), 2 (less than usual) and 3 (much less than usual). Total scores range from 0 (no distress) to 36 (Goldberg and Williams 1988). The Norwegian version has demonstrated good psychometric properties in university students (Nerdrum et al. 2006). Cronbach’s α was .90 in our sample.
Subjective well-being (SWB) was measured using four items (Moum et al. 1990). In accordance with consensus regarding essential well-being dimensions (Røysamb et al. 2002), SWB assessment included items measuring cognitive life satisfaction, positive affect (happy and strong) and negative affect (unhappy and tired). Higher scores reflect increased SWB. The scale has demonstrated good psychometric properties, and construct validity was indicated via strong correlation with the Satisfaction With Life Scale in a student sample (Røysamb et al. 2002) and Cronbach’s α of .81 in the present sample.
Coping was measured using the 42-item Ways of Coping Checklist, which contains five coping dimensions ‘problem-focused coping’, ‘seeking social support’, ‘self-blaming’, ‘avoidance’ and ‘wishful thinking’ (Vitaliano et al. 1984). The scale has been shown to predict mental health and subjective well-being in Norwegian medical students (Kjeldstadli et al. 2006). Problems in replicating the original factor structure (Edwards and Baglioni 1993; Kjeldstadli et al. 2006) prompted the use of principal components factor analysis for our dataset. This analysis justified retaining only three components. The first, ‘problem-focused coping’ (PFC) (α = .79), consisted of 14 items related to cognitive coping (i.e. identifying new ways of looking at the situation and benefit finding) and active problem solving. The second, ‘seeking social support’ (α = .86), consisted of nine items related to seeking help and advice, including three reverse-scored items pertaining to hiding one’s feelings and avoiding social contact. The third, ‘avoidance-focused coping’ (AFC) (α = .82), comprised 17 items related to blaming oneself, wishful thinking and avoidance.
Mindfulness was measured using the 39-item Five Facet Mindfulness Questionnaire (FFMQ), in which four facets contain eight items each, and one facet contains seven items. The five response categories range from 1 (never or very seldom true) to 5 (very often or always true). Higher scores indicate increased mindfulness. The psychometric properties of the scale are good (Baer et al. 2006), and the questionnaire has been validated in a Norwegian student population (Dundas et al. 2013). The facets and their corresponding Cronbach’s α’s in the current study were as follows: ‘observing’ (.78), ‘describing’ (.89), ‘acting with awareness’ (.88), ‘non-judging of inner experience’ (.92) and ‘non-reactivity to inner experience’ (.73).
Student compliance was measured according to class attendance and the extent of home-based mindfulness practice. Attendance was represented by the number of classes attended (0–7). Two questions were used to measure the frequency (six categories, with responses provided using a scale ranging from 0 [never] to 5 [daily]) and duration (six categories, with responses provided using a scale ranging from 0 [0 min] to 5 [> 45 min]) of formal mindfulness practice during the preceding 4 weeks.
Data Analyses
We used SPSS 22 for all statistical analyses. Possible baseline group differences in continuous and dichotomous variables were examined using Student’s t and chi-square tests, respectively.
Treatment effects were examined via mixed model regression analysis, using an identity covariance matrix. Dependence between measurement occasions was adjusted for by estimating a variance component for the random intercept factor. Standard errors were estimated using the restricted maximum likelihood function. Hypothesised group differences at specified time points were examined using least square differences as planned comparisons. The baseline score was included as a covariate to reduce statistical noise and increase statistical power in the RCT design (Egbewale et al. 2014). The fixed Group factor (treatment vs. control) represented the overall treatment effect; the fixed Time factor represented the change in outcomes over time; and the interaction (Group × Time) represented differential change between groups. In the final analysis, gender was included as a fixed factor and allowed to interact with the Group and Time, to facilitate examination of gender-specific effects. The significance level was set at p < .05. The duration and frequency of mindfulness practice were measured in the same manner, to allow examination of the effects of Group and Time. As duration and frequency of practicing mindfulness may predict outcomes, these items were also added as factors in the final analyses of primary and secondary outcomes and allowed to interact with Group and Time. Covariates included age, study site (coincident with instructor effects), study field (medicine vs. psychology) and student class and were excluded from the model in a backward fashion if non-significant. The size of the treatment effects is reported as Cohen’s d for between-groups effects. Effect sizes were defined as small (d = .2), medium (d = .5) and large (d = .8), consistent with Cohen’s (1988) recommendations. The mixed model analysis has been recommended in longitudinal clinical trials because it provides a natural way to deal with missing values or drop outs (Chakraborty and Gu 2009). Mixed models without any ad hoc imputation have been found to provide more power than mixed models with missing values imputed (Chakraborty and Gu 2009) do, and no imputation was performed. Mixed models handle missing data under the assumption that data are ‘missing at random’ or ‘missing completely at random’ (MCAR) (Twisk 2006). Little’s MCAR test and Student’s t test were performed to determine whether the data met this assumption.
