Abstract
We previously reported the propensity of Bacopa monnieri (BM) leaf powder to modulate endogenous levels of oxidative stress markers in the brain of prepubertal mice. In this study, we tested the hypothesis that pretreatment with an alcoholic extract of BM (BME) could provide neuroprotection against 3-nitropropionic acid (3-NPA)-induced oxidative stress under in vitro and in vivo conditions. In chemical systems, BME exhibited multiple free radical scavenging ability. Further, BME pretreatment completely abolished 3-NPA-induced oxidative stress response in brain (striatum, St) mitochondria in vitro. Likewise, pretreatment of dopaminergic (N27 cell lines) cells with BME not only abrogated the generation of reactive oxygen species (ROS) levels, but also offered marked protection against 3-NPA-mediated cytotoxicity. These findings were further validated employing a 3-NPA mice model in vivo. We determined the degree of oxidative stress induction, redox status, enzymic antioxidants, protein oxidation, and cholinergic function in various brain regions of male mice provided with BME for 10 days (prophylaxis) followed by 3-NPA challenge (75 mg/kg bw/day, i.p.). BME prophylaxis completely prevented 3-NPA-induced oxidative dysfunctions in St and other brain regions. 3-NPA-induced robust elevation of oxidative markers (malondialdehyde levels, ROS generation, hydroperoxide levels and protein carbonyls) in cytosol of brain regions was predominantly abolished among mice given BME prophylaxis. Interestingly, BME prophylaxis also prevented the depletion of reduced glutathione, thiol levels, and perturbations in antioxidant enzymes caused by 3-NPA. Collectively these findings provide evidence on the significant prophylactic neuroprotective efficacy of BME in prepubertal mice brain. Based on these data, it is hypothesized that BME can serve as a useful adjuvant in protecting brain against oxidative-mediated neurodegenerative disorders involving oxidative stress conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacopa monnieri (BM, Brahmi, family—Scrophulariaceae) is well-known traditionally in Ayurvedic system of medicine for its various neuropharmacological properties (Chopra 1958). Used as a brain tonic, BM is known to enhance memory, cognitive functions, promote longevity, and provide relief to patients with anxiety or epileptic disorders (Gohil and Patel 2010). Major chemical components viz., steroidal saponins—bacoside A and B are speculated to be responsible for the memory-facilitating action of BM (Shinomol and Muralidhara 2011). In addition, the presence of other phytoactives such as dammarane-type triterpenoid saponins with jujubogenin and pseudo-jujubogenin as the aglycones, bacosides A1–A3 (Rastogi and Kulshreshtha 1999), bacopasaponins A–G (Mahato et al. 2000), and bacopasides I–V (Chakravarty et al. 2003) have been reported in alcoholic extract of BM.
The biological effects of BM have been reviewed periodically (Shinomol et al. 2011a; Gohil and Patel 2010; Russo and Borrelli 2005). Recently, BM has been reported to exert protective effects in an animal model of ischemia-induced brain injury (Saraf et al. 2011). Administration of bacosides attenuated experimentally induced anterograde amnesia, improved memory in mice (Kishore and Singh 2005) and enhanced spatial learning performance as well as memory retention in rats (Vollala et al. 2010). Earlier, alcoholic extract of BM was shown to facilitate cognition, inhibit amnesic effects of scopolamine, electroshock, and immobilization stress in rats (Singh and Dhawan 1997). Standardized BM extract (BME) was previously reported to normalize stress-mediated transient deregulation of plasma corticosterone and monoamine changes in brain (Rai et al. 2003). Further, BME was shown to inhibit multiple components of the β-amyloid-induced oxidative stress pathway that can contribute to Alzheimer’s pathology and reduce β-amyloid levels in a transgenic mouse model (Dhanasekaran et al. 2007).
Various attributes such as metal ion chelation, upregulation of antioxidative enzymes, and scavenging of free radicals (Tripathi et al. 1996; Shinomol et al. 2011a) are believed to be responsible for the neuroprotective effects of BME. The antistress activity of BM in animal models is attributed to its potential to modulate the expression levels of Hsp70, cytochrome P450, superoxide dismutase (SOD), enhancement of kinase activity, neuronal synthesis, and restoration of synaptic activity (Chowdhuri et al. 2002; Kishore and Singh 2005). Despite the extensive usage of BM plant, its extracts and isolated bacosides, studies related to its prophylactic efficacy to render the brain tissue less vulnerable to neurotoxicant-induced oxidative dysfunctions are limited.
One of the long-term objectives of our laboratory has been to understand the potential of various natural compounds to modulate the endogenous antioxidant defenses in vivo and to exploit this ability to achieve neuroprotection. This approach would largely aid in identifying compounds which could be employed for targeting the pathways implicated in reactive oxygen species (ROS) production and oxidative stress (Dumont and Beal 2011). Earlier, we demonstrated the neuroprotective efficacy of BM against neurotoxicants viz., rotenone and paraquat in Drosophila (Hosamani and Muralidhara 2009, 2010). Further, our recent findings in prepubertal mice revealed the propensity of BM leaf powder to modulate the endogenous levels of oxidative markers in different brain regions (Shinomol and Muralidhara 2011). Hence, we hypothesized that BM prophylaxis is likely to render the brain less susceptible to oxidative stress-mediated neuronal dysfunctions. The hypothesis was tested in prepubertal mice administered with 3-NPA, a well-known fungal mitochondrial toxin which causes selective neuronal degeneration in the striatum (St). While the precise mechanism/s by which 3-NPA causes striatal degeneration is not known, various mechanisms including oxidative injury, glutamate receptor excitotoxicity, mitochondrial dysfunctions, and energy depletion have been proposed (Herrera-Mundo and Sitges 2010; Shinomol and Muralidhara 2008a, b; Beal and Ferrante 2004).
