Abstract
Major depression disorder is one of the most common psychiatric disorders that greatly threaten the mental health of a large population worldwide. Previous studies have shown that endoplasmic reticulum (ER) stress plays an important role in the pathophysiology of depression, and current research suggests that brain-derived neurotrophic factor precursor (proBDNF) is involved in the development of depression. However, the relationship between ER and proBDNF in the pathophysiology of depression is not well elucidated. Here, we treated primary hippocampal neurons of mice with corticosterone (CORT) and evaluated the relationship between proBDNF and ERS. Our results showed that CORT induced ERS and upregulated the expression of proBDNF and its receptor, Follistatin-like protein 4 (FSTL4), which contributed to significantly decreased neuronal viability and expression of synaptic-related proteins including NR2A, PSD95, and SYN. Anti-proBDNF neutralization and ISRIB (an inhibitor of the ERS) treatment, respectively, protected neuronal viabilities and increased the expression of synaptic-related proteins in corticosterone-exposed neurons. ISRIB treatment reduced the expression of proBDNF and FSTL4, whereas anti-proBDNF treatment did not affect ERS markers (Grp78, p-PERK, ATF4) expression. Our study presented evidence that CORT-induced ERS negatively regulated the neuronal viability and the level of synaptic-related protein of primary neurons via the proBDNF/FSTL4 pathway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depressive disorder (MDD) is a common psychiatric illness that seriously affects social function and reduces patients’ quality of life (Malhi and Mann 2018; Smith 2014). Chronic stress is considered a predominant trigger of depression (Roozendaal et al. 2009), which brings about the over-activation of hypothalamic-pituitary-adrenal (HPA) axis and the release of glucocorticoids(Herman et al. 2016; Joels et al. 2018; Murphy 1991). According to the reports, approximately 40–60% of patients with MDD experience HPA disorders (Keller et al. 2017). Over-activation of HPA induces the release of large quantities of cortisol in humans and corticosterone (CORT) in rodents (De Kloet et al. 1998).
Glucocorticoid exerts its effects on the central nervous system (CNS) by activating glucocorticoid receptors (GRs) and mineralocorticoid receptors (MRs). These receptors provide critical negative feedback signals to the HPA axis and determine the responsiveness of the HPA axis to stress-related hormones (Jacobson and Sapolsky 1991; Robinson et al. 2016). It has been reported that dysregulation of the HPA axis and subsequent secretion of glucocorticoid lead to irreversible cellular death and reversible structural changes in limbic and forebrain regions, including the hippocampus, prefrontal cortex (PFC), and amygdaloid nucleus (Drevets 2000; McEwen 2007). GRs and MRs are both expressed in these regions (Li et al. 2017; Sterner and Kalynchuk 2010). As a result, the hippocampus is most susceptible to chronic stress, an extensively studied area in the context of depression. Additionally, accumulating evidence has demonstrated that chronic exposure to excessive CORT may lead to irreversible hippocampal damage. Studies showed that the excess CORT decreases dendritic branching of hippocampal pyramidal neurons and dampens hippocampal neurogenesis and the expression of glucocorticoid receptor mRNA (Sterner and Kalynchuk 2010). While there is much evidence showing that CORT can impair the function and structure of hippocampus, the underlying mechanism is still unclear.
The endoplasmic reticulum (ER) is the largest organelle in eukaryotic cells. The ER is responsible for the synthesis, folding, and structural maturation of proteins. Exposure to chronic stress can interfere with ER function leading to endoplasmic reticulum stress (ERS) (Oakes and Papa 2015). Evidence suggests that ERS is a primary contributor to the pathogenesis of several nervous system diseases, including MDD, Alzheimer’s disease, Parkinson’s disease, and post-traumatic stress disorder(Oakes and Papa 2015). Dysregulation of CORT jeopardized the homeostasis of ER leading to ERS in neuron linking stress to neurodegenerative and neuropsychiatric disorders (Sterner and Kalynchuk 2010).
Brain-derived neurotropic factor (BDNF) is one of the most abundant and ubiquitous neurotrophins in CNS and has been implicated in mood regulation. Evidence suggests that levels of BDNF are associated with MDD and thus play a pivotal factor in pathophysiology of depression (Furuse et al. 2019). Reduction of BDNF occurs in the brain of MDD patients, and this process is reversed by antidepressants (Duman and Monteggia 2006). Furthermore, BDNF has been confirmed to promote neuronal survival and increase synaptic plasticity by binding its high-affinity receptor, tropomyosin-related kinase B (TrkB) (Hiester et al. 2013; Huang and Reichardt 2003). The precursor form of BDNF (proBDNF) elicits opposite effects in CNS (Shen et al. 2018; Sun et al. 2012). ProBDNF promotes neuronal death by activating membrane receptor p75NTR-mediated apoptotic signaling (Lee et al. 2001). Woo et al. reported that proBDNF induced long-term depression through p75NTR signaling pathway activation (Woo et al. 2005). Clinical studies show that the proBDNF and its receptors, p75NTR and sortilin, are increased in the patients with MDD (Zhou et al. 2013). Experimental studies have also shown that proBDNF and its receptors were increased in the mice with depressive-like behavior, and anti-proBDNF antibody (Ab-proBDNF) via intra-cerebroventricular or intra-hippocampal injection reversed the stress-induced depressive behavior presumably due to neutralizing the excessive proBDNF in rodents’ brain (Bai et al. 2016). The aforementioned studies suggest that proBDNF plays a significant role in the development of chronic stress-induced mood disturbances.
Given the detrimental effects of proBDNF on hippocampal neurons, we hypothesized that ERS-induced expression of proBDNF may promote the development of MDD. In this study, we conducted experiments on primary hippocampal neurons treated with CORT, detected hippocampal neuronal viability and the expression of synaptic-related proteins, proBDNF/p75NTR/FSTL4 and ERS markers (Grp78, p-PERK). In addition, we further quantified the effect anti-proBDNF neutralization and ISRIB (an inhibitor of the ERS) treatment in CORT-exposed neurons to identify the underlying pathological mechanisms after CORT treatment.
Materials and Methods
Animals
Pregnant C57BL/6J mice were purchased from Hunan Silaike Jingda Experimental Animal Co., Ltd. All animal experiments were approved by the Animal Care and Use Committee of Central South University in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals (no. 2019-s08).
Reagents
The anti-proBDNF monoclonal antibody (Ab-proBDNF) used in this study was developed by the Shanghai Yile Biotechnology Company. Its biological function was previously characterized (Luo et al. 2016). The reagents used in this study are listed in Table 1.
