Abstract
Mindfulness meditation and progressive muscle relaxation (PMR) practices are both effective in reducing stress, anxiety, and depression. To examine the mechanisms of change in mood in these two treatments, 95 participants were randomly assigned to present awareness mindfulness (PAM; N = 47) or PMR (N = 48). They were each given a 5-min audiotape of PAM or PMR and were asked to practice at least 5 min a day for 3 months. After attrition, 55 participants completed the post-intervention assessment. An additional 47 participants were assigned to a waitlist control group. Mindfulness, perceived stress, well-being, and mood symptoms were measured at pre-treatment, post-treatment, and 1-month follow-up assessment periods. PAM and PMR both led to a significant improvement in mindfulness and reduction in stress. Results of the latent growth curve analyses revealed that mindfulness and non-reactivity mediated changes in mood for PAM more than for PMR. These results suggest that differential treatment mechanisms underlie PAM and PMR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mindfulness meditation and progressive muscle relaxation (PMR) are efficacious interventions that decrease stress, anxiety, and depression (Boronkrupinska and Kulmatycki 2014; Harris 2003; Hofmann et al. 2010; Khoury et al. 2013; Moritz et al. 2015; Morledge et al. 2013; Robb 2000; Warnecke et al. 2011; Wolever et al. 2012; Younge et al. 2014). Mindfulness meditation has been proposed to foster increases in dispositional mindfulness, defined as “the awareness that emerges through paying attention, on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment by moment” (Kabat-Zinn 2003, p. 145). PMR has been thought to induce physiological relaxation by way of tensing and relaxing different muscle groups (McCallie et al. 2006).
Thus, it is possible that differential treatment mechanisms underlie mindfulness meditation and PMR. Several studies have identified potential candidates serving as differential mechanisms of mindfulness meditation and PMR. For instance, it has been proposed that decentering might be a potential mechanism that is unique to mindfulness interventions. In a study comparing a single treatment component of mindfulness (i.e., mindful breathing) to PMR, the mindfulness intervention led to greater increases in decentering relative to PMR (Feldman et al. 2010). One study found significant improvements in discriminability on a signal detection task following 4 weeks of mindfulness meditation compared to PMR (Semple 2010), suggesting that mindfulness training could enhance attentional performance. In another study by Jain et al. (2007), a 1-month mindfulness meditation was compared to a somatic relaxation intervention, which integrated techniques of PMR, autogenic relaxation, breathing techniques, and guided imagery. Results of the study indicated that significant decreases in distress, as well as increases in positive mood, were found in both meditation and relaxation groups. However, compared to the control group, reductions in rumination mediated the effect of the cognitive mindfulness intervention on symptoms of distress. These studies suggest that mindfulness treatments may be efficacious by enhancing psychological processes such as attention, decentering, and rumination reduction.
A number of studies have provided evidence that overall mindfulness functions as a treatment mechanism in mindfulness-based interventions (Bränström et al. 2010; Nyklíček et al. 2014; Nyklíček and Kuijpers 2008; Shapiro et al. 2008). For instance, one study demonstrated that mindfulness meditation was associated with increased mindfulness, which in turn predicted symptom reduction and improved well-being (Carmody and Baer 2008). Moreover, changes in mindfulness have been found to precede changes in perceived stress in a standard MBSR course, and changes in mindfulness early in treatment predicted overall improvement in perceived stress (Baer et al. 2012). To our knowledge, only a few studies have explored treatment mechanisms of PMR, which is designed to induce physiological relaxation to reduce stress (McCallie et al. 2006). One study suggested that reductions in anxiety and stress were associated with an increase in subjective well-being after PMR training (Vancampfort et al. 2011). Another study revealed that reductions in stress accounted for lower blood sugar levels in diabetes patients after PMR training (Avianti et al. 2016). Extant literature points to differential mechanisms across mindfulness-based interventions and PMR. Specifically, changes in overall mindfulness might be a treatment mechanism more specifically associated with mindfulness-based interventions relative to PMR. A comprehensive meta-analysis by Gu et al. (2015) provided evidence that increases in overall mindfulness function as a mediator of mindfulness-based interventions, which is consistent with theoretical models of mindfulness (Curtiss et al. 2017).
Research has shown that short-term, self-help mindfulness and PMR trainings demonstrated some efficacy for reducing distress (Banks et al. 2015; Chen et al. 2013; Singh et al. 2009; Weidt et al. 2015). Therefore, in order to provide mindfulness and PMR exercises that are easy to practice, we developed an audiotape containing 5 min of self-help mindfulness meditation or PMR practice for a 3-month period of time. The 5-min audio-based PMR training in the present study was based on adaptations by Bernstein and Borkovec (1973). The mindfulness meditation intervention was derived from present awareness mindfulness (PAM; Liu et al. 2016). PAM entails “Being aware of any object with acceptance, just at present moment.” (Liu et al. 2016). In PAM, practitioners do not broaden their scope of awareness by first focusing on only one object and then moving on to more objects. Instead, PAM entails monitoring of the present moment with an open scope of awareness. This distinguishes PAM from other short-term mindfulness interventions, which gradually expand the scope of awareness to facilitate mindfulness (Colzato et al. 2015; Ainsworth et al. 2015).
