Abstract
The contribution of neuroimmune functioning and brain-derived neurotrophic factor (BDNF) to functional dysregulation in autism spectrum disorder was assessed in 29 patients under treatment in two specialized centers of Basilicata (Chiaromonte and Matera), Southern Italy, through analysis of serum levels of cytokines and BDNF. Elevated levels of the pro-inflammatory cytokine, including interleukin-1, interleukin-6, interleukin-12, interleukin-23, tumor necrosis factor-α and BDNF were observed, regardless of age and gender. Comparisons were made with age- and gender-related healthy controls. The present findings reinforce current notions regarding immunoexcitotoxic mechanisms contributing to the pathophysiology of autistic disorder.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (ASD), a neurodevelopmental disorder with onset in the first 3 years of life, presents an incidence almost 6,000 new cases in the United States in 2008 (Buehler 2011) and in Italy 6–10 new cases per 10,000 children per year (Eurispes 2006). The disorder, which may be due to risk factors that include genetic, prenatal and perinatal involvement, neuroanatomical abnormalities and environmental agents (Johnson et al. 2013), presents an emerging medical social interest, particularly with regard to the economic, social and familial issues that are involved.
Neuroinflammation is involved in the pathophysiology of both neurologic and neuropsychiatric disorders (Hurley and Tizabi 2013). Disruption/dysregulation of neuroimmune functioning, whether expressed in the patient or during the course of the individual’s brain development, are implicated in Idiopathic ASD (Onore et al. 2012; Ramos et al. 2012; Sacco et al. 2010). It has been shown that several mediators of the immune system play a key role in the development of the central nervous system, affecting neurogenesis, neuronal migration, axonal growth, the formation and plasticity of synapses (Garay and McAllister 2010). The dysfunctional immune activity observed in ASD spans both innate and adaptive arms of the immune system and suggests that perturbations in either area may have profound effects on neurodevelopment (McAllister and van de Water 2009). The immune and nervous systems are highly interconnected in a neuroimmune interaction that affects several aspects of brain structure and function (Archer et al. 2011). For example, studies have shown that SCID mice (severe combined immunodeficient), lacking in T lymphocytes, show severe alterations in the acquisition of cognitive abilities; however, the insertion of T cells to these mice by bone marrow transplantation, improved the cognitive performance of these mice, in addition to the recovery of adaptive immunity (Brynskikh et al. 2008). There is much evidence showing that peripheral cells of the immune system may modulate cognitive performance without infiltrating the brain and central nervous system (Rook et al. 2011). Various mediators of the immune system, normally expressed in the CNS, are essential for normal brain development. The components of the large family of cytokines are physiologically produced in the CNS, where they control neurogenesis, migration, differentiation, synapse formation and plasticity, and damage response (Green et al. 2012).
From early in development onwards, the relationship between the immune and nervous systems is exceedingly complex and continues throughout life. Abnormal immune responses, including self-reactive antibodies, have been reported in individuals affected with ASD and significantly higher plasma concentrations of IL-1β, IL-5, IL-8, IL-12 in patients compared to the matched normal controls have recently been detected (Ashwood et al. 2011; Li et al. 2009). Studies performed on brains taken at autopsy from subjects with autism or control subjects showed elevated levels of tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6) in subjects with autism compared to controls (Kalkbrenner et al. 2010). Increased pro-inflammatory or Th1 cytokines were associated with greater impairments in core features of ASD as well as aberrant behaviors (Ashwood et al. 2011). Under physiological conditions, cytokines provide trophic support to neurons and enhance neuronal integrity, but excessive cytokine production, that is, immunoexcitotoxic mechanisms that enhance neurotoxic reactions (Al-Ayadhi and Mostafa 2012; Mostafa and Al-Ayadhi 2011a, b, 2012; Blaylock 2008), has been shown to lead to brain disorder conditions, in part due to disruption of growth factor production and neurogenesis thereby contributing to the etiopathogenesis of the disorder. A hyperexcitatory action of glutamate, and the glutamatergic receptors NMDA and AMPA, leads to activation of enzymes that damage cellular structure, membrane permeability and electrochemical gradients. Excitotoxicity, due to overactivity in glutamatergic pathways, oxidative stress and impaired mitochondrial function are major factors implicated in the neuronal dysfunction of autistic patients (Essa et al. 2013). Immunoexcitotoxicity refers to the evolving pathological and neurodevelopmental changes in autism and presents a common mechanism in several neurodegenerative disorders (Blaylock 2008, 2009; Blaylock and Maroon 2012). Immune receptor–excitatory glutamate receptor interactions trigger neurotoxic events, such as extensive reactive oxygen species/reactive nitrogen species generation, accumulation of lipid peroxidation products, and prostaglandin activation, which then leads to dendritic retraction, synaptic injury, damage to microtubules, and mitochondrial suppression (Blaylock and Maroon 2011). In addition, several epidemiological studies have found a correlation between autism and autoimmunity as well as with allergies (Goines and Van de Water 2010).
