Abstract
It is challenging to identify potential patients with acute coronary syndrome (ACS) in the emergency department (ED), although these cases should immediately undergo further evaluation in the observation unit. This study aimed to establish a new and rapid assessment system for triaging patients with potential ACS in the ED. Data from 1022 cases (June 2012–August 2015) were evaluated using latent class analysis to identify key symptoms and medical histories. Significant variables in the latent class analysis were entered as predictors for the new triaging system, and the final model was selected based on the false alarm rate, hit rate, and discriminability index. The new system provided better discriminability and significantly reduced the false alarm rate, compared to conventional methods. Our results indicate that symptom clustering analysis can facilitate the identification of potential ACS cases using a risk stratification system in the ED. The symptom clustering may facilitate a rapid assessment tool that reduces the costs of unnecessary diagnosis and hospitalization. Furthermore, this system might be developed as an application for embedding in ambient assisted living homes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Cardiovascular diseases were the top global causes of death during 2000–2015, with the proportion of global deaths due to cardiovascular diseases increasing from 27.7% in 2000 to 31.3% in 2015 out of all-cause mortality (World Health Organization 2018). Acute coronary syndrome (ACS) is a heart disease that is commonly encountered in the emergency department (ED), where observation units (OU) are used to admit patients with potential ACS and monitor them using non-invasive tests and diagnostic procedures (Hess et al. 2012; Simon et al. 2014). Early diagnosis of heart disease is the key to reducing patient mortality rates and can help reduce health care costs. Hospitals in Taiwan and throughout the world have developed triaging systems to determine whether patients with suspected ACS should be first admitted to the OU (e.g. Zarich et al. 2004; López et al. 2010). However, as missed diagnoses can lead to death, all current methods tend to admit patients with a low risk of ACS. This strategy results in a high false alarm rate that is associated with increased patient wait times, higher costs, and increased burden on healthcare providers. Therefore, triaging potential ACS patients prior to admission of OU is a great challenge for triage nurses and physicians in EDs.
As reported by Goodacre et al. (2005), in England and Wales, among all patients who presented with chest pain, 66% were admitted to the OU. Among those admitted, only 34.5% were clinically diagnosed with ACS. Admitting low-risk patients to the OU is a substantial burden for the healthcare sector of the United Kingdom. Thus, it would be useful to have a tool that could rapidly determine whether a patient should be admitted to the OU for further testing, while screening out patients with a very low risk of ACS.
The most conventional triage system is the chest pain method, which selects patients with non-traumatic chest pain or chest discomfort as potential ACS cases (Wright et al. 2011). In the OU, cases of suspected ACS with non-traumatic chest pain or discomfort undergo triage classification based on protocol-driven diagnostic testing (Wright et al. 2011). The protocol-driven diagnostic testing includes 12-lead electrocardiography (ECG), biomarker measurements, and treadmill tests. However, previous studies (Brieger et al. 2004; McNamara et al. 2010; Hess et al. 2012a, b; Rosenfeld et al. 2015) have indicated that chest pain/discomfort alone is inadequate for triaging potential ACS cases, as it is associated with a high false alarm rate and missed diagnoses in low-risk groups, such as female patients (Jayes et al. 1992; Rosengren et al. 2004) and young adults (Tungsubutra et al. 2007; Khan et al. 2013). Thus, studies have aimed to improve the triaging process using modifications of the chest pain strategy. For example, to reduce the high false alarm rate, Zarich et al. (2004) proposed only admitting patients to the OU if they were greater than 35-year-old or female patients who were greater than 40 years. Similarly, López et al. (2010) developed a flowchart process that discharged patients with chest pain from the ED using five conditions, including age of less than 40 years and the absence of diabetes, coronary artery disease history, non-oppressive pain, or retrosternal pain. Although these methods can reduce the false alarm rate, they cannot address the missed diagnoses in cases without chest pain. Moreover, patients can present with other non-thoracic symptoms, and the critical presenting symptoms can vary according to age and sex (Rosegengren et al. 2004). As the existing ACS triaging systems have limited accuracy for young or female patients (Chang et al. 2007; Kuhn et al. 2013), it may not be appropriate to rely on chest pain or a one-size-fits-all checklist for assessing patients for OU admission.
Recent studies have indicated that clinical data analysis can be useful in selecting key predictors for ACS screening and risk stratification system. For example, Kong et al. (2012) developed a system based on a belief-rule based system for classifying risk among patients with chest pain according to sex, age (greater than 40 years), worsening angina, and diabetes. In addition, Rosenfeld et al. (2015) used latent class analysis to evaluate data from patients with potential ACS, which revealed that chest pain/discomfort was not a significant symptom for 22% of the cases in a particular latent class; this group of patients typically experienced shortness of breath, unusual fatigue, and lightheadedness. Ryan et al. (2007) also reported that patients with myocardial infarction (MI) did not have symptom clusters that contained all typical symptoms. Nevertheless, both reports indicated that sex and age can predict risk classification, and Rosenfeld et al. (2015) suggested that further research was needed to develop a procedure that applies key symptom cluster-based predictors for improved ACS risk classification. More recently, Ahmadi et al. (2017) implemented the neural network and decision tree to develop a clinical decision support system for predicting coronary artery disease in patients. However, they did not demonstrate the efficacy of their model when compared to other current practices.