We hypothesized that both PAM and PMR would reduce participants’ stress levels and mood symptoms more than a waitlist control group. However, we expected these effects to be mediated through different mechanisms. We hypothesized that mindfulness constitutes a treatment mechanism specifically associated with PAM as opposed to PMR, because only the former intervention comprises mindfulness exercises as a principal treatment ingredient. Specifically, we hypothesized that mindfulness would function as a mediator for reductions in mood symptoms because available research supports the efficacy of mindfulness-based interventions for depression (Hofmann et al. 2010). In addition to examining whether overall mindfulness is a treatment mechanism specific to PAM, we investigated whether individual facets of mindfulness mediate treatment outcome for mindfulness meditation. Consistent with prior literature (Curtiss and Klemanski 2014a), we considered the following mindfulness constructs as potential mediators: non-reactivity (i.e., permitting thoughts of different emotional valence and intensity to pass through one’s mind without reaction), non-judgment (i.e., considering one’s thoughts in a non-evaluative, accepting manner), and acting with awareness (i.e., attending to one’s present activity without distraction).
Method
Participants
Participants were recruited through online advertisements and posters at Capital Normal University, inviting them to participate in a study examining stress reduction methods, in May 2014. No money or financial remuneration was given. Inclusion criteria required participants to be 18 years or older, and to be willing to participate in the 3-month online stress reduction training and a 1-month follow-up assessment.
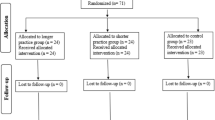
A total of 96 subjects were initially recruited for the study. One subject registered repeatedly and was excluded. The 95 remaining subjects were randomly assigned to one of the two intervention groups: 48 were assigned to the present awareness mindfulness (PAM) training group and 47 to the progressive muscle relaxation (PMR) group. Figure 1 depicts the flow of participants. Moreover, we invited 47 participants to join mindfulness training groups after a waiting period. These participants served as the waiting list control group (see Fig. 1).
With respect to attrition, 11 (11.6%) participants did not complete the assessments and trainings (5 in PAM and 6 in PMR). There were 29 (30.5%) participants who dropped out from the active interventions (13 discontinued from PAM and 16 from PMR). Of the 29 dropouts, 25 discontinued in the first month, 3 in the second month, and 1 in the third month. Chi-square analyses suggested that attrition rate did not significantly differ between the two active treatment conditions (χ2(1) = 0.72, p = 0.40). In the control group, 22 (46.8%) participants dropped out (16 did not complete the baseline assessments, and 6 withdrew before the post-treatment assessment period). Among the three groups, chi-square analyses revealed that attrition rate did not significantly differ (χ2(2) = 3.23, p = 0.20).
A total of 80 participants (30 in PAM, 25 in PMR, and 25 in control group) completed the pre-treatment and post-treatment assessment questionnaires. Of those, 55 were females (18 in PAM, 21 in PMR, and 16 in control group) and 25 were males (12 in PAM, 4 in PMR, and 9 in control group). The average age of participants was 31.67 (SD = 8.19) in the PAM group, 31.36 (SD = 9.46) in the PMR group, and 29.24 (SD = 9.49) in the control group. With respect to occupation, 31 participants were students (11 in PAM, 7 in PMR, and 13 in the control group) and 49 were employed. Forty-seven participants (17 in PAM, 16 in PMR, and 14 in the control group) reported limited prior experience with meditation, yoga, or Taiji (i.e., a few times a year or less). No significant differences between the three groups were observed at baseline for occupation (χ2(2) = 3.12, p = 0.21) or previous meditation experiences (χ2(2) = 0.42, p = 0.81). One month after the end of treatment, 22 participants from the PAM group and 14 from the PMR group completed the follow-up assessment.
Procedures
Enrollment in the current study required participants to commit to a 3-month treatment period. Participants were randomized into one of two active treatment conditions (i.e., PAM and PMR) and were instructed to download the 5-min audiotapes for self-practice. All participants were asked to complete a battery of self-report instruments at pre-treatment, post-treatment, and 1-month follow-up assessments. Participants in the control group, who had been randomly assigned to a waitlist control condition as part of another study, completed questionnaires at pre- and post-treatment time points.
To enhance treatment compliance, participants in the PAM and PMR groups were reminded to practice daily (Alliger and Williams 1993). Participants were also required to report how long they exercised each day. Participants were required to answer at least one third of all messages (30 messages total) during the 3 months (90 days). If participants did not respond after 3 days, then the instructor would contact them to determine whether they were still practicing.
Present Awareness Mindfulness (PAM) Training Material
Each intervention was designed as a 5-min instructional audiotape. Participants were required to listen to the audiotapes at least once per day. The self-help PAM was based on the PAM developed by Liu (Liu et al. 2016). The instructions required participants to monitor the present moment. Specifically, they were instructed to be aware of any aspects of their experience (e.g., sound, bodily sensations, breath, emotion, and thoughts) and cultivate acceptance of their present moment experience. More detail about PAM was listed in Table 1.
Progressive Muscle Relaxation (PMR) Training Material
The self-help PMR incorporated tension and relaxation of different muscles to reduce stress (Cohen et al. 1983). The audiotape guided participants to progressively tense and relax a variety of muscles (e.g., arms, palms, shoulders, chest, thighs, and feet). For each muscle, participants were instructed to keep them tensed for 5 s and then to relax them. More detail about PMR was listed in Table 2.
Measures
Five Facet Mindfulness Questionnaire
The 39-item Five Facet Mindfulness Questionnaire (FFMQ) is a self-report measure of mindfulness, which was developed by Baer et al. (2006). It contains five subscales: observing, describing, acting with awareness, non-judgment, and non-reactivity. Participants responded to each question on a 7-point Likert-type scale, from 1 (never) to 5 (very often). Higher scores indicated a higher level of mindfulness. The Chinese version of FFMQ was revised by Deng et al. (2011); the test-retest reliability ranged from 0.44 to 0.74. In the current study, Cronbach’s alpha for the five subscales ranged from 0.75 to 0.89 at baseline, 0.81–0.90 at post-test, and 0.76–0.92 at follow-up.
