Abstract
Background
Prognosis of gallbladder cancer (GBC) is grim even after curative surgery. Lymph node metastasis is the most important prognostic factor, but distant relapses occurring in their absence point towards additional factor. Lymph node micrometastasis could be one. The present study aimed to evaluate the incidence and clinical significance of lymph node micrometastasis.
Methods
This is a prospective study of patients undergoing curative surgery for GBC from 1 March 2013 to 30 April 2015, at our institute. All lymph nodes were examined with hematoxylin and eosin and immunohistochemistry against CK7. The incidence of lymph node and its relation to other clinicopathological parameters, recurrence, and survival was evaluated.
Results
Out of 589 lymph nodes retrieved from 40 patients, metastasis was seen in 13 (2.20%) nodes from 8 (20%) patients and micrometastasis in 4 (0.68%) nodes from 3 (7.5%) patients. Micrometastases were absent in pT1 tumors (0/10 in pT1 vs. 3/30 in pT2–4) and more common in patients with nodal metastasis (13% vs. 6%). Though the presence of micrometastasis would have upstaged the disease, it did not statistically relate to clinicopathological parameters, recurrence, and survival.
Conclusions
Incidence of lymph node micrometastasis in GBC was low and did not correlate with other clinicopathological parameters, recurrence, and survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gallbladder cancer (GBC) is a common malignancy in Indian subcontinent, with its highest incidence in women living in northern India (21.5 cases per 100,000 population annually) [1]. It has a grave prognosis with 5-year overall survival of 15% to 20%, as only 10% cancers are localized to gallbladder at the time of diagnosis [2]. Surgery is the mainstay of treatment for localized GBC, but cancer recurrence is fairly common and this points to a gap in our understanding of the biology and natural history of this cancer.
In GBC, involvement of lymph node is the most important prognostic factor and it would be prudent if efforts were directed at detecting cancer cells in such nodes. However, 5-year overall survival of 50% in node-negative disease and relapse occurring predominantly in distant sites points to an additional factor responsible for poor prognosis [3, 4]. Nodal micrometastasis may be responsible for systemic spread as they are speculated to be free cancer cells that can enter the systemic bloodstream via venous route or the thoracic duct [5]. Thus, nodal micrometastasis, defined as those identified on immunohistochemistry (IHC) but missed on routine histopathology, may be the additional prognostic indicator.
The identification of nodal micrometastasis using IHC is considered to be a poor prognostic factor, and its prognostic and therapeutic implications have been reported in other malignancies [6,7,8,9,10]. However, studies related to IHC-detected lymph nodes in GBC are relatively few and are controversial in terms of incidence as well as their significance. This study aims to detect lymph micrometastasis in gallbladder cancer using immunohistochemistry and draw conclusion regarding its clinical utility. In the present study, incidence of lymph node micrometastasis in GBC was evaluated and correlated with clinicopathological variables and survival. The study gains its importance, as there are no documented reports on the role of IHC in GBC from the country with the highest incidence of the lethal disease.
Methods
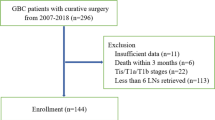
This was a prospective study performed in Gastrointestinal Oncosurgery Unit at a tertiary cancer center after taking approval from the institution’s ethical committee. All patients who underwent surgery for carcinoma gallbladder with a curative intent from 1 March 2013 to 30 April 2015 were included in the study. However, patients who were offered surgery after neoadjuvant therapy were excluded. Detailed consent regarding the study was taken from all the patients. All the patients underwent preoperative workup, which included routine blood investigations, tumor markers, contrast-enhanced CT abdomen, and chest X-ray. In patients with incidental GBC, intraoperative details were noted and histopathology slides were reviewed at our institute. PET CT was not done routinely.
Staging laparoscopy was done in all the patients to exclude distant metastasis, except in recently operated incidental GBC patients. Interaortocaval lymph nodes were dissected and sent for frozen section to confirm absence of metastasis, before proceeding further. Hepatoduodenal (HDL), retropancreatic (R/P), common hepatic artery (CHA), and celiac lymph nodes were dissected. Extent of liver resection was decided according to the location of tumor and extent of liver infiltration. Multivisceral resections were performed, if required to achieve R0 resection.
All the retrieved specimens were examined grossly and sent for histopathological examination. The first 4-μm sections were stained with hematoxylin and eosin (H&E), and the second and sixth sections were stained with anticytokeratin 7 antibody for immunohistochemistry (IHC). The IHC was performed with a standard method, in a fully automated system for immunohistochemistry, by Ventana Benchmark XT. The lymph nodes seen to be positive on H&E were documented as metastatic. Micrometastasis was diagnosed if the lymph node was negative on H&E but positive on IHC.