Brain-derived neurotrophic factor (BDNF), a small protein found throughout the brain, CNS and in peripheral blood, plays a pivotal role in the development and plasticity of the brain. Much experimental data strongly suggest an involvement of BDNF in autism, for instance, increased BDNF-immunoreactive protein in the disorder (Garcia et al. 2012). Additionally, it was observed that BDNF levels in the blood reflected BDNF levels in the brain. BDNF is involved in the survival and differentiation of dopaminergic neurons in the developing brain and plays an important role in the formation and the plasticity of synaptic connections. BDNF is trophic for serotonergic neurons, and abnormalities in serotonin levels are the most common biochemical findings in autism. Al-Ayadhi (2012) reported a correlation between sonic hedgehog homolog (SHH), BDNF and oxygen free radicals (OFR) in autistic children, suggesting a pathological role of oxidative stress and SHH in ASDs. Under conditions of brain damage and aggravated neurotoxicity, levels of BDNF have been shown to be increased (Bovolenta et al. 2010; Fredriksson et al. 2011).
The main purpose of the present study was to assess the existence of excessive cytokine concentration and neurotrophin, circulating levels of BDNF, in the serum of young patients presenting ASD.
Materials and Methods
Sample Demographics
Twenty-nine patients, aged 2–21 years, including 27 males, were recruited for this study at the Center for Autism of hospital of Chiaromonte/Lagonegro (PZ) and at the Pediatrics Neuropsychiatry Department of Matera: regional centers that coordinate services for persons with autism from which they were recruited. The clinical characteristics of the individual 29 patients included in the study are available (see Table 1). All patients present developmental records documenting characteristics and behaviors that met a standardized definition for ASDs based on the Diagnostic and Statistical Manual of the American Psychiatric Association (DSM-IV-TR 2000). Nineteen autistic patients were classified as severe, based on a Childhood Autism Rating Scale (CARS) score of 37 or more; three patients were classified with mild-to-moderate disease as determined by CARS score between 32 and 37; eight patients were classified as mild, according to CARS score below 32.
Twenty-nine healthy age- and gender-matched subjects with no overt neurological or psychiatric abnormalities were selected as the control group.
Anamnestic Medical Social Questionnaire
The questionnaire, administrated to the families of patients, was composed of four sections: (i) child’s data, including age, weight, height, residence, blood type, age of first diagnosis and the severity of the disease, as well as the type of vaccination, the stages of language development, the sleep patterns and age-at-weaning, weaning, nutrition, food allergies and intolerance, (ii) parental data, (iii) presence of allergies, food allergies, autoimmune diseases and other diseases, type of diet, working site and exposure to possible harmful factors, personal lifestyles, pregnancy and childbirth, previous surgery and family history for major diseases (especially for autoimmune diseases like rheumatoid arthritis, psoriasis, Crohn’s disease, etc.), (iv) socio-economic aspects, such as the use of computers and mobile phones, services and support provided by local health authorities, town councils, social and family health associations.
Blood Sample Assays
Venous blood from each individual was collected and stored at 4 °C overnight. Serum was obtained after centrifuging at 1,500 rpm for 10 min at RT, aliquoted and stored at −80 °C until use.
All the children were medication free and in good physical health at time of blood sample assays.