Index of Well-Being
The 9-item Chinese version of Index of Well-Being (IWB) was used to assess overall well-being (Campbell et al. 1976; Chinese version: Wang et al. 1999). It contains two subscales: an index of general affect (8-item) and an index of life satisfaction (1-item). Participants responded to questions on a 7-point Likert-type scale: from 1 (positive) to 7 (negative). The scores were reversed and higher scores indicated higher levels of well-being. The final score was the combination of the average of the two index scores (weight value was 1:1). The test-retest reliability was 0.85 (Wang et al. 1999). In the current study, Cronbach’s alpha at baseline was 0.77, 0.86 at post-test, and 0.93 at follow-up.
Perceived Stress Scale
The 14-item Chinese version of the Perceived Stress Scale was used to measure levels of stress (Cohen et al. 1983; Chinese version: Chu and Gao 2005). The scale asked participants to rate how often they felt out of control, overloaded, and overwhelmed on a 5-point Likert-type scale, from 0 (never) to 4 (very often). The test-retest reliability was 0.85 (Chu and Gao 2005). In the current study, Cronbach’s alpha of Perceived Stress Scale (PSS) was 0.89 at baseline, 0.88 at post-test, and 0.92 at follow-up.
Brief Profile of Mood State
The 30-item short form of the Profile of Mood States (Mcnair et al. 1971; Chinese version: Chi and Lin 2003) was used to assess present mood state and included six dimensions of mood: tension-anxiety, depression-dejection, anger-hostility, vigor-activity, fatigue-inertia, and confusion-bewilderment. Participants were asked to indicate mood reactions during the last week by answering the 30 adjectives describing feelings and mood on a 4-point Likert-type scale: from 0 (not at all) to 4 (extremely). The test-retest reliability was 0.41–0.66 (Chi and Lin 2003). In the current study, Cronbach’s alpha of total scale was 0.90 at baseline, 0.91 at post-test, and 0.87 at follow-up.
Data Analyses
Principle analyses of pre- to post-treatment data consisted of traditional repeated measure analyses of variance (ANOVA), which investigate the effectiveness of PAM and PMR. The alpha level was set at 0.05. All post-hoc comparisons from omnibus ANOVAs were conducted using Bonferroni corrections to mitigate the inflation of type 1 error.
To address the mechanism hypotheses, we employed a parallel process latent growth curve strategy to investigate longitudinal mediation. This procedure permits robust estimation of longitudinal growth processes, from which structural models can be derived to evaluate indirect effects (Cheong 2011). In general, latent growth curve models consist of an intercept factor and a slope factor. Whereas the former is often specified to represent the value of the initial time point, the latter estimates the mean growth of a construct over time (Preacher 2015). Consistent with established precedent (Preacher 2015; Cheong et al. 2003), longitudinal mediation was implemented in a stepwise fashion. First, unconditional parallel process latent growth curve models of mindfulness (i.e., FFMQ total score or subscales) and mood symptoms (i.e., total Profile of Mood States (POMS) score) were specified to estimate growth trajectories. In the current study, the slope factors comprised three time points (i.e., pre-treatment, post-treatment, and follow-up). Because the assumption of linear growth from pre-treatment to follow-up is likely untenable, the slope factor loadings followed an unspecified shape model (i.e., 0, *, and 1) such that the second factor loading of the slope latent variable (i.e., post-treatment time point) was freely estimated. By not imposing a priori assumptions about the form of the trajectory, unspecified shape slopes facilitate flexible modeling of non-linear growth trajectories (Brown 2007). Thus, in the current model, the means of the intercept factors represent initial pre-treatment scores, and the means of the slope factors reflect the extent of change from the pre-treatment to follow-up time points.
The second step entailed estimation of the full mediation model such that treatment condition (i.e., PAM versus PMR) predicted the mindfulness slope factor (a), which then predicted the mood symptom slope factor (b). To mitigate undue collinearity between the b pathways of individual mindfulness facets, separate mediation models were estimated for each potential mediator (i.e., total mindfulness score, non-reactivity, non-judgment, and acting with awareness). To further corroborate the hypothesis that changes in mindfulness mediated treatment efficacy, the slope factor of mindfulness was regressed onto the intercept factor of mood symptoms, and the slope factor of mood symptoms was regressed onto the intercept factor of mindfulness. Thus, the final mediation model estimated the indirect effect while controlling for baseline levels of mindfulness and mood symptoms (see Fig. 2). Finally, to establish temporal precedence, reverse mediation models (i.e., treatment condition → POMS slope → mindfulness facet slope) were pursued for statistically significant mediators. To determine the statistical significance of indirect effects, we used non-parametric bootstrapping procedures to create 95% confidence intervals (BCI) (Preacher and Hayes 2008).
Parallel process latent growth curve mediation model. Illustration of final mediation model. Tx, treatment; i.Mindfulness, intercept factor of mindfulness facet; s.Mindfulness, slope factor of mindfulness facet; i.Mood, intercept factor of mood symptoms; s.Mood, slope factor of mood symptoms. *, freely estimated parameter
For the latent growth curve analyses, missing data were accommodated with full-information maximum likelihood estimation. The following fit indices were examined to evaluate global model fit: chi-square statistic, comparative fit index (CFI), Tucker-Lewis index (TLI), and the root mean square error of approximation (RMSEA). In addition to the presence of a non-significant chi-square statistic, a good model fit was evidenced by CFI and TLI values exceeding 0.90, as well as RMSEA values less than 0.08 (Hu and Bentler 1998). All latent growth curve analyses were conducted using the R package Lavaan (Rosseel 2012).