Short-term changes in dispositional mindfulness scores were examined as mediators of the observed long-term intervention effects. To ensure that the analytical procedure was as parsimonious as possible, we used only the total FFMQ score as a mediator. The longitudinal design implied a temporal sequence consisting of group randomisation (T0 group), pre-post change in mindfulness caused by the intervention (FFMQ scores at T1) and long-term outcome (e.g. GHQ at T2-T3). To investigate the possibility of reversed causality (Kazdin 2007), pre-post change in outcomes (e.g. GHQ scores at T1) was examined as mediators of long-term effects in mindfulness (FFMQ scores at T2-T3). Data collected subsequent to the intervention were adjusted for baseline observations, in accordance with Roth and MacKinnon (2013) recommendations for longitudinal mediation analysis. Therefore, baseline scores for outcome and mediator variables were included as covariates (Lubans et al. 2008). Mediation was deemed present if the indirect coefficient (Group X Mediator) was statistically significant. The proportion of the variance explained by the mediator was calculated as the ratio of the indirect effect to the total effect. Use of this traditional mediation effect-size measure has been recommended for mediation models in which indirect and direct effects occur in the same direction (Wen and Fan 2015). The analysis was performed using the PROCESS procedure for SPSS (Hayes 2013). Bias-corrected 95% confidence intervals (CIs) were estimated for the indirect effects, using bootstrapping with 10,000 resamples. We repeated the mediation analyses after excluding participants in the treatment group who had received an insufficient dose of treatment (Kazdin 2007), defined according to the MBSR literature as attendance at < 4 sessions (Teasdale et al. 2000).
Results
Descriptive statistics for baseline data are shown in Table 1. The randomisation procedure was effective, as no outcome measures or demographic variables showed a significant group difference, with the exception of gender, which indicated that the number of men allocated to the control group was significantly higher relative to that allocated to the intervention group (N = 43 vs. 26). As men displayed significantly lower scores for baseline mental distress (t = 2.85, p < .01) and the ‘observing’ mindfulness facet (t = 2.27, p < .05), relative to those observed in women, gender was included as a variable in the effect analyses, showing no significant interactions involving gender.
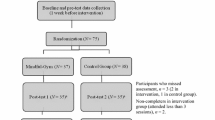
Study Flow, Attrition and Comparisons Between Completers and Non-completers
Figure 1 illustrates the study flow chart. Dropout rates for T1, T2 and T3 were 3%, 19% and 32%, respectively. Student’s t tests revealed that baseline outcome measures did not differ significantly between dropouts and completers at T3. Dropouts from the intervention group showed higher levels of mental distress and lower levels of mindfulness at T2 and lower adherence to mindfulness practice at T1 relative to that observed in completers (p values ranged from .02 to .05). Missing value analysis, performed using Little’s MCAR test to examine primary and secondary outcome measures (GHQ, SWB, coping scales and FFMQ scores), indicated no statistically reliable deviation from randomness, χ2 = 118, df = 100, p = .104.
Intervention Effects
All covariates, including study site, study topic (medicine vs. psychology), study class and age, were omitted, as their effects were non-significant.
Mental Distress/GHQ
The intervention improved mental distress significantly (Group F1, 263 = 24.20, p < .001). A significant Group × Time interaction (F2, 468 = 5.01, p = .007) indicated a decrease in the intervention effect over time. Planned comparisons revealed a relatively large effect at T1 (F1, 657 = 36.42, p < .000, d = .73), and smaller effects at T2 (F1, 674 = 6.13, p = .014, d = .32) and T3 (F1, 689 = 2.81, p = .094, d = .24). A non-significant decrease in mental distress in the control group at T3 provided a partial explanation for the decline in effects. Within-group effects for the intervention group remained significant from T0 to T2 and T3 (p > .01). Effect sizes and p values are presented in Table 2.
SWB
The intervention did not exert a significant long-term effect on subjective well-being. A moderate size effect was observed at T1(F1, 602 = 13.72, p = .000, d = .46), decreasing to non-significance at T2 and T3.
Coping, Mindfulness and Intervention Compliance
Effect sizes and p values are presented in Table 3. Two covariates (study topic and age) were significant predictors of mindfulness (i.e. total FFMQ score), indicating increased mindfulness scores in older students and those studying psychology (p < .05). Age was a significant predictor of avoidance-focused coping (AFC) (p < .05); avoidance-focused coping was more prevalent in younger, relative to older, students. Study site was a significant predictor of problem-focused coping (PFC) (p = .05) and the effect observed in South Norway (Oslo) was stronger relative to that observed in North Norway (Tromsø), indicating a potential teacher effect on this coping measure. Effect analyses were adjusted for these differences.
Coping Strategies
The effect of the intervention on PFC strategy use persisted over time (Group F1, 260 = 13.06, p = .000, overall d = .42), as neither the main effect of Time nor the Time × Group interaction was significant. The intervention also reduced the use of AFC (Group F1, 266 = 4.48, p = .035, overall d = .23). The significant main effect of Time indicated a parallel decline in both groups (Time F2, 451 = 12.79, p = .000), as the Time × Group interaction was non-significant. The intervention did not exert a significant effect on seeking social support.
Mindfulness (FFMQ)
The intervention led to a significant overall increase in total FFMQ scores (Group F1, 275 = 4.63, p = .032, overall d = .23). Both groups reported a parallel increase in dispositional mindfulness over time (Time F2, 454 = 11.80, p = .000), as the Time × Group interaction was non-significant.
