Abstract
Mindfulness-based cognitive therapy (MBCT) has been shown to be an effective treatment for mood and anxiety disorders. Little is known, however, about the specific psychological skills that may improve with MBCT. The present study investigated the relationship between history of MBCT and emotion regulation ability. Specifically, we examined cognitive reappraisal ability (CRA) in a sample of individuals with a history of MBCT compared with two control groups: a group without a history of any type of therapy and a group with a history of cognitive behavioral therapy (CBT). Groups were matched on key variables including age, sex, education, working memory, emotional reactivity, and life stress. CRA was measured using a standardized laboratory challenge. Results indicated that participants with a history of MBCT demonstrated higher CRA than both the no-therapy control group and the CBT control group. These results suggest that, by guiding people to accept thoughts and feelings without judgment and to focus on the present moment, MBCT may lay the foundation for increased CRA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mindfulness-based cognitive therapy (MBCT) is an 8-week group training class (Segal et al. 2002) that combines Kabat-Zinn’s (1990) Mindfulness-Based Stress Reduction program, which involves daily meditation and self-awareness exercises, with techniques used in cognitive behavioral therapy (CBT). The core aim of MBCT is to increase psychological health by increasing mindfulness, which can be characterized by the following skills: (1) acceptance of thoughts and feelings without judgment, and, (2) focusing fully on the present moment (Allen et al. 2006; Baer et al. 2004; Coffey et al. 2010). Previous research has shown that MBCT is an effective treatment for mood and anxiety disorders (Hofmann et al. 2010; Kim et al. 2009; Manicavasgar et al. 2011; Teasdale et al. 2000).
Although an increasing body of research supports the effects of MBCT on psychological health, much less is known about the specific psychological skills that may improve with MBCT. One particular skill that may be improved by MBCT is emotion regulation. Below, we outline theoretical and empirical evidence that suggests that MBCT may lead to improvements in the ability to use a particularly adaptive emotion regulation strategy: cognitive reappraisal. Cognitive reappraisal is defined as changing how one thinks about an emotional stimulus in order to change its emotional impact (Gross and Thompson 2007). Improvements in this type of emotion regulation would be important because self-reported use of reappraisal has been robustly linked to a wide range of psychological health outcomes, including increased well-being and decreased psychopathology (Garnefski et al. 2003; Gross and John 2003).
Recent research has focused specifically on cognitive reappraisal ability (CRA), which has been defined as the degree to which individuals can successfully change their emotions when using reappraisal during a laboratory challenge, rather than how frequently individuals report using reappraisal in their daily life (Troy and Mauss 2011). This research has shown that CRA is empirically distinct from trait cognitive reappraisal use (McRae et al. 2012) and explains variance in psychological health over and above the effects of trait reappraisal use (Troy et al. 2010).
The hypothesis that mindfulness training promotes cognitive reappraisal was first articulated by Garland (2007) and has subsequently been expanded upon by Garland and colleagues (Garland et al. 2010, 2011, 2009). This model of mindful reappraisal provides several theoretical considerations that suggest that MBCT may lead to increased CRA. First, MBCT aims to cultivate acceptance of thoughts and feelings without judgment. The practice of acceptance is thought to bring about a “decentered” metacognitive state, which is characterized by the ability to distinguish the self from the content of negative thoughts and emotions and to recognize that thoughts and emotions are passing events rather than permanent reality (Allen et al. 2006; Corcoran et al. 2010). In turn, this decentered metacognitive state may bring about increased cognitive flexibility and facilitate disengagement from initial thoughts and feelings. Importantly, Garland and colleagues have suggested that successful reappraisal relies on disengaging from the initial negative appraisal (Garland et al. 2009). In support of this hypothesis, research has shown that mindfulness training is associated with increased ease in “letting go” of negative thoughts (Frewen et al. 2008). After disengaging from the initial appraisal, the next step in the successful reappraisal process is cognitive switching—replacing the initial negative appraisal with a new, more meaningful, and more positive appraisal. Because acceptance and mindful decentering are thought to improve cognitive flexibility, which includes the ability to switch attention from one stimulus to another, this important component of successful reappraisal should be improved as well. In support of this hypothesis, previous research has shown that mindfulness training increases the ability to switch attention from one object to another (Jha et al. 2007). In sum, cognitive improvements brought about by acceptance and mindful decentering may increase CRA by allowing individuals to more easily let go of initial negative appraisals and more effectively replace these appraisals with positive interpretations.