Accordingly, we examined the efficacy of BME to prevent 3-NPA-induced oxidative stress in cytosolic milieu in St and other brain regions. Initially, we established the antioxidant activity of BME in various chemical test systems as well as its potential to inhibit 3-NPA-induced oxidative stress in brain mitochondria in vitro. Further, the efficacy of BME to attenuate 3-NPA-induced oxidative stress response and cytotoxicity was evidenced in dopaminergic neuronal cells (N27cell line). To assess its in vivo neuroprotective efficacy, prepubertal mice were provided with BM prophylaxis (10 days) prior to the challenge with 3-NPA.
Materials and Methods
Chemicals
Thiobarbituric acid (TBA), 1,1,3,3-tetramethoxypropane, 2′,7′-dichloro-fluorescein (DCF), 2′,7′-dichloro-fluorescein diacetate (DCF-DA), 3-NPA, and other fine chemicals were procured from M/s Sigma Chemical Co., St Louis, USA. All other chemicals used were of analytical grade.
Animals and Care
Prepubertal male mice (CFT-Swiss, 4-week-old) drawn from the stock colony of the “institute animal house facility” were housed in polypropylene cages (three per cage) provided with dust free paddy husk as a bedding material. Mice were housed in a controlled atmosphere with a 12 h light/dark cycle. They were acclimatized for 1 week prior to the start of the experiment and were maintained on a powdered diet and tap water ad libitum. The experiments were conducted strictly in accordance with approved guidelines by the “Institute Animal Ethical Committee” regulated by the Committee for the purpose of Control and Supervision of Experiments on Animals (CPCSEA), Ministry of Social justice and Empowerment, Government of India, India (Registration number; 49/1999/CPCSEA).
Bacopa monnieri Powder and Ethanolic Extract
Bacopa monnieri plant was collected during early summer from the state of Kerala, India and authenticated by Prof. C.M Joy, Department of Botany, Sacred Heart College Thevara, Mahatma Gandhi University, Kerala, India. In brief, fresh BM plant was shade dried, the leaves were separated from the stem and powdered (using a mill) without production of much heat and was sieved through a 400 micron sieve. The ethanolic extract was prepared according to the method of Jyoti and Sharma (2006) with minor modifications. The percent total yield of the ethanolic extract was 20%. The HPLC chromatogram of the extract has been previously reported (Shinomol and Muralidhara 2011).
Free Radical Scavenging Potency of BM Extract In Vitro
Antioxidant Potential of BME: In Vitro Evidences
Chemical Systems: The antioxidant potential of BME was assessed employing a battery of chemical systems following the methods described previously (Shinomol and Muralidhara 2008b). The assay systems used were DPPH radical scavenging assay (Cotelle et al. 1996); nitric oxide scavenging assay (Marcocci et al. 1994); hydroxyl radical scavenging assay (Chung et al. 1997); superoxide scavenging assay (Robak and Gryglewski 1998); deoxyribose oxidation assay (Halliwell et al. 1987); and iron chelation assay (Carter 1971).
Inhibition of 3-NPA-Induced Oxidative Stress in Mitochondria of Brain Regions In Vitro
Mitochondria isolated from different brain regions viz., cortex (Ct), cerebellum (Cb), hippocampus (Hc), and St were preincubated with BME (0.5 and 1 μg/ml) for 30 min. Further, untreated and BME pretreated mitochondria were exposed to 3-NPA (2 mM) for 1 h. The extent of oxidative damage was evaluated in terms of malondialdehyde (MDA) formation, ROS generation, and hydroperoxide levels.
Experiments in N27 Cells
Rat dopaminergic cell line 1RB3AN27 (N27) cells used in this study was grown and maintained as described earlier (Jagatha et al. 2008). In brief, cells were grown in RPMI 1640 medium containing 10% fetal bovine serum, penicillin (100 units/ml), and streptomycin (100 μg/ml) and maintained at 37°C in a humidified atmosphere of 5% CO2/95% air. Cells were subcultured once a week via trypsin treatment. Initially, confluent N27 cells (in 96-well plates) were exposed first to 3-NPA at various concentrations for 24 h to determine the LC50 value. Further experiments were conducted by pretreating cells with BME at various concentrations for first 24 h followed by exposure to 3-NPA (LC50—4 mM) for an additional 24 h. At the end of treatment, the neuroprotective potency of BME against cell death was assessed by cell viability assay. Further the modulatory effect of BME (2, 4, and 6 μg/ml) was assessed employing a sublethal (3 mM) concentration of 3-NPA.
For cell survival studies, cells were seeded in 96-well plates at a density of 5,000 cells per well. Following treatment of untreated or BME pretreated cells with 3-NPA (3 mM), viability was determined using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) as described earlier (Vali et al. 2007).
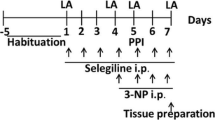
Prophylactic Efficacy of BME Against 3-NPA-Induced Oxidative Stress In Vivo
The criteria of dosage selection of 3-NPA was based on our previous studies (Shinomol and Muralidhara 2008b). The dosage of BME was selected based on a preliminary dose-determinative study. Prepubertal male mice were orally administered with BME (5 mg/kg bw) for a period of 10 days (prophylaxis group). Both untreated and mice given BME prophylaxis were administered 3-NPA (75 mg/kg bw, i.p.) on days 9 and 10 and killed 24 h after the last dose. Mice given physiological saline served as the untreated controls. Biochemical analysis was carried out in cytosolic preparations obtained from St and brain regions viz., Ct, Cb, and Hc.
Preparation of Cytosolic and Mitochondrial Fractions
Cytosolic fractionation of N27 cells: Cells were harvested by trypsin treatment and homogenates were prepared on ice using a glass homogenizer in ice-cold phosphate buffered saline (pH 7.4). Later the homogenates were sonicated for two cycles of 5 s each, centrifuged at 10,000×g for 10 min and the supernatant was used for biochemical assays.
Cytosolic fractionation of brain regions: 10% homogenate of each brain region was prepared in ice-cold phosphate buffer (0.1 M; pH 7.4) using a glass–teflon grinder at 4°C, centrifuged at 1000×g for 10 min at 4°C to obtain the nuclear pellet. Crude cytosol was prepared by centrifuging the post-nuclear supernatant at 10,000×g for 20 min at 4°C. The pellet was discarded and the supernatant was used for assays.