All patients were staged as per the seventh American Joint Committee on Cancer (AJCC) system and advised chemotherapy, chemoradiotherapy, or follow up according to the decision by multidisciplinary tumor board at our institute. Follow up of all patients was done every 3 months with history, physical examination, and investigations [tumor markers (CEA, CA19–9) every 3 months and CECT abdomen every 6 months or as clinically indicated]. The patients who failed to follow up at RGCI were contacted on telephone.
Data was collected prospectively. Statistical calculations were performed with SPSS version 22. Mann–Whitney U test (for continuous variables) and chi-squared test (for categorical variables) were used to find the relation of micrometastasis with various clinicopathological parameters. Overall and disease-free survivals after surgery were calculated using the Kaplan–Meier method in 38 patients (excluding two patients with perioperative mortality); the log rank test was used to compare cumulative survival. P<0.05 was considered statistically significant.
Results
Patient characteristics
A total of 40 patients underwent surgery for GBC (excluding patients operated after neoadjuvant chemotherapy) from 1 March 2013 to 30 April 2015. The mean age was 56.25±10.25 years. There were 7 males and 33 females. Nineteen patients were incidental GBC and pain was the presenting complaint in rest of the patients. The details of type of surgery performed are provided in Table 1. Out of 40 patients, 38 had adenocarcinoma (well differentiated = 11, moderately differentiated = 22, poorly differentiated = 5) and the remaining 2 had squamous cell carcinoma. As per the AJCC 2010, 10 patients were pT1, 15 were pT2, 14 were pT3, and 1 was pT4. Thirty-two patients were pN0 and the remaining were pN+ (pN1 = 5, pN2 = 3). Twenty-four patients received adjuvant chemotherapy and 3 patients received chemoradiation after 4 to 6 weeks of surgery, which they tolerated well with acceptable toxicity.
Incidence of micrometastasis
A total of 589 lymph nodes were obtained from 40 patients (mean = 14.7 ± 6.6). All the lymph nodes were examined with H&E and IHC against CK7. Thirteen out of 589 (2.20%) lymph nodes from 8/40 (20%) patients showed the presence of overt metastasis (H&E). All these 13 lymph nodes were positive on IHC against CK7 also. Lymph node micrometastasis (H&E −ve, IHC +ve) was detected in four (0.68%) of the remaining lymph nodes in 3 out of 40 (7.5%) patients. Seven lymph nodes in hepatoduodenal (HDL) region and five lymph nodes in retropancreatic (R/P) region were positive on H&E. Two lymph nodes each in HDL and R/P region showed micrometastasis. Though frozen was done in all interaortocaval lymph nodes to rule out metastasis, one lymph node was positive on H&E after paraffin sectioning (Table 2).
Relation of micrometastasis with other clinicopathological parameters
In the patients with micrometastasis, mean age was 62.33±0.57 years and two were females. The histopathology revealed adenocarcinoma in all three patients (well differentiated = 1, moderately differentiated = 2) with lymphovascular invasion (LVI) in one and perineural invasion (PNI) in two patients. All these parameters were comparable to those in patients without nodal micrometastasis (Table 3).
The three patients with micrometastasis belonged to pT2 (1) or pT3 (2) and pN0 (2) or pN1 (1) stage as per the present staging system. None of the 10 patients with T1 tumors (pT1a = 1, pT1b = 9) showed evidence of micrometastasis. A higher percentage of lymph node micrometastasis was seen in patients with lymph node metastasis (1 of 8 patients, 12.5%) than without (2 of 32 patients, 6.2%).
However, on statistical analysis, pT stage/pN stage/pTNM stage were not found to be related to the presence or absence of nodal micrometastasis (p = 0.766/0.339/0.552; Table 3). In patients with nodal metastasis, relation of presence of micrometastasis was related to positivity ratio as shown in Table 4. However, the sample size was too small to document significance.
Clinical significance
Upstaging of disease
In the present study, it was observed that all the three patients showing nodal micrometastasis would have been upstaged if its presence was included in the staging system. Two of these three patients were pN0 and would have been upstaged to pN1 (HDL LN + ve) and pN2 (R/P LN + ve). The third patient was pN1 and would have been upstaged to pN2 as two lymph nodes showed micrometastasis in the same patient (HDL and R/P LN).
Effect on pattern of recurrence
In the present study, recurrence was seen in 10 out of 38 patients (liver = 6, regional lymph nodes = 2, omental/peritoneal = 2). One patient with micrometastasis had recurrence in liver. The site of recurrence was more commonly locoregional and was not affected by presence or absence of micrometastasis.