Results
In the current sample, missing data was not associated with any of the measured variables, as indicated by the non-significant results of the Jamshidian and Jalal (2010) non-parametric test (p = 0.23). In such instances, listwise deletion is not biased (Enders 2010), and individuals missing post-treatment were omitted (i.e., 13 in PAM, and 16 in PMR).
No significant differences between the three groups were observed at baseline for age (F(2,77) = 0.56, p = 0.57) and sex (χ2(2) = 4.04, p = 0.13). One-way ANOVAs also indicated that the three groups did not differ in baseline levels of mindfulness (F(2,77) = 0.03, p = 0.97), well-being (F(2,77) = 1.02, p = 0.36), perceived stress (F(2,77) = 0.47, p = 0.63), and mood symptoms (F(2,77) = 0.48, p = 0.62) (Table 3).
Prior to exploring treatment mediators in PAM and PMR, we examined whether the interventions would improve mindfulness, well-being, perceived stress, and mood symptoms from pre- to post-treatment.
The total score of the FFMQ was entered into a repeated measure ANOVA with group (PAM, PMR, BC) as a between-subject factor, and time (pre-treatment, post-treatment) as a within-subject factor. Results revealed a significant main effect of measure time (F(1,77) = 30.04, p < 0.001, partial η2 = 0.28, observed power = 1), a significant main effect group (F(2,77) = 3.22, p = 0.05, partial η2 = 0.08, observed power = 0.60), and a significant interaction effect of group × measure time (F(2,77) = 8.03, p = 0.001, partial η2 = 0.17, observed power = 0.95). Follow-up analyses tested whether each of the three groups differed in mindfulness over time. Participants in the PAM group (t(29) = − 4.95, p < 0.001) and PMR group (t(24) = − 3.43, p = 0.002) exhibited improvements in mindfulness following these interventions over time. Moreover, participants in the PAM group improved more than those in PMR (t(1,53) = 2.57, p = 0.01) and the control group (t(1,53) = 3.42, p = 0.001). No other significant differences were observed.
A repeated measure ANOVA for the PSS revealed a significant main effect of measure time (F(1,77) = 15.25, p < 0.001, partial η2 = 0.17, observed power = 0.97) and a significant interaction effect of group × measure time (F(2,77) = 4.20, p = 0.02, partial η2 = 0.10, observed power = 0.72). Participants in the PAM (t(29) = 3.66, p = 0.001) and PMR groups (t(24) = 2.57, p = 0.02) exhibited a significant decrease in stress following these interventions over time. Moreover, participants in the PAM group decreased more than those in the control group (t(1,53) = − 2.67, p = 0.01). No other significant differences were observed (i.e., PAM vs. PMR or PMR vs. control).
With respect to POMS, only a significant main effect of measure time (F(1,77) = 8.47, p = 0.005, partial η2 = 0.10, observed power = 0.82) was found. There was a non-significant interaction effect of group × measure time for POMS (F(2,77) = 2.57, p = 0.08, partial η2 = 0.06, observed power = 0.50). No other significant differences were observed. No significant effects were observed for well-being.
The amount of average daily practice was compared across groups. An independent sample t-test (t(1,53) = 2.55, p = 0.01) revealed that participants in the PAM group (M = 10.54, SD = 6.29) practiced more often than those in the PMR group (M = 6.95, SD = 3.45).
To account for differences between practice time in PAM and PMR groups, the total score of the FFMQ, PSS, POMS, and well-being was entered into a repeated measure ANCOVA with group (PAM, PMR, BC) as a between-subject factor, measure time (pre-treatment, post-treatment) as a within-subject factor, and the time of average daily practice as covariates. Results only revealed a significant main effect of measure time (F(1,76) = 8.37, p = 0.005, partial η2 = 0.10, observed power = 0.82) for FFMQ, and a significant interaction effect of group × measure time (F(2,76) = 3.87, p = 0.03, partial η2 = 0.09, observed power = 0.68). No other significant effects were observed.
To test the mediation hypotheses, latent growth curve models were used. Missing data in follow-up was accommodated with FIML. Furthermore, results of Mardia’s multivariate normality test revealed that both skewness (γ1,p = 117.91, p = 0.23) and kurtosis (γ2,p = 250.79, p = 0.58) were normal for all variables pursued in the latent growth curve models. All of the slope factors of the unconditional latent growth models were statistically significant and in the appropriate direction (i.e., mood symptomatology decreased over time, whereas levels of mindfulness increased) (Table 4). No statistically significant covariances occurred between slope and intercept factors. Furthermore, the freely estimated factor loadings for T2 indicate the proportion of overall change that occurred between T1 and T2 relative to the total change across the three time points. Inspection of these parameter estimates indicates that the majority of the growth occurred between the first two time points for all constructs (Table 4). In the case of acting with awareness, it appears as if there were no further gains in this construct after T2. Because each unconditional latent growth model was just identified (i.e., degrees of freedom were equal to zero), standard fit indices do not apply.