Challenges in diagnosing ACS involve the high costs of ED assessments, as well as the possibility of misdiagnosis, which can lead to missed treatment opportunities and poor outcomes. Therefore, the present study aimed to improve existing triaging systems using key presenting symptoms and medical histories, which were identified using latent class analysis. Additionally, we aimed to use symptom clustering to further improve the ACS triaging system. As we hypothesized that symptom clusters, detected by using latent class analysis, could help us to extract key predictors of a potential ACS patient and consequentially improve the risk stratification in the ED. In this context, latent class analysis considers the patient’s presenting symptoms and medical histories, as well as their interactions with the ED physician’s final diagnosis at discharge from the ED. This approach could be implemented to create a more effective triaging system for the admission process to the OU that can operate without triaging nurses and ED physicians. The final new Heart Broken Index (HBI) checklist can be implemented at the front desk of the ED in hospitals worldwide as well as in the ambient living system where the triaging of potential ACS patient starts; in other words, it can start at the patient’s home rather than at the ED department.
The remaining sections of this paper are constructed as follows: In Sect. 2, we summarize the data collection strategy and how we proceeded with the data analysis. In Sect. 6, we present the results of the data analysis and evaluate the efficiency of the purposed method. In Sect. 4, we discuss the clinical applicability of our findings and the limitations of this study. In Sect. 5, we summarize the major contributions of this study.
2 Methods
2.1 Study design and setting
The present study is part of a longitudinal study that is being performed in collaboration with the Far Eastern Memorial Hospital (Northern Taiwan), which is a 1000-bed regional teaching hospital with a percutaneous coronary intervention center and an ED that serves more than 400 patients per day. The ED has performed various projects to improve patient processing, modify bottle-neck processes, and improve the triaging system for directing patients to the OU. The current HBI was developed at this center (Hsu et al. 2011; Chen et al. 2012), and considers four criteria: age of > 30 years with chest discomfort (2 points), epigastric pain/epigastralgia (1 point), cold sweating (1 point), and dyspnea (1 point). This system is implemented at the triaging station to shorten wait times, and patients with a score of greater or equal to 2 points are admitted to the OU. Although the existing HBI provides a high hit rate (98.39%), it also has a high false alarm rate (92.23%), which increases wait times and medical expenses in the ED. Therefore, the present study aimed to re-design the HBI to reduce its false alarm rate and more rapidly classify cases of suspected ACS. The study’s protocol was approved by the institutional ethics review board, and no personal data were retained as part of the study.
2.2 Data collection
For our study, we included patients who visited the ED of the Far Eastern Memorial Hospital between June 2012 and August 2015. All non-traumatic adult patients who were older than 18 years of age and who presented with at least one symptom or a medical history related to ACS (see Table 1) were included. A total of 1022 patients were randomly selected from a total of 10,184 that satisfied the abovementioned criteria. Data were collected by ED nurses, who randomly retrieved the medical records and transferred the relevant information into a Google form. For each case, sex, age, medical history (heart disease, diabetes, hypertension, and kidney disease), presenting symptoms at the ED, and diagnosis before discharge from the ED were recorded. Age was recorded as a continuous variable, and all other data were recorded in a binary format.
Several pre-analysis tasks were performed before the latent analyses. Since the patients’ symptoms had been recorded by various ED physicians at different times using different names and formats, the ED physician on our research team categorized and summarized all symptoms using combined and standardized names. For example, as shown in Table 1, “chest discomfort” included chest pain, chest discomfort, chest heaviness, chest pressure, chest tightness, and chest compression. As another example, shock encompassed pallor, shock, and diaphoresis. Furthermore, based on the final diagnosis of each patient, the ED physician decided whether a patient should have been suspected as having ACS. Potential ACS patients were those diagnosed with ACS, acute myocardial infarction (AMI), myocardial infarction (MI), ST-segment elevation myocardial infarction (STEMI), non-ST-segment elevation myocardial infarction (NSTEMI), and unstable angina (UA).
2.3 Data analysis and validation
The current HBI triaging system is a self-developed system for the ED that is based on ED physicians’ domain knowledge, clinical experiences, and previous research. To complement the physicians’ domain knowledge, we collected the patients’ characteristics and medical histories, which were used to create symptom clusters that could be objectively evaluated using latent class analysis. This approach allowed us to extract data regarding the key predictors for triaging potential ACS cases, which served as the foundation for the new HBI system.