The intervention effect also remained significant for the ‘non-reactivity’ facet (Group F1, 271 = 9.02, p = .003, overall d = .20). A significant effect of Time (F2, 458 = 9.40, p = .000) reflected a parallel increase in both groups, as the Time × Group interaction was non-significant. The intervention did not affect the following mindfulness facets: ‘non-judging of inner experience’, ‘observing’, ‘acting with awareness’ and ‘describing’. Both groups showed increasing levels of these facets, with the exception of ‘observing’.
Intervention Compliance and the Role of Mindfulness Practice
Students attended an average of 5.3 MBSR sessions (SD 1.9, range 1–7). During the 4-year follow-up period, 46% of students declined to join the seven booster sessions, while 21% attended one session, 25% attended between two and four sessions and 5% attended between five and seven sessions. No differences were observed between booster session attenders and decliners. Booster session attendance did not predict variation in any of the primary or secondary outcome measures.
The results showed significant main effects of Group on practice frequency (F1, 263 = 63.78, p = .000) and duration (F1, 265 = 9.87, p = .002). The effect of the Group × Time interaction on practice frequency was also significant (F2, 445 = 17.59, p = .000), indicating a significant decrease and non-significant increase in practice frequency in the intervention and control groups, respectively, over time. Despite these results, planned comparisons revealed that the intervention group practised mindfulness exercises significantly more frequently, relative to the control group, at all measurement points. Intervention effects regarding practice duration were significant only at T1.
More specifically, 80% of intervention group participants practised mindfulness 1.5 times a week, on average, at T1 (mean duration 13 min per session); 59% of participants practised twice monthly, on average, at T2 (8 min per session); and 58% of participants practised twice monthly, on average, at T3 (11 min per session). However, the control group practised mindfulness more often at T3 than they did at T1. Thus, 37% of participants practised twice monthly, on average, at T3 (16 min per session). Further, 37 students in the control group reported undertaking mindfulness training during the follow-up period; excluding their data from the analyses did not exert a significant effect on the results.
Frequency and duration of formal mindfulness practice did not predict levels of mental distress nor coping, but positively predicted self-report mindfulness scores (FFMQ total: frequency of practice F5, 621 = 6.12, p < .001 and duration of practice F5, 599 = 2.35, p < .05). There were no interactions with Group or Time; hence, duration and frequency of formal mindfulness practice positively influenced self-report mindfulness independently of group allocation and at all measure points. Follow-up regression analyses indicated that frequency and duration of practice at T1 and at T3 positively predicted total FFMQ scores measured concurrently for the whole sample (p < .05). At T2, frequency but not duration of practice significantly predicted total FFMQ scores (p < .05).
Mediators of Long-term Intervention Effects
Dispositional mindfulness was examined as a mediator of the long-term intervention effects. The Group factor significantly changed the mediator (FFMQ total T1), and the mediator significantly changed the outcome, hence supporting the presence of mediation.
Regarding mental distress, mediation was only examined for GHQ at T2 since the effect of the intervention on GHQ at T3 was below significance (p = .094) although Cohen’s d showed a small effect. The mediational effect of mindfulness observed at T1 was supported for GHQ at T2, as the bootstrap CIs did not include zero (Table 4). The mediation path explained 23% of the variance in the intervention effect.
As the effects of the intervention on PFC and AFC were comparable at 2- and 4-year follow-up, the two time points were combined. As the bootstrapped CIs for the mediation paths did not include zero, mediation was supported for both coping variables and explained 25% and 47% of the variance in the total intervention effect in PFC and AFC, respectively (Table 4).
Sensitivity analysis, which excluded 11 participants from the treatment group because of low intervention attendance (< 4 sessions), showed similar mediational effects for mindfulness (explaining 24% and 50% of the variance in PFC and AFC, respectively). The mediational effect of mindfulness on GHQ scores at T2 was slightly stronger using sensitivity analysis (explaining 32% of the variance in the intervention effect).
The reversed mediation analysis indicated that pre-post changes in GHQ, PFC and AFC mediated long-term effects in mindfulness (FFMQ T2 and T3 combined), explaining 67%, 19% and 31% of the variance in the total long-term intervention effect in FFMQ, respectively.
Discussion
We examined the four-year effects of a mindfulness-based intervention in a healthy sample. Previously reported findings regarding short-term positive effects of the 7-week MBSR programme on mental distress, mindfulness, avoidance-focused coping and problem-focused coping observed 1 month after the intervention (de Vibe et al. 2013; Halland et al. 2015) persisted at 4-year follow-up. Formal mindfulness practice was a positive predictor of mindfulness levels during follow-up. Furthermore, pre-post changes in mindfulness scores mediated the long-term effects of the intervention on mental distress and coping. However, since reversed mediation was also observed (i.e. pre-post changes in mental distress and coping mediating long-term effects in mindfulness), and we did not include any outcome measures during the intervention period, we cannot infer that changes in dispositional mindfulness underpin long-term changes in outcome. Pre-post changes in outcomes and dispositional mindfulness occurred concurrently; therefore, which of the two change processes most strongly influence long-term results is not settled. The short-term effects of the intervention on SWB and coping by seeking social support were not maintained. Nevertheless, our findings provided evidence suggesting that the 7-week abridged MBSR intervention reduced mental distress and enhanced coping in a small but enduring fashion in a non-clinical sample.