Primary Mouse Hippocampal Neuron Culture
Pregnant C57BL/6J mice at day 17 of pregnancy were anesthetized with sevoflurane, then sacrificed by cervical vertebra dislocation. The fetal mice were removed and placed in pre-cooled sterile PBS. The fetal mouse brains were isolated, and the hippocampus tissue was separated under a stereo microscope and transferred to a new petri dish with pre-cooled sterile PBS. The tissues then were carefully transferred to a small petri dish with 3 mL of 2 mg/mL papain solution, then digested with trypsin for 12 min at 37 °C. Three milliliters of DMEM/FBS solution was added to terminate the digestion, and the cells were transferred to a 15-mL centrifuge tube. The cells were centrifuged for 5 min at 1000 rpm, the supernatant was discarded, and the tissue pellets were suspended in 3 mL of DMEM/FBS solution. The cell suspension was filtered using a 70-μm cell strainer to remove large cell clumps, and the filtrate was transferred to a 15-mL centrifuge tube. After centrifugation at 1000 rpm for 5 min, the supernatant was discarded, and the pellet was resuspended in 3 mL of DMEM/FBS. The cells were plated on polylysine-coated culture flasks or glass coverslips (12 mm diameter) at a density of 1.0 × 105 cells/cm2, then cultured in a 5% CO2 incubator. The cells were allowed to attach for 2 h, then the medium was replaced with neurobasal medium containing 2% B27 supplement. The medium was changed every 2 days. At 7 days in vitro (DIV), the neurons were used for further experiments.
Cell Treatments
After 7 DIV, the neurons were exposed to CORT (1, 10, or 100 μM) for 24 h. The concentration of CORT was based on other reports (Donoso et al. 2019; Geng et al. 2003; Latt et al. 2018; Nakatani et al. 2014; Nitta et al. 2004). In addition, the neurons were exposed to ISRIB (1 μM) for 24 h to inhibit ERS. To antagonize proBDNF, the neurons were exposed to Ab-proBDNF (1 μg/mL) for 24 h; treatment with isotype-matched IgG (10 μg/mL) was used as a control.
Immunofluorescence
Cells cultured on coverslips were washed with pre-cooled PBS 3 times and fixed using 4% paraformaldehyde for 30 min. After washing with pre-cooled PBS 3 times, the slides were treated with 5% fetal bovine serum albumin (BSA) with 0.2% Triton X-100 for 2 h at room temperature. The slides were incubated with primary antibodies (BDNF, 1:100; proBDNF, 1:200; SYN, 1:200; PSD95, 1:200; NR2A, 1:200; or MAP2, 1:400) at 4 °C overnight. The slides were then incubated with fluorescence-labeled secondary antibodies (1:200) at room temperature for 2 h in the dark and then counterstained with 4,6-diaino-2-phenylindole (DAPI) for 10 min. Immunofluorescence images were captured using a computer-controlled microscope (Nikon, H600L Light Microscope) and analyzed using ImageJ software (National Institutes of Health).
Western Blotting
The treated cells were collected and lysed using a cocktail lysis buffer with protease and phosphatase inhibitors (Roche Applied Science, Mannheim, Germany) for 20 min. After centrifugation (4 °C at 12,000 rpm), the supernatant was collected. The samples were mixed with loading buffer and denatured in boiling water for 8 min. Proteins were separated on 10% Bis-Tris SDS-PAGE gels and transferred to 0.22-μm nitrocellulose membranes. The membranes were blocked using 5% non-fat milk for 2 h at room temperature. The membranes were then incubated with primary antibodies in PBS-T (BDNF, 1:2000; proBDNF, 1:500; p-PERK, 1:500; ATF4, 1:4000; Grp78, 1:500; SYN, 1:2000; PSD95, 1:2000; NR2A, 1:2000; or MAP2, 1:2000) at 4 °C overnight. After washing three times with TBS-T, the membranes were incubated with HRP-conjugated secondary antibodies in 5% skim milk (1:2000) for 2 h at room temperature. Bands were visualized using an ECL kit and analyzed using NIH ImageJ software (Tu et al. 2019; Zhang et al. 2019).
Real-Time qPCR Analysis
The treated cells were collected and total RNA was extracted using RNA extraction kit. A reverse transcription kit was used to obtain cDNA. Then, RT-qPCR analysis was performed, and the data were analyzed using the 2−ΔΔCt method (Chen et al. 2019; Zhang et al. 2019). The primer sequences were as follows:
BDNF forward | CGGTATCCAAAGGCCAACTG |
BDNF reverse | GTAGTTCGGCATTGCGAGTT |
GAPDH forward | ACTTTGGCATTGTGGAAGGG |
GAPDH reverse | AGTGGATGCAGGGATGATGT |
TUNEL Staining
Cells were cultured on slides, washed three times using pre-cooled PBS, then fixed with 4% paraformaldehyde for 30 min. A TUNEL solution kit (Beyotime Biotechnology, China) was used to detect apoptotic cells according to the manufacturer’s instructions. Fifty microliters of TUNEL test solution was added to the sample in the dark at 37 °C for 1 h. The slides were washed three times with pre-cooled PBS and incubated with an anti-fluorescence quenching liquid containing DAPI. Images were captured using a computer-controlled microscope (Nikon, H600L Light Microscope) and analyzed using ImageJ software (National Institutes of Health).
CCK-8 Cell Assay
Primary hippocampal neuron suspensions (100 μL/well) were plated into a 96-well plate and incubated for 7 days. After treatment, 10 μL of CCK-8 reagent was added to each well. A well filled with the same volume of culture medium and a well filled with CCK-8 reagent (Wanleibio, Shenyang, China) were used as blank controls. After 1 h of incubation, the absorbance at 450 nm was detected using a microplate reader. Cell viability was calculated as follows: Cell viability (%) = [treatment group − blank group] / [control group − blank group] × 100.
Statistical Analysis
Statistical analysis was performed using GraphPad Prism 7 software (GraphPad Software, San Diego, CA, USA). The data are presented as the mean ± SEM. All data were normally distributed as determined by the Shapiro-Wilk test. Significant differences were determined using Student’s t test for two-group comparisons or one-way ANOVA followed by Bonferroni’s post hoc testing for multiple comparisons among more than two groups. p < 0.05 was considered statistically significant.