Preparation of mitochondrial fractions: Mitochondria were prepared by differential centrifugation according to the method of Moreadith and Fiskum (1984) and Trounce et al. (1996) with minor modifications.
Biochemical Analysis
Determination of Lipid Peroxidation
Induction of oxidative damage was ascertained by measuring the extent of lipid peroxidation (LPO) in the cytosol of different brain regions (Ct, Cb, Hc, and St). LPO was quantified by measuring the formation of TBA reactive substances (TBARS) following the method described earlier (Ohkawa et al. 1979).
Measurement of ROS Generation
ROS generation in brain regions or N27 cells was assayed using dihydro-dichlorofluorescein diacetate (H2 DCFH-DA), a non-polar compound that, after conversion to a polar derivative by intracellular esterases, can rapidly react with ROS to form the highly fluorescent compound dichlorofluorescein (Shinomol and Muralidhara 2007). ROS formation was calculated from a DCF-standard curve and the data was expressed as p mol DCF formed/min/mg protein.
Measurement of Hydroperoxide Levels
The hydroperoxide levels were determined in cytosolic fractions following the method described previously (Wolff 1994) and results were expressed as μmoles hydroperoxides (HP)/mg protein
Measurement of Protein Carbonyls
Protein carbonyl content in cytosolic fractions was determined according to the method of Levine et al. (1990) and the results were expressed as nmoles carbonyls/mg protein using MEC 22.0 mM−1 cm−1.
Determination of Reduced Glutathione
Reduced glutathione (GSH) content was measured according to the fluorimetric method of Mokrasch and Teschke (1984). Concentration of GSH was calculated from a standard curve and the values were expressed as μg GSH/mg protein.
Quantification of Total Thiols and Non-Protein Thiols
The levels of total thiols and non-protein thiols were determined according to the method of Ellman (1959). The levels were calculated using MEC 13.6 mM−1 cm−1 and expressed as nmol oxidized DTNB formed/mg protein.
Determination of Ascorbic Acid
Ascorbic acid (AA) content in different brain regions was analyzed by 2,4-dinitrophenyl-hydrazine method as described earlier (Omaya et al. 1979) and concentration was expressed as ng/mg tissue using AA standard.
Estimation of Iron Levels
Iron content in the samples was determined by bathophenanthroline method (Peters et al. 1956) with minor modifications and expressed as OD/mg protein. This method is a sensitive colorimetric method for determining both the intrinsic and added iron. The method measures only the non-heme iron as compared to atomic absorption spectroscopy which determines both heme and non-heme iron.
Activities of Antioxidant Enzymes
Each brain region was homogenized in phosphate buffer (50 mM, pH 7.4) and sonicated at 4°C. The activities of antioxidant enzymes viz., catalase, glutathione-S-transferase, glutathione peroxidase, and SOD were measured in cytosolic fractions with minor modifications (Aebi 1984; Flohe and Gunzler 1984; Guthenberg et al. 1985; McCord and Fridovich 1969).
Activities of Cholinergic Enzymes
Activities of acetylcholinesterase (AChE) and butyrylcholinesterase (BuChE) were determined according to the method of Ellmann et al. (1961). The enzyme activities were expressed as nmoles of substrate hydrolyzed/min/mg protein.
Determination of Protein
Protein content in mitochondria and cytosol were determined according to the method of Lowry et al. (1951), using bovine serum albumin as the standard.
Statistical Analysis
Experimental data obtained were expressed as mean ± standard deviation (SD) and analyzed by one-way analysis of variance (ANOVA) using SPSS software for windows (version 10.0.1., SPSS Inc, New York, 1999). The in vitro data were analyzed only by one-way ANOVA. Post hoc multiple comparisons were performed between groups using Duncan’s Multiple Range Test (DMRT) in all the studies. A “P” value <0.05 was taken as significant throughout the study.
Results
Free Radical Scavenging Potency of BME In Vitro
BME was able to reduce the stable free radical DPPH to the yellow colored, 1,1-diphenyl-2-picrylhydrazyl in a concentration-dependent manner (IC50: 9.41 μg/ml compared to BHT standard: IC50: 4.16 μg/ml). Likewise, BME was also found to scavenge nitric oxide radicals in a concentration-dependent manner (IC50: 9.21 μg/ml). Further, BME exerted a concentration-dependent superoxide radical (IC50: 10 μg/ml vs. standard caffeic acid: IC50: 4.15 μg/ml) and hydroxyl radical scavenging activity (IC50: 436.77 μg/ml compared to BHT standard: IC50: 6.85 μg/ml). In the deoxyribose oxidation assay, BME elicited a concentration-dependent inhibition of deoxyribose oxidation (IC50: 217.34 μg/ml). Interestingly, BME also showed concentration-dependent iron chelation effect (IC50:160 μg/ml) in comparison to the chelating effect of the standard iron chelator, EDTA (IC50: 50 μg/ml).
Inhibition of 3-NPA-Induced Oxidative Impairments in Brain Mitochondria In Vitro
BME per se caused significant diminution of basal MDA levels (39–49%) at both concentrations in striatum mitochondria, while 3-NPA (2 mM) markedly elevated the MDA levels (113%). BME pretreatment completely inhibited the 3-NPA-induced LPO. Likewise, 3-NPA exposure resulted in robust ROS generation (120%) and HP levels (126%) in striatal mitochondria which were also abolished by BME pretreatment (Fig. 1).
Attenuation of 3-NPA-induced oxidative stress by Bacopa monnieri ethanolic extract (BME) in mitochondria of brain regions of male mice in vitro. Data analyzed by one-way ANOVA (analysis were made between control vs. BME alone § P < 0.05; control vs. 3-NPA *P < 0.001; 3-NPA vs. BME + 3-NPA # P < 0.0.05). Ct Cortex, Cb cerebellum, Hc hippocampus, St striatum, MDA malondialdehyde, ROS reactive oxygen species, HP hydroperoxides, 3-NPA 3-nitropropionic acid (2 mM)
In mitochondria of other brain regions, BME alone significantly diminished the basal levels of MDA (38–67%), ROS (15–47%), and HP levels (10–37%). While, 3-NPA exposure markedly elevated the MDA levels, BME pretreatment completely inhibited the induction of LPO. Likewise, 3-NPA also caused marked enhancement in the levels of ROS and HP in mitochondria of other brain regions which were also abolished by BME pretreatment (Fig. 1).