The effects of the intervention on problem-focused and avoidance-focused coping and dispositional mindfulness scores remained stable within a narrow range throughout the 4-year follow-up period. In contrast, effect sizes for mental distress decreased from moderate (post-test) to small at 2- and 4-year follow-up. A decline in intervention effects and generally low effect sizes were expected, as modest effects have been reported in previous clinical and non-clinical mindfulness studies involving shorter follow-up durations (Fjorback et al. 2013; Henderson et al. 2012; Shapiro et al. 2011).
An intervention effect was observed for the ‘non-reactivity’ mindfulness facet, which has been shown to play a unique role as a predictor of psychological health (Curtiss and Klemanski 2014; Desrosiers et al. 2014). The combined effects of increased mindfulness (particularly ‘non-reactivity’), increased problem-focused coping and reduced avoidance-focused coping could indicate an enduring increase in the ability to actively choose adaptive responses to internal or external stressors. The observation of long-term improvements in mindfulness and coping was encouraging considering the considerable workload and stress expected in students’ future professional careers, and the detrimental consequences of stress for the quality of patient care (Shanafelt et al. 2010). Therefore, our findings make a case for the value of mindfulness training as a curricular tool.
The initial level of participants’ stress was significantly lower relative to that reported in a previous study involving Norwegian medical students (Holm et al. 2010). Our findings could indicate a floor effect, which would account for the lack of intervention effects on SWB. Further, over the 4-year study period, distress levels remained stable in the control group, while avoidance coping decreased and coping by seeking social support increased. In contrast, previous studies have documented increased levels of stress and mental distress (Ludwig et al. 2015; Moffat et al. 2004; Niemi and Vainiomaki 2006) and reduced SWB during medical school (Kjeldstadli et al. 2006) and reduced use of engagement coping (Tyssen et al. 2001) during the first post-graduate years.
Increases in dispositional mindfulness and use of formal mindfulness exercises observed in the control group during the 4-year follow-up period could have contributed to the relatively low levels of psychological distress and weakening of between-group effects. While personal maturity could explain the gradual increase in mindfulness, given evidence indicating higher mindfulness levels in older individuals (Lilja et al. 2011), mindfulness practice predicted mindfulness scores in both groups. In addition, 36% of control group participants engaged in various forms of mindfulness training (i.e. qigong, yoga, tai chi, relaxation and meditation) during the follow-up period. However, the exclusion of these participants did not alter the results significantly. Nonetheless, the presence of ‘contamination’ as the cause of the gradual weakening of the effect cannot be ruled out. This could indicate that the self-selected participant sample was quite selective, in that many students might have agreed to participate in the study in the hope of receiving mindfulness training and attempted to pursue mindfulness alone when allocated to the control group.
Via the documentation of an enduring dose-response relationship between mindfulness practice and dispositional mindfulness, our unique longitudinal data support fundamental theoretical assumptions about the viability of meditation-based mindfulness interventions. Both frequency and time engaged in formal mindfulness practice during follow-up positively predicted the levels of total FFMQ scores over time, validating formal mindfulness practice as a key component of MBSR. Duration of practice predicted post-intervention mental distress (de Vibe et al. 2013). However, practice effects were not observed for mental distress or coping strategies at follow-up, echoing patterns observed in previous research involving follow-up of intermediate duration (Carlson et al. 2007).
There were unexpected between-group similarities in the average frequency and duration of formal mindfulness practice at 4-year follow-up, because of significant reductions and increases in practise in the intervention and control groups, respectively. However, the number of students in the intervention group who reported practicing was higher relative to that observed in the control group (i.e. 58% vs. 36% at 4-year follow-up). This could partly explain why mindfulness levels remained higher in the intervention group, relative to those observed in the control group, across time, despite an increase in mindfulness in the control group. Nevertheless, the duration and frequency of formal practice were far below recommended levels. Similarly, the numbers of students attending booster sessions were relatively low and declined with time, and booster session attendance did not predict variation in outcome measures. Unsystematic feedback from students indicated attendance difficulties, as the sessions were arranged irregularly and students were off campus periodically. However, this low rate of booster session attendance could also indicate waning motivation to practise mindfulness. Greater engagement in practice in both the short and long term could have provided more robust results.
Qualitative data from this study highlight how motivation, intention and attitude in learning mindfulness influence the range of experienced programme benefits (Solhaug et al. 2016). While some students approached mindfulness primarily as a means to improve concentration or achieve relaxation, others considered mindfulness training as a way to engage in intra- and interpersonal exploration. The latter position tended to be associated with greater engagement in practice and a broader range of experienced programme benefits relative to those observed for the former. Future studies could examine whether more frequent booster sessions and ongoing supervision could help students to deepen their mindfulness experience, maintain practice and transfer learning to their roles as helping professionals. Further, mindfulness programmes that emphasise the interrelational dimensions of mindfulness to a larger degree, relative to the MBSR programme (i.e. Cohen and Miller 2009; Krasner et al. 2009; Surrey and Kramer 2013), could also help increase motivation, and further research along these lines are encouraged.
Previous short-term research examining mechanisms of change in non-clinical samples suggested that enhanced dispositional mindfulness mediated the effects of MBIs on cognitive reactivity, emotion regulation and negative and positive affect (Bergen-Cico et al. 2013; Keng et al. 2012; Raes et al. 2009; Snippe et al. 2015). In addition, a study with a follow-up period of intermediate duration (Kuyken et al. 2010) showed that increases in mindfulness and self-compassion mediated the effects of MBCT on depressive symptoms. However, the current study indicated that increased mindfulness could have been one of the factors that mediated the long-term benefits of mindfulness training in a healthy, non-clinical sample. These results are consistent with theory (Garland et al. 2009) and empirical findings (Britton et al. 2012; Desrosiers et al. 2014; Hayes et al. 2004) suggesting that non-reactive attention could help individuals to break unproductive styles of cognitive (i.e. rumination, worry, catastrophizing) and emotional (i.e. avoidance, denial, suppression) processing, which could prolong or intensify the stressful experience.