The second key aim of MBCT is to encourage individuals to focus their attention fully on the present moment. This important aim of MBCT may also enhance CRA. Specifically, focus on the present moment may lead to broadened awareness of a wide range of stimuli (thoughts, feelings, physical sensations, etc.). Theoretically, it would be extremely difficult for people to successfully re-interpret their thoughts and feelings using reappraisal if they are not fully aware of what they are thinking and feeling. Thus, by engaging in more present-centered thinking, individuals may be able to more accurately and more quickly identify negative cognitions and emotions (Allen et al. 2006). Indeed, research suggests that highly mindful individuals are more aware of how they are feeling, as evidenced by high concordance between implicit and explicit measures of emotion (Brown and Ryan 2003). Thus, improvements in awareness brought about by MBCT may provide an important foundation for improved CRA. In addition, enhanced awareness should provide individuals with more information from the environment with which to form reappraisals. That is, if an individual is more aware of his/her current situation, as well as the thoughts, feelings, and sensations he/she is experiencing, he/she will likely be able to think of multiple ways to reappraise the current situation successfully. In sum, enhanced focus on the present moment should improve CRA because it allows people to more easily identify negative appraisals that need to be changed, and it provides more useable information with which to form reappraisals.
Thus, based on the theoretical and empirical considerations outlined above, the two key targets of MBCT—acceptance without judgment and present-centered awareness—may lead to improvements in cognitive flexibility and broadened attention, which may lay the foundation for improved CRA. In support of the idea that MBCT may enhance CRA, research has found a positive relationship between trait mindfulness and self-reported general ability to regulate negative emotions (Coffey et al. 2010). Extending upon these initial findings, a subsequent study found that mindfulness training is associated with increases in the self-reported trait use of cognitive reappraisal, more specifically (Garland et al. 2011). Importantly, however, previous research suggests that self-reported use of reappraisal may not perfectly translate into the ability to use cognitive reappraisal as measured by performance during emotional challenges (McRae et al. 2012; Troy et al. 2010). Thus, it remains unknown whether MBCT is associated with and may lead to increased ability to use cognitive reappraisal successfully. The present study extends previous research by using a standardized laboratory measure of cognitive reappraisal ability, rather than a self-report measure of reappraisal use, to examine the relationship between a history of MBCT and CRA.
MBCT Versus CBT
While the theoretical model described above predicts that treatment with MBCT leads to increased CRA, it may be that treatment with any form of therapy may lead to increased CRA. It is thus important to compare MBCT to other types of therapy. Comparing MBCT to CBT is especially important because CBT is one of the most commonly used interventions, and it has received wide empirical support for treating many forms of psychopathology (Hofmann and Smits 2008). While CBT encompasses a number of different techniques (Compton et al. 2004; Hofmann and Asmundson 2008), there are some systematic commonalties as well as differences between CBT and MBCT. In terms of overlap, MBCT and CBT both focus broadly on increasing attention to individuals’ thoughts and emotions in order to improve psychological health (Corcoran et al. 2010; Hofmann and Asmundson 2008). Thus, CBT may also be associated with increased CRA. However, we believe that MBCT should lead to greater increases in CRA, relative to CBT, for two reasons. First, although MBCT and CBT both aim to bring awareness to appraisals, these two therapies have different goals related to appraisals. CBT focuses on changing the content of individuals’ negative thoughts in order to break the link between negative thoughts, negative emotions, and behavior (Ellis 2003; Newman 2003). Often, this involves encouraging individuals to examine the evidence for certain beliefs or appraisals, to identify logical errors, and to generate alternative thoughts and beliefs (Borkovec et al. 2002).
MBCT, on the other hand, emphasizes acceptance of, rather than control over, one’s thoughts and feelings. Relative to CBT, MBCT more heavily emphasizes changing the relationship that people have with their thoughts and feelings (metacognition), rather than changing the content of thoughts and feelings. As outlined above, using acceptance to decenter from one’s thoughts and feelings may be highly effective in helping individuals let go of negative appraisals, a first critical step in the reappraisal process (Garland et al. 2009). Additionally, as described above, acceptance and decentering may lead to increases in the ability to switch attention, which may be particularly effective at helping individuals reorient towards positive reinterpretations. Thus, MBCT’s emphasis on acceptance may lead to larger improvements in CRA, relative to CBT, because of important improvements in metacognition and cognitive flexibility.
Second, the types of awareness thought to be cultivated by MBCT and CBT are quite different from one another. CBT focuses specifically on bringing awareness to negative thoughts and feelings (Newman 2003), whereas, as outlined above, MBCT cultivates an increased awareness of all experiences in the present moment, including awareness of the external environment, bodily sensations, thoughts, and feelings (Corcoran et al. 2010; Semple 2010). As described above, mindfulness-related improvements in broadened attention may allow individuals to more easily and quickly identify appraisals that need to be changed, and may also provide more information to draw from when forming reappraisals. Thus, MBCT’s emphasis on present centered awareness may lead to larger improvements in CRA, relative to CBT, because of improvements in broadened attention.
In sum, although both CBT and MBCT broadly target awareness of appraisals and emotions, MBCT additionally focuses on acceptance and present-centered awareness, which may lead to greater improvements in cognitive flexibility and broadened attention. Therefore, both CBT and MBCT may both lead to increased CRA because they target appraisals. However, MBCT may lead to larger increases in CRA because it targets a wider range of metacognitive and cognitive processes that may act as important antecedents for effective cognitive reappraisal.
