Abstract
The anti-Parkinson iron chelator-monoamine oxidase inhibitor M30 [5-(N-methyl-N-propargyaminomethyl)-8-hydroxyquinoline] was shown to possess neuroprotective activities in vitro and in vivo, against several insults applicable to several neurodegenerative diseases, such as Alzheimer’s disease, Parkinson’s disease, and ALS. In the present study we sought to examine the effect of M30 on a pre-existing lesion induced by the parkinsonism-inducing toxin, MPTP (N-methyl-4-phenyl-1,2,3,6-tetrahydropyridine). In this neurorescue paradigm, M30 orally administered to mice for 14 days (2.5 mg/kg/day) following MPTP was shown to significantly elevate striatal dopamine levels, reduce its metabolism, and elevate tyrosine-hydroxylase protein levels (from 25.86 ± 5.10 to 68.35 ± 10.67% of control) and activity (from 7.52 ± 0.98 to 16.33 ± 2.92 pmol/mg protein/min). Importantly, M30 elevated MPTP-reduced dopaminergic (from 62.8 ± 4.1 to 84.2 ± 5.9% of control) and transferrin receptor (from 31.3 ± 2.6 to 80.4 ± 7.6% of control) cell count in the SNpc. Finally, M30 was shown to decrease mitosis, thus providing additional protection. These findings suggest that brain-permeable M30 may clearly be of clinical importance for the treatment of PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
To prevent and/or treat Parkinson’s disease (PD), Alzheimer’s disease (AD), and other neurodegenerative diseases, several therapeutic strategies, including iron chelation, antioxidation, and selective monoamine oxidase-B (MAO-B) inhibition, have been proposed. Indeed, several such compounds show neuroprotection in animal models, but most of them fail in the clinic (Gilgun-Sherki et al. 2001; Kaur et al. 2003; Mandel et al. 2003).
6-OHDA and MPTP, the most widely used models of parkinsonism, have many similarities in their mechanisms of action. Both neurotoxins initiate an increase in total iron in the SN and striatum, at the sites of neurodegeneration, in monkeys, rats, and mice (Hall et al. 1992; Oestreicher et al. 1994; Lin et al. 1997; Lin and Lin 1997; Ben-Shachar et al. 2004). Treatment with these neurotoxins results in OS, as a consequence of dysregulation of mitochondrial iron and glutathione, giving rise to the formation of H2O2 through the Fenton reaction and ultimately to the hydroxyl radical, the most reactive of reactive oxygen species (ROS) (Han et al. 1999). MPTP (Ramsay et al. 1987) and 6-OHDA (Glinka and Youdim 1995; Glinka et al. 1996; Glinka et al. 1998) are inhibitors of mitochondrial complex I (Glinka and Youdim 1995), a process which may be prevented by the prototype iron chelator, DFO, which activates this complex by a Ca+2 process (Glinka et al. 1998).
The neuroprotective effect of iron chelation may be attributed to three main mechanisms of action: the first is the prevention of ROS formation, similar to other strong iron chelators, such as DFO, which can bind iron to form stable iron complexes that block the OH• radical production via the Fenton reaction, and therefore protect against OS-induced cell death. The second, direct radical scavenging, as previously described in the text. The third mechanism is inhibition of the iron-dependent hypoxia inducible factor (HIF) prolyl 4-hydroxylases that negatively regulate HIF stability. In this scheme, iron chelators would stabilize HIF-1α and transactivate the expression of established protective genes involved in cell survival, proliferation, and differentiation, including those coding for vascular endothelial growth factor and erythropoietin (Zaman et al. 1999; Siddiq et al. 2005).