Modulatory Effect of BME in N27 Cells
Toxicity Profile of 3-NPA in N27 Cells
From our preliminary study, we computed the 24 h LC50 for 3-NPA in N27 cells as 4 mM.
Modulation of 3-NPA-mediated cytotoxicity
BME pretreatment conferred a concentration-dependent protective effect against 3-NPA (4 mM)-induced cell death as evidenced in the MTT assay (Fig. 2a). While BME per se was devoid of cytotoxic effect even at the highest concentration (6 μg), it offered significant concentration-dependent protection (10–35%) against 3-NPA-induced cell death.
Neuroprotection against 3-nitropropionic acid (3-NPA)-induced cytotoxic response in N27 cells by pretreatment with Bacopa monnieri ethanolic extract (BME) as measured by MTT assay (a); ROS generation (b); and hydroperoxide levels (c). Values are mean ± SD of six determinations each. Data analyzed by one-way ANOVA (analysis were made between control vs. BME alone § P < 0.05; control vs. 3-NPA *P < 0.001; 3-NPA vs. BME + 3-NPA # P < 0.05; ## P < 0. 01; ### P < 0. 001). NS Not significant
Abrogation of 3-NPA-Induced ROS Generation and Hydroperoxides
Treatment of N27 cells with BME alone was associated with significantly (14–32%) lower levels of ROS. Further, 3-NPA treatment caused a dramatic (nearly 4-folds) elevation in the ROS generation (as reflected by increased fluorescence intensity) compared to untreated control cells. Interestingly, pretreatment of cells with BME extract offered varying degree (20–100%) of protection against 3-NPA-induced ROS generation (Fig. 2b). Likewise, treatment of cells with BME alone resulted in a significant (10–40%) reduction in the basal levels of HP. While robust (nearly 3-folds) elevation was evident in the HP levels among cells exposed to 3-NPA, BME pretreatment caused significant diminution of 3-NPA-induced HP levels (Fig. 2c).
Prophylactic Efficacy Against 3-NPA-Induced Oxidative Dysfunctions In Vivo
Body Weight, Organ Weights, and Food Intake
3-NPA administration caused a marginal decrease (15%) in body weight and significant decrease in the weights of liver (21%), heart (20%), spleen (24%), and thymus (48%). 3-NPA caused only a marginal decrease in food intake (data not shown).
Attenuation of 3-NPA-Induced Oxidative Dysfunctions in Brain Regions
Striatum: BME treatment alone resulted in a significant decrease in the basal levels of oxidative markers in cytosol (MDA-23%; ROS-24%; HP-38%). Among mice administered 3-NPA, the cytosol of St exhibited robust elevation in MDA (70%), ROS (65%), and HP (57%) levels suggesting induction of oxidative stress in vivo. Interestingly, BME prophylaxis significantly diminished 3-NPA-mediated oxidative damage (Fig. 3).
Modulatory effects of BM extract prophylaxis on 3-NPA-induced oxidative impairments in cytosol of brain regions of prepubertal male mice (Ct Cortex, Cb cerebellum, Hc hippocampus, St striatum). Values are mean ± SD (n = 6). Data analyzed by one-way ANOVA (P < 0.05) followed by post hoc “Tukey” test. Means followed by different letters differ significantly; BME-Bacopa monnieri ethanolic extract (5 mg/kg bw/day for10 days); 3-NPA-3-nitropropionic acid (75 mg/kg bw/day for 2 days). MDA Malondialdehyde, ROS reactive oxygen species, HP hydroperoxide, PC protein carbonyls
Other Brain Regions: BME treatment alone also caused diminution in the endogenous levels of oxidative markers in cytosol of other brain regions. 3-NPA administration caused a marked increase in the levels of MDA (56–71%), ROS (44–58%), and HP (34–45%) in all brain regions of untreated mice, which were significantly decreased among mice given BME prophylaxis (Fig. 3).
Protective Effect Against Protein Carbonyls Formation
BME treatment alone caused a significant (26%) decrease in protein carbonyls content in St and other brain regions (22–34%). On the other hand, 3-NPA administration significantly enhanced the protein carbonyls content in St (38%) and other brain regions (23–48%). However, brain regions of mice given BME prophylaxis were completely resistant to 3-NPA-induced protein oxidative damage (Fig. 3).
Effect of BME on Reduced Glutathione and Thiol Status
Striatum: BME treatment alone resulted in enhanced levels of GSH (25%), total thiols (21%), and non-protein thiols (20%). However, 3-NPA administration was associated significant depletion of GSH (23%), total thiols (21%), and non-protein thiols (19%) in straitum. However, BME prophylaxis prevented 3-NPA-mediated depletion of GSH and total thiols (Table 1).
Other Brain Regions: BME treatment alone also resulted in significant increase in GSH levels (19–30%), TSH (19–25%), and non-protein thiols (10–23%). On the other hand, 3-NPA administration resulted in varying levels of depletion in GSH, total thiols, and non-protein thiols (Table 1). A sustained increase (Ct-50%; Cb-33%; Hc-20%) was observed in GSSG levels on exposure to 3-NPA, where as marginal decrease (10–15%) was observed in BME prophylaxis group (data not shown). However, mice given BME prophylaxis were not susceptible to 3-NPA-induced depletion of antioxidant molecules, suggesting total protection (Table 1).
Effect on Antioxidant Enzymes
Striatum: BME treatment alone significantly enhanced the activities of antioxidant enzymes in St (CAT: 34%; GPx: 17%; SOD: 35%). However, 3-NPA administration resulted in significant decrease in catalase (37%), GPx (25%) and SOD (19%) activity levels, while increasing GST activity (15–27%). In contrast, mice provided with BME prophylaxis exhibited normal levels of enzyme activities despite 3-NPA administration, indicating neuroprotective effect of BME (Table 2).