Latent class analysis is a mixed model that is commonly applied to screen for and identify clinically important factors (Whitson et al. 2016), and it has been used in numerous disease-specific studies (DeVon et al. 2010; Mahr et al. 2013; Rosenfeld et al. 2015; Divon et al. 2016; Lunt et al. 2016). As most variables were treated as binary variables, latent class analysis can consider multiple possible causes and determine the optimal number of classes using objective criteria (e.g., the Akaike information classification [AIC] and/or Bayesian information classification [BIC]) or subjective criteria (e.g., class interpretability). Furthermore, as the presenting symptoms of ACS vary according to sex (Rosenfeld et al. 2015) and age (Halon et al. 2004; Tungsubutra et al. 2007), the present study classified the patients using those variables. To group young and old patients, previous studies (Zarich et al. 2004; Tungsubutra et al. 2007; López et al. 2010) have specified age cutoff values of 34, 45, and 40 years. We chose the cutoff value of 45 years used in the study of Tungsubutra et al. (2007) for two reasons. First, Tungsubutra et al. (2007) conducted their study in Thailand, which shares similar geographic characteristics and biologic characteristics in the population with Taiwan (where the data was collected and the target hospital is located). The other reason is that the study conducted by Tungsubutra et al. (2007) had a similar objective as that in our study. The authors focused on investigating the difference in presenting symptoms between young and old patients. The admission threshold score of the new HBI checklist remained the same (2 points). The development steps for the new triaging system are shown below:
Step 1 The patients’ presenting symptoms and medical histories were collected.
Step 2 The patients were categorized into four subgroups: (1) men who were ≥ 45-year-old, (2) men who were < 45-year-old, (3) women who were ≥ 45-year-old, and (4) women who were < 45-year-old.
Step 3 The latent class analysis was performed for each subgroup, with the ED physicians’ diagnoses (i.e., admit to the OU or not) as the grouping variable and the presenting symptoms and medical histories as the model features.
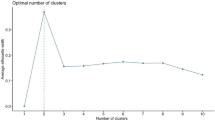
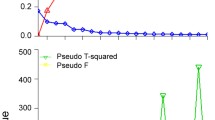
Step 4 The optimal number of classes was selected based on the best AIC and BIC values. For example, if the optimal numbers of classes for ≥ 45-year-old women were three for AIC and four for BIC, we recoded the latent classification results of both three-class clusters and four-class clusters before proceeding to step 5.
Step 5 The significant presenting symptoms and medical histories of each subgroup were extracted as possible predictors to include in the new HBI checklist of that group. To determine which predictor is significant, we develop three selection rules. The first two rules aimed to identify indicators associated with patients who should be admitted into the OU. The third rule aimed to identify indicators associated with patients who should not be admitted into the OU. First, features in each latent class of patients who should be admitted to the OU with an occurrence probability ≥ 0.55 were assigned a weighted score of 1 s, variables with a moderate occurrence probability among patients who should be admitted to the OU, and a low occurrence probability (< 0.1) for patients who should not be admitted to the OU, were also assigned a weighted score of 1. The symptoms designated a weighted score of 1 were potential indicators associated with patients who should be admitted to the OU. Once these potential indicators were found, we proceeded to step 6.
Step 6 For the third rule, variables with a moderate occurrence probability (> 0.1) among patients who should not be admitted to the OU and an extremely low occurrence probability (< 0.05) among patients who should be admitted to the OU, were assigned a weighted score of − 1. In contrast to the first two rules, the third rule aimed to search for symptoms which might indicate the patients belong to a low-risk group of ACS. Therefore, a negative weight was assigned to symptoms selected by rule 3.
Step 7 Although the weighted score for chest discomfort was set to 2 based on the existing HBI, the weighted score of chest discomfort was designed to match the threshold score of admitting a patient into the OU. This implies that a patient who presented to the ED with chest discomfort would be recognized as a potential ACS patient; this complies with the chest discomfort strategy purposed by America Heart Association (Wright et al. 2011). The weighted score of these three rules were designed so that presenting symptoms and medical histories served as minor factors, and chest discomfort served as a dominating exclusion or inclusion factor(s). After the variables were selected, the new HBI system was generated based on the selected variables. The combination of variables with the best predictability, based on their weighted scores from step 6, was selected as the final model. The total score was calculated for each person, and the decision regarding whether to admit the patient to the OU was guided by Eq. (2):
Step 8 As chest discomfort was common among all patients, this variable was non-significant in the logistics regression equation. Thus, we searched all combinations of selected features plus a weighted score of 2 for chest discomfort. The signal and detection theory (Green and Swets 1966) was implemented to quantify the discriminability of these combinations, with the results being calculated for the discriminability index (d′), the hit rate, and the false alarm rate. The formula for calculating the discriminability index is shown in Eq. (3) below. More significantly, the initial combination content all significant predictors and the best combination of the variables are selected by eliminating the variable which will reduce the discriminability index. We refer to this as the backward selection method. The combinations with the best discriminability and highest hit rate were recorded, although the checklist was limited to a maximum of six features to ensure that it is simple enough to use in the ED.
where \({\Phi ^{ - 1}}( \cdot )\) is an inverse function of the standard normal distribution.
Step 9 The d′ values were compared for the new system, the current HBI system, and the chest pain strategy.
3 Results
3.1 Clinical case analyses
Among the 1022 included cases, the clinical case analyses identified 43 symptoms and 6 diagnoses (unstable angina: 0.5%, MI: 0.6%, non-ST-segment elevation myocardial infarction: 0.7%, ST-segment elevation myocardial infarction: 1.5%, AMI: 2.4%, and ACS: 12.1%). These six diagnoses provided an overall signal rate of 17.8%. The 43 symptoms were compiled into eight symptom clusters: chest discomfort, acute heart failure, difficulty breathing, pallor and sweating, neurological symptoms, shock, nausea, and proximal radiation of pain (Table 1). The medical histories included hypertension, diabetes, kidney disease, and heart disease. These data allowed us to identify most expressive variables which influencing the risk stratification of patients who should and should not be admitted to the OU for further testing in latent classification clusters.