Cytokine Production
Levels of serum cytokines were determined by ELISA following the manufacturer’s instructions, using the following kits:
-
IL1β (Abcam, cat. ab46052, UK, detection limits: 5 pg/ml)
-
IL-6 (Quantikine, R&D Systems, cat. D6050, USA, detection limits: 0.70 pg/ml)
-
IL-12 (Quantikine, R&D Systems, cat. D1200, USA, detection limits: 5 pg/ml)
-
IL-13 (Quantikine, R&D Systems, cat. D1300, USA, detection limits: 32 pg/ml)
-
IL-23 (eBioscience, cat. 88-7239, USA, detection limits: 15 pg/ml)
-
TNF-α (Immunological Sciences, cat. IK4185, detection limits: 1 pg/ml)
-
BDNF (Immunological Sciences, cat. IK-10144, detection limits: 15 pg/ml)
Each standard curve was generated using eight points of concentrations. Serum aliquots had not undergone any previous freeze/thaws cycle.
Statistical Analysis
Values are expressed as mean ± SD in the text and figures. Comparisons between two groups were analyzed by Student’s two-tailed t test. When the equal variance test failed, a Mann–Whitney rank sum test was used. Levels of significance are stated. Pearson’s rank correlation coefficients were calculated.
Results
Analysis of Anamnesis
Four children were intolerant to milk, casein, gluten, fish and vegetables. As for the sleep–wake cycle, in five patients, it is irregular. Language development: in 11 children, there was a delay in babbling, and in seventeen, current language is poor, if not absent. Five children were born preterm and eleven by cesarean section. In addition, two siblings are both affected by autism. Seven out of thirty mothers gave birth at an age between 35 and 37 years, all with a normal diet. Eleven mothers experience allergies to pollen, dust, nickel and food intolerances, especially lactose, two of these have had amalgam fillings, outside the period of pregnancy. Seven are smokers. No mother is significantly exposed to harmful factors, and most of them are housewives. Fifteen children presented a family history of hypertension, six of diabetes, six of dyslipidemia, eleven of tumors, fourteen of heart disease, six of obesity, ten of thyroid disease, four of neurological and psychiatric diseases and six of autoimmune diseases. In the present study, focus was placed on the presence of autoimmune disorder, since the other conditions are present in almost comparable levels in the group of healthy patients: maternal autoimmune diseases include psoriasis (four mothers), rheumatoid arthritis, celiac disease and Takayasu’s arteritis. In one child, we found paternal familiarity for psoriasis. Another child has a sister suffering from rheumatoid arthritis.
Immune Cytokine Dysregulation
Pairwise comparisons using Student’s two-tailed t tests indicated the following differences between the autistic group (n = 29) and the healthy control group (n = 29) of children:
-
IL-1β: t (df: 1, 28) = 12.75, p < 0.0001: autism > control (see Fig. 1).
-
IL-6: t (1, 29) = 5.10, p < 0.0001: autism > control (see Fig. 2).
-
IL-23: t (1, 29) = 2.62, p < 0.02: autism > control (see Fig. 3).
-
IL-12: t (1, 29) = 4.18, p < 0.0001: autism > control (see Fig. 4).
-
TNF-α: t (1, 29) = 6.22, p < 0.0001: autism > control (see Fig. 5).
There was no significant difference between the autism and control groups with regard to IL-13. Table 2 presents the inflammatory cytokines and BDNF levels for individual patients in the study.
Table 3 presents the inflammatory cytokines and BDNF levels for individual healthy control subjects in the study.
Figures 1–6 presents the levels of each of the cytokines, IL-1β, IL-6, IL-23, IL-12 and TNF-α, respectively, for the ASD patient group compared with the healthy control group.
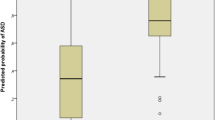
BDNF Overexpression
Pairwise comparisons using Student’s two-tailed t tests indicated the following differences between the autistic group (n = 29) and the control group (n = 29) of children:
BDNF: t (1, 29) = 12.79, p < 0.0001: autism > control (see Fig. 7).