Other Brain Regions: In general, BME treatment alone enhanced the activities of antioxidant enzymes in other brain regions (Table 2). However, 3-NPA administration resulted in significant decrease in GPx (25%) and SOD (21–27%) activity levels, while increasing GST activity (14–27%). Further, varying degree of normalization in enzyme activities occurred among mice given BME prophylaxis (Table 2).
Status of Iron and Vitamin C Levels
BME treatment alone caused a general decease in free iron levels in St (27%) and other brain regions (Ct-20%; Cb-14%; Hc-30%). In contrast, 3-NPA administration caused a significant increase in free iron levels in St (40%) and other brain regions (Ct-21%; Cb-47%; Hc-33%). Interestingly, BME prophylaxis caused in marked reduction in the free iron levels in St and other regions of mice administered 3-NPA (Table 3).
BME treatment alone did not have any effect on the vitamin C levels in any of the brain regions. However, 3-NPA administration caused a marginal decrease in the vitamin C levels in St and Ct, while the levels were higher in Cb and Hc, and BME prophylaxis had no effect on 3-NPA-induced alterations (Table 3).
Activity of Cholinergic Enzymes
BME treatment alone caused significant decrease in the activities of AChE in St (18%) and other brain regions (18–32%). The activity of BChE was also decreased (13–23%) in all the brain regions. 3-NPA administration reduced the activities of AChE in St (20%) and other brain regions (14–32%). Likewise 3-NPA administration also significantly decreased the activities of BChE in all the brain regions (10–45%). However, among mice given BME prophylaxis and administered 3-NPA, the activity levels of AChE were higher (Fig. 4).
Effects of BM extract prophylaxis on 3-NPA-induced perturbations in the AChE and BuChE in brain regions of prepubertal male mice Values are mean ± SD (n = 6). Data analyzed by one-way ANOVA (P < 0.05) followed by post hoc “Tukey” test. Means followed by different letters differ significantly (Ct Cortex, Cb cerebellum, Hc hippocampus, St striatum); BME: Bacopa monnieri ethanolic extract (5 mg/kg bw/day for 10 days). 3-NPA: 3-nitropropionic acid (75 mg/kg bw/day for 2 days)
Discussion
Establishing new lines of evidence on the neuroprotective properties of BM assumes greater relevance since several over-the-counter formulations of BM are currently available resulting in increased human consumption. In general, BM is advocated for the treatment of anxiety, improvement of intellect/memory among children and adults as well as in the treatment of various neurological disorders (Singh and Dhawan 1997; Russo and Borrelli 2005; Shinomol et al., 2011a). Previously, we demonstrated the ability of BM-enriched diet to diminish endogenous levels of oxidative markers, enhance the redox status (reduced GSH and total thiols) and increase in the activities of several antioxidant enzymes in brain regions of prepubertal mice (Shinomol and Muralidhara, 2011). In view of this, we tested the hypothesis that prophylaxis with BME could offset neurotoxicant-induced oxidative stress in prepubertal mice brain.
Alcoholic extract of BM has been tested by numerous researchers since it contains several types of saponins including Bacopa saponins (A, B, C, and D), pseudojujobogenins, bacopaside I, II, III, IV, and V (Chakravarty et al. 2003; Deepak et al. 2005). Hence in this study, we employed an alcoholic extract of BM to obtain evidences in favor of our hypothesis. The HPLC chromatogram of our extract was highly identical with previously published data (Deepak et al. 2005; Shinomol and Muralidhara 2011). Our findings employing chemical systems with BME demonstrated the ability to scavenge various radicals, clearly suggesting its multiple mechanism of action in vitro. BME effectively scavenged DPPH, superoxide, and nitric oxide radicals and showed significant inhibition of deoxyribose oxidation. These data corroborate with earlier findings in which BME exhibited robust antioxidative activity against hydrogen peroxide-induced LPO and blocked the activity of lipoxygenase in vitro (Dhanasekaran et al. 2007). Further, in this study BME also exhibited significant metal chelation in vitro, indicating its potential to chelate divalent iron in vivo. The ability of BM to scavenge diverse free radicals as well as its chelating property indicates the presence of several neuroprotective antioxidant compounds in the extract which may be highly effective in regulating the dyshomeostasis of redox-active biometals including copper and iron which are suggested to contribute to the neuropathology of Alzheimer’s disease (Mattson and Chan 2003; Dumont and Beal 2011).
Having established the potential of BME to scavenge free radicals in chemical systems, we further examined its efficacy to inhibit 3-NPA-induced oxidative stress in mitochondria isolated from different brain regions of mice in vitro. Striatal mitochondria were more sensitive to 3-NPA-induced oxidative damage. However, in the presence of BME, 3-NPA failed to enhance the levels of any oxidative markers suggesting total protection at the tested concentrations. This effect was consistent irrespective of the brain region indicating the ability of BME to protect different brain regions. Interestingly, these protective effects were highly reproducible in a dopaminergic cell model in which BME pretreatment effectively reduced 3-NPA-mediated cytotoxicity. In the cell model, BME pretreatment offered significant protection against 3-NPA-induced cell death and strongly inhibited oxidative stress induction response as evidenced by reduced formation of ROS and HP. Since 3-NPA toxicity is known to be mediated by oxidative damage, the protective effects of BME observed could be a direct reflection of its antioxidative potency. Further mechanistic studies are in progress to identify specific mechanism/s by which BME offers neuroprotection in the cell model.