Age- and sex-specific classifications were performed for the included patients. Young adults (< 45-year-old) were classified as having a low risk of ACS in the presence of atypical presenting symptoms or no medical history. Table 2 shows the eight presenting symptoms and four medical histories with the highest frequencies and occurrences.
3.2 Latent class analyses and extracted symptoms
The goodness-of-fit of the latent class analysis model for each subgroup was examined for models with 3, 4, 5, 6, and 7 classes. The optimal number of classes was selected based on the AIC/BIC values (e.g., the lowest AIC was observed for five classes, while the lowest BIC was observed for three classes among women who were ≥ 45-year-old). The proportions of latent classes for each latent class analysis subgroup are summarized in Table 3, along with the incidence of the occurrences of the chest discomfort. The effects of age and sex on symptom clustering was evaluated for male/female patients and young/old patients (Table 2). The results indicate that sex was a significant predictor of latent class, thus each latent class was investigated individually.
Table 3 shows that chest discomfort/pain was a significant factor in all latent classes across all subgroups. Tables 4, 5 and 6 summarize the occurrence rates of each symptom in all latent classes selected by AIC or BIC values.
3.3 Extracted symptoms and new HBI checklist
Tables 4, 5 and 6 indicate the key predictors (in boldface for significant predictors) that were selected in steps 5 and 6 in Sect. 2.3. More specifically, predictors selected by rules 1 and 2 for ACS were assigned positive scores (as summarized in Table 7), whereas symptoms of very-low-risk patients who generally should not be admitted to the OU (rule 3) were assigned negative scores (as summarized in Table 8). Although a history of heart disease had a relatively low occurrence rate among patients who should be admitted to the OU, it is a widely recognized risk factor for potential ACS, and thus it was assigned an initial score of 1.
The backward selection method indicated in Sect. 2.3 was used to select significant symptoms and medical histories. This approach required that the final model include less than six presenting symptoms or medical histories for each new HBI checklist, as well as a false alarm rate that was less than that of the original HBI checklist. Our final model (the new HBI checklist), original HBI checklist, and the chest pain strategy were subsequently evaluated using the signal and detection theory to compare their discriminability. The hit rates, false alarm rates, and d′ values are shown in Table 9.
Figure 1 shows the two sets of the new proposed checklists, which were selected based on a high d′ value (checklist 1) and a low false alarm rate (checklist 2). The only difference between these two checklists was whether ≥ 45-year-old men were admitted to the OU if they present with non-traumatic chest pain, and the checklists were identical for the three remaining subgroups. The patient flow and critical symptoms for the new triaging system of a potential ACS patient who should be admitted to OU is shown in Fig. 1. Since the final HBI checklist will be embedded in the computer system at the front desk or portable device for the triaging nurse, the triaging nurse need only to input the age, sex, and symptoms as shown in Fig. 1. As the symptom list appears, the nurse can check if a patient presents with the listed symptoms, then the computer automatically calculates the score and determines if the patient should be admitted to the OU.
4 Discussion
The extracted symptoms and medical histories obtained in our results were significantly different from those in the existing HBI checklist. The selected key symptoms and medical histories show that young and old patient groups should use different HBI checklists. For example, younger patients generally had atypical symptoms, such as nausea and proximal radiation pain. Cardiac disease-related history (e.g., hypertension, diabetes, and heart disease) was a significant predictor among older women and young men. In the final model, a history of heart disease and acute heart failure were significant risk factors for older women and young men, and these variables were not considered in the original HBI checklist. In Table 2, significantly different occurrence rates of presenting symptoms were noted between sexes. For the same sex, the occurrence rates of presenting symptoms were also different between young and old patients, suggesting that sex and age were both strong predictors of class membership. Furthermore, we observed from the latent class analyses in Tables 4, 5 and 6 that the predictors in the new HBI checklist, which were selected by the proposed method for each subgroup, should be significantly different. For example, Table 4 indicated that for older women, shock had an occurrence rate of 93.31% in cluster 3 for patients who should be admitted to the OU. Hence, according to rule 1 of step 5 in Sect. 2.3, hypertension was selected as one of the positive predictors of admission to the OU. In contrast, Table 6 indicated that for young women, shock had an extremely low (0%) occurrence rate across all clusters for patients who should be admitted to the OU, but had a high occurrence rate for cluster 3 (92.33%) of patients who should not be admitted to the OU. Hence, shock was selected as one of the potential negative predictors for the new HBI list for young women according to rule 3 of step 6 in Sect. 2.3. Therefore, from the latent class analyses, we concluded that the subgroups should not share the same HBI checklist, since not all subgroups had the same predictors of potential ACS.