The usage of iron chelation therapy for the treatment of PD offers further advantages. Recent studies have shown that overexpression of the PD-associated α-synuclein protein can form toxic aggregates in the presence of iron (Ostrerova-Golts et al. 2000). Similar to ferritin, the mRNA of α-synuclein contains a predicted iron-responsive element in its 5′-untranslated region (5′UTR), and thus it is regulated by iron (Friedlich et al. 2007). Furthermore, DFO was shown to translocate α-synuclein from perinuclear region into the nucleus, thus preventing its aggregation (Sangchot et al. 2002). Furthermore, iron chelation therapy may help in the prevention of glutamate neurotoxicity. Kainate, a glutamate analog, which constitutes a model of hippocampal neurodegeneration, similarly to MPTP, leads to accumulation of ferric and ferrous iron in the hippocampus (Coyle and Puttfarcken 1993). Furthermore, glutamate-induced excitotoxicity is a major contributor to pathological cell death within the nervous system and appears to be mediated by reactive oxygen species.
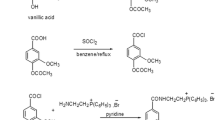
Recently, we have proposed a novel neuroprotective/neurorestorative combination strategy, in neurodegenerative diseases, which may require a drug combining iron chelation with antioxidant capacity and MAO-B inhibitory properties (Mandel et al. 2003). In searching for such neuroprotective/neurorestorative agents, a series of multi-functional iron chelators was synthesized and partially evaluated (Warshawsky et al. 2004; Youdim et al. 2004; Zheng et al. 2005b). The synthesis of the drugs was based on introducing the neuroprotective and MAO inhibitory moiety, N-propargylamine, which is associated with other anti-Parkinson MAO-B inhibitor drugs, rasagiline and selegiline (Youdim 2003; Zheng et al. 2005b), into the 8-hydroxyquinoline-containing pharmacophore of our prototype brain permeable neuroprotective iron chelator, VK28 (Ben-Shachar and Youdim 1990; Zheng et al. 2005b).
Indeed, M30 was shown to confer neuronal protection and neurorestorative action through several mechanisms, including inhibition of caspase 3 cleavage and prevention of Ser139 phosphorylation of apoptosis-associated protein H2A.X. Moreover, the mechanism of neurorescue associated with M30 involved induction of the pro-survival protein, Bcl-2, and reduction of the levels of the pro-apoptotic members, Bad and Bax, as demonstrated in SH-SY5Y cells following serum withdrawal (Avramovich-Tirosh et al. 2007). These effects of M30 on these Bcl-2 family proteins are of great importance, since they imply further protection against MPTP and therefore, possibly against PD. Support for this comes from studies demonstrating that the antiapoptotic Bcl-2 protein over-expression (Offen et al. 1998; Yang et al. 1998) or proapoptotic Bax ablation (Vila et al. 2001) in neuronally derived cell cultures and animal models, employing MPTP, prevented the neurotoxicity and cell death inducing activity of the toxin. Furthermore, activation of Bax relies, in most instances, not only on its transcriptional induction, but also on its posttranslational modification. The latter results in Bax translocation and insertion into the mitochondrial outer membrane, thereby eliciting cytochrome c release and activation of the caspase cascade, which ultimately causes cell death. Both transcriptional and posttranslational activation of Bax have been observed in the SNpc of MPTP-intoxicated mice and PD patients (Perier et al. 2007).
Other propargylamine-containing drugs, such as rasagiline and ladostigil, have been shown to confer neurorescue/neuroprotective activity against cell death induced by a variety of insults [e.g., serum withdrawal and the neurotoxins N-morpholino sydnonimine and N-methyl(R)salsolinol] (Maruyama et al. 2002; Bar-Am et al. 2004; Weinreb et al. 2004; Youdim et al. 2005). The neuroprotection by propargylamine derivatives was previously demonstrated to be attributed to: (i) stabilization of the mitochondrial membrane potential (ΔΨm) and prevention of permeability transition pore (PTP) (Maruyama et al. 2001b); (ii) induction of the anti-apoptotic Bcl-2 protein, regulating mitochondrial membrane permeability transition (Akao et al. 2002); (iii) the increase in brain-derived neurotrophic factor (BDNF) and glial cell line-derived neurotrophic factor (GDNF) (Weinreb et al. 2004; Bar-Am et al. 2005); and (iv) activation of antioxidant enzymes, such as superoxide dismutase and catalase (Carrillo et al. 2000). Furthermore, it was shown that propargylamines induced neuroprotection via regulation of the pro-survival PKC pathway in association with gene regulation of the Bcl-2-related protein family (Weinreb et al. 2004). The above described mechanisms of action are independent of the MAO inhibitory action of these compounds, since the optical s-isomers of rasagiline (TVP1022) and ladostigil (TVP3275) and propargylamine which have more than 1000 fold less MAO inhibitory activity as compared to rasagiline, have similar mechanisms of neuroprotective action and potency (Maruyama et al. 2001a; Youdim et al. 2001; Weinreb et al. 2006; Youdim et al. 2006).