Autism spectrum disorder patients and controls were divided into two groups by age. Further, patients were divided into three groups on the basis of severity which provided means and standard deviations for each group for BDNF values as follows: mild autism: mean = 602.2 pg/ml; standard deviation = 395.1; moderate autism: mean = 619.3 pg/ml; standard deviation = 538.0; severe autism: mean = 791 pg/ml; standard deviation = 475.4; healthy control sample: means = 351.4 pg/ml; standard deviation = 347.2. Although this trend was not found to be significant, possibly due to patient severity group size, all three patient groups showed significantly higher levels of BDNF (t > 3.34, df 10–14, p < 0.01).
Figure 7 presents the levels of BDNF neurotrophin for the ASD patient group compared with the healthy control group.
Correlational Analysis
Correlational analyses (Pearson’s rank) were performed between each of the above cytokines, and BDNF, against CARS (ASD diagnosis) scores. Only one of the six correlations was found to be significant: IL-1β versus CARS indicating a cytokine-diagnosis association.
Figure 8 presents the correlations between IL-1β and CARS.
Discussion
The purpose of the present study was to investigate the relationship between ASD and the presence of a chronic inflammatory condition, expressed by immunoexcitotoxicity, with altered levels of serum cytokines, as associated with prevailing health conditions (Adams et al. 2011). The results from 29 ASD patients compared with age- and gender-matched healthy controls indicated that cytokines IL-1β, IL-6, IL-12, TNF-α and IL-23 were increased significantly in the blood serum of ASD patients compared with healthy controls. Ancillary to the primary purpose, it was found also that serum BDNF was elevated significantly in the ASD patients compared with healthy controls. Several brain disorders, associated with alterations of the normal mechanisms controlling development, have been associated with specific variants of cytokines and/or their receptors (Angelidou et al. 2012; Petitto et al. 2012; Vezzani and Friedman 2011). Cytokines may originate from peripheral immune cells and reach the CNS by crossing the blood–brain barrier or may be produced directly within the CNS by neurons and glial cells. Cytokines are signaling molecules, responsible for the cross talk between cells of the immune system and neuroendocrine system. They are produced by macrophages and lymphocytes as well as by microglia and astrocytes in the CNS. Two main clusters of cytokines have been recognized, based on the specific T helper cells producing them: type 1 helper cells, generally engaged in cellular immune response and type 2 helper cells involved in humoral immunity. Cytokines activate specific cytokine receptors on neurons and glial cells thereby directly influencing brain function and neurogenesis.
In this connection, the microenvironment where precursors of mature neuronal cells (neural stem cells) reside are specialized “niches” where several different stimuli, including neurotrophic factors, cytokines and drugs, may modulate neurogenesis processes; it should be recalled that neuroinflammation may influence the neural stem cell niche, altering proliferation, migration, survival and maturation of neuron precursor cells (Boulanger 2009; Garay and McAllister 2010). An altered cytokine network may underline the onset and the progression of psychiatric and systemic diseases and favor the progression of depression and Alzheimer’s disease (Ricci et al. 2012). It has been demonstrated that pro-inflammatory cytokines increase the activity of hypothalamic–pituitary–adrenal (HPA) axis (Pucak et al. 2007). Chronic activation of the HPA axis induces anxiety and depression (Zunszain et al. 2011), commonly seen in patients with autism since depression is co-morbid with many other conditions with pro-inflammatory cytokine activation and neurodegenerative damage (Leonard and Maes 2012). The hyperreactivity of both the HPA axis and pro-inflammatory neuroimmunological markers in response to acute negative emotions seems to provide a common denominator in several brain disorder conditions (Weinstein et al. 2010). Pro-inflammatory cytokines lead to a glutamatergic overproduction (Müller and Schwarz 2007) which implicates an immunoexcitotoxic mediation.