4.1 Predictors for patients who should to be admitted into the OU
As shown in Fig. 1, the predictors of subgroups were significantly different. However, from Table 9, we can observe that the chest pain strategy is a simple and effective strategy for men aged > 45 years. Thus, in this subsection, we focus on predictors that are not traditionally considered. Women aged > 45 years and men aged < 45 years were appointed four positive weighted predictors for admission to the OU. In addition, hypertension and a history of heart disease contributed to positive weighted scores for older patients and young men (see Table 7), but not for young women. Shock was the only significant symptom found for older women. Our results are consistent with those of studies that have identified a number of positive predictors for women (see Table 7). However, in the final new HBI checklists shown in Fig. 1, we found that the only significant positive predictor for young women was chest discomfort. This might indicate that even women report more presenting symptoms. For young women, most of the presenting symptoms were not effective predictors of potential ACS. A study conducted by Canto et al. (2007) indicated that women appear to report more presenting symptoms (2.6 on average) compared to that in men (1.8 on average) and are more likely to present without chest pain. In contrast, a study by Rosenfeld et al. (2015) reported that women of all ages are more likely to report chest pain and discomfort with symptoms associated with acute heart failure (dyspnea, shortness of breath, and cough). In our study, young women did not exhibit the behavior of reporting more ACS predictors. This might be due to the fact that pre-menopausal women have a very low risk of ACS, and there was a limited number of cases in the current data set. The problem of underrepresentation of young women is discussed in Sect. 4.6.
Young men also exhibit significantly more predictors in the new HBI checklist (see Fig. 1), compared to that of other subgroups. In this context, young men have a low incidence of previous heart disease, which is a significant predictor of potential ACS in the ED. Our results from the latent class analysis are consistent with those of Schoenenberger et al. (2011) and Fournier et al. (1996); these studies reported that a history of heart disease was a risk factor for ACS among young men. Thus, our results indicate that a latent class analysis can effectively isolate key risk factors that might otherwise be overlooked.
4.2 Predictors for patients who should not to be admitted into the OU
In this study, we introduced a new set of predictors that can help identify symptoms among patients who should not be admitted into the OU. These predictors included pallor, sweating, and nausea across both age groups of women. Traditionally, these symptoms are considered predictors of potential ACS. Our contradictory result may be explained by sex differences and the low occurrence rate of ACS among women. DeVon et al. (2008) investigated the difference in ACS symptoms among men and women and they found that while women were more likely to report nausea, the dizziness (which is one of the presenting symptoms of nausea) is a significant predictor associated with men who experience MI (type of ACS) rather than women. In contrast, women with UA and MI are more likely to report weakness and cough (both are associated with acute heart failure). Our new HBI checklist is consistent with the findings of DeVon et al. (2008), who suggested that nausea is not a significant indicator of ACS for women.
Women, especially those who are premenopausal, have a low risk of developing ACS when compared to that of men (Maas and Appelman 2010). In addition, we found that young women had fewer significant predictors but more negatively weighted predictors, compared to other subgroups (Tables 7, 8), which is inconsistent with the previous literature (e.g. Rosenfeld et al. 2015). This might be because the number of clinical cases of young women with ACS is low. The final model revealed that young women who presented with chest discomfort along with pallor and sweating or nausea represented a group of patients at very-low-risk patients for developing ACS. As Tungsubutra et al. (2007) and Mass and Appelman (2010) stated in their studies, ACS among young patients (< 45 years) is more likely to be associated with personal characteristics such as smoking, obesity, and family history, rather than the preceding angina. Amsterdam et al. (2010) also stated that the false alarm rate for ACS among younger patients is very high; these researchers reported that among 220 young patients (< 40 years) admitted into the OU, only six of them were suspected to have ACS according to the diagnostic tests. Among all six of these patients, none were confirmed to have ACS. These results may explain the higher number of negative predictors for the young patients.
4.3 The final model’s effectiveness
We developed two new HBI checklists based on the hit rate, false alarm rate, and d′ value (Table 9), with checklist 1 providing a better d′ value and checklist 2 providing a better false alarm rate, compared to the rates using the chest pain strategy. In addition, checklist 1 reduced the false alarm rate by 5.8% compared to the current HBI checklist and reduced the false alarm rate by 10.65% compared to the chest pain strategy. Furthermore, checklist 2 provided a perfect hit rate and reduced the false alarm rate by 2.2% compared to the current HBI checklist and reduced the false alarm rate by 6.65% compared to the chest pain strategy. Moreover, the current HBI checklist had poorer results for the hit rate and false alarm rates among young men, compared to that of checklist 1. This result is problematic, as a misdiagnosis of younger men is associated with poor outcomes. Tungsubutra et al. (2007) reported that younger men were more likely to have high-risk types of ACS (e.g., STEMI) compared to that of older men and women. Thus, our new checklists perform better for women and young men, compared to the current checklist, with similar performance for older men.