Results
Corticosterone Treatment Reduced Primary Neuron Viability and Upregulated the Expression of proBDNF and Its Receptors
The excessive activation of HPA axis plays an important role in MDD (Robinson et al. 2016), partly due to the attenuation of glucocorticoid negative feedback mechanisms (Tafet and Nemeroff 2016). We treated primary hippocampal neurons with different concentrations (1, 10, and 100 μM) of CORT for 24 h and evaluated neuronal function and the expression of proBDNF and its receptors. Analysis using the CCK-8 kit showed that 100 μM CORT treatment significantly reduced cell viability compared to the control group (p = 0.0002; Fig. 1a) and upregulated the expression of proBDNF and its receptor FSTL4 and decreased p75NTR expression compared to the control group, as determined using Western blot (proBDNF: p = 0.0436; FSTL4: p < 0.0001; p75NTR: p < 0.0001; Fig. 1b, c) and immunofluorescence (proBDNF: p = 0.0047; FSTL4: p < 0.0001; p75NTR: p = 0.0111; Fig. 1d, e). However, no significant differences were found in the 1 and 10 μM treated group compared to the control group. Thus, 100 μM concentration was used in subsequent experiments.
Results of treatment of primary neurons with different concentrations of CORT. a Results of CCK-8 analysis. b Representative immunoblot bands for p75NTR, FSTL4, and proBDNF relative to tubulin as the loading control. c Quantitative analysis of protein level of p75NTR, FSTL4, and proBDNF. d Immunofluorescence results (p75NTR: green; FSTL4, proBDNF: red; DAPI: blue; scale bar = 40 μM). e Quantitative analysis of the relative density of p75NTR, FSTL4, and proBDNF. The quantitative data represent mean ± SEM from 3 to 4 independent experiments and calculated by one-way ANOVA followed by multiple comparisons using post hoc Tukey test. *p < 0.05 compared with Ctrl; **p < 0.01 compared with Ctrl; ***p < 0.001 compared with Ctrl; ****p < 0.0001 compared with Ctrl
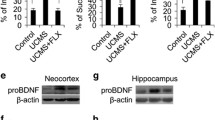
Corticosterone Treatment Upregulated proBDNF Through Activation of ERS
We investigated the mechanism by which CORT treatment increased proBDNF expression. Studies have shown that CORT treatment induces ERS (Liu et al. 2014; Zhou et al. 2018); this suggests that CORT-induced ERS may lead to increased proBDNF expression. Our results showed that the expression of ERS markers, Grp78 (t = 3.075, p = 0.0152), p-PERK (t = 3.149, p = 0.0346), and ATF4 (t = 2.6, p = 0.0316), was increased in the CORT treatment group compared with the control group (Fig. 2a, b), suggesting that CORT induced ERS. In addition, treatment with the ERS inhibitor, ISRIB, significantly decreased the expression of ATF4 (p < 0.0001, vs. CORT; Fig. 2c, d), indicating that ISRIB treatment inhibited CORT-induced ERS. We also observed that ISRIB treatment significantly suppressed CORT-mediated upregulation of proBDNF (p < 0.0001, vs. CORT) and FSTL4 (p = 0.0017, vs. CORT) (Fig. 3a, b).
Western blot of ERS-related protein expression following CORT treatment with or without ISRIB. a, c Representative immunoblot bands for p-PERK, Grp78, and ATF4 relative to tubulin as the loading control. b, d Quantitative analysis of protein levels of p-PERK, Grp78, and ATF4. The quantitative data represent mean ± SEM from 3 independent experiments and calculated by Student’s t test and one-way ANOVA followed by multiple comparisons using post hoc Tukey test. *p < 0.05 compare with Ctrl; **p < 0.01 compare with Ctrl; ***p < 0.001 compare with Ctrl; ****p < 0.0001 compare with Ctrl; ####p < 0.0001 compare with CORT
Activation of ERS and expression of proBDNF, FSTL4, and BDNF following CORT treatment with or without ISRIB. a Representative immunoblot bands of proBDNF, FSTL4, and BDNF relative to tubulin as the loading control. b Quantitative analysis of protein levels of proBDNF, FSTL4, and BDNF. c Ratio of proBDNF/BDNF. dBdnf mRNA expression. The quantitative data represent mean ± SEM from 3 independent experiments and calculated by one-way ANOVA followed by multiple comparisons using post hoc Tukey test. ***p < 0.001 compare with Ctrl; ****p < 0.0001 compare with Ctrl; ##p < 0.01 compare with CORT; ###p < 0.001 compare with CORT; ####p < 0.0001 compare with CORT
The ratio of proBDNF to BDNF, and the mRNA levels of Bdnf expression were evaluated. The results demonstrated that CORT treatment increased the ratio of proBDNF to BDNF (p < 0.0001, vs. Ctrl) and increased the expression of Bdnf (p < 0.0001, vs. Ctrl). These increases were reversed by ISRIB treatment (proBDNF/BDNF: p < 0.0001; Bdnf: p < 0.0001 vs. CORT; Fig. 3c, d). These results indicated that CORT induced ERS and increased the expression of proBDNF and FSTL4.
We used Ab-proBDNF to neutralize endogenous proBDNF and measured the expression of ERS makers (Grp78, p-PERK, ATF4) to evaluate the relationship between proBDNF and ERS. We found that Ab-proBDNF treatment did not affect Grp78 (p = 0.0985), p-PERK (p = 0.2888), or ATF4 (p = 0.3649) expression compared to the CORT + IgG group (Fig. 4a, b). However, the combination of Ab-proBDNF and ISRIB treatment decreased the expression of ATF4 (p < 0.0001, vs. CORT + IgG; Fig. 4a, b). These results suggested that proBDNF may be a downstream effector of ERS.