Results of the parallel process latent growth curve models substantiate our hypothesis of mindfulness as a treatment mechanism underlying PAM (Table 5). There was a significant indirect effect of treatment condition on changes in mood symptoms by way of increases in overall mindfulness (γa.b = − 16.29; 95% BCI = [− 28.40, − 4.17]), controlling for baseline levels of mindfulness and mood symptoms. Specifically, the role of mindfulness as a treatment mediator was stronger for PAM than for PMR. This model evidenced excellent fit with a non-significant chi-square statistic (χ2 = 5.91, p = 0.85.), as well as good fit indices (i.e., CFI = 1; TLI = 1; and RMSEA = 0.00). Furthermore, the predictors accounted for 37% of the variance. Results of the reverse mediation model, which specified an indirect effect of treatment condition on increases in mindfulness through changes in mood symptoms, revealed good fit indices (i.e., χ2 = 13.48, p = 0.32; CFI = 0.99; TLI = 0.99; and RMSEA = 0.03). However, the indirect effect was not significant (γa.b = 36.81; 95% BCI = [− 24.92, 98.53]), thereby confirming the temporal precedence of the original mediation pathway.
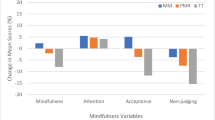
With respect to the individual facets of mindfulness, evidence of mediation was found for only non-reactivity. The indirect effect was significant (γa.b = − 29.29; 95% BCI = [− 55.17, − 3.42]), controlling for baseline levels of non-reactivity and mood symptoms. This model exhibited excellent fit with a non-significant chi-square statistic (χ2 = 11.44, p = 0.33), as well as good fit indices (i.e., CFI = 0.99; TLI = 0.99; and RMSEA = 0.06). Furthermore, 43% of the variance was accounted for by the predictors. Results of the reverse mediation model evidenced good model fit (i.e., χ2 = 11.57, p = 0.33; CFI = 0.99; TLI = 0.99; and RMSEA = 0.06); however, the indirect effect was not statistically significant (γa.b = 8.32; 95% BCI = [− 1.96, 18.60]). Thus, the results support the temporal precedence of non-reactivity as a treatment mediator for PAM. Although the latent growth curve models for non-judgment and acting with awareness exhibited good model fit, neither of the indirect effects was statistically significant (γa.b = − 30.60; 95% BCI = [− 140.20, 78.99]; and γa.b = 5.96; 95% BCI = [− 9.73, 21.66], respectively).
Discussion
The primary objective of the current study was to investigate differential treatment mechanisms in PAM and PMR. In brief, the results indicate that PAM and PMR are both efficacious interventions. Relative to the control condition, PAM and PMR resulted in greater increases in mindfulness and greater reductions in perceived stress. Mood symptoms improved across time among groups. Furthermore, no significant differences in well-being were observed between the three conditions.
To test the treatment mechanism hypothesis, a number of latent growth curve analyses were pursued to determine whether increases in mindfulness differentially mediate the efficacy of PAM and PMR in mood symptoms. Results of the current study substantiate our initial hypothesis that mindfulness is a treatment mechanism underlying PAM more than PMR. Specifically, it appears as if PAM conveys its effect on mood symptom remission by enhancing non-reactivity. Reverse mediation models suggested that changes in mood symptoms do not mediate the effect of treatment condition on changes in mindfulness. Thus, these collective findings establish temporal precedence of mindfulness as a treatment mediator of PAM. This study provides evidence that mindfulness differentially mediates the efficacy of PAM and PMR.
Our finding that mindfulness mediated the effect of PAM on mood symptoms accords well with previous studies (Baer et al. 2012; Bränström et al. 2010; Carmody and Baer 2008; Nyklíček et al. 2014; Nyklíček and Kuijpers 2008; Shapiro et al. 2008). Non-reactivity was supported as a specific mindfulness facet that accounted for symptom remission in PAM, which suggests that this particular construct may be an important treatment target. In PAM, we instructed participants to accept and let go of any unwanted thoughts, body sensations, and emotions, without trying to change them, leading to a state of non-reactivity. Indeed, prior research has suggested that non-reactivity contributes to the maintenance of emotional disorders and accounts for symptom change in mindfulness-based interventions (Curtiss and Klemanski 2014b; Desrosiers et al. 2014; Baer et al. 2012; Curtiss et al. 2017). The encouraging results of this study afford impetus for future research to consider the role of non-reactivity in PAM and other mindfulness-based interventions.
Although mindfulness is a treatment mechanism specific to PAM, it appears that both PAM and PMR can lead to improvements in mindfulness, which is consistent with prior research (Agee et al. 2009; Moritz et al. 2015). A number of reasons may explain this result. Some aspects of PMR overlap with PAM, as both interventions contain components that cultivate attentional processes. Because people in PMR are instructed to direct their attention to their muscles during tension and relaxation, this present moment awareness may contribute to increases in mindfulness. However, the results indicate that PAM results in significantly higher levels of mindfulness than PMR. Such results make sense when considering the individual treatment protocols associated with each intervention. PAM emphasizes cultivation of present moment awareness and acceptance, which are the core features of mindfulness, whereas PMR aims to decrease physical tension though muscle relaxation (Luebbert et al. 2001). Moreover, because only the PAM condition explicitly instructed individuals to engage in mindful observation (i.e., observing in a non-reactive, non-judgmental manner), this might explain why mindfulness was more strongly associated with PAM as a mediator.