Some studies have been conducted to evaluate possible differences in the levels of pro-inflammatory or anti-inflammatory cytokines in sera of children with autism compared to healthy controls (Jyonouchi et al. 2001, 2002; Molloy et al. 2006). The results, sometimes conflicting, possibly due to diagnostic complications and unsuitable choice of controls, have nevertheless shown an increase of certain pro-inflammatory cytokines in the sera of children with autism. The present immunochemical evaluations suggest the presence of a dysregulation in the cytokine network, with a significant increase of IL-1β, IL-6, IL-12, IL-23 and TNF-α in the ASD patient group compared to the controls matched by gender and age. IL-23, a member of IL-12 family of cytokines, is able to induce the polarization of CD4+ T lymphocytes to Th17 cells which produce a cytokine specifically involved in autoimmune inflammation. Th17 cells were specifically detected within active lesions of multiple sclerosis (MS) patients and within the brain of mouse model for MS developing experimental autoimmune encephalomyelitis, prior to the development of clinical symptoms of MS. Of note, anti-myelin basic protein autoantibody, a hallmark of MS, has been reported in autism patients: Mostafa and Al-Ayadhi (2011a, b) observed that autistic children expressed significantly higher serum levels of serotonin and anti-MBP auto-antibodies than healthy children.
In a previous study, an inflammatory condition was detected in the brains of deceased individuals with autism, as evidenced by high amounts of cytokines and activated microglial and astroglia cells (Pardo et al. 2005; Vargas et al. 2005). This disease pattern was present in subjects ranging in age from 5 to 44 years, suggesting that once the activation of the immune system was induced, it remains unchanged over time. The results we obtained seem to confirm this finding, since the alteration found in the serum levels of cytokines compared to controls was measured in patients ranging in age from 3 to 20 years. The overproduction of IL-1β was of particular interest as elevated levels of this cytokine were found in individuals suffering from depression, and the increase was related to chronic activation of the HPA axis that are known to induce anxiety and depression (Besedovsky et al. 1986). Similarly, the same process may underlie the behavioral disturbances observed in individuals with ASD. In addition, IL-1β promotes the expression of the β amyloid precursor protein (Cacabelos et al. 1991), and several studies reported that plasma levels of the secreted amyloid-β (Aβ) precursor protein-alpha form (sAPPα) were significantly elevated in plasma of patients with severe autism (Ray et al. 2011; Sokol et al. 2006).
The observed increase in serum BDNF is consistent with recent evidence of a steady increase in the number of neurons in the prefrontal cortex of ASD patients (Courchesne et al. 2011; Lainhart and Lange 2011). In autistic children, using whole blood polymorphonuclear leukocytes, significantly higher levels of OFR were obtained (22), as well as serum Sonic hedgehog (SHH) protein, a signaling protein vital during embryonic development, up-regulates both BDNF and vascular endothelial growth factor (VEGF); here, it was found that BDNF levels were elevated. Furthermore, there was a significant positive correlation between the CARS index and level of SHH protein (Pardo et al. 2005). In this regard, it is necessary to consider that enhanced BDNF signaling, in addition to neurogenesis, neuritic sprouting, electrophysiological activity, etc., also renders brain regions more vulnerable to hyperexcitability and/or excitotoxic damage (Murray and Holmes 2011). In conclusion, the present data suggest that ASD patients present a dysregulation of cytokine networks with an imbalance toward pro-inflammatory cytokines.
Gene variations for cytokines and their receptors have been reported in autism (Ziats and Rennert 2011). Microarray experiments have shown a dysregulation of cytokine and chemokine genes in the brain of autistic patients (Lintas et al. 2012). Both the observed increases of pro-inflammatory cytokines and BDNF suggest the influence of immunoexcitotoxic actions in the pathophysiology of ASD; this dysregulation of cytokine and neurotrophin levels may play a contributory role in the etiopathogenesis of the disorder. Finally, Mostafa et al. (2013) have suggested the possible link between certain human leukocyte antigen alleles to autism and to family history of autoimmunity indicates the possible contributing role of these alleles to autoimmunity in some autistic children. Two aspects of the present findings appear quite unique: (i) the elevation of both cytokine levels and BDNF and (ii) the elevated expression of BDNF in a chronic neurodevelopmental disorder, rather than acute brain damage.