Western blot of ERS-related protein expression following anti-proBDNF antibody intervention. a Representative immunoblot bands for p-PERK, Grp78, and ATF4 relative to tubulin as the loading control. b Quantitative analysis of protein levels of p-PERK, Grp78, and ATF4. The quantitative data represent mean ± SEM from 3 independent experiments and calculated by one-way ANOVA followed by multiple comparisons using post hoc Tukey test. ****p < 0.0001 compare with Ctrl; ####p < 0.0001 compare with CORT + IgG
Corticosterone Decreased the Expression of Synaptic-Related Proteins of the Primary Hippocampal Neuron Via the ERS-proBDNF Pathway
We evaluated the roles of the ERS-proBDNF pathway in CORT-induced impaired primary hippocampal neurons. We treated primary hippocampal neurons with CORT, CORT plus ISRIB, CORT plus Ab-proBDNF, or CORT plus ISRIB and Ab-proBDNF. The results showed that CORT treatment significantly decreased the expression of a neuron dendritic marker MAP2 (p < 0.0001) and synaptic-related proteins, N-methyl-D-aspartate receptor subtype 2A (NR2A) (p < 0.0001), PSD95 (p < 0.0001), and synaptophysin (SYN) (p < 0.0001), compared to control treatment. The ERS inhibitor ISRIB reversed CORT-induced decreases in MAP2 (p < 0.0001, vs. CORT), NR2A (p < 0.0001, vs. CORT), PSD95 (p = 0.0028, vs. CORT), and SYN (p < 0.0001, vs. CORT) expression. Treatment with Ab-proBDNF reversed the downregulation of NR2A (p < 0.0001, vs. CORT + IgG), PSD95 (p < 0.0001, vs. CORT + IgG), and SYN (p < 0.0001, vs. CORT + IgG) by neutralizing excessive proBDNF (Fig. 5a, b). In addition, treatment with the combination of Ab-proBDNF and ISRIB also reversed CORT-induced reduction in MAP2 (p = 0.0126, vs. CORT + IgG), NR2A (p < 0.0001, vs. CORT + IgG), SYN (p < 0.0001, vs. CORT + IgG), and PSD95 (p = 0.0009, vs. CORT + IgG) expression (Fig. 5a, b). These results were verified using immunofluorescence (Fig. 6a, b). The results demonstrate that CORT treatment significantly decreased the expression of MAP2 (p = 0.0271) and SYN (p = 0.0032) compared to the control group. Treatment with ISRIB can reverse the reduced expression of MAP2 (p = 0.0105, vs. CORT) and PSD95 (p = 0.0004, vs. CORT), and anti-proBDNF antibody reversed the CORT-induced decreases in NR2A (p < 0.0001, vs. CORT + IgG) and PSD95 (p = 0.0341, vs. CORT + IgG) (Fig. 6a, b). Furthermore, co-treatment with ISRIB and Ab-proBDNF resulted in increased expression of MAP2 (p = 0.0254), NR2A (p < 0.0001), PSD95 (p = 0.0018), and SYN (p = 0.0004) compared to the CORT + IgG groups (Fig. 6a, b). These results revealed that CORT damaged synaptic-related proteins of primary hippocampal neuron via the ERS-proBDNF pathway.
Western blot results for synaptic and cellular function-related protein expression following CORT treatment and various interventions. a Representative immunoblot bands for MAP2, NR2A, PSD95, and SYN relative to tubulin as the loading control. b Quantitative analysis of protein levels of MAP2, NR2A, PSD95, and SYN. The quantitative data represent mean ± SEM from 3 independent experiments and calculated by one-way ANOVA followed by multiple comparisons using post hoc Tukey test. **p < 0.01 compare with Ctrl; ****p < 0.0001 compare with Ctrl; #p < 0.05 compare with CORT; ##p < 0.01 compare with CORT; ###p < 0.001 compare with CORT; ####p < 0.0001 compare with CORT; &p < 0.05 compare with CORT + IgG; &&p < 0.01 compare with CORT + IgG; &&&p < 0.001 compare with CORT + IgG; &&&&p < 0.0001 compare with CORT + IgG
Immunofluorescence results for synaptic and cellular function-related protein expression following CORT treatment and various interventions. a Immunofluorescence results for MAP2, NR2A, PSD95, and SYN (MAP2, NR2A: red; PSD95, SYN: green; DAPI: blue; scale bar = 40 μM). b Quantitative analysis of relative density of MAP2, NR2A, PSD95, and SYN. The quantitative data represent mean ± SEM from 3 independent experiments and calculated by one-way ANOVA followed by multiple comparisons using post hoc Tukey test. *p < 0.05 compare with Ctrl; **p < 0.01 compare with Ctrl; #p < 0.05 compare with CORT; ###p < 0.001 compare with CORT; ####p < 0.0001 compare with CORT; &p < 0.05 compare with CORT + IgG; &&p < 0.01 compare with CORT+IgG; &&&p < 0.001 compare with CORT + IgG; &&&&p < 0.0001 compare with CORT + IgG
Corticosterone Reduced Primary Hippocampal Neuron Survival Via the ERS-proBDNF Pathway
We investigated whether CORT induced cytotoxicity through the ERS-proBDNF pathway in neurons. We found that CORT treatment significantly increased the number of TUNEL-positive cells compared to the control (p = 0.0120) (Fig. 7a, b). This effect was reversed by treatment with ISRIB (p = 0.0030, vs. CORT) (Fig. 7a, b). Analysis using the CCK-8 kit showed that treatment with ISRIB (p < 0.0001, vs. CORT), Ab-proBDNF alone (p = 0.0081, vs. CORT + IgG), or ISRIB plus Ab-proBDNF (p = 0.0445, vs. CORT + IgG) attenuated CORT-mediated cell viability inhibition of primary hippocampal neurons (Fig. 7c). These results indicated that CORT reduced primary hippocampal neuron survival via the ERS-proBDNF pathway.
TUNEL and CCK-8 results following CORT treatment and various interventions. a TUNEL results (TUNEL: green; DAPI: blue; scale bar = 40 μM). b Quantitative analysis of cell count ratio of TUNEL-stained cells:DAPI (n = 6). c CCK-8 results following treatment. The quantitative data represent mean ± SEM from 4 to 6 independent experiments and calculated by one-way ANOVA followed by multiple comparisons using post hoc Tukey test. *p < 0.05 compare with Ctrl; **p < 0.01 compare with Ctrl; ***p < 0.001 compare with Ctrl; ##p < 0.01 compare with CORT; ###p < 0.001 compare with CORT; ####p < 0.0001 compare with CORT; &p < 0.5 compare with CORT+IgG; &&p < 0.01 compare with CORT + IgG; &&&p < 0.001 compare with CORT + IgG
Discussion
In this study, we found that CORT evoked ERS, which likely led to increased expression of proBDNF and FSTL4, neuronal apoptosis, decreased cell viability, and decreased the level of synaptic-related proteins. Treatment with the ERS inhibitor ISRIB significantly inhibited the expression of ATF4 and reversed CORT-mediated upregulation of proBDNF, cell viability inhibition, neuronal apoptosis, and synaptic-related protein reduction. Treatment with Ab-proBDNF protected neurons from CORT-induced cytotoxicity but did not alter the expression of the ERS marker proteins Grp78, p-PERK, or ATF4. These results suggest that CORT treatment induced ERS in primary hippocampal neurons, which resulted in increased expression of proBDNF and FSTL4, impaired synaptic-related protein expression, and induced neuronal apoptosis.