Based on these evidences, we examined the neuroprotective efficacy of BME employing a prophylactic approach in a prepubertal mice model. BM has been used in Ayurvedic medicine for several hundred years and the therapeutic doses are not associated with any known side-effects (Allan et al. 2007). In this study, BME was administered to prepubertal mice only for 10 days. As anticipated, administration of 3-NPA to prepubertal mice induced robust oxidative stress in both cytosolic and mitochondrial fractions of St and other brain regions (Shinomol and Muralidhara 2008b). Our salient findings viz., marked elevation in ROS and MDA levels, alterations in the activities of antioxidant enzymes, diminished GSH levels and enhanced protein carbonyl levels in St and other brain regions clearly suggested the existence of state of oxidative stress in vivo. These findings are in direct agreement with previous reports (Binienda et al. 1998; Shinomol and Muralidhara 2008a, b; Shinomol et al. 2009). Interestingly, BME prophylaxis completely attenuated 3-NPA-induced oxidative stress in cytosol in St as well as other brain regions suggesting its ability to render protection against neurotoxicant insult. These data corroborate our recent findings in which BM-enriched diet not only significantly diminished the basal levels of oxidative markers in Drosophila melanogaster, but also offered marked protection against rotenone as well as paraquat-induced oxidative stress, locomotor deficits, and mortality (Hosamani and Muralidhara 2009, 2010). Similarly, we have evidenced the prophylactic efficacy of BME against 3-NPA-induced oxidative stress and mitochondrial dysfunctions in St (Shinomol et al. 2011b).
GSH-associated metabolism is a major mechanism for cellular protection against toxicants which generate oxidative stress. It is becoming increasingly apparent that the glutathione tripeptide is central to a complex multifaceted detoxification system, where there is substantial inter-dependence between separate component members. GSH participates in detoxification at several levels, and may scavenge free radicals, reduce peroxides or be conjugated with electrophilic compounds. Thus, GSH provides the cell with multiple defenses not only against ROS, but also against their toxic products (Bharath and Andersen 2005; Aoyama et al. 2008). In this study, BME per se significantly enhanced the basal levels of GSH, total/non-protein thiols in cytosol of all brain regions in prepubertal mice. Interestingly, BME prophylaxis offered marked protection against 3-NPA-induced GSH depletion as evident by the restoration of GSH levels in St as well as other brain regions. Hence, we speculate that GSH-related mechanism/s may play a significant role in the observed neuroprotective effect of BME against 3-NPA-induced oxidative stress. In addition, the observed enhanced levels of enzymatic antioxidant defenses in St and other brain regions could also have played a significant role in ameliorating the effects of 3-NPA. The ability of BME to uniformly upregulate the GSH levels and related defenses provides a highly useful paradigm to attenuate oxidative damage-mediated neurodegenerative disorders. Another important finding in the in vivo study was a general decrease in the free iron levels in cytoplasm of St and other brain regions of mice given BME prophylaxis. This suggests that the strong iron chelating ability of BME could complement its other antioxidant mechanisms in rendering brain less vulnerable to neurotoxic insults.
Elevated levels of protein carbonyls are considered as sensitive index of protein oxidation and have been implicated in pathophysiolgy of various neurodegenerative diseases (Butterfield et al. 2010). In the present model, we observed elevated levels of the protein carbonyls in cytosol of all brain regions among 3-NPA administered mice especially in the St, whereas BME prophylaxis completely prevented the protein oxidation. It is suggested that protein carbonyl formation might be due to ROS-mediated oxidation of amino acid side chains or by covalent binding to products of LPO or glycoxidation (Butterfield and Stadtman, 1997). The elevated levels probably reflect a very low rate of oxidized protein degradation and or low repair activity (Dalle-Donne et al. 2003). We speculate that the protective effect observed with BME prophylaxis is probably due to the high antioxidant capacity of the extract.
It is well known that inhibition of AChE is an important therapeutic target for the treatment of neurodegenerative diseases (Kaufer et al. 1999; Meshorer et al. 2002). Significant decrease in the activity of AChE indicates an increase in the acetylcholine levels in the synaptic cleft and is known to enable an improvement in cognitive functions such as learning and memory. In this study, brain regions of mice provided with BME prophylaxis exhibited consistent reduction in the activities of cholinergic enzymes viz., AChE and BChE clearly suggesting alterations in cholinergic functions in vivo. Previously, subchronic administration of bacosides-rich extract of BM was shown to reverse the experimentally induced cognitive deficits and reduction in acetylcholine concentration in frontal Ct/Hc (Bhattacharya et al. 1999). However, 3-NPA administration also caused a reduction in the activity levels of AChE among untreated mice, while the activity of levels were higher among mice given BME prophylaxis. Although speculative, the higher levels of AChE in the prophylaxis group are most likely to be result of the counter-regulatory mechanism to compensate the reduced levels. However, this needs to be experimentally verified.
In conclusion, our findings clearly demonstrate the prophylactic neuroprotective efficacy of BME as it markedly prevented 3-NPA-induced oxidative stress in vivo. Based on the data obtained in chemical systems and N27 cells, we hypothesize that the antioxidative property may be partly responsible for its neuroprotective action. Further, our findings in the mouse model give credence to the prophylactic neuroprotective efficacy of BME in offsetting the neurotoxicant-induced oxidative stress uniformly in all the brain regions. While the precise mechanism/s by which the bioactive components of BM protect brain against cytosolic oxidative stress and mitochondrial dysfunctions merit further study, we hypothesize that it may be predominantly related to its robust antioxidant potency, upregulation of enzymatic antioxidant defenses and enhanced GSH/thiol status. These findings besides illustrating the ability of BM to offset neurotoxicant-induced brain oxidative stress strongly emphasize the need to further identify the specific biochemical pathways responsible for the neuroprotective propensity of BM phytochemicals. This assumes importance as BM is widely consumed by general human population and is also being employed as a therapeutic agent to alleviate various neurodegenerative disorders.
