Abstract
Objective
To assess the feasibility of the use of 3-dimensional (3-D) stereolithographic (SLA) technology in complex maxillofacial reconstructive surgery.
Materials and Methods
3-D SLA technology was used in the treatment planning of complex maxillofacial procedures performed by the Department of Oral and Maxillofacial Surgery at Boston University. Specialized 3-D models were ordered and utilized for surgical treatment of a variety of indications including trauma surgery, temporomandibular joint surgery, orthognathic surgery, secondary correction of facial and skull deformities, and extensive jaw pathology. This technology was also used in one patient for jaw reconstruction using novel bone and tissue engineering techniques.
Results
The use of 3-D models in Oral and Maxillofacial Surgery significantly improved predictability of clinical outcomes when compared to similar treatments without its use. Total operating time was reduced which had the benefit of decreasing the duration of general anesthesia and reducing wound exposure time. They allowed for assessment of extensive traumatic and pathologic defects in three-dimensions prior to surgical reconstruction. The models were also useful in the design and fabrication of custom prostheses, sizing of bone grafts and allowed for manufacturing of scaffolds for bone regeneration.
Conclusions
3-D SLA models can be very effectively used in oral and maxillofacial surgery for multiple indications and diverse clinical scenarios. Successful incorporation of this technology for jaw bone regeneration using tissue engineering techniques offers exciting new prospects for the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ultimate goal of any surgical procedure is to reproduce or improve pre-operative form and function. In doing so, the secondary goal is to minimize operative and postoperative morbidity. Many exciting and new technological advances have ushered in a new era in the field of Oral and Maxillofacial Surgery over the last 20 years. Use of new technology and surgical techniques has enabled the modern oral and maxillofacial surgeon to effectively accomplish these goals. One example of such technology that is continuing to increase in prevalence is the use of 3-dimensional (3-D) models to guide and assist in surgical procedures.
3-D models, also known as stereolithographs have been utilized for a variety of different purposes since their development. Charles Hull in 1986 is credited with introducing his technological advance. The use began in the automobile industry for fabrication of polyurethane models and prototypes for various models, parts and tools [1]. Subsequently, numerous advances in radiology and computer-aided manufacture (CAD–CAM) processes resulted in improved materials and accuracy. In the 1990s, use of 3-D models began in the medical and surgical setting after the realization that models could reproduce anatomically accurate representations of a patient’s hard tissue structures.
Recent literature has shown that stereolithographic (SLA) models can be successfully used in the perioperative period for improving the predictability of treatment of maxillofacial defects secondary to traumatic or pathologic conditions [1–7]. This article is aimed to illustrate a diverse range of clinical scenarios where 3-D models have been successfully utilized for maxillofacial reconstruction; the range of procedures includes trauma surgery, pathology-induced defects, tissue engineering, complex TMJ reconstruction, and correction of complicated facial asymmetry cases. It is widely accepted that utilization of 3-D models offers many distinct advantages for improved patient care. At our center, we use these models for diagnosis and treatment planning, and for patient education with direct visualization of anatomic structures. Models can be used for surgical guides and templates, as well as surgical rehearsal for training residents as well as experienced surgeons. One can easily design soft tissue incisions, surgical resection margins, assess bony defects for grafting, adaptation and pre-bending of reconstruction plates, and fabrication of custom prostheses.
In a retrospective review of surgical cases in our hospital, the use of 3-D models has proven to greatly decrease surgical operating time, decrease time under general anesthesia, and decrease wound exposure time. The cumulative effect has produced better patient care, improved colleague communication and more predictable and accurate surgical results. Table 1 lists some advantages of incorporation of 3-D SLA technology in oral and maxillofacial surgery.
Manufacture Process and Types of Models
The most commonly used models in maxillofacial surgery are those created from either acrylate (Fig. 1b) or epoxy resin (Fig. 4a), or 3-dimensional printing (3-DP) models (Fig. 5a). Fabrication of SLA models involves a process that utilizes specialized software to link information gathered from a CT scan and transferred to form a resin replica. The process of fabrication begins with a tank of ultraviolet (UV)-curable photopolymerizer resin and a UV laser. The model is fabricated in a series of layers, each that correspond to the equivalent of a slice of an axial image on CT scan. “A platform is immersed in the liquid plastic, then raised to a level just below the surface of the photopolymerizer. A software-guided beam from a helium-cadmium laser strikes the surface of the liquid and draws each layer of the object onto the surface of the liquid. This causes the plastic to solidify. After the first layer is built, the platform lowers slightly and the laser once again strikes the liquid for sequential polymerization” [1]. Each layer is polymerized at a thickness of typically 0.05–0.15 mm. This process is continued until each corresponding slice of the CT image is duplicated in the resin model. The final step is curing the entire model after fabrication. The final product is a solid and accurate 3-D representation of the patient. 3-DP models are sequentially fabricated in a similar way. An inkjet printer utilizes images that are transformed from a CT scan to sequentially fuse separate layers in formation of the 3-D product. Layers of a powder or plaster are bonded following injection of an adhesive in the shape of the axial CT image from the inkjet printer. Once the model is completed, the excess plaster is removed and the final model is cleaned and refined [4].