In prior research, it was found that the number of dropouts in self-help programs is usually higher than in face-to-face intervention. For example, in the study by Meyer et al. (2009), 55% participants completed the post-test 9 weeks later. In the study by Morledge et al. (2013), only 57% people completed follow-up questionnaires. In the study by Cavanagh et al. (2013), 52.3% participants completed the questionnaires at both pre- and post-test. Indeed, in a study by Carrington et al. (1980), discontinuation was greater in the audio-based PMR intervention (37%) than in the audio-based meditation intervention (19%). Furthermore, only the meditation group demonstrated comparative efficacy against the waitlist control. In the present study, the attrition rate was 30.5%, which is lower than past studies, possibly because we regularly reminded participants to practice daily.
Limitations
Certain limitations to the current study warrant mention. First, although better than some studies, the attrition rate of 30.5% is not insignificant and might have influenced the results. It might be beneficial for future studies to determine which mode of delivery (e.g., individual, group, and self-directed without formal instruction) is most warranted for PAM. Such missing data poses several problems to ANOVA-based analyses. Because the missing data was not associated with any of the measured variables, listwise deletion is not biased (Enders 2010). Furthermore, the latent growth curve analyses were estimated using FIML. Nonetheless, the differential dropout rate across the conditions may pose difficulties in interpreting the results.
Second, in the present study, random allocation occurred only for the PAM and PMR conditions. The control condition consisted of participants enrolled in a waitlist from a different mindfulness treatment. However, we focused our investigation of treatment mechanisms to a comparison of PAM and PMR, in which participants were randomly allocated. This permitted a more rigorous experimental examination of mediation. Furthermore, baseline differences were not revealed between participants across the three conditions. That notwithstanding, it would be beneficial for future research to conduct random assignment across every experimental and control condition.
Third, our latent growth curve analyses were limited to only three time points. Future research should include more frequent assessment points of mediator and outcome variables to better establish temporal precedence and to foster greater statistical power for parallel process latent growth curve analyses.
Fourth, our study assessed follow-up outcomes only after 1 month following treatment termination. In the future, additional follow-up periods (e.g., 3 and 6 months) should be included to explore whether treatment gains are maintained over longer periods of time.
Fifth, because the interventions consisted of 5 min of daily practice, it might be the case that individuals in the PMR group did not have sufficient time to relax all muscle groups adequately.
Sixth, once practice time was included as a covariate, group differences between PAM and PMR were no longer significant. Although this may indicate that treatment effects were driven by a dose-response relationship, it could be the case that PAM was better received by participants.
Seventh, an a priori power analysis was not initially conducted to determine the appropriate sample size. Although we have been able to identify meaningful effects, our sample size is limited compared to other self-help intervention studies (Morledge et al. 2013), which may affect the power of some of our analyses. More well-powered studies will be necessary to corroborate our findings.
In summary, the present study represents an initial effort to examine differential treatment mechanisms across PAM and PMR. Results of the latent growth curve analyses established that overall mindfulness and non-reactivity mediated treatment outcome specifically for PAM. These collective findings suggest that different mechanisms of action might underlie PAM and PMR. Future research can extend this work by examining whether certain neurological and physiological changes mediate the effect of mindfulness-based interventions.
Change history
11 January 2018
The authors would like to acknowledge a formatting error in Table 5 of the results section of this paper.
References
Agee, J. D., Danoff-Burg, S., & Grant, C. A. (2009). Comparing brief stress management courses in a community sample: mindfulness skills and progressive muscle relaxation. Explore the Journal of Science and Healing, 5, 104–109.
Ainsworth, B., Marshall, J. E., Meron, D., Baldwin, D. S., Chadwick, P., & Munafò, M. R. (2015). Evaluating psychological interventions in a novel experimental human model of anxiety. Journal of Psychiatric Research, 63, 117–122.
Alliger, G. M., & Williams, K. J. (1993). Using signal-contingent experience sampling methodology to study work in the field: a discussion and illustration examining task perceptions and mood. Personnel Psychology, 46, 525–549.
Avianti, N., Desmaniarti, Z., & Rumahorbo, H. (2016). Progressive muscle relaxation effectiveness of the blood sugar patients with type 2 diabetes. Open Journal of Nursing, 6, 248–254.
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13, 27–45.
Baer, R. A., Carmody, J., & Hunsinger, M. (2012). Weekly change in mindfulness and perceived stress in a mindfulness-based stress reduction program. Journal of Clinical Psychology, 68, 755–765.
Banks, J. B., Welhaf, M. S., & Srour, A. (2015). The protective effects of brief mindfulness meditation training. Consciousness and Cognition, 33, 277–285.
Bernstein, D. A., & Borkovec, T. D. (1973). Progressive relaxation training: a manual for the helping professions. Champaign, Illinois: Research Press.
Boronkrupinska, K., & Kulmatycki, L. (2014). Effectiveness of progressive muscle relaxation (pmr) in alleviating psychophysical disorders-a systematic review (1982–2012). Global Journal for Research Analysis, 3, 113–115.
Bränström, R., Kvillemo, P., Brandberg, Y., & Moskowitz, J. T. (2010). Self-report mindfulness as a mediator of psychological well-being in a stress reduction intervention for cancer patients—a randomized study. Annals of Behavioral Medicine, 39, 151–161.
Brown, T. A. (2007). Temporal course and structural relationships among dimensions of temperament and DSM–IV anxiety and mood disorder constructs. Journal of Abnormal Psychology, 116, 313–328.
Campbell, A., Converse, P. E., & Rodgers, W. L. (1976). The quality of American life: perceptions, evaluations, and satisfactions. New York: Russell Sage.
Carmody, J., & Baer, R. A. (2008). Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine, 31, 23–33.