References
Adams JB, Audhya T, McDonough-Means S, Rubin RA, Quig D, Geis E, Gehn E, Loresto M, Mitchell J, Atwood S, Barnhouse S, Lee W (2011) Nutritional and metabolic status of children with autism vs neurotypical children, and the association with autism severity. Nutr Metab 8:34
Al-Ayadhi LY (2012) Relationship between sonic hedgehog protein, brain-derived neurotrophic factor and oxidative stress in autism spectrum disorders. Neurochem Res 37:394–400
Al-Ayadhi LY, Mostafa GA (2012) Elevated serum levels of interleukin-17A in children with autism. J Neuroinflamm 9:158
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders DSM-IV-TR, 4th edn. American Psychiatric Association, Washington, DC
Angelidou A, Asadi S, Alysandratos KD, Karagkouni A, Kourembanas S, Theoharides TC (2012) Perinatal stress, brain inflammation and risk of autism: review and proposal. BMC Pediatr 12:89. doi:10.1186/1471-2431-12-89
Archer T, Fredriksson A, Schütz E, Kostrzewa RM (2011) Influence of physical exercise on neuroimmunological functioning and health: aging and stress. Neurotox Res 20:69–83
Ashwood P, Krakowiak P, Hertz-Picciotto I, Hansen R, Pessah I, Van de Water J (2011) Elevated plasma cytokines in autism spectrum disorders provide evidence of immune dysfunction and are associated with impaired behavioral outcome. Brain Behav Immun 25:40–45
Besedovsky H, del Rey A, Sorkin E, Dinarello CA (1986) Immunoregulatory feedback between interleukin-1 and glucocorticoid hormones. Science 233:652–654
Blaylock RL (2008) A possible central mechanism in autism spectrum disorders, part 1. Altern Ther Health Med 14:46–53
Blaylock RL (2009) A possible central mechanism in autism spectrum disorders, part 2: immunoexcitotoxicity. Altern Ther Health Med 15:60–67
Blaylock RL, Maroon J (2011) Immunoexcitotoxicity as a central mechanism in chronic traumatic encephalopathy: a unifying hypothesis. Surg Neurol Int 2:107
Blaylock RL, Maroon J (2012) Natural plant products and extracts that reduce immunoexcitotoxicity-associated neurodegeneration and promote repair within the central nervous system. Surg Neurol Int 3:19
Boulanger LM (2009) Immune proteins in brain development and synaptic plasticity. Neuron 64:93–109
Bovolenta R, Zucchini S, Paradiso B, Rodi D, Merigo F, Navarro MG, Osculati F, Berto E, Marconi P, Marzola A, Fabene PF, Simonato M (2010) Hippocampal FGF-2 and BDNF overexpression attenuates epileptogenesis-associated neuroinflammation and reduces spontaneous recurrent seizures. J Neuroinflamm 7:81–87
Brynskikh A, Warren T, Zhu J, Kipnis J (2008) Adaptive immunity affects learning behavior in mice. Brain Behav Immun 22:861–869
Buehler MR (2011) A proposed mechanism for autism: an aberrant neuroimmune response manifested as a psychiatric disorder. Med hypothes 76:863–870
Cacabelos R, Franco-Maside A, Alvarez XA (1991) Interleukin-1 in Alzheimer’s disease and multi-infarct dementia: neuropsychological correlations. Methods Find Exp Clin Pharmacol 13:703–708
Courchesne E, Mouton PR, Calhoun ME, Semendeferi K, Ahrens-Barbeau C, Hallet MJ, Barnes CC, Pierce K (2011) Neuron number and size in prefrontal cortex of children with autism. JAMA 306:2001–2010
Essa MM, Braidy N, Vijayan KR, Subash S, Guillemin GJ (2013) Excitotoxicity in the pathogenesis of autism. Neurotox Res 23(4):393–400
Eurispes (2006) 18° Rapporto Italia, vol 8. Eurispes, p 245
Fredriksson A, Stigsdotter IM, Hurtig A, Ewalds-Kvist B, Archer T (2011) Running wheel activity restores MPTP-induced functional deficits. J Neural Tranms 18:407–420
Garay PA, McAllister AK (2010) Novel roles for immune molecules in neural development: implications for neurodevelopmental disorders. Front Synaptic Neurosci 2:136