Based on these considerations, it was important to include a control group of individuals with a history of CBT in addition to a control group with no history of therapy. In this way, we can test the hypothesis that MBCT is associated with increases in CRA over and above the effects of other types of therapy and even other types of cognitive therapy. Thus, including a CBT history control group allows for a fairly rigorous test of our hypothesis and for specific conclusions about the psychological skills that may be enhanced by MBCT. We predicted that participants with a history of MBCT would exhibit greater CRA relative to a matched no-therapy control group and a matched CBT-history group.
Method
Participants
Participants were recruited through postings to community bulletin boards and online announcements as part of a larger study on stress and emotion. So as not to alert participants to our hypotheses, no mention of mindfulness was made in any of the recruitment materials. This study was approved by the University’s Institutional Review Board and was performed in accordance with the ethical standards described in the 1964 Declaration of Helsinki. All participants provided written informed consent prior to inclusion in this study. A total of 283 people participated in this study. Of these 283 participants, 44 (15.5 %) indicated a history of CBT and 14 (4.9 %) indicated a history of MBCT.
Preliminary group comparisons revealed that those with CBT or MBCT history did not differ from the rest of the sample (n = 231) on several important variables including age, race, education, income, verbal IQ, working memory, and emotional reactivity. Those with a history of MBCT or CBT did differ from the rest of the sample on a few key variables: current use of psychiatric medication (% yes in MBCT = 42.9, CBT = 35.1, rest of sample = 13.9, χ 2(2) = 15.7, and p < .01) and life stress (MBCT M = 21.5, SD = 10.0; CBT M = 15.5, SD = 11.1; rest of sample M = 12.4, SD = 9.8, F(2, 280) = 6.67, p < .01). There were also marginally significant group differences in sex (% female in MBCT = 78.6, CBT = 59.5, rest of sample = 50.4, χ 2(2) = 4.9, and p = .08) and depressive symptoms (MBCT M = 15.5, SD = 8.7; CBT M = 9.6, SD = 9.6; rest of sample M = 9.8, SD = 9.1, F(2, 280) = 2.59, p = .08). To avoid confounds associated with these factors, we selected a sub-set of the sample to form a no-therapy history control group (n = 40), a CBT history group (n = 27), and a MBCT history group (n = 13). The three groups were matched to one another on all of the following variables: age, sex, race, education, family income, verbal IQ, working memory, emotional reactivity, and life stress (see Table 1 for characteristics of matched groups). Neither of the therapy groups differed significantly from the control group on depressive symptoms. Those in the MBCT group, however, were significantly more depressed than those in the CBT group. Because of relatively small cell sizes for the CBT and MBCT groups, these two groups could not be matched to each other. This issue is addressed in the “Secondary Analyses.”
As explained in “Procedure,” individuals for whom the baseline sadness induction failed were excluded from the matched groups (MBCT history n = 1, CBT history n = 6). Six participants in the MBCT group also indicated that they had a history of CBT. For the purposes of maintaining power for our main analyses, these six participants are included in the MBCT history group. However, these six participants are also examined separately in the “Secondary Analyses.” We were unable to match the groups on current use of psychiatric medication because a very small number of people with no therapy history were currently taking medication (n = 11). Therefore, no participant in the matched control group had a history of any type of therapy or was currently taking any psychiatric medication. This point is further addressed in the “Secondary Analyses.”
To ensure that none of the effects reported in Table 1 were driven by outliers, all analyses were re-run, this time removing values that were greater than three times the inter-quartile range above or below the mean for each variable. There were two outliers on education, one outlier on verbal IQ, one outlier on working memory, one outlier on emotional reactivity, and one outlier on depressive symptoms. When we removed each of these outliers individually, and re-ran each of the analyses listed in Table 1, group differences on education, verbal IQ, working memory, and emotional reactivity remained statistically non-significant, and the differences in depressive symptoms between groups remained statistically significant. Therefore, the matching analyses reported in Table 1 do not appear to be driven by outliers.
Procedure
Participants completed the study in two stages. First, participants filled out an online survey assessing demographic information (e.g., gender, age, and history of therapy) and psychosocial characteristics (e.g., depression symptoms and stress). Second, about a week later (M = 8.37 days, SD = 7.02), participants came to an individual laboratory session at which time CRA was measured using a laboratory challenge. The CRA task followed the procedures reported in detail by Troy and colleagues (2010). Participants first watched a short neutral film clip in order to induce a comparable neutral baseline across all participants. Next, participants were presented with three sad film clips, each approximately 2 min long. The order of the three sad films was the same for all participants.