4.4 Future study and applications in an ambient assisted living environment
Although the present study primarily aimed to create a new HBI system, our findings lay the foundation for developing a self-triaging system in the ambient assisted living setting. Previous reports have indicated that telemedicine and home-healthcare are inevitable avenues of progress, especially for elderly individuals (O’Grady et al. 2010; Li 2013). Thus, it will be important to integrate diagnostic, triaging, and/or assessment systems into smart homes. Wang et al. (2010) have proposed a healthcare application that connects nutritional experts and the patient to improve their eating habits. Furthermore, elderly individuals have a high risk of ACS and other cardiac syndrome and may benefit from ambient assisted living settings, as Halon et al. (2004) found a lower mortality rate among ≥ 80-year-old patients with ACS compared to the rate among ≥ 70-year-old patients. Therefore, the new HBI checklist can also serve as an alarm system that determines if the results of a critical non-inventive tests (such as a 12-lead ECG, which is recorded for old patients on a daily basis in a smart home Hussein et al. 2017) should be transferred to the hospital and examined in real time. Thus, our new HBI checklist App and the ECG in smart homes can be simultaneously used for triage if a patient needs to be admitted to the OU. Therefore, we speculate that our new HBI checklist could be incorporated into downloadable applications for mobile devices, which could potentially allow elderly patients to provide data for ACS triaging from their home (Fig. 2). The new HBI checklist only assesses presenting symptoms that can be easy identified by motion sensors in the smart home or heart rate and blood pleasure from a smart bracelet (Amiribesheli et al. 2015). An early start to the triaging process with the help of an application would likely reduce the door-to-ECG time and the mortality rate among elderly patients (Diercks et al. 2006). The implementation process is split into two stages. The first stage is called “HBI ambient system development” stage, in which the HBI checklist is constructed based on the method proposed in Sect. 2.3. The final HBI checklist is then packaged as a downloadable APP/APK and embedded in the smart home or device (Fig. 2). The second stage “embedded in ambient assisted living system” is where the checklist assesses the patient’s motion, heart rate, and other critical symptoms in real time. The application will alarm the ED if the total score excessed the threshold.
4.5 Contributions
The present study provides three important contributions. First, we created a new HBI checklist based on latent analysis, which provided significant improvements in the hit and false alarm rates. These improvements could help decrease wait times, treatment costs, and the burden on healthcare providers. For example, the standard diagnostic time for the 12-lead ECG is 10 min (c.f. Lee et al. 2013; Acute Coronary Syndromes Algorithm 2018). Our new HBI checklist can reduce the overall false alarm rate by 6.2% and consequentially save 634 min of diagnostic time with our current data of 1022 patients. Second, we developed a general procedure for applying symptom clustering in improving triaging tools. Third, our findings lay the foundation for application-based triaging in the ambient assisted living setting, as the new HBI checklists can be incorporated into applications that allow users to perform periodic updates, which can then be used during the triaging process. These applications would be expected to decrease wait times and improve the mortality rate among this high-risk population (Cannon et al. 2000). In addition, our new HBI triaging list can be easily implemented in an ambient assist living system.
4.6 Limitations
Despite providing a simple and effective procedure to use latent classes in a triaging system, the present study also has several limitations. First, we only selected patients with at least one ACS-related symptom (see Table 1), and it is possible that we did not include enough patients with atypical symptoms. Furthermore, the retrospective data used in this study might have limitations regarding the comprehensive symptoms of a patient. For example, in an extremely busy situation, an ED physician might record critical symptoms and ignore minor symptoms once she/he felt confident about making the triaging decision. However, this limitation may have had little effect on our model development since ED physicians rarely neglect any symptoms when patients arrive at the ED. Second, since this study focused on triaging for admission to the OU at the ED, we only collected the patient’s presenting symptoms and medical history but did not include other risk factors of ACS such as smoking, obesity, race, and family history. However, the patient’s habits such as smoking and genetic characteristics such as race and family history might not be available as the patient arrives the emergency department. More specifically, as discussed in Sect. 4.2, previous literature (Mass and Appelman 2010; Tungsubutra et al. 2007; Amsterdam et al. 2010) indicates that these risk factors are more predominant in young patients and women than in older patients. This information might greatly improve the accuracy of the OU admission checklist that is currently used in ambient living systems. Thus, to improve the applicability of the purposed method for ambient living systems, the user should add these risk factors into the data analysis.
Third, the decision of whether the patient should have been admitted to the ED was made by an ED physician, who tend to overestimate the patient’s risk of ACS, compared to a cardiologist who uses the same scoring system (Wu et al. 2017). Thus, the ED physician’s diagnosis may not be consistent with the final diagnosis at their discharge. Fourth, the random case selection process provided a smaller group of female patients, especially young female patients, compared to male patients. As previous literature has indicated, young patients and woman are typically underrepresented. Therefore, the results might not represent the population due to the limited number of patients.
These limitations point towards several avenues for future research. First, unequal sampling may be needed to provide more representative data from female or young patients to train ACS triaging models. Second, the patient’s final diagnosis at discharge could be used to define their group assignment. Third, logistic regression analysis may be useful to develop a prediction model that overcomes the extraordinarily high occurrence of chest pain or discomfort in this setting. Fourth, in constructing an ambient living system, personal behaviors such as smoking, diet and/or family medical history can be included as risk factors to improve the predictability of woman and young ACS patients.