Effect on overall and disease-free survival
At the final follow up, 4 out of 38 patients succumbed to the disease. All the three patients with micrometastasis were alive at 9, 18, and 23 months after their surgery. The mean overall survival was 23.26±1.26 months and was not affected by the presence of micrometastasis (p = 0.487) (Fig. 1).
Out of three patients with micrometastasis, recurrence was seen in one patient (33.33%). In those without nodal micrometastasis, nine (25.7%) patients showed presence of recurrence till the final follow up. The mean disease-free survival was slightly less in those with micrometastasis (15.5 vs. 18.74 months) but was not significant (p = 0.940) (Fig. 1).
Discussion
Cytokeratins are intermediate filament proteins that are present in epithelial cells and are not lost even on development of malignancy or metastasis [11, 12]. So, the presence of cytokeratin in lymph node suggests the presence of metastasis from epithelial primary. Antibodies against CK7 or CK 8 and 18 were shown to have high affinity for gallbladder epithelium and thus have been used to detect micrometastasis in lymph nodes in patients with GBC [13, 14]. In various studies, an incidence varying from 1.6% to 2.5% in GBC and 1.4% to 3.3% in other biliary tract cancers have been seen [3, 5, 15,16,17,18].
In our study, lymph node micrometastasis using IHC against CK7 was detected in 4 out of 589 (0.68%) lymph nodes from 3 out of 40 patients (7.5%). Our study was comparable to other studies in terms of number of patients evaluated, number of lymph nodes examined per patient, and the technique used to detect IHC. A slightly lower incidence of nodal metastasis as well as micrometastasis seen in our study may be due to exclusion of locally advanced patients receiving neoadjuvant therapy.
Out of the four lymph nodes identified on IHC, two were from the hepatoduodenal ligament and the other two were from the retropancreatic region. There was no evidence of micrometastasis in the dissected lymph nodes from para aortic, celiac, or hepatic artery regions. In other studies, an incidence of 0.6% was reported in the para aortic region and HDL and retropancreatic regions were seen to be more commonly involved.
Most of the studies suggest a higher incidence of lymph node micrometastasis in patients with lymph node metastasis (H&E); i.e. presence of nodal disease on H&E increases the chance of IHC-detected lymph node micrometastasis in other H&E-negative lymph nodes of the same patient [16]. In our study also, higher rate of nodal micrometastasis was seen in patients with nodal metastasis (12.5% vs. 6.2%). This observation is important as the nodal positivity in other nodal basins might change the staging of these patients from N1 to N2 or from locoregional disease to metastatic disease (interaortocaval node positivity). So, the benefit of detecting lymph node disease using IHC is of value even in patients with proven nodal disease on H&E.
The presence of lymph node micrometastasis has been related to aggressiveness of disease in various studies. A few studies on other digestive tract malignancies have reported an association between micrometastasis and depth of tumor invasion, lymphovascular invasion, microscopic vascular invasion, histologic subtype, and stage [19,20,21]. Most of the studies on GBC have failed to detect evidence of micrometastasis in T1 (tumor limited to muscle layer) disease [15, 18, 22]. Moreover, Nagakura et al. documented more advanced disease features in patients with micrometastasis in biliary tract cancers. They observed that a significant correlation was found between nodal micrometastasis and pTNM stage (p = 0.001), type of resection (p = 0.001), pT classification (p = 0.002), M classification (p = 0.002), lymphatic vessel invasion (p = 0.009), and perineural invasion (p = 0.013) [5]. However, other studies did not find any correlation between lymph node micrometastasis and other clinicopathological parameters [3, 18].
None of the 10 patients with pathologically T1 tumors were seen to have lymph node micrometastasis in our study, while it was present in 3 (10%) of the remaining 30 patients. However, on statistical analysis, the patients with micrometastasis were similar to those without in terms of all the clinicopathological parameters evaluated.
As per the present AJCC 2010 classification, the presence of micrometastasis is included in staging of carcinoma breast and subclassifies stage I into Ia and Ib. Its prognostic role is being evaluated in luminal gastrointestinal tract malignancies, but is not yet included in staging. Tajima et al. in their study on GBC found that if IHC-detected lymph nodes were included in the staging, one patient would have been upstaged from stage II to stage III and another patient from stage III to IV. Out of five patients with nodal micrometastasis in their study, one patient was upgraded from pN0 to pN1a, two patients from pN1a to pN1b, and one patient from pN1b to para aortic node positivity [18]. In our study, upstaging of all the three patients was seen with inclusion of micrometastasis in staging system.