However, a reversed mediation analysis revealed that T0-T1 changes in the outcome variables (i.e. mental distress, problem-focused coping and avoidance coping) mediated long-term effects in mindfulness, indicating that these change processes positively influence each other. Thus, the exact chain of causality remains unsettled. This problem may in future trials be remedied by including process measures of the mediator variables that are collected for example weekly during the intervention period, or between the pre-test and the first post-test follow-up. To date, most studies into mindfulness-based treatments examining mediation have serious limitations (Gu et al. 2015). While failing to rule out reversed causality, our study adds to the literature by suggesting possible longitudinal mediating mechanisms to be examined more thoroughly in future studies.
Limitations and Future Research Directions
While there were indications of genuine treatment-specific effects, their precise psychological and neurobiological underpinnings warrant further investigation. Such investigation could address methodological implications of self-rated psychological outcome measures. As in the present study, such measures could be subject to response bias (e.g. social desirability or impression management) and might not be sensitive to the particular changes induced by the intervention. Further, self-reported measurement of mindfulness involves unique problems (Grossman 2011). For instance, higher post-intervention scores could reflect familiarity with, or desirability of, the concept of mindfulness rather than a real change in dispositional mindfulness. Future studies examining the mechanisms of mindfulness should therefore use additional modes of assessment including physiological, neuro-hormonal and objective cognitive measures; judgements from significant others, patients or supervisors; qualitative interviews and behavioural experiments. To separate the roles of meditation practice in outcomes, more sensitive measures of engagement in mindfulness practice, which assess quality and content rather than merely counting duration and frequency, should be adopted (Goldberg et al. 2014).
Some other limitations of the present study should be noted. First, participants were self-selected, young, predominantly white medical and psychology students. Therefore, the results might not be generalizable to other age or ethnic groups, individuals with less education or those less motivated to undertake a mindfulness course. Further, 4-year follow-up drop outs in the intervention group showed lower adherence to mindfulness practice at post-intervention, and higher levels of mental distress and lower levels of dispositional mindfulness at T2. Therefore, longitudinal results might not be generalizable to students less motivated to practise mindfulness exercises and who develop higher levels of mental distress. Lastly, the lack of an active control group made it impossible to control for non-specific elements of the intervention, such as support from the group or mindfulness instructor. Future research should provide more detailed analysis involving comparison of MBSR or MBCT and active matched-control or mindfulness interventions that place less emphasis on formal meditation practice, such as acceptance and commitment therapy (Hayes et al. 2012).
The strengths of the study include the rigorous RCT design and a longer follow-up period relative to those of previous mindfulness studies. This allowed for the conclusion that the effects of MBIs can be traced for up to 4 years. Despite the need for replication studies and more sophisticated methods to separate effects and causal mechanisms, our findings demonstrate the value of using an abridged MBSR intervention to promote medical and psychology students’ health and resilience in coping with expected future professional challenges.
References
Amutio, A., Martinez-Taboada, C., Hermosilla, D., & Delgado, L. C. (2015). Enhancing relaxation states and positive emotions in physicians through a mindfulness training program: a one-year study. Psychology, Health & Medicine, 20(6), 720–731.
Arch, J. J., & Craske, M. G. (2006). Mechanisms of mindfulness: emotion regulation following a focused breathing induction. Behaviour Research and Therapy, 44(12), 1849–1858.
Baer, R. A. (2011). Measuring mindfulness. Contemporary Buddhism, 12(1), 241–261.
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45.
Baer, R. A., Carmody, J., & Hunsinger, M. (2012). Weekly change in mindfulness and perceived stress in a mindfulness-based stress reduction program. Journal of Clinical Psychology, 68(7), 755–765.
Bergen-Cico, D., Possemato, K., & Cheon, S. (2013). Examining the efficacy of a brief mindfulness-based stress reduction (Brief MBSR) program on psychological health. Journal of American College Health, 61(6), 348–360.
Berghmans, C., Godard, R., Joly, J., Tarquinio, C., & Cuny, P. (2012). Effects of the mindfulness based stress reduction (MBSR) approach on psychic health (stress, anxiety, depression) and coping mode of diabetic patients: a controlled and randomized pilot study. Annales Médico-Psychologiques, 170(5), 312–317.
Bohlmeijer, E., Prenger, R., Taal, E., & Cuijpers, P. (2010). The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. Journal of Psychosomatic Research, 68(6), 539–544.
Britton, W. B., Shahar, B., Szepsenwol, O., & Jacobs, W. J. (2012). Mindfulness-based cognitive therapy improves emotional reactivity to social stress: results from a randomized controlled trial. Behaviour Therapy, 43(2), 365–380.
Brown, K. W., Ryan, R. A., & Creswell, J. D. (2007). Mindfulness: theoretical foundations and evidence for its salutary effects. Psychological Inquiry, 18(4), 211–237.