In human, patients with MDD exhibit persistent activation of the HPA axis (Keller et al. 2017). Stress life events are closely related to an increased risk for developing depression (Tennant 2002). Several studies reported that the HPA axis becomes activated upon stress exposure. Thereafter, the hypothalamus releases corticotropin-releasing hormone (CRH), which stimulates the secretion of adrenocorticotropic hormone (ACTH) from the pituitary gland. Meller et al. reported that people with anxiety and depression exhibited an attenuated ACTH response to exogenous CRH compared to healthy people (Meller et al. 1995). In general, cortisol increases in the morning and decreases in the evening operating on a circadian cycle. However, the level of cortisol remains significantly higher in the morning compared to non-depressed individuals and remains consistently high in the evening in the patient with depression (Kessing et al. 2011). Cortisol can remain high even after recovery from major depression (Beluche et al. 2009), suggesting that cortisol plays a vital role in the development of depression. Rao et al. found that females with MDD are less sensitive to dexamethasone compared to females with anxiety (Rao et al. 1989). These results showed that patients with anxiety and depression have HPA axis dysfunction. One explanation for excessive HPA axis activity is impaired inhibition of feedback by the over-elevated endogenous glucocorticoid cortisol that is mediated by the MRs and GRs in the brain (Meller et al. 1995).
In rodents, chronic stress results in continuous activation of HPA axis and subsequently persistently elevated glucocorticoid levels, which can impair hippocampal neuronal activity, induce hippocampal atrophy, reduce neurogenesis, downregulate hippocampal glucocorticoid receptor expression, and undermine the sensitivity of hippocampal neurons involved in feedback regulation and ultimately aggravate depressive symptoms (Duman 2004; Lee et al. 2002; Mahar et al. 2014; McKinnon et al. 2009). CORT is the rodent homolog of cortisol. Extensive studies reported that exogenous CORT administration can lead to depression-like behavior in rodents (Sterner and Kalynchuk 2010). Continuous infusion of CORT resulted in increased levels of depression-like behaviors in animal models (Gong et al. 2016; Ngoupaye et al. 2018). Treatment with CORT induced apoptosis of PC12 cells (Jiang et al. 2015; Peng et al. 2018) and primary hippocampal neurons (Sun et al. 2004; Zheng et al. 2018). Studies reported that CORT administration at a concentration greater than 50 μM could induce cytotoxicity and apoptosis of primary hippocampal neurons in a dose-dependent manner (Latt et al. 2018). Many studies reported that high concentrations of CORT lead to depression via hippocampal impairment (Donoso et al. 2019; Latt et al. 2018). According to these literary works, we set a concentration gradient from 1 to 100 μM to observe CORT effects. In our study, we found that 100 μM CORT treatments significantly increased the number of TUNEL-positive cells compared to the control, revealing that CORT treatment induced neuronal apoptosis, which is consist with prior observations (Latt et al. 2018).
proBDNF, the precursor of BDNF, exerts opposing effects on BDNF (Cowansage et al. 2010). Clinical studies have shown that serum levels of proBDNF have been shown to be increased in patients with depression (Zhao et al. 2017; Zhou et al. 2013), and proBDNF was decreased in the postmortem cerebellum and spleen of depressed patients (Yang et al. 2017). In the hippocampus or mPFC, proBDNF was increased following unpredictable chronic moderate stress (Bai et al. 2016), chronic restraint stress (Zhou et al. 2018), or inescapable stress (Yang et al. 2016). Ab-proBDNF intra-cerebroventricular or intra-hippocampal injection reversed the stress-induced depressive behavior (Bai et al. 2016; Zhong et al. 2018). Moreover, antidepressant drug, fluoxetine, could reverse unpredictable chronic mild stress-induced by increasing of proBDNF in the hippocampus (Bai et al. 2016). These results show that the increased proBDNF plays a vital role during depression. Moreover, CORT treatment resulted in increased expression of proBDNF in the ventral hippocampus, a region closely related to abnormal emotional behaviors (Willner et al. 2013) and depression-related neuroendocrine dysfunction (Li et al. 2019). Our study showed that the treatment of primary mouse hippocampal neurons with CORT induced significant upregulation of proBDNF expression. proBDNF preferentially binds to p75NTR to exert nerve cell apoptosis (Cowansage et al. 2010). In addition, binding of proBDNF to FSTL4 has been shown to negatively regulate BDNF maturation (Suzuki et al. 2018). Our results showed increased expression of FSTL4 and decreased expression of BDNF following CORT treatment, which indicated that FSTL4 could be a critical downstream effector of proBDNF and may negatively affect neuronal function.
Administration of different neuroprotective agents can reduce CORT-induced cell damage, reverse the expression of ERS proteins, and restore ER function (Peng et al. 2018). Our study showed that CORT treatment significantly increased the expression of the ERS-related proteins Grp78, phospho-PERK, and ATF4 in primary hippocampal neurons. PERK is a critical point of intersection between the comprehensive stress response and the unfolded protein response (UPR), which maintains protein-folding homeostasis in the ER (Pavitt and Ron 2012). A previous study showed that the ERS inhibitor ISRIB significantly inhibited the function of PERK and causes ATF4 expression decrease without impairing PERK phosphorylation. That is, ISRIB specifically blocks the PERK signal of UPR, which helps the cells resist eIF2α phosphorylation and restore protein translation in ER (Sidrauski et al. 2013). Our results showed that ISRIB inhibited CORT-induced increases in ATF4 expression in primary hippocampal neurons, which indicated that ISRIB reduced ERS.
Chronic hypoxic stress has been shown to increase the expression of proBDNF and Grp78 in the hippocampus (Sharma et al. 2019), which was consistent with our recent results. We showed that ISRIB reduced the expression of ATF4 in primary hippocampal neurons and reduced CORT-induced expression of proBDNF. This suggests that CORT-induced proBDNF was associated with ERS. Endoplasmic reticulum stress is characterized by the accumulation of unfolded and misfolded proteins in the ER through the activation of a number of cellular stress pathways. For example, ERS triggers the expression of pro-IL-1β through NF-κB activation and promotes IL-1β secretion (Kim et al. 2014). In this study, inhibition of ERS by ISRIB significantly inhibited proBDNF expression and increased BDNF levels, which indicated that abnormal ER function may lead to abnormal proBDNF. However, the mechanisms by which ERS induces BDNF mRNA and proBDNF protein upregulation and suppresses the proBDNF to BDNF transformation have not yet been characterized.