Garcia KL, Yu G, Nicolini C, Michalski B, Garzon DJ, Chiu VS, Tongiorgi E, Szatmari P, Fahnestock M (2012) Altered balance of proteolytic isoforms of pro-brain-derived neurotrophic factor in autism. J Neuropathol Exp Neurol 71:289–297
Goines P, Van de Water J (2010) The immune system’s role in the biology of autism. Curr Opin Neurol 23:111–117
Green HF, Treacy E, Keohane AK, Sullivan AM, O’Keeffe GW, Nolan YM (2012) A role for interleukin-1β in determining the lineage fate of embryonic rat hippocampal neural precursor cells. Mol Cell Neurosci 49:311–321
Hurley LL, Tizabi Y (2013) Neuroinflammation, neurodegeneration, and depression. Neurotox Res 23(2):131–144. doi:10.1007/s12640-012-9348-1
Johnson NL, Giarelli E, Lewis C, Rice CE (2013) Genomics and autism spectrum disorder. J Nurs Scholarsh 45(1):69–78. doi:10.1111/j.1547-5069.2012.01483.x
Jyonouchi H, Sun S, Le H (2001) Proinflammatory and regulatory cytokine production associated with innate and adaptive immune responses in children with autism spectrum disorders and developmental regression. J Neuroimmunol 120:170–179
Jyonouchi H, Sun S, Itokazu N (2002) Innate immunity associated with inflammatory responses and cytokine production against common dietary proteins in patients with autism spectrum disorder. Neuropsychobiology 46:76–84
Kalkbrenner AE, Daniels JL, Chen JC, Poole C, Emch M, Morrissey J (2010) Perinatal exposure to hazardous air pollutants and autism spectrum disorders at age 8. Epidemiology 21:631–641
Lainhart JE, Lange N (2011) Increased neuron number and head size in autism. JAMA 306:2031–2032
Leonard B, Maes M (2012) Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neurosci Bio Behav Rev 36:764–785
Li X, Chauhan A, Sheikh AM, Patil S, Chauhan V, Li XM, Ji L, Brown T, Malik M (2009) Elevated immune response in the brain of autistic patients. J Neuroimmunol 207:111–116
Lintas C, Sacco R, Persico AM (2012) Genome-wide expression studies in autism spectrum disorder, Rett syndrome, and Down syndrome. Neurobiol Dis 45:57–68
McAllister AK, van de Water J (2009) Breaking boundaries in neural-immune interactions. Neuron 64:9–12
Molloy CA, Morrow AL, Meinzen-Derr J, Schleifer K, Dienger K, Manning-Courtney P, Altaye M, Wills-Karp M (2006) Elevated cytokine levels in children with autism spectrum disorder. J Neuroimmunol 172:198–205
Mostafa GA, Al-Ayadhi LY (2011a) The possible link between the elevated serum levels of neurokinin A and anti-ribosomal P protein antibodies in children with autism. J Neuroinflamm 8:180
Mostafa GA, Al-Ayadhi LY (2011b) A lack of association between hyperserotonemia and the increased frequency of serum anti-myelin basic protein auto-antibodies in autistic children. J Neuroinflamm 8:71
Mostafa GA, Al-Ayadhi LY (2012) The relationship between the increased frequency of serum antineuronal antibodies and the severity of autism in children. Eur J Paediatr Neurol 16(5):464–468
Mostafa GA, Shehab AA, Al-Ayadhi LY (2013) The link between some alleles on human leukocyte antigen system and autism in children. J Neuroimmunol 255(1–2):70–74. doi:10.1016/j.jneuroim.2012.10.002
Müller N, Schwarz MJ (2007) The immune-mediated alteration of serotonin and glutamate: towards an integrated view of depression. Mol Psychiatry 12:988–1000
Murray PS, Holmes PV (2011) An overview of brain-derived neurotrophic factor and implications for excitotoxic vulnerability in the hippocampus. Int J Pept. doi:10.1155/2011/654085
Onore C, Careaga M, Ashwood P (2012) The role of immune dysfunction in the pathophysiology of autism. Brain Behav Immun 26:383–392
Pardo CA, Vargas DL, Zimmerman AW (2005) Immunity, neuroglia and neuroinflammation in autism. Int Rev Psychiatry 17:485–495