Burton, A., Burgess, C., Dean, S., Koutsopoulou, G. Z., & Hugh-Jones, S. (2016). How effective are mindfulness-based interventions for reducing stress among healthcare professionals? A systematic review and meta-analysis. Stress and Health, 33(1), 3–13.
Carlson, L. E., Speca, M., Faris, P., & Patel, K. D. (2007). One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain, Behavior, and Immunity, 21(8), 1038–1049.
Chakraborty, H., & Gu, H. (2009). A mixed model approach for intent-to- treat analysis in longitudinal clinical trials with missing values. RTI Press publication No. MR-0009-0903. Research Triangle Park: RTI International Retrieved 6.9.18 from http://www.rti.org/rtipress.
Chien, W. T., & Thompson, D. R. (2014). Effects of a mindfulness-based psychoeducation programme for Chinese patients with schizophrenia: 2-year follow-up. British Journal of Psychiatry, 205(1), 52–59.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale: L. Erlbaum Associates.
Cohen, J. S., & Miller, L. J. (2009). Interpersonal mindfulness training for well-being: A pilot study with psychology graduate students. Teachers College Record, 111(12), 2760–2774.
Cousin, G., & Crane, C. (2016). Changes in disengagement coping mediate changes in affect following mindfulness-based cognitive therapy in a non-clinical sample. British Journal of Psychology, 107 (3), 434–447.
Curtiss, J., & Klemanski, D. H. (2014). Teasing apart low mindfulness: Differentiating deficits in mindfulness and in psychological flexibility in predicting symptoms of generalized anxiety disorder and depression. Journal of Affective Disorders, 166, 41–47.
Desrosiers, A., Vine, V., Curtiss, J., & Klemanski, D. H. (2014). Observing nonreactively: a conditional process model linking mindfulness facets, cognitive emotion regulation strategies, and depression and anxiety symptoms. Journal of Affective Disorders, 165, 31–37.
de Vibe, M., Solhaug, I., Tyssen, R., Friborg, O., Rosenvinge, J. H., Sorlie, T., & Bjorndal, A. (2013). Mindfulness training for stress management: a randomised controlled study of medical and psychology students. BMC Medical Education, 13, 107.
de Vibe, M., Bjørndal, A., Fattah, S., Dyrdal, G. M., Halland, E., & Tanner-Smith, E. E. (2017). Mindfulness-based stress reduction (MBSR) for improving health, quality of life, and social functioning in adults. Campbell Systematic Reviews, 13(11).
Dundas, I., Vøllestad, J., Binder, P. E., & Sivertsen, B. (2013). The five factor mindfulness questionnaire in Norway. Scandinavian Journal of Psychology, 54(3), 250–260.
Eberth, J., & Sedlmeier, P. (2012). The effects of mindfulness meditation: a meta-analysis. Mindfulness, 3(3), 174–189.
Edwards, J. R., & Baglioni, A. J. (1993). The measurement of coping with stress: construct validity of the ways of coping checklist and the cybernetic coping scale. Work and Stress, 7(1), 17–31.
Egbewale, B. E., Lewis, M., & Sim, J. (2014). Bias, precision and statistical power of analysis of covariance in the analysis of randomized trials with baseline imbalance: a simulation study. BMC Medical Research Methodology, 14(49). https://doi.org/10.1186/1471-2288-14-49.
Fjorback, L. O., Arendt, M., Ornbol, E., Walach, H., Rehfeld, E., Schroder, A., & Fink, P. (2013). Mindfulness therapy for somatization disorder and functional somatic syndromes - randomized trial with one-year follow-up. Journal of Psychosomatic Research, 74(1), 31–40.
Garland, E. L., Gaylord, S., & Park, J. (2009). The role of mindfulness in positive reappraisal. Explore-the Journal of Science and Healing, 5(1), 37–44.
Goldberg, D., & Williams, P. (1988). A user’s guide to the General Health Questionnaire. Windsor: NFER.
Goldberg, S. B., Del Re, A. C., Hoyt, W. T., & Davis, J. M. (2014). The secret ingredient in mindfulness interventions? A case for practice quality over quantity. Journal of Counseling Psychology, 61(3), 491–497.
Gotink, R. A., Chu, P., Busschbach, J. J. V., Benson, H., Fricchione, G. L., & Hunink, M. G. M. (2015). Standardised mindfulness-based interventions in healthcare: an overview of systematic reviews and meta-analyses of RCTs. PLoS One, 10(4). https://doi.org/10.1371/journal.pone.0124344.
Goyal, M., Singh, S., Sibinga, E. M. S., Gould, N. F., Rowland-Seymour, A., Sharma, R., . . . Haythornthwaite, J. A. (2014). Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Internal Medicine, 174(3), 357–368.
Grossman, P. (2011). Defining mindfulness by how poorly I think I pay attention during everyday awareness and other intractable problems for psychology's (re) invention of mindfulness: comment on Brown et al. (2011). Psychological Assessment, 23(4), 1034–1040.
Grossman, P. (2015). Mindfulness: awareness informed by an embodied ethic. Mindfulness, 6(1), 17–22.
Grossman, P., Tiefenthaler-Gilmer, U., Raysz, A., & Kesper, U. (2007). Mindfulness training as an intervention for fibromyalgia: evidence of postintervention and 3-year follow-up benefits in well-being. Psychotherapy and Psychosomatics, 76(4), 226–233.