Research efforts have focused until recently on the prevention of PD. Indeed, a recently described theory depicts the predictable sequence of a multi-organ slow progression of developmental stages of PD (Braak et al. 2004), and Berg and colleagues have reported that there are unique ultrasound characteristics which occur both in PD patients and some of their relatives who were shown to develop PD later in life (Berg et al. 2005; Zecca et al. 2005; Berg et al. 2006). These pioneering studies may help diagnose patients earlier than had been possible previously. However, at present, most PD patients are not diagnosed and therefore remain untreated until at least 50–75% of the dopaminergic (DA) neurons have undergone degeneration (Morrish et al. 1998; Sagi et al. 2007). Therefore, it is imperative to find a drug that would reverse the neurodegenerative processes.
Indeed, it has been recently reported of the in vivo neurorestorative effect of propargylamine-containing rasagiline in the MPTP model of parkinsonism, which was shown to occur via induction of the tyrosine-kinase ligands, BDNF and GDNF mRNA level, and activation of the PKC pathway (Sagi et al. 2007).
We have previously shown the neuroprotective effect of M30 in the MPTP mouse model of parkinsonism, simulating preventive disease treatment (Gal et al. 2005). Thus, in the present study, we sought to determine whether M30 also possesses neurorescue/neurorestorative properties following chronic MPTP treatment in mice.
Materials and Methods
Animals and Treatment
All procedures were carried out in accordance with the National Institutes of Health Guide for Care and Use of Laboratory Animals, and were approved by the Animal Ethics Committee of the Technion, Haifa, Israel. Male C57/BL mice (20–22 g, Harlan, Rehovot, Israel) were housed under a 12-h light/dark cycle. Mice were handled daily and allowed at least 4 days to acclimatize before any treatment.
Five groups of mice (n =8–10) were assigned for the neurorescue study. N-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP, 24 mg/kg, i.p, per day) (Sigma-Aldrich, Israel) was administered for 4 days, followed by a further 4 days resting period (day 8) to allow for the full conversion of MPTP to its active metabolite, MPP+ (Levites et al. 2001). The groups of mice killed at day 8 (MPTP day 8), was enrolled for evaluation of spontaneous recovery following the lesion. At day 8, either M30 (0.5 or 2.5 mg/kg/day) or water (MPTP day 22) was administered orally for 14 days, reaching a total treatment period of 22 days. The last three groups consisted of mice receiving M30 only (0.5, 2.5 mg/kg, orally) and water (orally) as controls. All mice were killed by cervical dislocation. Isolated striata of mice were biochemically analyzed for catecholamine content by HPLC and protein expression analysis.
Neurochemical Analysis
Striata were rapidly dissected and tyrosine hydroxylase (TH) activity, dopamine (DA) and its metabolites, homovanilic acid (HVA) and dihydroxyphenyl acetic acid (DOPAC) (Sigma-Aldrich, Israel) levels were analyzed using electrochemical (EC) coupled HPLC, as was previously described (Gal et al. 2005).