Depression is closely linked to changes in hippocampal synaptic plasticity (Duman et al. 2016). A number of studies have shown that SYN and PSD95 expression are downregulated in animal models of depression (Liu et al. 2017; Zhong et al. 2018). In addition, the expression of NR2A and PSD95 protein was decreased in patients with MDD (Feyissa et al. 2009). Our results showed that CORT treatment resulted in decreased expression of MAP2, NR2A, PSD95, and SYN, and increased apoptosis and reduced cell viability damaging neuronal function in vitro. Our results suggested that CORT treatment could induce a similar molecular expression pattern as MDD. We also showed that inhibition of ERS could increase the expression of MAP2, NR2A, PSD95, and SYN, and decrease neuronal apoptosis, and we postulated that inhibition of ERS restored the neuronal survive via reversing the synaptic protein expressions.
A previous study showed that high proBDNF expression resulted in decreased neuron dendrites, reduced spine density, and thus altered synaptic plasticity (Li et al. 2017; Pang et al. 2004; Teng et al. 2005). In this study, Ab-proBDNF exerted cytoprotective effects, which was substantiated by the inhibition of apoptosis, increased expression of MAP2, NR2A, PSD95, and SYN, and increased cell viability. However, Ab-proBDNF treatment did not affect the expression of the ERS markers like Grp78, p-PERK, and ATF4. Treatment with ISRIB decreased proBDNF and FSTL4 levels. Co-treatment with ISRIB and Ab-proBDNF also reduced CORT-induced apoptosis. These results showed that CORT induced ERS and abnormal proBDNF expression resulting in cellular dysfunction, such as apoptosis and impaired synaptic-related protein expressions in primary neurons.
Conclusion
CORT treatment induced ERS activation in primary hippocampal neurons, upregulated the expression of proBDNF and FSTL4, promoted neuronal apoptosis, and decreased synapse-related protein expression. Activation of the neuronal ERS/proBDNF/FSTL4 axis may be a critical pathway in MDD development.
Data Availability
There is no additional data, software, database, or application/tool available apart from that reported in the present study. All data is provided in the manuscript.
References
Bai YY, Ruan CS, Yang CR, Li JY, Kang Z et al (2016) ProBDNF signaling regulates depression-like behaviors in rodents under chronic stress. Neuropsychopharmacology 41:2882–2892
Beluche I, Chaudieu I, Norton J, Carriere I, Boulenger JP et al (2009) Persistence of abnormal cortisol levels in elderly persons after recovery from major depression. J Psychiatr Res 43:777–783
Chen S, Liang T, Zhou FH, Cao Y, Wang C et al (2019) Regular music exposure in juvenile rats facilitates conditioned fear extinction and reduces anxiety after foot shock in adulthood. Biomed Res Int 2019:8740674
Cowansage KK, LeDoux JE, Monfils MH (2010) Brain-derived neurotrophic factor: a dynamic gatekeeper of neural plasticity. Curr Mol Pharmacol 3:12–29
De Kloet ER, Vreugdenhil E, Oitzl MS, Joels M (1998) Brain corticosteroid receptor balance in health and disease. Endocr Rev 19:269–301
Donoso F, Ramirez VT, Golubeva AV, Moloney GM, Stanton C et al (2019) Naturally derived polyphenols protect against corticosterone-induced changes in primary cortical neurons. Int J Neuropsychopharmacol 22:765–777
Drevets WC (2000) Functional anatomical abnormalities in limbic and prefrontal cortical structures in major depression. Prog Brain Res 126:413–431
Duman RS (2004) Neural plasticity: consequences of stress and actions of antidepressant treatment. Dialogues Clin Neurosci 6:157–169
Duman RS, Aghajanian GK, Sanacora G, Krystal JH (2016) Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med 22:238–249
Duman RS, Monteggia LM (2006) A neurotrophic model for stress-related mood disorders. Biol Psychiatry 59:1116–1127
Feyissa AM, Chandran A, Stockmeier CA, Karolewicz B (2009) Reduced levels of NR2A and NR2B subunits of NMDA receptor and PSD-95 in the prefrontal cortex in major depression. Prog Neuro-Psychopharmacol Biol Psychiatry 33:70–75
Furuse K, Ukai W, Hashimoto E, Hashiguchi H, Kigawa Y, Ishii T, Tayama M, Deriha K, Shiraishi M, Kawanishi C (2019) Antidepressant activities of escitalopram and blonanserin on prenatal and adolescent combined stress-induced depression model: possible role of neurotrophic mechanism change in serum and nucleus accumbens. J Affect Disord 247:97–104
Geng ZH, Cheng YY, Ma XL, Li ST (2003) Effect of zinc on the corticosterone-induced injury of primary cultured rat hippocampal neurons. Sheng Li Xue Bao 55:736–741
Gong MJ, Han B, Wang SM, Liang SW, Zou ZJ (2016) Icariin reverses corticosterone-induced depression-like behavior, decrease in hippocampal brain-derived neurotrophic factor (BDNF) and metabolic network disturbances revealed by NMR-based metabonomics in rats. J Pharm Biomed Anal 123:63–73
Herman JP, McKlveen JM, Ghosal S, Kopp B, Wulsin A, Makinson R, Scheimann J, Myers B (2016) Regulation of the hypothalamic-pituitary-adrenocortical stress response. Compr Physiol 6:603–621
Hiester BG, Galati DF, Salinas PC, Jones KR (2013) Neurotrophin and Wnt signaling cooperatively regulate dendritic spine formation. Mol Cell Neurosci 56:115–127
Huang EJ, Reichardt LF (2003) Trk receptors: roles in neuronal signal transduction. Annu Rev Biochem 72:609–642
Jacobson L, Sapolsky R (1991) The role of the hippocampus in feedback regulation of the hypothalamic-pituitary-adrenocortical axis. Endocr Rev 12:118–134