The detection of micrometastasis using immunohistochemistry is upcoming, and there are many studies on its role in other malignancies. Most commonly being studied in breast cancer, the presence of nodal micrometastasis has found its place in the staging. The lymph node micrometastasis is defined as 0.2- to 2-mm-sized metastasis detected in lymph node using H&E or IHC, is designated as pNmic, and forms the basis of subgrouping stage I into stage Ia and Ib in breast cancer [23]. Among the digestive tract malignancies, role of nodal micrometastasis is being studied and has shown varied results. Some studies have shown them to be affecting the survival, while few others negate their prognostic significance. So far, there is not confirmatory evidence for the prognostic role of lymph node micrometastasis in lower or upper luminal digestive tract malignancies to include it in the staging [6,7,8,9,10, 24,25,26].
The impact of nodal micrometastasis on survival has been studied in various studies on GBC and other biliary tract malignancies and has shown inconsistent results. Nagakura et al. found micrometastasis to be the strongest predictor of survival in GBC, and Yokoyama et al. showed a trend towards poor survival in patients with micrometastasis [5, 22]. In another study, both nodal micrometastasis and metastasis were seen to be affecting the survival. They found worst survival when both were present and best when both were absent. They recommended for extensive nodal sectioning and staining for accurate staging in GBC [3]. Contradictory to these studies, Yonemori et al. and Tojima et al. failed to show the effect of micrometastasis on overall or disease-free survival [27, 18]. Tojima et al. reported that micrometastases were detected in 11 (24.4%) of 45 patients and in 13 (1.4%) of 954 lymph nodes among patients with node-negative hilar cholangiocarcinoma. Survival curves were essentially similar between patients with and without micrometastasis. In addition, the grade of micrometastasis showed no effect on survival. The Cox proportional hazard model identified microscopic venous invasion, microscopic resection margin status, and histologic differentiation as significant prognostic factors in patients with pN0 disease. They recommended that IHC has no role in prognosis and such an extensive analysis should not be done for hilar duct carcinoma. In our study, all three patients with micrometastasis were alive at the time of final follow up (9, 18, and 23 months) and its presence was not seen to have any impact on disease-free or disease-specific survival.
A higher likelihood of systemic recurrence in patients with micrometastasis in GBC suggests the hypothesis of nodal micrometastasis being a gateway to systemic disease [5, 15]. In our study, 10 patients had recurrence (8 locoregional and 2 systemic). Though the micrometastases were not related to the pattern of recurrence in our study, lower incidence of micrometastasis and lower systemic recurrences in our study reflect the exclusion of locally advanced patients (receiving neoadjuvant therapy).
With the highest incidence of GBC reported in India and the resource poor setting, it is imperative that any new technique intending to improve the survival is brought in, at the earliest, but with an eye on the cost benefit analysis. It is worthwhile to mention that the cost of performing IHC on around 15 lymph nodes (on average) per patient is high and the benefit shall be questionable till its incidence and clinical significance are established.
References
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300.
Miura F, Asano T, Amano H, et al. New prognostic factor influencing long-term survival of patients with advanced gallbladder carcinoma. Surgery. 2010;148:271–7.
Sasaki E, Nagino M, Ebata T, et al. Immunohistochemically demonstrated lymph node micrometastasis and prognosis in patients with gallbladder carcinoma. Ann Surg. 2006;244:99–105.
Jarnagin WR, William R, Ruo L, et al. Patterns of initial disease recurrence after resection of gallbladder carcinoma and hilar cholangiocarcinoma: implications for adjuvant therapeutic strategies. Cancer. 2003;98:1689–700.
Nagakura S, Shirai Y, Yokoyama N, Hatakeyama K. Clinical significance of lymph node micrometastasis in gallbladder carcinoma. Surgery. 2001;129:704–13.
McGuckin M, Cummings M, Walsh M, Hohn B, Bennett J, Wright R. Occult axillary node metastasis in breast cancer: their detection and prognostic significance. Br J Cancer. 1996;73:88–95.
Ishida K, Katsuyama T, Sugiyama A, Kawasaki S. Immunohistochemical evaluation of micrometastasis from gastric carcinomas. Cancer. 1997;79:1069–76.
Greenson J, Isenhart M, Rice R, Mojzisik C, Houchens D, Martin E. Identification of occult micrometastasis in pericolic lymph nodes of Dukes’ B colorectal cancer patients using monoclonal antibodies against cytokeratin and CC49. Cancer. 1994;73:563–8.