Immunohistochemistry
Eight mice per group were deeply anesthetized with Ketamine hydrochloride 100 mg/ml (Font-dodge, Iowa, USA) plus Xylazine 20 mg/ml (VMD, Arendonk, Belgium) and were transcardially perfused with PBS for 2 min followed by 90 ml of 4% (vol/0.1 M PBS vol) paraformaldehyde for 9 min. Brains were post-fixed in 4% (vol/0.1 M PBS vol) paraformaldehyde (48 h, 4°C) and incubated in 70% ethanol followed by subsequent dehydration steps as described (Huang et al. 2005). Paraffin sections were deparaffinized in xylene, hydrated in graduated alcohol solutions and incubated for 30 min in 3% H2O2 in methanol to inactivate endogenous peroxidases. Following antigen retrieval in citrate buffer for 20 min in a microwave, sections were blocked overnight at 4°C with 10% non-immune serum compatible with species type of the second antibody. Sections were reacted overnight at 4°C with specific antibodies against the desired protein. For detection of primary Ab, the HISTOSTAIN-SPTM Kit (Zymed Laboratories Inc. San Francisco, CA, USA) was used. Detection was done by the appropriate biotinylated second antibody with a streptavidin-peroxidase conjugate and S-(2-aminoethyl)-l-cysteine (AEC) as substrate. Counterstaining was done with hematoxylin.
Sections were stained employing primary antibodies of mouse monoclonal anti-tyrosine-hydroxylase (Sigma-Aldrich, Israel), mouse monoclonal anti-transferrin receptor (Zymed, Invitrogen, Carlsbad, CA), and HRP-conjugated mouse monoclonal anti-BrdU (5-bromo-2′-deoxyuridine-5′-monophosphate) (Zymed, Invitrogen, Carlsbad, CA).
Assessment of Neuronal Immunolabeling
Assessment of neuronal loss in the substantia nigra (SN) pars compacta (SNpc) was determined by serial section analysis of the area encompassed between −3.08 and −3.20 from bregma since the reduction of TH-positive neurons in response to MPTP treatment is most prominent at medial levels of the SNc, around the medial terminal nucleus, as shown previously (Hayley et al. 2004). A total of 6–8 mice per treatment group were employed. Analysis was performed as previously described (Sagi et al. 2007).
Protein Determination and Expression Analysis
These were done as previously described (Avramovich-Tirosh et al. 2007).
Statistics
Differences in all biochemical measures were evaluated by one-way ANOVA, followed by a post hoc student t-test, whereas differences in immunochemical staining were processed with the non-parametric Kruskal–Wallis analysis of variance (ANOVA) followed by the Mann–Whitney U-test. Values of P < 0.05 were considered significant.
Results
Neurorescue Effect of M30 from MPTP-Induced Neurotoxicity in Mice: Neurochemical Analysis
In the present study, we sought to determine the “neurorescue” properties of M30 following repetitive sub-chronic MPTP regimen (Sagi et al. 2003). For this purpose, MPTP (24 mg/kg, i.p, per day) was administered to mice in the neurorescue paradigm, as described in the “Materials and Methods” section. In the present study, M30 was administered at either M30 (0.5 or 2.5 mg/kg/day). The dose of 0.5 mg/kg was chosen based on a previous study in which rasagiline administered at 0.05 mg/kg/day p.o. for 10 days was shown to induce neurorestoration (Sagi et al. 2007), and we have shown that the IC50 value of rasagiline for MAO-B inhibition is an order of magnitude lower than M30. For the evaluation of any spontaneous recovery following MPTP, an additional mice group, killed at day 8, was included (MPTP day 8).
In the neurorescue paradigm, M30 (2.5 mg/kg/day, p.o.) given subsequently to MPTP, induced a significant elevation of striatal DA levels, compared to MPTP (day 22) (Fig. 1), and fully restored the increased DA turnover induced by MPTP (Fig. 2), while a dose of 0.5 mg/kg/day, p.o. had weaker effects. Similar to other propargylamine-containing drugs, such as ladostigil (Weinstock et al. 2003), M30 increased 5-HT (Table 1), an effect which was more prominent following MPTP treatment.