Jiang Y, Li Z, Liu Y, Liu X, Chang Q, Liao Y, Pan R (2015) Neuroprotective effect of water extract of Panax ginseng on corticosterone-induced apoptosis in PC12 cells and its underlying molecule mechanisms. J Ethnopharmacol 159:102–112
Joels M, Karst H, Sarabdjitsingh RA (2018) The stressed brain of humans and rodents. Acta Physiol (Oxf) 223:e13066
Keller J, Gomez R, Williams G, Lembke A, Lazzeroni L, Murphy GM Jr, Schatzberg AF (2017) HPA axis in major depression: cortisol, clinical symptomatology and genetic variation predict cognition. Mol Psychiatry 22:527–536
Kessing LV, Willer IS, Knorr U (2011) Volume of the adrenal and pituitary glands in depression. Psychoneuroendocrinology 36:19–27
Kim S, Joe Y, Jeong SO, Zheng M, Back SH, Park SW, Ryter SW, Chung HT (2014) Endoplasmic reticulum stress is sufficient for the induction of IL-1beta production via activation of the NF-kappaB and inflammasome pathways. Innate Immun 20:799–815
Latt HM, Matsushita H, Morino M, Koga Y, Michiue H, Nishiki T, Tomizawa K, Matsui H (2018) Oxytocin inhibits corticosterone-induced apoptosis in primary hippocampal neurons. Neuroscience 379:383–389
Lee AL, Ogle WO, Sapolsky RM (2002) Stress and depression: possible links to neuron death in the hippocampus. Bipolar Disord 4:117–128
Lee R, Kermani P, Teng KK, Hempstead BL (2001) Regulation of cell survival by secreted proneurotrophins. Science 294:1945–1948
Li J, Chen J, Ma N, Yan D, Wang Y, Zhao X, Zhang Y, Zhang C (2019) Effects of corticosterone on the expression of mature brain-derived neurotrophic factor (mBDNF) and proBDNF in the hippocampal dentate gyrus. Behav Brain Res 365:150–156
Li J, Xie X, Li Y, Liu X, Liao X et al (2017) Differential behavioral and neurobiological effects of chronic corticosterone treatment in adolescent and adult rats. Front Mol Neurosci 10:25
Liu Y, Shen S, Li Z, Jiang Y, Si J, Chang Q, Liu X, Pan R (2014) Cajaninstilbene acid protects corticosterone-induced injury in PC12 cells by inhibiting oxidative and endoplasmic reticulum stress-mediated apoptosis. Neurochem Int 78:43–52
Liu YM, Hu CY, Shen JD, Wu SH, Li YC, Yi LT (2017) Elevation of synaptic protein is associated with the antidepressant-like effects of ferulic acid in a chronic model of depression. Physiol Behav 169:184–188
Luo C, Zhong XL, Zhou FH, Li JY, Zhou P, Xu JM, Song B, Li CQ, Zhou XF, Dai RP (2016) Peripheral brain derived neurotrophic factor precursor regulates pain as an inflammatory mediator. Sci Rep 6:27171
Mahar I, Bambico FR, Mechawar N, Nobrega JN (2014) Stress, serotonin, and hippocampal neurogenesis in relation to depression and antidepressant effects. Neurosci Biobehav Rev 38:173–192
Malhi GS, Mann JJ (2018) Depression. Lancet 392:2299–2312
McEwen BS (2007) Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev 87:873–904
McKinnon MC, Yucel K, Nazarov A, MacQueen GM (2009) A meta-analysis examining clinical predictors of hippocampal volume in patients with major depressive disorder. J Psychiatry Neurosci 34:41–54
Meller WH, Kathol RG, Samuelson SD, Gehris TL, Carroll BT, Pitts AF, Clayton PJ (1995) CRH challenge test in anxious depression. Biol Psychiatry 37:376–382
Murphy BE (1991) Steroids and depression. J Steroid Biochem Mol Biol 38:537–559
Nakatani Y, Tsuji M, Amano T, Miyagawa K, Miyagishi H, Saito A, Imai T, Takeda K, Ishii D, Takeda H (2014) Neuroprotective effect of yokukansan against cytotoxicity induced by corticosterone on mouse hippocampal neurons. Phytomedicine 21:1458–1465
Ngoupaye GT, Yassi FB, Bahane DAN, Bum EN (2018) Combined corticosterone treatment and chronic restraint stress lead to depression associated with early cognitive deficits in mice. Metab Brain Dis 33:421–431
Nitta A, Zheng WH, Quirion R (2004) Insulin-like growth factor 1 prevents neuronal cell death induced by corticosterone through activation of the PI3k/Akt pathway. J Neurosci Res 76:98–103
Oakes SA, Papa FR (2015) The role of endoplasmic reticulum stress in human pathology. Annu Rev Pathol 10:173–194
Pang PT, Teng HK, Zaitsev E, Woo NT, Sakata K, Zhen S, Teng KK, Yung WH, Hempstead BL, Lu B (2004) Cleavage of proBDNF by tPA/plasmin is essential for long-term hippocampal plasticity. Science 306:487–491
Pavitt GD, Ron D (2012) New insights into translational regulation in the endoplasmic reticulum unfolded protein response. Cold Spring Harb Perspect Biol 4
Peng R, Dai W, Li Y (2018) Neuroprotective effect of a physiological ratio of testosterone and estradiol on corticosterone-induced apoptosis in PC12 cells via Traf6/TAK1 pathway. Toxicol in Vitro 50:257–263
Rao ML, Vartzopoulos D, Fels K (1989) Thyroid function in anxious and depressed patients. Pharmacopsychiatry 22:66–70
Robinson SA, Brookshire BR, Lucki I (2016) Corticosterone exposure augments sensitivity to the behavioral and neuroplastic effects of fluoxetine in C57BL/6 mice. Neurobiol Stress 3:34–42
Roozendaal B, McEwen BS, Chattarji S (2009) Stress, memory and the amygdala. Nat Rev Neurosci 10:423–433
Sharma D, Barhwal KK, Biswal SN, Srivastava AK, Bhardwaj P, Kumar A, Chaurasia OP, Hota SK (2019) Hypoxia-mediated alteration in cholesterol oxidation and raft dynamics regulates BDNF signalling and neurodegeneration in hippocampus. J Neurochem 148:238–251
Shen LL, Mañucat-Tan NB, Gao SH, Li WW, Zeng F, Zhu C, Wang J, Bu XL, Liu YH, Gao CY, Xu ZQ, Bobrovskaya L, Lei P, Yu JT, Song W, Zhou HD, Yao XQ, Zhou XF, Wang YJ (2018) The ProNGF/p75NTR pathway induces tau pathology and is a therapeutic target for FTLD-tau. Mol Psychiatry 23:1813–1824
Sidrauski C, Acosta-Alvear D, Khoutorsky A, Vedantham P, Hearn BR, Li H, Gamache K, Gallagher CM, Ang KKH, Wilson C, Okreglak V, Ashkenazi A, Hann B, Nader K, Arkin MR, Renslo AR, Sonenberg N, Walter P (2013) Pharmacological brake-release of mRNA translation enhances cognitive memory. Elife 2:e00498