Carrington, P., Collings Jr., G. H., Benson, H., Robinson, H., Wood, L. W., Lehrer, P. M., et al. (1980). The use of meditation-relaxation techniques for the management of stress in a working population. Journal of Occupational and Environmental Medicine, 22, 221–231.
Cavanagh, K., Strauss, C., Cicconi, F., Griffiths, N., Wyper, A., & Jones, F. (2013). A randomised controlled trial of a brief online mindfulness-based intervention. Behaviour Research & Therapy, 51(9), 573–578.
Chen, Y., Xueling, Y., Liyuan, W., & Xiaoyuan, Z. (2013). A randomized controlled trial of the effects of brief mindfulness meditation on anxiety symptoms and systolic blood pressure in Chinese nursing students. Nurse Education Today, 33, 1166–1172.
Cheong, J. (2011). Accuracy of estimates and statistical power for testing meditation in latent growth curve modeling. Structural Equation Modeling, 18, 195–211.
Cheong, J., MacKinnon, D. P., & Khoo, S. T. (2003). Investigation of mediational processes using parallel process latent growth curve modeling. Structural Equation Modeling, 10, 238–262.
Chi, S., & Lin, W. (2003). The preliminary revision of brief profile of mood states (BPOMS)—Chinese edition. Chinese Mental Health Journal, 17, 768–770.
Chu, L., & Gao, S. (2005). The influence perceive stress towards mental health: the effect of meditation experience and emotion intelligence regulation. Chinese Journal of Psychology, 47, 157–179.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396.
Colzato, L. S., Sellaro, R., Samara, I., & Hommel, B. (2015). Meditation-induced cognitive-control states regulate response-conflict adaptation: evidence from trial-to-trial adjustments in the Simon task. Consciousness and Cognition, 35, 110–114.
Curtiss, J., & Klemanski, D. H. (2014a). Factor analysis of the five facet mindfulness questionnaire in a heterogeneous clinical sample. Journal of Psychopathology and Behavioral Assessment, 36, 683–694.
Curtiss, J., & Klemanski, D. H. (2014b). Teasing apart low mindfulness: differentiating deficits in mindfulness and in psychological flexibility in predicting symptoms of generalized anxiety disorder and depression. Journal of Affective Disorders, 166, 41–47.
Curtiss, J., Klemanski, D. H., Andrews, L., Ito, M., & Hofmann, S. G. (2017). The conditional process model of mindfulness and emotion regulation: an empirical test. Journal of Affective Disorders, 212, 93–100.
Deng, Y., Liu, X., Rodriguez, M. A., & Xia, C. Y. (2011). The five facet mindfulness questionnaire: psychometric properties of the Chinese version. Mindfulness, 2, 123–128.
Desrosiers, A., Vine, V., Curtiss, J., & Klemanski, D. H. (2014). Observing nonreactively: a conditional process model linking mindfulness facets, cognitive emotion regulation strategies, and depression and anxiety symptoms. Journal of Affective Disorders, 165, 31–37.
Enders, C. K. (2010). Applied missing data analysis. Guilford Press.
Feldman, G., Greeson, J., & Senville, J. (2010). Differential effects of mindful breathing, progressive muscle relaxation, and loving-kindness meditation on decentering and negative reactions to repetitive thoughts. Behaviour Research & Therapy, 48, 1002–1011.
Gu, J., Strauss, C., Bond, R., & Cavanagh, K. (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37, 1–12.
Harris, G. E. (2003). Progressive muscle relaxation: highly effective but often neglected. Guidance and Counseling, 18, 142–148.
Hofmann, S. G., Sawyer, A. T., Witt, A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. Journal of Consulting and Clinical Psychology, 78, 169–183.
Hu, L. T., & Bentler, P. M. (1998). Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychological Methods, 3, 424–453.
Jain, S., Shapiro, S. L., Swanick, S., Roesch, S. C., Mills, P. J., Bell, I., & Schwartz, G. E. (2007). A randomized controlled trial of mindfulness meditation versus relaxation training: effects on distress, positive states of mind, rumination, and distraction. Annals of Behavioral Medicine, 33, 11–21.
Jamshidian, M., & Jalal, S. (2010). Tests of homoscedasticity, normality, and missing completely at random for incomplete multivariate data. Psychometrika, 75, 649–674.
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: past, present, and future. Clinical Psychology: Science and Practice, 10, 144–156.
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., Chapleau, M. A., Paquin, K., & Hofmann, S. G. (2013). Mindfulness-based therapy: a comprehensive meta-analysis. Clinical Psychology Review, 33, 763–771.
Liu, X., Xu, J., Zhang, Q., & Wu, Y. (2016). Definition, treatment procedure and feasibility report of “present awareness” mindfulness training. China Journal of Health Psychology, 24, 1224–1229.
Luebbert, K., Dahme, B., & Hasenbring, M. (2001). The effectiveness of relaxation training in reducing treatment-related symptoms and improving emotional adjustment in acute nonsurgical cancer treatment: a meta-analytical review. Psycho-Oncology, 10, 490–502.
McCallie, M. S., Blum, C. M., & Hood, C. J. (2006). Progressive muscle relaxation. Journal of Human Behavior in the Social Environment, 13, 51–66.
Mcnair, D., Lorr, M., & Droppleman, C. (1971). Profile of mood states. San Diego: Educational & Industrial Testing Service.
Meyer, B., Berger, T., Caspar, F., Beevers, C. G., Andersson, G., & Weiss, M. (2009). Effectiveness of a novel integrative online treatment for depression (deprexis): randomized controlled trial. Journal of Medical Internet Research, 11(2), e15.