The type of model to be selected is dependant on its desired use. Models fabricated through the 3-DP method, are useful for educational purposes and direct visualization of anatomic structures. They do, however, have some limitations; they have been proven to be somewhat less accurate than their SLA counterparts, and because of the starch/plaster components, they cannot be sterilized for use on the surgical field since the materials do not hold up under extreme temperatures. SLA models are preferred because of higher strength, higher temperature resistance, lower moisture absorption, and lower shrinkage. They can be sterilized for surgical use, and literature has shown superior accuracy [1]. Barker et al. conducted a study comparing a model to a dry bone skull. They found a mean difference of 0.85 mm, with accuracy ranging 97.7–99.12% [7]. Choi et al. performed a similar study and reported on the percentage errors with SLA models. They found an extremely small error percentage of 0.56%, which was deemed acceptable for clinical use [8]. Table 2 summarizes basic characteristics of the three most common types of 3-D models used in the United States.
The following part of this article focuses on case examples where 3-D SLA models were used for treatment planning, surgical simulation and intraoperative guidance. It is believed that the use of SLA models in each case played an integral role, in making final surgical result more predictable and efficient.
Case 1: Trauma Surgery
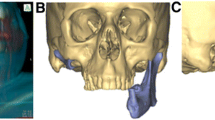
A 45-year old male presented to the medical center with a gunshot wound injury (GSW) to the left face. Following an initial surgery for closure of soft tissue injuries, a SLA model was obtained to evaluate sustained bony injuries (Fig. 1a). This patient was noted to have significant, avulsive bony injuries to the left maxilla, zygoma, orbital floor, nasal bone and medial canthal tendon regions (Fig. 1a). The SLA model in this case was used as a patient educational tool to illustrate the facial defect that resulted. Treatment options were presented to the patient including autogenous reconstruction with bone grafts, or alloplastic reconstruction using custom made implants, or bone plates and mesh. The patient elected to undergo reconstruction using only bone plates. The model was used to pre-bend the bone plates in order to re-create this patient’s pre-injury bony contour and allow for adequate soft tissue support (Fig. 1b). The procedure consisted of alloplastic reconstruction of the left zygomatic prominence, left maxillary lateral wall, left orbital rim and left orbital floor using the pre-bent and subsequently sterilized plates. A medial canthopexy was performed by placing a bone anchor into the left frontal bone. The final post-operative result showed adequate reconstruction of facial contours and adequate facial symmetry.
Case 2: Delayed Correction of Post-Traumatic Defects
A 34-year old male was referred for evaluation and surgical management of injuries sustained 2 years prior, secondary to a GSW to the right face. The patient had undergone multiple surgical procedures by other surgeons in attempt to correct severely comminuted and displaced right zygomaticomaxillary complex and orbital fractures. Upon initial presentation to our clinic (Fig. 2a), he was diagnosed with right side facial asymmetry and significant right-sided enophthalmos due to malunion of the facial fractures. An SLA model was obtained (Fig. 2b) and this model allowed for precise analysis of the displacement of bony fractures and the hard tissue defect. A wax-up was performed to further analyze the defect and to visualize re-creation of appropriate orbital volume (Fig. 2b). The orbito-zygomatic osteotomy was performed in the laboratory for training and bony interferences were marked. The patient underwent a right orbito-zygomatic osteotomy, and reconstruction using autogenous cranial bone grafts to reconstruct the orbital floor, roof and lateral walls. The surgery was performed in a laboratory, and intraoperatively, the areas of bony interferences were easy to find and reduce owing to this past experience with laboratory surgery. The final result shows restoration of facial form and contour, with good symmetry and correction of enophthalmos (Fig. 2c).