Abbreviations
- LPO:
-
Lipid peroxidation
- ROS:
-
Reactive oxygen species
- TBARS:
-
Thiobarbituric acid reactive substances
- MDA:
-
Malondialdehyde
- DCF:
-
2′,7′-Dichloro-fluorescein
- DCF-DA:
-
2′,7′-Dichloro-fluorescein diacetate
- BM:
-
Bacopa monnieri
References
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126
Allan J, Damodaran A, Deshmukh NS, Goudar KS, Amit A (2007) Safety evaluation of a standardized phytochemical composition extracted from Bacopa monnieri in Sprague-Dawley rats. Food Chem Toxicol 45:1928–1937
Aoyama K, Watabe M, Nakaki T (2008) Regulation of neuronal glutathione synthesis. J Pharmacol Sci 108:227–238
Beal MF, Ferrante RJ (2004) Experimental therapeutics in transgenic mouse models of Huntington’s disease. Nat Rev Neurosci 5:373–384
Bharath S, Andersen JK (2005) Glutathione depletion in a midbrain-derived immortalized dopaminergic cell line results in limited tyrosine nitration of mitochondrial complex I subunits: implications for Parkinson’s disease. Antioxid Redox Signal 7:900–910
Bhattacharya SK, Kumar A, Ghosal S (1999) Effect of Bacopa monniera on animal models of Alzheimer’s disease and perturbed central cholinergic markers of cognition in rats. Res Commun Pharmacol Toxicol 4:1–12
Binienda Z, Simmons C, Hussain S, WJr Slikker, Ali SF (1998) Effect of acute exposure to 3-nitropropionic acid on activities of endogenous antioxidants in the rat brain. Neurosci Lett 251:173–176
Butterfield DA, Stadtman ER (1997) Protein oxidation processes in aging brain. Adv Cell Aging Gerontol 2:161–191
Butterfield DA, Hardas SS, Lange ML (2010) Oxidatively modified glyceraldehyde-3-phosphate dehydrogenase (GAPDH) and Alzheimer’s disease: many pathways to neurodegeneration. J Alzheimers Dis 20:369–393
Carter P (1971) Spectrophotometric determination of serum iron at submicrogram level with a new reagent (ferrozine). Anal Biochem 40:450–458
Chakravarty AK, Garai S, Masuda K, Nakane T, Kawahara N (2003) Bacopasides III–V: three new triterpenoid glycosides from Bacopa monniera. Chem Pharm Bull 51:215–217
Chopra RN (1958) Indigenous drugs of India, 2nd ed. U.N. Dhur and Sons, Calcutta, p 341.22
Chowdhuri DK, Parmar D, Kakkar P, Shukla R, Seth PK, Srimal RC (2002) Antistress effects of bacosides of Bacopa monnieri: modulation of Hsp70 expression, superoxide dismutase and cytochrome P450 activity in rat brain. Phytother Res 16:639–645
Chung SK, Osawa T, Kawakishi S (1997) Hydroxyl radical scavenging effects of spices and scavengers from Brown Mustard (Brassica nigra). Biosci Biotech Biochem 61:118–123
Cotelle A, Bernier JL, Catteau JP, Pommery J, Wallet JC, Gaydou EM (1996) Antioxidant properties of hydroxyl-flavones. Free Radic Biol Med 20:35–36
Dalle-Donne I, Rosi R, Giustarini D, Milzani A, Colombo R (2003) Protein carbonyl groups as biomarkers of oxidative stress. Clin Chim Acta 329:23–38
Deepak M, Sangli GK, Arun PC, Amit A (2005) Quantitative determination of the major saponin mixture bacoside A in Bacopa monnieri by HPLC. Phytochem Anal 16:24–29
Dhanasekaran M, Tharakan B, Holcomb LA, Angie RH, Young KA, Manyam BV (2007) Neuroprotective mechanisms of ayurvedic antidementia botanical Bacopa monniera. Phytother Res 21:965–969
Dumont MF, Beal M (2011) Neuroprotective strategies involving ROS in Alzheimer disease. Free Radic Biol Med 51:1014–1026
Ellman GE (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82:70–77
Ellmann GE, Courtney KD, Andersen V, Featherstone RM (1961) A new and rapid colorimetric determination of acetyl cholinesterase activity. Biochem Pharmacol 7:88–95
Flohe L, Gunzler WA (1984) Assays of glutathione peroxidase. Methods Enzymol 105:114–121
Gohil KJ, Patel JA (2010) A review on Bacopa Monneira: Current research and future prospects. Intl J Green Pharma 4:1–9
Guthenberg C, Alin P, Mannervik B (1985) Glutathione transferase from rat testis. Methods Enzymol 113:507–510
Halliwell B, Gutteridge JM, Aruoma OI (1987) The Deoxyribose method: a simple test tube assay for determination of rate constants for reactions of hydroxyl radicals. Anal Biochem 165:215–259.23
Herrera-Mundo N, Sitges M (2010) Mechanisms underlying striatal vulnerability to 3-nitropropionic acid. J Neurochem 114:597–605
Hosamani R, Muralidhara (2009) Neuroprotective effects of Bacopa monnieri against rotenone induced oxidative stress and neurotoxicity in Drosophila melanogaster. NeuroToxicology 30:987–995
Hosamani R, Muralidhara (2010) Prophylactic treatment with Bacopa monnieri leaf powder mitigates Paraquat induced lethality and oxidative stress in Drosophila melanogaster. Indian J Biochem Biophys 47:75–82
Jagatha B, Mythri RB, Vali S, Bharath MM (2008) Curcumin treatment alleviates the effects of glutathione depletion in vitro and in vivo: therapeutic implications for Parkinson’s disease explained via in silico studies. Free Radic Biol Med 44:907–917
Jyoti A, Sharma D (2006) Neuroprotective role of Bacopa monnieri extract against aluminium-induced oxidative stress in the hippocampus of rat brain. NeuroToxicology 27:451–457
Kaufer D, Friedman A, Seidman S, Soreq H (1999) Anticholinesterases induce multigenic transcriptional feedback response suppressing cholinergic neurotransmission. Chem Biol Interact 119–120:349–360
Kishore K, Singh M (2005) Effect of bacosides, alcoholic extract of Bacopa monniera Linn (Brahmi) on experimental amnesia in mice. Indian J Exp Biol 43:640–645
Levine RL, Garland D, Oliver CN, Amici A, Climent I, Lenzi A, Ahn BW, Shaltiel S, Stadtman ER (1990) Determination of carbonyl content in oxidatively modified proteins. Methods Enzymol 186:464–478