Moritz, S., Cludius, B., Hottenrott, B., Schneider, B. C., Saathoff, K., Kuelz, A. K., & Gallinat, J. (2015). Mindfulness and relaxation treatment reduce depressive symptoms in individuals with psychosis. European Psychiatry, 30, 709–714.
Morledge, T. J., Allexandre, D., Fox, E., Fu, A. Z., Higashi, M. K., Kruzikas, D. T., et al. (2013). Feasibility of an online mindfulness program for stress management—a randomized, controlled trial. Annals of Behavioral Medicine, 46, 137–148.
Nyklíček, I., & Kuijpers, K. F. (2008). Effects of mindfulness-based stress reduction intervention on psychological well-being and quality of life: is increased mindfulness indeed the mechanism? Annals of Behavioral Medicine, 35, 331–340.
Nyklíček, I., Dijksman, S. C., Lenders, P. J., Fonteijn, W. A., & Koolen, J. J. (2014). A brief mindfulness based intervention for increase in emotional well-being and quality of life in percutaneous coronary intervention (PCI) patients: the MindfulHeart randomized controlled trial. Journal of Behavioral Medicine, 37, 135–144.
Preacher, K. J. (2015). Advances in mediation analysis: a survey and synthesis of new developments. Annual Review of Psychology, 66, 825–852.
Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891.
Robb, S. L. (2000). Music assisted progressive muscle relaxation, progressive muscle relaxation, music listening, and silence: a comparison of relaxation techniques. Journal of Music Therapy, 37, 2–21.
Rosseel, Y. (2012). Lavaan: an R package for structural equation modeling. Journal of Statistical Software, 48, 1–36.
Semple, R. J. (2010). Does mindfulness meditation enhance attention? A randomized controlled trial. Mindfulness, 1, 121–130.
Shapiro, S. L., Oman, D., Thoresen, C. E., Plante, T. G., & Flinders, T. (2008). Cultivating mindfulness: effects on well-being. Journal of Clinical Psychology, 64, 840–862.
Singh, V. P., Rao, V., Prem, V., Sahoo, R. C., & Pai, K. (2009). Comparison of the effectiveness of music and progressive muscle relaxation for anxiety in COPD—a randomized controlled pilot study. Chronic Respiratory Disease, 6, 209–216.
Vancampfort, D., De Hert, M., Knapen, J., Maurissen, K., Raepsaet, J., Deckx, S., et al. (2011). Effects of progressive muscle relaxation on state anxiety and subjective well-being in people with schizophrenia: a randomized controlled trial. Clinical Rehabilitation, 25, 567–575.
Wang, X., Wang, X., & Ma, H. (1999). Manual of psychological health evaluation and measurement (revised edition). Beijing: Chinese Mental Health Journal Publisher.
Warnecke, E., Quinn, S., Ogden, K., Towle, N., & Nelson, M. R. (2011). A randomised controlled trial of the effects of mindfulness practice on medical student stress levels. Medical Education, 45, 381–388.
Weidt, S., Klaghofer, R., Kuenburg, A., Bruehl, A. B., Delsignore, A., Moritz, S., & Rufer, M. (2015). Internet-based self-help for trichotillomania: a randomized controlled study comparing decoupling and progressive muscle relaxation. Psychotherapy and Psychosomatics, 84, 359–367.
Wolever, R. Q., Bobinet, K. J., McCabe, K., Mackenzie, E. R., Fekete, E., Kusnick, C. A., & Baime, M. (2012). Effective and viable mind-body stress reduction in the workplace: a randomized controlled trial. Journal of Occupational Health Psychology, 17, 246–258.
Younge, J. O., Gotink, R. A., Baena, C. P., Roos-Hesselink, J. W., & Hunink, M. M. (2014). Mind-body practices for patients with cardiac disease: a systematic review and meta-analysis. European Journal of Preventive Cardiology, 22, 1385–1399.
Acknowledgements
The authors thank Leigh Andrews for the proofreading work.
Funding
This research was supported by the National Science Foundation of China (Project 31271114). Dr. Hofmann receives support from NIH/NCCIH (R01AT007257), NIH/NIMH (R01MH099021, R34MH099311, R34MH086668, R21MH102646, R21MH101567, K23MH100259), the James S. McDonnell Foundation 21st Century Science Initiative in Understanding Human Cognition–Special Initiative, and the Department of the Army for work unrelated to the studies reported in this article. He receives compensation for his work as an advisor from the Palo Alto Health Sciences and Otsuka Digital Health, Inc., and for his work as a Subject Matter Expert from John Wiley & Sons, Inc. and Silver Cloud Health, Inc. He also receives royalties and payments for his editorial work from various publishers.
Author information
Authors and Affiliations
Contributions
The first two authors contributed equally to this paper. LYG and JC contributed to the study idea, drafting of the manuscript, and data analyses. XHL and SH contributed to the study idea and drafting of the manuscript.
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study received ethical approval from the Academic Committee of College of Psychology, Capital Normal University. No adverse events were reported in this study. These participants were contacted by telephone to obtain verbal informed consent.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
The original version of this article was revised: The authors would like to acknowledge a formatting error in Table 5 of the results section of this paper. The header row of Table 5 was improperly formatted. This error has no implications for the results.
Rights and permissions
About this article
Cite this article
Gao, L., Curtiss, J., Liu, X. et al. Differential Treatment Mechanisms in Mindfulness Meditation and Progressive Muscle Relaxation. Mindfulness 9, 1268–1279 (2018). https://doi.org/10.1007/s12671-017-0869-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-017-0869-9