Gu, J., Strauss, C., Bond, R., & Cavanagh, K. (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37, 1–12.
Halland, E., De Vibe, M., Solhaug, I., Tyssen, R., Friborg, O., Rosenvinge, J. H., . . . Bjørndal, A. (2015). Mindfulness training improves problem-focused coping in psychology and medical students. College Student Journal 49(3), 387–398.
Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press.
Hayes, S. C., Strosahl, K., Wilson, K. G., Bissett, R. T., Pistorello, J., Toarmino, D., . . . McCurry, S. M. (2004). Measuring experiential avoidance: a preliminary test of a working model. Psychological Record, 54(4), 553–578.
Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (2012). Acceptance and commitment therapy: The process and practice of mindful change (2nd ed.). New York: Guilford Press.
Henderson, V., Clemow, L., Massion, A., Hurley, T., Druker, S., & Hebert, J. R. (2012). The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients: a randomized trial. Breast Cancer Research and Treatment, 131(1), 99–109.
Hofmann, S. G., Sawyer, A. T., Witt, A. A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. Journal of Consulting and Clinical Psychology, 78(2), 169–183.
Holm, M., Tyssen, R., Stordal, K. I., & Haver, B. (2010). Self-development groups reduce medical school stress: a controlled intervention study. BMC Medical Education, 10, 23.
Kabat-Zinn, J. (2005). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain and illness. New York: Bantam Dell.
Kabat-Zinn, J., Lipwoth, L., Burncy, R., & Sellers, W. (1987). Four-year follow-up of a meditation-based program for the self-regulation of chronic pain: treatment outcomes and compliance. The Clinical Journal of Pain, 2(3), 159–173.
Kazdin, A. E. (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27.
Keng, S.-L., Smoski, M. J., Robins, C. J., Ekblad, A. G., & Brantley, J. G. (2012). Mechanisms of change in mindfulness-based stress reduction: self-compassion and mindfulness as mediators of intervention outcomes. Journal of Cognitive Psychotherapy, 26(3), 270–280.
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., . . . Hofmann, S. G. (2013). Mindfulness-based therapy: a comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763–771.
Khoury, B., Sharma, M., Rush, S. E., & Fournier, C. (2015). Mindfulness-based stress reduction: a meta-analysis. Journal of Psychosomatic Research, 78(6), 519–528.
Kjeldstadli, K., Tyssen, R., Finset, A., Hem, E., Gude, T., Gronvold, N., . . . Vaglum, P. (2006). Life satisfaction and resilience in medical school: a six-year longitudinal, nationwide and comparative study, BMC Medical Education, 6(1), 48.
Krasner, M. S., Epstein, R. M., Beckman, H., Suchman, A. L., Chapman, B., Mooney, C. J., & Quill, T. E. (2009). Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. Journal of the American Medical Association, 302(12), 1284–1293.
Kuyken, W., Watkins, E., Holden, E., White, K., Taylor, R. S., Byford, S., . . . Dalgleish, T. (2010). How does mindfulness-based cognitive therapy work? Behaviour Research and Therapy, 48(11), 1105–1112.
Lilja, J. L., Frodi-Lundgren, A., Hanse, J. J., Josefsson, T., Lundh, L. G., Skold, C., . . . Broberg, A. G. (2011). Five facets mindfulness questionnaire-reliability and factor structure: a Swedish version. Cognitive Behavioral Therapy, 40(4), 291–303.
Lubans, D. R., Foster, C., & Biddle, S. J. H. (2008). A review of mediators of behavior in interventions to promote physical activity among children and adolescents. Preventive Medicine, 47(5), 463–470.
Ludwig, A. B., Burton, W., Weingarten, J., Milan, F., Myers, D. C., & Kligler, B. (2015). Depression and stress amongst undergraduate medical students. BMC Medical Education, 15, 141.
Malarkey, W. B., Jarjoura, D., & Klatt, M. (2013). Workplace based mindfulness practice and inflammation: a randomized trial. Brain, Behavior, and Immunity, 27(1), 145–154.
Meadows, G. N., Shawyer, F., Enticott, J. C., Graham, A. L., Judd, F., Martin, P. R., . . . Segal, Z. (2014). Mindfulness-based cognitive therapy for recurrent depression: a translational research study with 2-year follow-up. Australian and New Zealand Journal of Psychiatry, 48(8), 743–755.
Miller, J. J., Fletcher, K., & Kabat-Zinn, J. (1995). Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. General Hospital Psychiatry, 17(3), 192–200.
Moffat, K. J., McConnachie, A., Ross, S., & Morrison, J. M. (2004). First year medical student stress and coping in a problem-based learning medical curriculum. Medical Education, 38(5), 482–491.
Moum, T., Naess, S., Sorensen, T., Tambs, K., & Holmen, J. (1990). Hypertension labeling, life events and psychological well-being. Psychological Medicine, 20(3), 635–646.
Nerdrum, P., Rustøen, T., & Rønnestad, M. H. (2006). Student psychological distress: a psychometric study of 1750 Norwegian 1st-year undergraduate students. Scandinavian Journal of Educational Research, 50(1), 95–109.
Niemi, P. M., & Vainiomaki, P. T. (2006). Medical students' distress--quality, continuity and gender differences during a six-year medical programme. Medical Teacher, 28(2), 136–141.