Participants were simply asked to “watch the following film clip carefully” during the first sad film clip (“baseline sad clip”). During a subsequent sad film clip, participants were asked to reappraise the situation they are watching in order to decrease its emotional impact, using the same instructions as in previous research (Troy et al. 2010). The instructions for this condition are presented as follows:
Please watch the following film clip carefully. This time, as you watch, try to think about the situation you see in a more positive light. You can achieve this in several different ways. For example, try to imagine advice that you could give to the characters in the film clip to make them feel better. This could be advice that would help them think about the positive bearing this event could have on their lives. Or, think about the good things they might learn from this experience. Keep in mind that even though a situation may be painful in the moment, in the long run, it could make one’s life better, or have unexpected good outcomes. In other words, try to think about the situation in as positive terms as you possibly can. This can be difficult at times, so it is very important that you try your best. Please ask the research assistant if you have any questions about this task. It is very important that you carefully watch the film clip, but think about it from a positive perspective.
Because we wanted to capture existing individual differences in ability, rather than performance that may be due to practice effects, there was not a practice session. To avoid confounding emotion-regulation effects with habituation to the sad film clips, regression to the mean, or effects specific to one film clip, participants were randomly assigned to use reappraisal either during the second or during the third sad film clip (group 1 received reappraisal instructions for the second sad film and group 2 for the third sad film). After each film clip, participants reported the greatest amount of sadness that they experienced during the film clip. The degree to which participants were able to decrease their sadness from the baseline sad film clip to the reappraised sad film clip served as the measure of CRA (see “Measures”). As in previous research (Troy et al. 2010), individuals who reported feeling no sadness (an answer of 1, “not at all,” on a 9-point scale) during the baseline sad film clip (n = 23) were excluded from analyses because these individuals’ change scores are difficult to interpret due to the baseline sadness manipulation failing.
Measures
History of Therapy
On the online questionnaires, each participant was asked, “Have you previously been in therapy?” If a participant answered “yes,” he or she was asked to indicate what type of therapy he or she had received by selecting from a drop-down list. For the present study, we only examine those who indicated a history of MBCT or CBT.
Cognitive Reappraisal Ability
Self-reported sadness was measured immediately after each film clip on a 1 (not at all) to 9 (extremely) Likert scale. Because the participants did not receive reappraisal instructions for the same sad film clip, sadness ratings were z-scored for each film clip so that scores could be compared across all participants. Then, change scores were calculated by subtracting sadness ratings reported after the reappraised film clip from sadness ratings reported after the baseline sad film clip. Thus, a greater score indicates a larger decrease in sadness and better CRA.
Control Variables
It was important to control for several different variables that may be associated either with CRA, therapy history, or both, and thus may lead to spurious relationships between therapy history and CRA. Eleven control variables were assessed. Age, sex, race, highest level of education, family income, and current use of psychiatric medication were all assessed with items on the online survey. Verbal intelligence was assessed during the laboratory session using the vocabulary subscale of the Shipley Institute of Living Scale (Zachary 1986). Working memory capacity was assessed in the laboratory session with a reverse word span task, which was based on the digit span subtest of the Wechsler Adult Intelligence Scale (Wechsler 1997). Emotional reactivity was assessed with the CRA task described above. To quantify sadness reactivity, sadness ratings on the neutral film clip were subtracted from sadness ratings on the baseline sad film clip. Life stress was assessed using the Life Experiences Survey (Sarason et al. 1978), which measures the cumulative negative impact of stressful life events that participants had experienced in the previous 18 months. Depression symptoms were assessed with the online survey using the Beck Depression Inventory (α = .93, Beck and Steer 1984).
Results
Preliminary Analyses
To confirm that each of the three sad film clips induced moderate and comparable amounts of sadness, sadness ratings for each film clip for unmanipulated (no reappraisal instructions) film viewings (the whole matched groups sample for the first sad film, group 2 for the second sad film, group 1 for the third sad film) were examined. Mean (SD) sadness ratings were 6.33 (2.22; Film 1), 6.44 (2.01; Film 2), and 6.28 (2.30; Film 3). All three of the sad film clips induced significantly greater reports of sadness than the neutral film clip (M = 1.20, SD = 0.80, all p < .01). In addition, all three film clips induced significantly greater amounts of sadness than anger, fear, or happiness (all p < .01). Lastly, sadness ratings for Film 1 were not significantly different from sadness ratings for Film 2, t(33) = −.08, p = .93, or Film 3, t(39) = .46, p = .65, and there were no significant differences between Films 2 and 3, t(39) = .09, p = .93.
To confirm that the three therapy groups did not differ on what order of reappraisal instructions they received, a chi-square was conducted to examine the relationship between therapy history group and order of instructions. The chi-square was not significant, χ 2(2) = 1.64, p = .44, indicating that randomization to instruction groups for the CRA task was not significantly different between therapy groups. For the MBCT group, 61 % were in the first instruction group (group 1), for the CBT group 49 % were in group 1, and for the control group 63 % were in group 1.
The data for the present study were derived from the same larger study as those reported in Hopp et al. (2011) and Mauss et al. (2012). These articles are concerned with variables and questions different from the ones addressed in the present article; therefore, there is no overlap with the present article.