Sasaki M, Watanabe H, Jass J, Ajioka Y, Kobayashi M, Hatakeyama K. Immunoperoxidase staining for cytokeratins 8 and 18 is very sensitive for detection of occult node metastasis of colorectal cancer: a comparison with genetic analysis of K-ras. Histopathology. 1998;32:199–208.
Sasaki M, Watanabe H, Jass J, Ajioka Y, Kobayashi M, Hatakeyama K. Occult lymph node metastases detected by cytokeratin immunohistochemistry predict recurrence in “node-negative” colorectal cancer. J Gastroenterol. 1997;32:758–64.
Battifora H. Recent progress in the immunohistochemistry of solid tumors. Semin Diagn Pathol. 1984;1:251–71.
Debus E, Moll R, Franke WW, Weber K, Osborn M. Immunohistochemical distinction of human carcinomas by cytokeratin typing with monoclonal antibodies. Am J Pathol. 1984;14:121–30.
Moll R, Franke WW, Schiller DL, Geiger B, Krepler R. The catalog of human cytokeratins: patterns of expression in normal epithelia, tumors and cultured cells. Cell. 1982;31:11–24.
Copper D, Schermer A, Sun T. Classification of human epithelia and their neoplasms using monoclonal antibodies to keratin: strategies, applications and limitations. Lab Investig. 1985;52:243–56.
Tajima Y, Tomioka T, Ikematsu Y, Ichinose K, Inoue K, Kanematsu T. Immunohistochemical demonstration of cytokeratin is useful for detecting micrometastasis foci from gall bladder carcinoma in regional lymph nodes. Jpn J Clin Oncol. 1999;29:425–8.
Tanabe M, Endo I, Masunari H, et al. Is lymph-node micrometastasis in gallbladder cancer a significant prognostic factor? Hepatogastroenterology. 2012;59:31–5.
Taniguchi K, Tabata M, Iida T, Hori T, Yagi S, Uemoto S. Significance of lymph node micrometastasis in pN0 hilar bile duct carcinoma. Eur J Surg Oncol. 2006;32:208–12.
Tojima Y, Nagino M, Ebata T, Uesaka K, Kamiya J, Nimura Y. Immunohistochemically demonstrated lymph node micrometastasis and prognosis in patients with otherwise node-negative hilar cholangiocarcinoma. Ann Surg. 2003;237:201–7.
Ishida K, Katsuyama T, Sugiyama A, Kawasaki S. Immunohistochemical evaluation of lymph node micrometastases from gastric carcinomas. Cancer. 1997;79:1069–76.
Maehara Y, Oshiro T, Endo K, et al. Clinical significance of occult micrometastasis in lymph nodes from patients with early gastric cancer who died of recurrence. Surgery. 1996;119:397–402.
Greenson JK, Isenhart CE, Rice R, Mojzisik C, Houchens D, Martin EW Jr. Identification of occult micrometastases in pericolic lymph nodes of Dukes’ B colorectal cancer patients using monoclonal antibodies against cytokeratin and CC49. Correlation with long-term survival. Cancer. 1994;73:563–9.
Yokoyama N, Shirai Y, Hatakeyama K. Immunohistochemical detection of lymph node micrometastasis from gall bladder carcinoma using monoclonal anticytokeratin antibody. Cancer. 1999;85:1465–9.
Krag DN, Anderson SJ, Julian TB, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11:927–33.
Liefers GJ, Cleton-Jansen AM, van de Velde CJ, et al. Micrometastases and survival in stage II colorectal cancer. N Engl J Med. 1998;339:223–38.
Koenig AM, Prenzel KL, Bogoevski D, et al. Strong impact of micrometastatic tumor cell load in patients with esophageal carcinoma. Ann Surg Oncol. 2009;16:454–62.
Ishigami S, Natsugoe S, Tokuda K, et al. Clinical impact of micrometastasis of the lymph node in gastric cancer. Am Surg. 2003;69:573–7.
Yonemori A, Kondo S, Matsuno Y, et al. Prognostic impact of regional lymph node micrometastasis in patients with node-negative biliary cancer. Ann Surg. 2010;252:99–106.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SHS, NG, GG, AM, and SS declare that they have no competing interests.
Ethics statement
The study was performed in a manner to confirm with the Helsinki Declaration of 1975, as revised in 2000 and 2008, concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Rights and permissions
About this article
Cite this article
Shah, S.H., Gupta, N., Gupta, G. et al. Lymph node micrometastasis in gallbladder cancer. Indian J Gastroenterol 36, 268–274 (2017). https://doi.org/10.1007/s12664-017-0775-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-017-0775-z