Petitto JM, Huang Z, Meola D, Ha GK, Dauer D (2012) Interleukin-2 and the septohippocampal system: intrinsic actions and autoimmune processes relevant to neuropsychiatric disorders. Methods Mol Biol 829:433–443
Pucak ML, Carroll KA, Kerr DA, Kaplin AI (2007) Neuropsychiatric manifestations of depression in multiple sclerosis: neuroinflammatory, neuroendocrine, and neurotrophic mechanisms in the pathogenesis of immune-mediated depression. Dialogues Clin Neurosci 9:125–139
Ramos PS, Sajuthi S, Langefeld CD, Walker SJ (2012) Immune function genes CD99L2, JARID2 and TPO show association with autism spectrum disorder. Mol Autism 3:4
Ray B, Long JM, Sokol DK, Lahiri DK (2011) Increased secreted amyloid precursor protein-α (sAPPα) in severe autism: proposal of a specific, anabolic pathway and putative biomarker. PLoS One 6:e20405
Ricci S, Fuso A, Ippoliti F, Businaro R (2012) Stress-induced cytokines and neuronal dysfunction in Alzheimer’s disease. J Alzheimers Dis 28:11–24
Rook GA, Lowry CA, Raison CL (2011) Lymphocytes in neuroprotection, cognition and emotion: is intolerance really the answer? Brain Behav Immun 25:591–601
Sacco R, Curatolo P, Manzi B, Militerni R, Bravaccio C, Frolli A, Lenti C, Saccani M, Elia M, Reichelt KL, Pascucci T, Puglisi-Allegra S, Persico AM (2010) Principal pathogenetic components and biological endophenotypes in autism spectrum disorders. Autism Res 3:237–252
Sokol DK, Chen D, Farlow MR, Dunn DW, Maloney B, Zimmer JA, Lahiri DK (2006) High levels of Alzheimer beta-amyloid precursor protein (APP) in children with severely autistic behavior and aggression. J Child Neurol 21:444–449
Vargas DL, Nascimbene C, Krishnan C, Zimmerman AW, Pardo CA (2005) Neuroglial activation and neuroinflammation in the brain of patients with autism. Ann Neurol 57:67–81
Vezzani A, Friedman A (2011) Brain inflammation as a biomarker in epilepsy. Biomark Med 5:607–614
Weinstein AA, Deuster PA, Francis JL, Bonsall RW, Tracy RP, Kop WJ (2010) Neurohormonal and inflammatory hyper-responsiveness to acute mental stress in depression. Biol Psychol 84:228–234
Ziats MN, Rennert OM (2011) Expression profiling of autism candidate genes during human brain development implicates central immune signaling pathways. PLoS One 6:e24691
Zunszain PA, Anacker C, Cattaneo A, Carvalho LA, Pariante CM (2011) Glucocorticoids, cytokines and brain abnormalities in depression. Prog Neuropsychopharmacol Biol Psychiatry 35:722–729
Acknowledgments
Research funded by REGIONE BASILICATA, ASP (Azienda Sanitaria Provinciale) Potenza, Italy—General Director Dott. Mario Marra; Center for Diet-Related diseases “G.Gioia”, CHIAROMONTE Hospital (PZ), ASP Potenza, Italy—Director Dott.ssa Rosa Trabace—Head of laboratory Dott.ssa Nicolina La Sala—Psychologist/Psychotherapist Dott.ssa Maria Tosti; ASP (Azienda Sanitaria Provinciale) Ospedale Chiaromonte/Lagonegro, Potenza, Italy—Pediatrician Dott. Rocco Orofino, MD—Childish Neuropsychiatrist Dott. Vincenzo D’Onofrio, MD—Administrative Manager Dott. Giacomo Chiarelli; ASP (Azienda Sanitaria Provinciale) Matera, Italy Hospital “Madonna delle Grazie” Department of Children and Adolescent Neuropsychiatry—Director U.O.C. Dott. Carlo Calzone, MD—Neuropsychiatrist Dott. Caterina Lattarulo, MD; Stella Maris Mediterraneo Foundation, ASP Potenza, Italy; Dr. Lars Göran Wallgren provided excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ricci, S., Businaro, R., Ippoliti, F. et al. Altered Cytokine and BDNF Levels in Autism Spectrum Disorder. Neurotox Res 24, 491–501 (2013). https://doi.org/10.1007/s12640-013-9393-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-013-9393-4