The neurorescue effect of M30 on striatal DA, DOPAC, and HVA in MPTP-treated mice. Mice were administered MPTP or saline i.p. once daily for 4 consecutive days. The mice were then orally treated with M30 0.5 mg/kg (a) or 2.5 mg/kg (b) once daily for 14 consecutive days. Striatal DA, DOPAC, and HVA were determined via EC-HPLC analysis. Results represent mean ± SEM (n = 6–8, # P < 0.05 vs. control, * P < 0.05 vs. MPTP day 22)
Neurorescue effect of M30 on DA turnover. Striatal DA turnover in control and MPTP treated mice was determined based on Fig. 1a, b. DA metabolism was expressed as the ratio (DOPAC + HVA)/DA. Results represent mean ± SEM (n = 6–8, # P < 0.05 vs. control, * P < 0.05 vs. MPTP day 22)
Functional analysis revealed that these effects correlated with striatal TH activity levels: M30 (2.5 mg/kg) fully rescued striatal TH activity, compared to MPTP (day 22) (Fig. 3). The expression of TH, as assessed by western blot is in line with the previous findings: M30 (2.5 mg/kg) induced a rescue effect, elevating TH levels from 25.86 ± 5.10 to 68.35 ± 10.67% of control (Fig. 4), while 60.41 ± 6.69% rescue were achieved with a dose of 0.5 mg/kg. The effect of M30 appears to be more effective in the SNpc than in the striatum, probably because MPTP affects initially and more intensely the dopaminergic terminals in the striatum rather than the neuron bodies in the SNpc.
Neurorescue effect of M30 on striatal tyrosine hydroxylase expression levels in MPTP-treated mice. Striatal tyrosine hydroxylase protein expression levels were evaluated in mouse striatum lysates by western blot analysis. Values were normalized with respect to β-actin and expressed as a percentage of control. Results represent mean (% of control) ± SEM (n = 6–8, # P < 0.05 vs. control, * P < 0.05 vs. MPTP day 22)
Immunohistochemistry Analysis of M30 Neurorescue Activity Against MPTP-Induced DA Cell Loss in Mice SNpc
Effect of M30 on TH Cell Count
In order to find out the reason for the increase in DA, TH activity levels, and TH expression levels, two hypotheses can be raised: the first is that these neurorestorative effects result from elevation in dopaminergic cell number, and the second, that there is a compensatory activity of the remaining DA neurons following MPTP toxicity. In order to address this issue, the neurorescue experiment was repeated, and M30 was administered at doses of 1 or 2.5 mg/kg/day, p.o., since a dose of 0.5 mg/kg was shown ineffective in the previous section.
Figure 5 shows the number of TH immunoreactive cells in the SNpc, as assessed by counting adjacent sections stained for TH antibody. The sections were taken from the area encompassed between −3.08 and −3.20 from bregma since the reduction of TH-positive neurons in response to MPTP treatment is most prominent at medial levels of the SNc, around the medial terminal nucleus, as shown previously (Hayley et al. 2004).
The neurorescue effect of M30 on TH cell count in the SNpc in MPTP-treated mice. Mice were treated with MPTP (24 mg/kg/day for 4 days followed by additional 4 days resting period. One mice group was either killed (MPTP day 8) or orally administered with M30 (2.5 mg/kg/day) or water (MPTP day 22) for 14 days. Control mice received water. Assessment of TH-positive cells in the SNpc was determined by serial section analysis of the area encompassed between −3.08 and −3.20 from bregma. Representative micrographs taken with ×4 objective (top), or with ×20 objective (bottom) (n = 6, # P < 0.05 vs. control, * P < 0.05 vs. MPTP day 22)
MPTP at day 8 caused a significant reduction (62.8 ± 4.1% of control) in TH-positive cells, whereas no spontaneous recovery was observed at MPTP day 22. Oral M30 administration at a dose of 0.5 or 2.5 mg/kg/day given for a period of 14 days after MPTP resulted in a marked recovery of TH-immunopositive cells (84.2 ± 5.9% of control) vs. MPTP (day 22) (Fig. 5), whereas a dose of 1 mg/kg M30 led to less recovery (74.6 ± 6.8% of control) (data not shown).