Primary Analyses: Comparing CRA in MBCT, CBT, and No-Therapy Groups
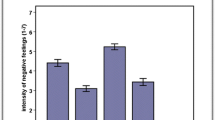
To assess whether the groups differed in CRA, an ANOVA was run with group (MBCT, CBT, and no-therapy controls) entered as the independent variable and CRA entered as the dependent variable. There was a significant effect of group on CRA, F(2, 77) = 5.03, p < .01, η 2p = .12. Post hoc comparisons using the LSD test indicated that the MBCT group (M = 0.97, SD = 0.93) had significantly greater CRA than both the CBT group (M = 0.02, SD = 1.01, p < .01, d = 1.02) and the no-therapy control group (M = 0.03, SD = 1.00, p < .01, d = 1.02, see Fig. 1). The CBT group did not significantly differ from the no-therapy control group (p = .97, d = .01). The same pattern of results was also present when examining differences in the entire (non-matched) sample, F(2, 257) = 3.94, p = .02, η 2p = .03 (MBCT history M = .97, SD = 0.83; CBT history M = .08, SD = 1.17; no therapy history M = .22, SD = .97). In addition, this relationship remained significant when removing each of the outliers described in “Method” (above).
Secondary Analyses
Controlling for Depressive Symptoms
Because the MBCT and CBT groups were significantly different from one another on depressive symptoms (see Table 1), the same ANOVA described above was run again, this time with current depressive symptoms simultaneously entered as a covariate. The effect of group on CRA remained significant, F(3, 76) = 3.48, p = .04, η 2p = .08. The effect of current depressive symptoms on CRA was marginally significant, F(3, 62) = 3.06, p = .08, η 2p = .04.
Controlling for Current Medication Use
Because we were not able to match the groups on current use of psychiatric medication, we ran another ANOVA with group (MBCT, CBT, and no-therapy controls) entered as the independent variable, current medication use (dummy coded) entered as a covariate, and CRA entered as the dependent variable. The effect of group on CRA remained significant, F(3, 75) = 5.68, p < .01, η 2p = .13. The effect of current medication was not significant, F(3, 75) = 1.47, p = .23, η 2p = .02.
Examining Effects of a History of Both CBT and MBCT
Six participants indicated that they had a history of both MBCT and CBT. To ensure that the pattern of results described above remained the same when removing these individuals from the MBCT group, a new group (MBCT/CBT) was formed. Group (MBCT only (n = 7), CBT only (n = 27), MBCT/CBT (n = 6), and no-therapy controls (n = 40)) was entered as the independent variable and CRA was entered as the dependent variable in an ANOVA. The effect of group on CRA remained significant, F(3, 76) = 3.71, p = .02, η 2p = .13. Post hoc comparisons using the LSD test showed that the MBCT/CBT group (M = 1.27, SD = 1.04) had higher CRA scores than the CBT only group (M = .02, SD = 1.01, p < .01, d = 1.22), and the no-therapy control group (M = .03, SD = 1.00, p < .01, d = 1.22), but the MBCT/CBT group did not differ from the MBCT only group (M = .71, SD = .56, p = .31, d = .67). In addition, the MBCT only group still exhibited marginally greater CRA than the CBT only group (p = .10, d = .84) and the no-therapy control group (p = .09, d = .84).
Discussion
The present study provides support for the hypothesis that MBCT is associated with improved CRA. More specifically, participants with a history of MBCT performed better on a laboratory measure of CRA than participants with a history of CBT and a no-therapy control group. The use of a laboratory challenge measure of CRA, rather than self-reported ability, makes it less likely that this association was driven by biases in socially desirable responding, retrospective reporting, or a lack of insight into one’s regulatory abilities. Importantly, the three therapy history groups were matched on ten potentially confounding variables, including age, sex, race, income, working memory, emotional reactivity, and life stress. This suggests that the present results are not due to third-variable confounds. In addition, our results held when controlling for depressive symptoms and current medication use, further suggesting that the present results are robust. When separating those individuals who had a history of both MBCT and CBT from those who had a history of MBCT only, the pattern of results remained comparable, suggesting that the results were not simply driven by participants who had received both types of therapy. Finally, the inclusion of a CBT control group in the present study provided a fairly rigorous test of the hypothesis that MBCT is associated with increased CRA over and above the effects of another type of therapy or even another type of cognitive therapy. Importantly, our results converge with others’ who have found a relationship between mindfulness and reappraisal use (Garland et al. 2011).
These results support a novel theoretical model in which treatment with MBCT leads to increased emotion regulation ability, and specifically, the ability to use cognitive reappraisal. The fact that MBCT does not focus on changing the content of cognitions, per se, but instead focuses on broader metacognitive changes by encouraging people to practice acceptance and to focus fully on the present moment, suggests that MBCT may lay the foundation for improvements in CRA by changing the way people relate to their thoughts and feelings (Hick and Chan 2010). In addition, MBCT may lead to cognitive improvements such as increased cognitive flexibility and broadened attention—processes that may serve as crucial antecedents for successful reappraisal. Future research is needed, however, to formally test which components of mindfulness lead to better CRA.