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement using folin-phenol reagent. J Biol Chem 193:265–275
Mahato SB, Garia S, Chakravarty AK (2000) Bacopasaponins E and F: two jujubogenin bisdesmodies from Bacopa monniera. Phytochemistry 53:711–714
Marcocci L, Maguire JJ, Droy-Lefaix MT, Packer L (1994) The nitric oxide-scavenging properties of Ginkgo biloba extract EGb 761. Biochem Biophys Res Commun 201:748–755
Mattson MP, Chan SL (2003) Neuronal and glial calcium signalling in Alzheimer’s disease. Cell Calcium 34:385–397
McCord JM, Fridovich I (1969) Superoxide dismutase- An enzymic function for erythrocuprein (Hemocuprein). J Biol Chem 244:6049–6055
Meshorer E, Erb C, Gazit R, Pavlovsky L, Kaufer D, Friedman A, Glick D, Ben-Arie N, Soreq H (2002) Alternative splicing and neuritic mRNA translocation under long-term neuronal hypersensitivity. Science 295:508–512
Mokrasch LC, Teschke EJ (1984) Glutathione content of cultured cells and rodent brain regions: a specific fluorimetric assay. Anal Biochem 140:506–509
Moreadith RW, Fiskum G (1984) Isolation of mitochondria from ascites tumor cells permeabilized with digitonin. Anal Biochem 137:360–367
Ohkawa H, Ohnishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Omaya ST, Turnball JD, Sauberlich HE (1979) Selected methods for dtermination of ascorbic acid in animal cells, tissues and fluids (ascorbic acid). Methods Enzymol 62:1–11
Peters T, Giovanniello TJ, Apt L, Ross JF (1956) A simple improved method for the determination of serum iron. J Lab ClinMed 48:280–288
Rai D, Bhatia G, Palit G, Pal R, Singh S, Singh HK (2003) Adaptogenic effect of Bacopa monniera (Brahmi). Pharmacol Biochem Behav 75:823–830
Rastogi S, Kulshreshtha DK (1999) Bacoside A2—a triterpenoid saponin from Bacopa monniera. Indian J Chem 38:353–356
Robak J, Gryglewski RJ (1998) Flavanoids are scavengers of superoxide anions. Biochem Pharmacol 37:837
Russo A, Borrelli F (2005) Bacopa monnieri, a reputed nootropic plant: an overview. Phytomedicine 12:305–317
Saraf MK, Prabhakar S, Khanduja KL, Anand A (2011) Bacopa monnieri attenuates scopalmine-induced impairment of spatial memory in mice Evidence-based complementary and alternative medicine. doi:10.1093/ecam/neq038
Shinomol GK, Muralidhara (2007) Differential induction of oxidative impairments in brain regions of male mice following subchronic consumption of Khesari dhal (Lathyrus sativus) and detoxified khesari dhal. NeuroToxicology 28:798–806
Shinomol GK, Muralidhara (2008a) Effect of Centella asiatica leaf powder on oxidative markers in brain regions of prepubertal mice in vivo and its in vitro efficacy to ameliorate 3-NPA-induced oxidative stress in mitochondria. Phytomedicine 15:971–984
Shinomol GK, Muralidhara (2008b) Prophylactic neuroprotective property of Centella asiatica against 3-nitropropionic acid induced oxidative stress and mitochondrial dysfunctions in brain regions of prepubertal mice. NeuroToxicology 29:948–957
Shinomol GK, Muralidhara (2011) Bacopa monnieri modulates endogenous cytoplasmic and mitochondrial oxidative markers in prepubertal mice brain. Phytomedicine 18:317–326
Shinomol GK, Hosamani R, Muralidhara (2009) Prophylaxis with Centella asiatica confers protection to prepubertal mice against 3-nitropropionic acid induced oxidative stress in the brain. Phytother Res 24:885–892
Shinomol GK, Muralidhara, Bharath MMS (2011a) Exploring the role of Brahmi (Bacopa monnieri and Centella asiatica) in brain function and therapy. Recent Patents Endocr Metab Immune Drug Discov 5:33–49
Shinomol GK, Muralidhara, MMS Bharath (2011b) Pretreatment with Bacopa monnieri extract offsets 3-nitropropionic acid -induced mitochondrial oxidative stress and dysfunctions in striatum of prepubertal mice brain. Can J Physiol Pharmacol (Revision submitted)
Singh HK, Dhawan BN (1997) Neuropsychopharmacological effects of the ayurvedic nootropic Bacopa monniera Linn (Brahmi). Indian J Pharmacol 29S:359–365
Tripathi YB, Chaurasia S, Tripathi E, Upadhyay A, Dubey GP (1996) Bacopa monniera Linn. as an antioxidant: mechanism of action. Indian J Exp Biol 34:523–526
Trounce IA, Kim YL, Jun AS, Wallace DC (1996) Assessment of mitochondrial oxidative phosphorylation in patient muscle biopsies, lymphoblasts and transmitochondrial cell lines. Methods Enzymol 264:484–509
Vali S, Mythri RB, Jagatha B, Padiadpu J, Ramanujan KS, Andersen JK, Gorin F, Bharath MMS (2007) Integrating glutathione metabolism and mitochondrial dysfunction with implications for Parkinson’s disease: a dynamic model. Neuroscience 149:917–930
Vollala VR, Upadhya S, Nayak S (2010) Effect of Bacopa monnieri Linn (brahmi) extract on learning and memory in rats: A behavioral study. J Vet Behav Clin Appl Res 5:69–74
Wolff SP (1994) Ferrous ion oxidation in the presence of ferric ion indicator xylenol orange for measurement of hydroperoxides. Methods Enzymol 233:182–189
Acknowledgements
We wish to thank the Director, CFTRI for his keen interest in this study. The first author thanks the Council of Scientific and Industrial research (CSIR), New Delhi for the award of a Junior and Senior Research Fellowship. A part of this study was funded by a fast-track grant from the Department of Science and Technology (DST), India (to MMSB).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shinomol, G.K., Bharath, M.M.S. & Muralidhara Neuromodulatory Propensity of Bacopa monnieri Leaf Extract Against 3-Nitropropionic Acid-Induced Oxidative Stress: In Vitro and In Vivo Evidences. Neurotox Res 22, 102–114 (2012). https://doi.org/10.1007/s12640-011-9303-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-011-9303-6