Effect of M30 on TfR Cell Count
We have shown that M30 exerts beneficial effects in the neurorescue paradigm in the MPTP mouse model, affecting dopaminergic cell count, DA levels, DA metabolism, and TH activity and expression levels. We next sought to determine whether this drug modulates iron levels, given the fact that M30 is an iron chelator (Zheng et al. 2005a; Zheng et al. 2005b). To test this hypothesis, consecutive sections of SNpc from mice of the neurorescue experiment were stained for transferrin receptor (TfR). Owing to the iron responsive elements found in the 3′UTR of its mRNA, TfR is an iron responsive protein, which has a pivotal role in maintaining cellular iron homeostasis, by internalization of iron into the cell when iron levels are low. Therefore, its expression is affected by cellular iron levels: when iron levels are limited, expression of TfR is elevated, owing to the fact that IRPs, proteins serving as cellular iron detectors, bind to the iron responsive elements found in the 3′UTR of the mRNA of TfR, thus stabilizing it and allowing for increased translation of the mRNA transcript (Zecca et al. 2004). Thus, measurement of TfR levels is indicative of iron chelation.
The effect of MPTP is known to be mediated by iron and OS resulting from increased iron levels (Ben Shachar et al. 2003; Gal et al. 2006). Therefore, following MPTP administration, iron levels would be expected to increase, and therefore, TfR levels would be expected to decrease in response. Indeed, Fig. 6 demonstrates that TfR-positive cell count was reduced to 29.8 ± 7.2% of control, evident in the SNpc of MPTP-treated mice on day 8. No spontaneous recovery of TfR cell count was found (31.3 ± 2.6% of control), in consistency with the TH cell count. However, both doses of M30 led to a significant increase in TfR cell count (47.8 ± 3.3 and 80.4 ± 7.6% of control for 1 and 2.5 mg/kg, respectively), compared to MPTP-treated mice, indicating that this drug maintains its iron chelation properties in vivo.
The neurorescue effect of M30 on TfR cell count in MPTP-treated mice Similar to Fig. 5, TfR-positive cells were counted in coronal sections from the SNpc bregma. Representative micrographs taken with ×4 objective (top), or with ×20 objective (bottom) (n = 6, # P < 0.05 vs. control, * P < 0.05 vs. MPTP day 22)
Effect of M30 on Cell Division
The intriguing increase in TH cell count induced by M30 when given chronically subsequently to MPTP raised the question of the origin of these cells. Three hypotheses can be suggested: the first is that MPTP puts many cells on the brink of death, yet M30 prevents them from crossing the threshold to commence apoptosis or necrosis cascades; the second hypostudy is that M30 induces neurogenesis via mitosis in the SNpc; the third hypostudy is that M30 induces neurogenesis via mitosis elsewhere, and the newly formed neurons migrate to the SNpc.
Neurogenesis in the adult brain is known to occur in four brain regions: olfactory bulbs, the forebrain sub-ventricular zone (SVZ) near the striatum, the hippocampal subgranular zone (SGZ), and the hippocampus, in response to various insults including MPTP and 6-OHDA), both spontaneously and growth factor-induced (Faiz et al. 2005; Yoshimi et al. 2005; Keilhoff et al. 2006; Van Kampen and Eckman 2006; Lagace et al. 2007; Tonchev et al. 2007). In order to test whether mitosis is involved, thymidine analog, 5-bromo-2′-deoxyuridine-5′-monophosphate (BrdU), was administered i.p. to the neurorescue experiment mice once daily for four consecutive days (50 mg/kg), starting on day 9 of the experiment, and sections from the SNpc, hippocampus, and sub-ventricular zone were stained for BrdU. Figure 7 shows that many BrdU-positive nuclei were found in the hippocampus of BrdU-MPTP-treated mice, compared to control, and to a lesser extent, in BrdU-MPTP-M30 (1, 2.5 mg/kg)-treated mice. Control mice displayed almost no BrdU staining, and mice untreated with BrdU displayed no BrdU staining at all. In sections from the SNpc and the sub-ventricular zone no prominent BrdU staining of nuclei was noted.