a Frontal view demonstrating facial asymmetry and right-sided enophthalmos. b SLA model with wax up of the right orbital defect performed to assess the severity of loss of orbital volume and malunion of fracture segments. c Pre- and post-operative views showing the improvement in facial asymmetry and malar projection after surgery
Case 3: Complex Facial Reconstruction Surgery
A 26-year old male presented for surgical management of severe and progressively worsening facial asymmetry due to an osteochondroma of the left mandible (Fig. 3a). There was significant facial asymmetry with deviation of the chin to the contralateral side, with elongation and bowing of the left body of the mandible. Intraoral examination revealed a skeletal and dental malocclusion characterized by an open-bite on the left side and significant dental cross-bite on the right side. A full-skull 3-DP model was fabricated after the recognition of the complexity of correcting this patient’s facial deformity. Appropriate markings were made on the model to assess the degree of deformity and model surgery performed in the laboratory (Fig. 3b). This 3-D model surgery was then duplicated on dental models and the patient taken to the operating room where the following surgery was performed: 4-piece Lefort I osteotomy, right-sided mandibular saggital split osteotomy, left mandibular inferior border osteotomy, left mandibular body osteotomy, left TMJ condylectomy and left TMJ reconstruction with costochondral graft. The postoperative results show good facial contour and symmetry with stable occlusion (Fig. 3c).
a Frontal view of the patient showing significant asymmetry due to a TMJ region mandibular tumor. b SLA models with complex multi-segmental surgical osteotomies completed and luted with sticky wax in their planned new positions. c Post-operative frontal view of the same patient demonstrating good facial contours and symmetry
Case 4: Mandibular Tumor Surgery
This 16-year old female was referred for evaluation and surgical management of a rapidly expanding pathologic lesion of the mandible (juvenile ossifying fibroma), which had failed multiple previous procedures by other surgeons. This lesion also had significant facial and lingual expansion. Due to the destruction of the native mandible and the loss of normal anatomic contour, the decision was made to obtain a SLA model of the mandible to assist in planning a staged reconstruction (Fig. 4a). Once the model was received, the gross alteration in normal architecture was appreciated. A laboratory bur was used to reduce the model back to “normal” form based on corrected cephalometric tracings. This model was then used as the foundation for pre-bending a reconstruction plate to near normal contour (Fig. 4b). The patient was then taken to the operating room where a resection and mandibular reconstruction procedure was performed. This patient’s postoperative course was complicated by an infection of the bone graft; however, she has subsequently undergone successful final reconstruction with re-grafting (Fig. 4c).
a SLA model demonstrating significant bony expansion of the mandible by a rapidly growing and extensive pathological lesion. b A reconstruction plate has been pre-bent and adapted on an osteoconductive framework which will later house the autogenous bone grafts. c Post-operative panoramic radiograph results of bone grafting with optimal bone volume
Case 5: Bone Tissue Engineering for Mandibular Augmentation
A 55-year old male was referred for treatment of refractory infection of the mandible. He gave a history of multiple (approximately nine) long bone fractures secondary to osteopetrosis. Clinical and radiographic evaluation revealed that this patient had sustained multiple compound mandible fractures. There was gross purulence present at the fracture sites. He had an underdeveloped alveolus, and multiple impacted teeth with bulbous roots. Due to the nature of this patient’s compromised medical condition (osteopetrosis), and dental and jaw condition (impacted teeth, poor oral hygiene, atrophic jaw bone), intermaxillary fixation and or autogenous bone grafting were not feasible options. This patient successfully underwent external pin fixation for stabilization of the fractures and resolution of infection. Next, a 3-D starch model was obtained (Fig. 5a) to assess the fractures as well as the other focal areas of deficiency in the mandible. A decision was made to reconstruct the regions of the fracture and the other deficient areas of the mandible using novel tissue engineering techniques.
a 3-DP starch model of the patient with fractured atrophic mandible and external pin fixation hardware. b Wax-up of the 3-D model has been completed. This wax up allowed for fabrication of custom scaffolds which served as carriers for the tissue engineering cells intraoperatively. c 8-year postopertaive panoramic radiograph showing successfully augmented mandible with bone-tissue engineering techniques
An initial surgical procedure was performed in the office under local anesthesia whereby a small sample of autogenous bone (approximately 1 cubic millimeter in size) was obtained from the patient’s mandibular ramus under local anesthesia. In vivo, these cells were then separated, expanded and cultivated into numerous new cells in a special laboratory. In addition, customized biodegradable PLGA scaffolds were fabricated based on the defects that were waxed-up on the 3-D model (Fig. 5b). At the time of reconstructive surgery, the laboratory-grown cells were then impregnated into the customized scaffolds, which were subsequently, surgically implanted and secured to the patients mandible with rigid fixation. Postoperative radiographic analysis showed healing of the fractures, excellent incorporation of the scaffolds into the mandible and an overall increase in the volume of normal and healthy appearing bone (Fig. 5c). At 8 years postoperatively, although the patient has had multiple other fractures of his long-bones, he has not suffered from any additional mandibular fractures.