Raes, F., Dewulf, D., van Heeringen, C., & Williams, J. M. (2009). Mindfulness and reduced cognitive reactivity to sad mood: evidence from a correlational study and a non-randomized waiting list controlled study. Behaviour Research and Therapy, 47(7), 623–627.
Roth, D. L., & MacKinnon, D. P. (2013). Mediation analysis with longitudinal data. In J. Newsome, R. N. Jones, & S. M. Hofer (Eds.), Longitudinal data analysis: a practical guide for researchers in aging, health, and social sciences (pp. 181–216). London: Routledge.
Røysamb, E., Harris, J. R., Magnus, P., Vittersø, J., & Tambs, K. (2002). Subjective well-being: sex-specific effects of genetic and environmental factors. Personality and Individual Differences, 32(2), 211–223.
Shanafelt, T. D., Balch, C. M., Bechamps, G., Russell, T., Dyrbye, L., Satele, D., . . . Freischlag, J. (2010). Burnout and medical errors among American surgeons. Annals of Surgery, 251(6), 995–1000.
Shapiro, S. L., Carlson, L. E., Astin, J. A., & Freedman, B. (2006). Mechanisms of mindfulness. Journal of Clinical Psychology, 62(3), 373–386.
Shapiro, S. L., Brown, K. W., Thoresen, C., & Plante, T. G. (2011). The moderation of mindfulness-based stress reduction effects by trait mindfulness: results from a randomized controlled trial. Journal of Clinical Psychology, 67(3), 267–277.
Snippe, E., Nyklicek, I., Schroevers, M. J., & Bos, E. H. (2015). The temporal order of change in daily mindfulness and affect during mindfulness-based stress reduction. Journal of Counseling Psychology, 62(2), 106–114.
Solhaug, I., Eriksen, T. E., de Vibe, M., Haavind, H., Friborg, O., Sørlie, T., & Rosenvinge, J. H. (2016). Medical and psychology student's experiences in learning mindfulness: benefits, paradoxes, and pitfalls. Mindfulness, 7, 838. https://doi.org/10.1007/s12671-016-0521-0.
Surrey, J. L., & Kramer, G. (2013). Relational mindfulness. In C. K. Germer, R. D. Siegel, & P. R. Fulton (Eds.), Mindfulness and psychotherapy (2nd ed., pp. 94–111). New York: Guilford Press.
Teasdale, J. D., Segal, Z. V., Williams, J. M. G., Ridgeway, V. A., Soulsby, J. M., & Lau, M. A. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68(4), 615–623.
Twisk, J. W. R. (2006). Applied multilevel analysis : A practical guide. Cambridge: Cambridge University Press.
Tyssen, R., Vaglum, P., Gronvold, N. T., & Ekeberg, O. (2001). Factors in medical school that predict postgraduate mental health problems in need of treatment: a nationwide and longitudinal study. Medical Education, 35(2), 110–120.
van der Velden, A. M., Kuyken, W., Wattar, U., Crane, C., Pallesen, K. J., Dahlgaard, J., et al. (2015). A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clinical Psychology Review, 37, 26–39.
Vettese, L. C., Toneatto, T., Stea, J. N., Nguyen, L., & Wang, J. J. (2009). Do mindfulness meditation participants do their homework? And does it make a difference? A review of the empirical evidence. Journal of Cognitive Psychotherapy, 23(3), 198–225.
Vitaliano, P. P., Russo, J., Carr, J. E., & Heerwagen, J. H. (1984). Medical school pressures and their relationship to anxiety. Journal of Nervous and Mental Disease, 172(12), 730–736.
Wen, Z. L., & Fan, X. T. (2015). Monotonicity of effect sizes: questioning kappa-squared as mediation effect size measure. Psychological Methods, 20(2), 193–203. https://doi.org/10.1037/met0000029.
Witek-Janusek, L., Albuquerque, K., Chroniak, K. R., Chroniak, C., Durazo-Arvizu, R., & Mathews, H. L. (2008). Effect of mindfulness based stress reduction on immune function, quality of life and coping in women newly diagnosed with early stage breast cancer. Brain, Behavior, and Immunity, 22(6), 969–981.
Acknowledgements
We warmly thank all of the students who participated in this study.
Funding
We would like to thank the Norwegian Medical Association, the Northern Norway Regional Health Authority and the Norwegian Knowledge Centre for the Health Services for funding this research project. These funding sources had no role in conducting the study.
Author information
Authors and Affiliations
Contributions
IS designed and executed the study, analysed the data and wrote the paper. MdV designed and executed the study and assisted with the data analyses and the writing. OF analysed the data and wrote part of the methods and results. RT, TS and AB collaborated in the design and the writing of the study. JHR collaborated in the design and writing and editing of the final manuscript. All authors approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interests.
Ethics Statement
The study was approved by the Regional Committee for Medical and Health Research Ethics in Norway and the Norwegian Data Inspectorate. All participants provided informed consent.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
All data are available at the Open Science Framework (https://osf.io/akbjc/).
Rights and permissions
About this article
Cite this article
Solhaug, I., de Vibe, M., Friborg, O. et al. Long-term Mental Health Effects of Mindfulness Training: a 4-Year Follow-up Study. Mindfulness 10, 1661–1672 (2019). https://doi.org/10.1007/s12671-019-01100-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-019-01100-2