Given that past research has found a relationship between CRA and psychological health (Troy et al. 2010), and that the current study found a relationship between MBCT and CRA, it may be the case that improvements in psychological health after treatment with MBCT are mediated by increases in CRA. Indeed, Garland et al. (2011) have found that increases in trait reappraisal use mediate the relationship between mindfulness and stress. It will be important for future research to examine whether changes in CRA mediate the relationship between MBCT and psychological health.
It bears noting that history of CBT was not associated with increased CRA relative to the no-therapy control group. This finding might strike some as surprising, given that CBT focuses on changing the content of negative appraisals (Ellis 2003). We highlight three possible explanations for this finding. First, individuals with deficits in CRA may be drawn to treatment with CBT, and the course of treatment may allow them to increase to “average” levels of CRA (i.e., the same as the no-therapy control group). Second, it may be that treatment with CBT leads to improvement in different sub-types of reappraisal. In the present study participants were instructed to use a positive reappraisal strategy. It may be that CBT leads to increases in other types of reappraisal that were not measured in the present study, such as detached or distancing reappraisal (McRae et al. 2011). Third, the term “CBT” refers to a heterogeneous set of techniques that clinicians can choose from depending upon the client’s needs. The present study did not allow us to examine the specific strategies that individuals were exposed to in CBT, which may have prevented us from detecting an effect in the CBT history group. Notably, there may have been some individuals in this sample who indicated a history of CBT, but who were only exposed to behavioral change techniques, rather than cognitive restructuring. This potential heterogeneity in the CBT history group may have resulted in the finding that the CBT group did not exhibit greater CRA than the control group.
Despite these open questions, there are systematic differences between MBCT and CBT, and the current study design allowed us to compare these broad differences as an important first step in testing our theoretical model. Although learning to change cognitions is considered an integral part of CBT, to our knowledge, the hypothesis that CBT increases CRA has not been tested previously. Therefore, future research is needed to better understand the relationship between CBT and CRA. It is important to note that our results do not suggest that CBT is an ineffective treatment, or that CBT has a negative effect on emotion regulation.
It is also important to note that although the difference between the MBCT/CBT group and the MBCT only group was not statistically significant in the present sample, the effect size (d = .67) was moderate, suggesting that the lack of statistical significance may have been due to sample size. The fact that the MBCT/CBT group had higher CRA scores than the MBCT only group is in line with others’ hypothesis that a hybridized therapy that teaches mindfulness in addition to cognitive restructuring may lead to even greater increases in CRA than would be observed with CBT or MBCT alone (Garland et al. 2010). Future research should further examine this hypothesis.
Limitations
The design of the present study allowed us to test our hypotheses in a diverse community sample using a standardized laboratory measure of CRA that minimizes self-report biases (Troy et al. 2010). This study design also has limitations, however. First, the relatively small sample size in the present study limited our statistical power, as well as the reliability and generalizability of our results.
Second, participants were not randomly assigned to therapy groups. Although we controlled for ten particularly important confounds, there may be some unmeasured third variable that may explain the relationship between MBCT and CRA. Five confounds appear possible: (a) because we were not able to measure CRA prior to the initiation of therapy (in addition to after therapy), it may be that those in the MBCT group simply had greater CRA before starting the therapy, relative to the other groups; (b) the present study did not examine self-reported trait mindfulness. Therefore, it is unknown whether those with a history of MBCT exhibited higher levels of trait mindfulness, which in turn caused greater CRA scores independent of the intervention they received; (c) the current study did not measure the length of time participants spent in therapy. It is possible, for instance, that those with a history of both MBCT and CBT had elevated (non-significantly) CRA scores because they spent longer in therapy. However, the fact that our hypothesis was supported in the present study without measuring or controlling for this factor suggests that length of therapy is not the sole cause of our results; (d) we were unable to examine how recently participants had been in therapy in the present study. Thus, it may be that those with a history of MBCT received more recent treatment, and that the effect of MBCT on CRA was due to this recency; and (e) the present study did not allow us to examine what individuals had sought therapeutic intervention for (e.g., depression or anxiety). It may be that the CBT and MBCT groups in the present study systematically differed in terms of what they sought treatment for.
From a theoretical perspective, it seems unlikely that these potential confounds would systematically differ between therapy history groups, or act as the sole driver of the current results. However, future research should measure differences in CRA and related constructs before as well as after interventions to arrive at firmer causal conclusions. More specifically, the limitations of the present study could be addressed with experimental studies that randomly assign individuals to treatment with CBT, MBCT, CBT + MBCT, or wait-list controls, that measure CRA pre- and post-treatment, and that use multi-method measures of CRA (e.g., autonomic activity in addition to self reported emotional responding). This would allow for a strong test of the hypothesis that MBCT causes increases in CRA, and would help to rule out potential confounds.