Smith K (2014) Mental health: a world of depression. Nature 515:181
Sterner EY, Kalynchuk LE (2010) Behavioral and neurobiological consequences of prolonged glucocorticoid exposure in rats: relevance to depression. Prog Neuro-Psychopharmacol Biol Psychiatry 34:777–790
Sun C, Liu N, Li H, Zhang M, Liu S et al (2004) Experimental study of effect of corticosterone on primary cultured hippocampal neurons and their Ca2+/CaMKII expression. J Huazhong Univ Sci Technolog Med Sci 24:543–546
Sun Y, Lim Y, Li F, Liu S, Lu JJ, Haberberger R, Zhong JH, Zhou XF (2012) ProBDNF collapses neurite outgrowth of primary neurons by activating. RhoA PLoS One 7:e35883
Suzuki R, Fujikawa A, Komatsu Y, Kuboyama K, Tanga N, Noda M (2018) Enhanced extinction of aversive memories in mice lacking SPARC-related protein containing immunoglobulin domains 1 (SPIG1/FSTL4). Neurobiol Learn Mem 152:61–70
Tafet GE, Nemeroff CB (2016) The links between stress and depression: psychoneuroendocrinological, genetic, and environmental interactions. J Neuropsychiatry Clin Neurosci 28:77–88
Teng HK, Teng KK, Lee R, Wright S, Tevar S et al (2005) ProBDNF induces neuronal apoptosis via activation of a receptor complex of p75NTR and sortilin. J Neurosci 25:5455–5463
Tennant C (2002) Life events, stress and depression: a review of recent findings. Aust N Z J Psychiatry 36:173–182
Tu BX, Wang LF, Zhong XL, Hu ZL, Cao WY, Cui YH, Li SJ, Zou GJ, Liu Y, Zhou SF, Zhang WJ, Su JZ, Yan XX, Li F, Li CQ (2019) Acute restraint stress alters food-foraging behavior in rats: taking the easier way while suffered. Brain Res Bull 149:184–193
Willner P, Scheel-Kruger J, Belzung C (2013) The neurobiology of depression and antidepressant action. Neurosci Biobehav Rev 37:2331–2371
Woo NH, Teng HK, Siao CJ, Chiaruttini C, Pang PT, Milner TA, Hempstead BL, Lu B (2005) Activation of p75NTR by proBDNF facilitates hippocampal long-term depression. Nat Neurosci 8:1069–1077
Yang B, Ren Q, Zhang JC, Chen QX, Hashimoto K (2017) Altered expression of BDNF, BDNF pro-peptide and their precursor proBDNF in brain and liver tissues from psychiatric disorders: rethinking the brain-liver axis. Transl Psychiatry 7:e1128
Yang B, Yang C, Ren Q, Zhang JC, Chen QX, Shirayama Y, Hashimoto K (2016) Regional differences in the expression of brain-derived neurotrophic factor (BDNF) pro-peptide, proBDNF and preproBDNF in the brain confer stress resilience. Eur Arch Psychiatry Clin Neurosci 266:765–769
Zhang WJ, Cao WY, Huang YQ, Cui YH, Tu BX, Wang LF, Zou GJ, Liu Y, Hu ZL, Hu R, Li CQ, Xing XW, Li F (2019) The role of miR-150 in stress-induced anxiety-like behavior in mice. Neurotox Res 35:160–172
Zhao G, Zhang C, Chen J, Su Y, Zhou R et al (2017) Ratio of mBDNF to proBDNF for differential diagnosis of major depressive disorder and bipolar depression. Mol Neurobiol 54:5573–5582
Zheng J, Yin F, Jin G, Zhang X, Zhang L et al (2018) In vitro neuroprotection of rat hippocampal neurons by manninotriose and astragaloside IV against corticosterone-induced toxicity. Molecules 23
Zhong F, Liu L, Wei JL, Hu ZL, Li L et al (2018) Brain-derived neurotrophic factor precursor in the hippocampus regulates both depressive and anxiety-like behaviors in rats. Front Psychiatry 9:776
Zhou B, Tan J, Zhang C, Wu Y (2018) Neuroprotective effect of polysaccharides from Gastrodia elata blume against corticosterone-induced apoptosis in PC12 cells via inhibition of the endoplasmic reticulum stress-mediated pathway. Mol Med Rep 17:1182–1190
Zhou L, Xiong J, Lim Y, Ruan Y, Huang C, Zhu Y, Zhong JH, Xiao Z, Zhou XF (2013) Upregulation of blood proBDNF and its receptors in major depression. J Affect Disord 150:776–784
Acknowledgments
We would like to thank Shanghai Yile Biotechnology Corp. for providing the monoclonal anti-proBDNF antibody.
Funding
This research was supported by the National Natural Science Foundation of China (31371212 to Chang-Qi Li; 81760238 and 81571256 to Fang-Fang Bi; 81771354 and 81471106 to Ru-Ping Dai; 81471372 to Fang Li; 81901231 to Zhao-Lan Hu) and by the Natural Science Foundation of Hunan Province, China (2018JJ3635 to Fang Li; 2019JJ40369 to Chang-Qi Li), and Graduate Research and Innovation Projects of Central South University, Changsha, Hunan, China (506021710 to Yu Liu; 506021717 to Guangjing Zou).
Author information
Authors and Affiliations
Contributions
LY and ZGJ contributed to the cellular and molecular experiments, and helped write the manuscript. TBX contributed to the cellular experiments and the molecular experiments and editing of the manuscript. HZL and Luo C contributed to cellular experiments. CYH and XY contributed to the molecular experiments. LF and DRP contributed to data analysis. BFF and LCQ contributed to experimental design, data analysis, figure construction, and manuscript writing. All authors read and agreed to the final version of the manuscript.
Corresponding authors
Ethics declarations
All animal experiments were approved by the Animal Care and Use Committee of Central South University in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals (no. 2019-s08).
Conflict of Interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, Y., Zou, GJ., Tu, BX. et al. Corticosterone Induced the Increase of proBDNF in Primary Hippocampal Neurons Via Endoplasmic Reticulum Stress. Neurotox Res 38, 370–384 (2020). https://doi.org/10.1007/s12640-020-00201-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-020-00201-4