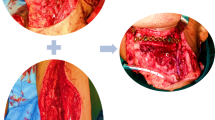
Case 6: Customized TMJ Reconstruction
A 55-year old man was referred for evaluation of his progressively worsening jaw function and progressive malocclusion. His past medical history was significant for rheumatoid arthritis that had affected multiple joints in his body including the TMJ’s. Clinical examination revealed severe mandibular retrusion and failure of previous TMJ reconstruction with extensive resorption of the mandibular rami bilaterally. Due to the destruction of the bilateral mandibular rami, it was decided to perform bone grafting to provide an adequate foundation for which to reconstruct the temporomandibular joint with TMJ prostheses. This patient’s 3-D model was extensively studied in order to determine the appropriate amount of advancement at pogonion that could be achieved, the appropriate mandibular ramus lengthening, and the deficit that would be created that would require bone grafting. Finally a wax-up was performed on the 3-D model to simulate the size and precise location of the cranial bone grafts needed (Fig. 6a). This exact simulation was replicated intraoperatively when placing the bone grafts and the TMJ prostheses (Fig. 6b). The fossa components were placed and secured with bone screws. The condylar prostheses were then secured to one of the cranial bone struts. A second cranial bone strut was then placed on the medial surface of the mandible. Bone screws were then placed through the prosthesis and both the medial and lateral bone grafts, thus sandwiching the native bone between the grafts. At the 9 years post-surgery follow-up examination, this patient had a stable occlusion, complete elimination of his obstructive sleep apnea, and a maximum inter-incisal opening of 33 mm [9].
a 3-D model has been waxed up to mimic normal bone contour of a mandibular ramus which has been destroyed multiple reconstructive surgical procedures in a patient affected with rheumatoid-induced TMJ disease. b Intraoperative view showing fixation of a patient-fitted, customized TMJ total joint replacement with an inlay cranial bone graft strut for simultaneous mandibular ramus reconstruction
Conclusions
SLA models have an important role in contemporary oral and maxillofacial surgery. As illustrated in the above-mentioned cases, they can be utilized in a variety of ways in the surgical arena. They are a useful tool to assess traumatic and pathologic defects requiring complicated surgery and reconstruction. They can be used for the fabrication of custom TMJ prostheses, and are effective tools to facilitate patient education and doctor to doctor communication. The specific types of 3-D model can be selected depending on the specific clinical indications. In our experience, the use of SLA models has significantly contributed to improved reconstruction of form and function, decreased operating room time due to advanced treatment planning, and ability to perform more precise and accurate surgical procedures.
References
Cunningham L, Madsen M, Peterson G (2005) Stereolithographic modeling technology applied to tumor resection. J Oral Maxillofac Surg 63:873–878
Chow L, Cheung L (2007) The usefulness of stereomodels in maxillofacial surgical management. J Oral Maxillofac Surg 65:2260–2268
Wong T, Fang J, Chung C, Huang J, Lee J (2005) Comparison of 2 methods of making surgical models for correction of facial asymmetry. J Oral Maxillofac Surg 63:200–208
Mazzoli A, Germani M, Moriconi G (2007) Application of optical digitizing techniques to evaluate the shape accuracy of anatomical models derived from computer tomography data. J Oral Maxillofac Surg 65:1410–1418
Schicho K, Figl M, Seemann R, Ewers R, Lambrecht JT, Wagner A, Watzinger F, Baumann A, Kainberger F, Fruehwald J, Klug C (2006) Accuracy of treatment planning based on stereolithography in computer assisted surgery. Med Phys 33(9):3408–3417
Fruhwald J, Schicho KA, Figl M, Benesch T, Watzinger F, Kainberger F (2008) Accuracy of craniofacial measurements: computed tomography and three-dimensional computed tomography compared with stereolithographic models. J Craniofac Surg 19(1):22–26
Barker TM, Earwaker WJS, Lisle DA (1994) Accuracy of stereolithographic models for human anatomy. Australas Radiol 38:106
Choi JY, Choi JH, Kim NK et al (2002) Analysis of errors in medical rapid prototyping models. Int J Oral Maxillofac Surg 31:23
Wolford L, Mehra P (2001) Simultaneous temporomandibular joint and mandibular reconstruction in an immunocompromised patient with rheumatoid arthritis: a case report with 7-year follow-up. J Oral Maxillofac Surg 59:345–350
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mehra, P., Miner, J., D’Innocenzo, R. et al. Use of 3-D Stereolithographic Models in Oral and Maxillofacial Surgery. J. Maxillofac. Oral Surg. 10, 6–13 (2011). https://doi.org/10.1007/s12663-011-0183-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-011-0183-3