In the present study, we were most interested in examining the relationship between MBCT and CRA. In future research, it will be important to examine the relationships between other types of therapy and CRA, particularly those therapies that also involve elements of mindfulness practice (e.g., Acceptance and Commitment Therapy; Hayes et al. 1999). Future research should also examine changes in the ability to use other emotion regulation strategies, such as increases in distraction and situation selection, which may also serve as important mechanisms of psychological improvement (Gross and Thompson 2007).
Concluding Comment
Despite some limitations, the present study is the first to provide evidence that MBCT is associated with improved CRA. These findings highlight a specific psychological skill that may be improved by practicing mindfulness and begin to provide insight into why MBCT is an effective treatment for mood and anxiety disorders.
References
Allen, N. B., Blashki, G., & Gullone, E. (2006). Mindfulness-based psychotherapies: a review of conceptual foundations, empirical evidence and practical considerations. The Australian and New Zealand Journal of Psychiatry, 40(4), 285–294. doi:10.1111/j.1440-1614.2006.01794.x.
Baer, R. A., Smith, G. T., & Allen, K. B. (2004). Assessment of mindfulness by self-report: the Kentucky inventory of mindfulness skills. Assessment, 11(3), 191–206.
Beck, A. T., & Steer, R. A. (1984). Internal consistencies of the original and revised Beck Depression Inventory. Journal of Clinical Psychology, 40(6), 1365–1367. doi:10.1002/1097-4679(198411)40:6<1365::AID-JCLP2270400615>3.0.CO;2-D.
Borkovec, T. D., Newman, M. G., Pincus, A. L., & Lytle, R. (2002). A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology, 70, 288–298. doi:10.1037//0022-006X.70.2.288.
Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–848. doi:10.1037/0022-3514.84.4.822.
Coffey, K. A., Hartman, M., & Fredrickson, B. L. (2010). Deconstructing mindfulness and constructing mental health: understanding mindfulness and its mechanisms of action. Mindfulness, 1, 235–253. doi:10.1007/s12671-010-0033-2.
Compton, S. N., March, J. S., Brent, D., Albano, A. M., Weersing, V. R., & Curry, J. (2004). Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: an evidence-based medicine review. Journal of the American Academy of Child and Adolescent Psychiatry, 43(8), 930–959. doi:10.1097/01.chi.0000127589.57468.bf.
Corcoran, K. M., Farb, N., Anderson, A., & Segal, Z. V. (2010). Mindfulness and emotion regulation: outcomes and possible mediating mechanisms. In A. M. Kring & D. M. Sloan (Eds.), Emotion regulation and psychopathology: a transdiagnostic approach to etiology and treatment (pp. 339–355). New York: Guilford Press.
Ellis, A. (2003). Cognitive restructuring of the disputing of irrational beliefs. In W. O'Donohue, J. E. Fisher, & S. C. Hayes (Eds.), Cognitive behavior therapy: applying empirically supported techniques in your practice (pp. 79–83). Hoboken: Wiley.
Frewen, P. A., Evans, E. M., Maraj, N., Dozois, D. J. A., & Partridge, K. (2008). Letting go: mindfulness and negative automatic thinking. Cognitive Therapy and Research, 32(6), 758–774. doi:10.1007/s10608-007-9142-1.
Garland, E. L. (2007). The meaning of mindfulness: a second-order cybernetics of stress, metacognition and coping. Complementary Health Practice Review, 12(1), 15–30. doi:10.1177/1533210107301740.
Garland, E., Gaylord, S., & Park, J. (2009). The role of mindfulness in positive reappraisal. Explore: The Journal of Science and Healing, 5(1), 37–44. doi:10.1016/j.explore.2008.10.001.
Garland, E., Fredrickson, B., Kring, A. M., Johnson, D. P., Meyer, P. S., & Penn, D. L. (2010). Upward spirals of positive emotions counter downward spirals of negativity: insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clinical Psychology Review, 30, 849–864. doi:10.1016/j.cpr.2010.03.002.
Garland, E. L., Gaylord, S. A., & Fredrickson, B. L. (2011). Positive reappraisal mediates the stress-reductive effects of mindfulness: an upward spiral process. Mindfulness, 2(1), 59–67. doi:10.1007/s12671-011-0043-8.
Garnefski, N., Boon, S., & Kraaij, V. (2003). Relationships between cognitive strategies of adolescents and depressive symptomatology across different types of life event. Journal of Youth and Adolescence, 32(6), 401–408. doi:10.1023/a:1025994200559.
Gross, J. J., & John, O. P. (2003). Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. Journal of Personality and Social Psychology, 85(2), 348–362. doi:10.1037/0022-3514.85.2.348.
Gross, J. J., & Thompson, R. A. (2007). Emotion regulation: conceptual foundations. In J. J. Gross (Ed.), Handbook of emotion regulation (pp. 3–24). New York: Guilford Press.
Hayes, S. C., Strosahl, K. D., & Wilson, K. G. (1999). Acceptance and commitment therapy: an experiential approach to behavior change. New York: Guilford Press.