5 Conclusions
In developed and emerging countries, heart disease is one of the ten leading causes of death. In this study, we aimed to assist ED physicians in developing a triaging system to determine who should enter the OU for further inspection of ACS. Our study identified and applied symptom clustering to develop a system for determining whether patients with potential ACS should or should not be admitted to the OU. The new OU triaging system consists of four HBI checklists for age- and sex-specific subgroups, which provide better performances in these subgroups, compared to that of existing methods. The average hit rate is 99.27%, and the average false alarm rate is 86.03% for the new HBI checklist 1, which is significantly better compared to the 98.39% hit rate and 92.23% false alarm rate of the current HBI checklist. Furthermore, the new system appears to be more accurate for triaging patients at the ED in our hospital, as it had better overall performance (d′ = 1.240 and 3.017 vs. 2.419 for the chest pain strategy and 0.721 for the current HBI checklist). Therefore, our system provides an enhanced ability to identify and triage patients with potential ACS in the ED. Moreover, our system may be useful in a self-triaging application that could be used in the ambient assisted living setting.
References
Acute Coronary Syndromes Algorithm (2018) Using the acute coronary syndromes algorithm for managing the patient. https://www.acls.net/acute-coronary-syndromes-algorithm.htm. Accessed 11 April 2018
Ahmadi E, Weckman GR, Masel DT (2017) Decision making model to predict presence of coronary artery disease using neural network and C5.0 decision tree. J Ambient Intell Humaniz Comput. https://doi.org/10.1007/s12652-017-0499-z
Amiribesheli M, Benmansour A, Bouchachia A (2015) A review of smart homes in healthcare. J Ambient Intell Humaniz Comput 6(4):495–517
Amsterdam EA, Kirk JD, Bluemke DA et al (2010) Testing of low-risk patients presenting to the emergency department with chest pain a scientific statement from the American Heart Association. Circulation 122(17):1756–1776
Brieger D, Eagle KA, Goodman SG et al (2004) Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest 126:46146–46149
Cannon CP, Gibson CM, Lambrew CT et al (2000) Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 283:2941–2947
Canto JG, Goldberg RJ, Hand MM, Bonow RO, Sopko G, Pepine CJ, Long T (2007) Symptom presentation of women with acute coronary syndromes: myth vs. reality. Arch Intern Med 167(22):2405–2413
Chang AM, Mumma B, Sease KL et al (2007) Gender bias in cardiovascular testing persists after adjustment for presenting characteristics and cardiac risk. Soc Acad Emerg Med 14(7):599–605
Chen KC, Hsu JC, Cheng IN et al (2012) Using presenting symptoms to revise the “heart-broken index” for the triage of acute myocardial infarction. APSC Subspecialty Congress Intervention and Imaging 2012. Taipei International Convention Center, Taipei, pp 1–78
DeVon HA, Ryan CJ, Ochs AL, Shapiro M (2008) Symptoms across the continuum of acute coronary syndromes: differences between women and men. Am J Crit Care 17(1):14–24
DeVon HA, Ryan CJ, Rankin SH, Cooper BA (2010) Classifying subgroups of patients with symptoms of acute coronary syndromes: a cluster analysis. Res Nurs Health 33(5):386–397
Diercks DB, Kirk JD, Lindsell CJ et al (2006) Door-to-ECG time in patients with chest pain presenting to the ED. Am J Emerg Med 24:1–7
Divo M, Casanova C, Marin JM, Celli B, de Torres JP, Polverino F et al (2016) Identification of clinical phenotypes in patients with and without COPD using cluster analysis. Eur Respir J 48(suppl 60):4613
Fournier JA, Sanchez A, Quero J, Fernandez-Cortacero JAP, González-Barrero A (1996) Myocardial infarction in men aged 40 years or less: a prospective clinical-angiographic study. Clin Cardiol 19:631–636
Goodacre S, Cross E, Arnold J, Angelini K, Capewell S, Nicholl J (2005) The health care burden of acute chest pain. Heart 91(2):229–230
Green DM, Swets JA (1966) Signal detection theory and psychophysics. Wiley, New York
Halon DA, Adawi S, Dobrecky-Mery I, Lewis BS (2004) Importance of increasing age on the presentation and outcome of acute coronary syndromes in elderly patients. J Am Coll Cardiol 43(3):346–532
Hess EP, Brison RJ, Perry JJ et al (2012a) Development of a clinical prediction rule for 30-day cardiac events in emergency department patients with chest pain and possible acute coronary syndrome. Ann Emerg Med 59:115–125
Hess EP, Knoedler MA, Shah ND, Kline JA, Breslin M, Branda ME et al (2012b) The chest pain choice decision aid. Circ Cardiovasc Qual Outcomes 5(3):251–259
Hsu J-C, Chen K-C, Cheng I-N, Li A-H (2011) Using heart broken index to improve the diagnostic accuracy of patient with STEMI and shorten door-to-balloon time on emergency department. American Heart Association 2011 Scientific Sessions, Orlando
Hussein AF, Hashim SJ, Aziz AFA, Rokhani FZ, Adnan WAW (2017) A real time ECG data compression scheme for enhanced bluetooth low energy ECG system power consumption. J Ambient Intell Humaniz Comput 1–14