Hick, S. F., & Chan, L. (2010). Mindfulness-based cognitive therapy for depression: effectiveness and limitations. Social Work in Mental Health, 8(3), 225–237. doi:10.1080/15332980903405330.
Hofmann, S. G., & Asmundson, G. J. G. (2008). Acceptance and mindfulness-based therapy: new wave or old hat? Clinical Psychology Review, 28, 1–16. doi:10.1016/j.cpr.2007.09.003.
Hofmann, S. G., & Smits, J. A. J. (2008). Cognitive behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. The Journal of Clinical Psychiatry, 69(4), 621–632.
Hofmann, S. G., Sawyer, A. T., Witt, A. A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. Journal of Consulting and Clinical Psychology, 78(2), 169–183. doi:10.1037/a0018555.
Hopp, H., Troy, A. S., & Mauss, I. B. (2011). The unconscious pursuit of emotion regulation: implications for psychological health. Cognition & Emotion, 25, 532–545.
Jha, A., Krompinger, J., & Baime, M. (2007). Mindfulness training modifies sub-systems of attention. Cognitive Affective Behavioral Neuroscience, 7, 109–119.
Kabat-Zinn, J. (1990). Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness. New York: Delta.
Kim, Y. W., Lee, S. H., Choi, T. K., Suh, S. Y., Kim, B., Kim, C. M., et al. (2009). Effectiveness of mindfulness-based cognitive therapy as an adjuvant to pharmacotherapy in patients with panic disorder or generalized anxiety disorder. Depression and Anxiety, 26, 601–606.
Manicavasgar, V., Parker, G., & Perich, T. (2011). Mindfulness-based cognitive therapy vs cognitive behaviour therapy as a treatment for non-melancholic depression. Journal of Affective Disorders, 130, 138–144. doi:10.1016/j.jad.2010.09.027.
Mauss, I. B., Savino, N. S., Anderson, C. L., Weisbuch, M., Tamir, M., & Laudenslager, M. L. (2012). The pursuit of happiness can be lonely. Emotion (in press).
McRae, K., Ciesielski, B., & Gross, J. J. (2011). Unpacking cognitive reappraisal: goals, tactics, and outcomes. Emotion. doi:10.1037/a0026351. Advance online publication.
McRae, K., Jacobs, S. E., Ray, R. D., John, O. P., & Gross, J. J. (2012). Individual differences in reappraisal ability: links to reappraisal frequency, well-being, and cognitive control. Journal of Research in Personality, 46, 2–7. doi:10.1016/j.jrp. 2011.10.003.
Newman, C. F. (2003). Cognitive restructuring: identifying and modifying maladaptive schemas. In W. O'Donohue, J. E. Fisher, & S. C. Hayes (Eds.), Cognitive behavior therapy: applying empirically supported techniques in your practice (pp. 89–95). Hoboken: Wiley.
Sarason, I. G., Johnson, J. H., & Siegel, J. M. (1978). Assessing the impact of life changes: development of the life experiences survey. Journal of Consulting and Clinical Psychology, 46(5), 932–946. doi:10.1037/0022-006x.46.5.932.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2002). Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford Press.
Semple, R. J. (2010). Does mindfulness meditation enhance attention? A randomized controlled trial. Mindfulness, 1, 121–130. doi:10.1007/s12671-010-0017-2.
Teasdale, J. D., Segal, Z. V., Williams, J. M. G., Ridgeway, V. A., Soulsby, J. M., & Lau, M. A. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68(4), 615–623. doi:10.1037/0022-006x.68.4.615.
Troy, A. S., & Mauss, I. B. (2011). Resilience in the face of stress: emotion regulation as a protective factor. In S. M. Southwick, B. T. Litz, D. Charney, & M. J. Friedman (Eds.), Resilience and mental health: challenges across the lifespan (pp. 30–44). Cambridge: Cambridge University Press.
Troy, A. S., Wilhelm, F. H., Shallcross, A. J., & Mauss, I. B. (2010). Seeing the silver lining: cognitive reappraisal ability moderates the relationship between stress and depressive symptoms. Emotion, 10(6), 783–795. doi:10.1037/a0020262.
Wechsler, D. (1997). WAIS-III administration and scoring manual. San Antonio: The Psychological Corporation.
Zachary, R. A. (1986). Shipley institute of living scale: revised manual. Los Angeles: Western Psychological Services.
Acknowledgments
The authors thank Betsy App, Taylor Newton, Victoria Floerke, and Kelly Wagner for assistance with data collection and the members of the Emotion Regulation Lab at the University of Denver for feedback on a previous draft of this manuscript. This research was supported by a grant from the National Institute on Aging (1R21AG031967) awarded to I. B. M. The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Troy, A.S., Shallcross, A.J., Davis, T.S. et al. History of Mindfulness-Based Cognitive Therapy Is Associated with Increased Cognitive Reappraisal Ability. Mindfulness 4, 213–222 (2013). https://doi.org/10.1007/s12671-012-0114-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-012-0114-5