Jayes RL, Beshansky JR, D’Agostino RB, Selker HP (1992) Do patients’ coronary risk factor reports predict acute cardiac ischemia in the emergency department? A multicenter study. J Clin Epidemiol 45:621–626
Khan NA, Daskalopoulou SS, Karp I, Eisenberg MJ, Pelletier R, Tsadok MA et al (2013) Sex differences in acute coronary syndrome symptom presentation in young patients. JAMA Intern Med 173(20):1863–1871
Kong A, Frigge ML, Masson G, Besenbacher S, Sulem P, Magnusson G et al (2012) Rate of de novo mutations and the importance of father’s age to disease risk. Nature 488(7412):471
Kuhn JE, Dunn WR, Sanders R, An Q, Baumgarten KM, Bishop JY et al (2013) Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg 22(10):1371–1379
Lee YF, Hu SC, Lai HL (2013) A comparison of the quality of emergency care for acute coronary syndromes before and after accreditation of emergency medical competency. Tzu Chi Nurs J 12(3):66
Li K-F (2013) Smart home technology for telemedicine and emergency management. J Ambient Intell Humaniz Comput 4:535–546
López B, Sánchez M, Bragulat E, Jiménez S, Coll-Vinent B, Ortega M et al (2010) Validation of a triage flowchart to rule out acute coronary syndrome. Emerg Med J 28:841–846
Lunt A, McGhee E, Rees D, Height S, Rafferty G, Thein SL, Greenough A (2016) Cluster analysis and lung function in sickle cell disease. Eur Respir J 48(suppl 60):2234
Maas AHEM, Appelman YEA (2010) Gender differences in coronary heart disease. Neth Heart J 18(12):598–603
Mahr A, Katsahian S, Varet H, Guillevin L, Hagen EC, Höglund P et al (2013) Revisiting the classification of clinical phenotypes of anti-neutrophil cytoplasmic antibody-associated vasculitis: a cluster analysis. Ann Rheum Dis 72(6):1003–1010
McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ et al (2006) Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 47:2180–2186
O’Grady MJ, Muldoon C, Dragone M, Tynan R, O’Hare GM (2010) Towards evolutionary ambient assisted living systems. J Ambient Intell Humaniz Comput 1:15–29
Rosenfeld AG, Knight EP, Steffen A, Burke L, Daya M, Devon HA (2015) Symptom clusters in patients presenting to the emergency department with possible acute coronary syndrome differ by sex, age, and discharge diagnosis. Heart Lung J Acute Crit Care 44:368–375
Rosengren A, Wallentin L, Gitt AK, Behar S, Battler A, Hasdai D (2004) Sex, age, and clinical presentation of acute coronary syndromes. Eur Heart J 25(8):663–670
Ryan CJ, DeVon HA, Horne R et al (2007) Symptom clusters in acute myocardial infarction: a secondary data analysis. Nurs Res 56(2):72–81
Schoenenberger AW, Radovanovic D, Stauffer JC, Windecker S, Urban P, Niedermaier G, Plus Investigators AMIS et al (2011) Acute coronary syndromes in young patients: presentation, treatment and outcome. Int J Cardiol 148:300–304
Simon EL, Griffin P, Medepalli K et al (2014) Door-to-balloon times from freestanding emergency departments meet ST-segment elevation myocardial infarction reperfusion guidelines. J Emerg Med 46:734–740
Tungsubutra W, Tresukosol D, Buddhari W, Boonsom W, Sanguanwang S, Srichaiveth B (2007) Acute coronary syndrome in young adults: the Thai ACS Registry. J Med Assoc Thai 90(Suppl 1):81–90
Wang M-H, Lee C-S, Hsieh K-L, Hsu C-Y, Acampora G, Chang C-C (2010) Ontology-based multi-agents for intelligent healthcare. J Ambient Intell Humaniz Comput 1:111–131
Whitson HE, Johnson KS, Sloane R, Cigolle CT, Pieper CF, Landerman L, Hastings SN (2016) Identifying patterns of multimorbidity in older Americans: application of latent class analysis. J Am Geriatr Soc 64(8):1668–1673
World Health Organization (2018) The top 20 causes of death. http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html. Accessed 10 April 2018
Wright RS, Anderson JL, Adams CD, Bridges CR, Casey DE, Ettinger SM et al (2011) 2011 ACCF/AHA focused update incorporated into the ACC/AHA 2007 guidelines for the management of patients with unstable angina/non–ST-elevation myocardial infarction: a report of the American college of cardiology foundation/American heart association task force on practice guidelines. J Am Coll Cardiol 57:215–367
Wu J, Platero-Luengo A, Sakurai M, Sugawara A, Gil MA, Yamauchi T et al (2017) Interspecies chimerism with mammalian pluripotent stem cells. Cell 168(3):473–486
Zarich SW, Sachdeva R, Fishman R et al (2004) Effectiveness of a multidisciplinary quality improvement initiative in reducing door-to-balloon times in primary angioplasty. J Interv Cardiol 17:191–195
Acknowledgements
This research was supported by funding from the Taiwan Ministry of Science and Technology (MOST103-2221-E-155-053-MY3). We thank Pei-Li Chung and Ming-Fen Guo for performing the data collection.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, C., Lin, R.F., Huang, TC. et al. A symptom cluster-based triaging system for patients presenting to the emergency department with possible acute coronary syndromes. J Ambient Intell Human Comput 14, 14595–14609 (2023). https://doi.org/10.1007/s12652-018-0907-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12652-018-0907-z