The neurorescue effect of M30 on BrdU nuclei count in MPTP-treated mice. Mice were treated as described in Fig. 20, and BrdU-positive nuclei were counted in coronal sections of hippocampus region adjacent to the SNpc. Representative micrographs taken with ×20 objective, micrograph on bottom-right taken with ×4 objective (n = 6, # P < 0.05 vs. control, * P < 0.05 vs. MPTP day 22)
Discussion
The results of the present study point to a neurorescue/neurorestorative activity for M30 in the MPTP mouse model of PD. A continuous 14-day administration of M30 following MPTP-induced lesion, managed to restore the severe reduction in dopaminergic cell count, striatal DA content and metabolism, and TH activity and expression levels, while water-treated mice did not show any spontaneous recovery.
The neurorestorative properties of M30 are in accordance with the recently reported neurorestorative action of the propargylamine-containing rasagiline, manifested following MPTP (N-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) lesion (Sagi et al. 2007), restoring the severe reduction in dopaminergic cell count, striatal DA content and turnover, and TH activity and protein expression. The neurorestorative property of rasagiline was shown to be mediated by tyrosine-kinase (Trk)-pathway ligands, including GDNF, BDNF, and NGF, in addition to activation of the Ras-PI3K-Akt pathway-related proteins (Sagi et al. 2007). Similar changes have also been documented on the gene level (Semkova et al. 1996; Tatton et al. 2002; Maruyama et al. 2004; Weinreb et al. 2004). These genes/proteins are known to promote cell survival via induction of neuronal growth and differentiation and prevention of apoptosis, properties which are attributed to the propargylamine moiety, shared by our proprietary drug, M30 (Avramovich-Tirosh et al. 2007). Similar to rasagiline, M30 appears to be more effective in the SN than in the striatum, probably because MPTP affects initially and more intensely the dopaminergic terminals in the striatum rather than the neuron bodies in the compacta (Sagi et al. 2007).
We have shown in the present study that M30 is a potent iron chelator, not only in vitro and ex vivo, as previously shown (Zheng et al. 2005a; Zheng et al. 2005b), but in vivo as well, elevating MPTP-reduced cell count of TfR-expressing neurons. We have previously shown that M30 exerts its propargylamine-ascribed MAO-inhibitory activity in the brain, indicating brain permeability. The finding that M30 affects SNpc TfR-positive cell count, implies that the 8-hydroxyquinoline-ascribed iron chelation moiety of M30 is also brain permeable and that it maintains its iron chelation property in vivo. Whether this iron chelation moiety enters the brain as part of M30 or as an individual metabolite, remains to be determined. We have also shown a dose-dependent effect of iron chelation, demonstrated by higher TfR cell count in mice receiving M30, 2.5 mg/kg/day, as compared to 1 mg/kg/day. While one can maintain that lower cell count may also stem from fewer cells, it is important to note that in MPTP-treated mice TfR-positive cells tend to display somewhat lighter staining, as well as smaller perinuclear stained area per cell. Since MPTP + M30-treated mice display staining properties resembling control cells in both aspects, indicating iron chelation by M30. Indeed 6-hydroxydopamine, MPTP, and ubiquitin-proteasome inhibitor, lactacystin, models of parkinsonism have been shown to increase iron in substantia nigra pars compacta of rats, monkeys, and mice, respectively (Hall et al. 1992; Mochizuki et al. 1994; Oestreicher et al. 1994; Temlett et al. 1994; Goto et al. 1996; Lan and Jiang 1997a; Lan and Jiang 1997b; Zhu et al. 2007), and iron chelator VK-28 and M30 have been shown to prevent the accumulation of iron in the 6-hydroxydamine and lactacystin model of parkinsonism (Youdim et al. 2004; Zhu et al. 2007). Further support for iron chelation by M30 in MPTP model has come from studies with the copper chelator d-penicillamine, which does not attenuate MPTP dopaminergic neurotoxicity in mice (Youdim et al. 2007).
The neuroprotective and more importantly, the neurorestorative effect of M30 in the MPTP model of parkinsonism are consistent with the effects of the drug in the lactacystin model of parkinsonism. Indeed, a growing body of evidence suggests that failure of the proteasomal function might play an important role in the pathogenic process of sporadic and familial PD and may underlie protein accumulation, Lewy body formation, and neurodegeneration in the SN (Grunblatt et al. 2004; McNaught and Olanow 2006). It has been shown that striatal microinfusions of the proteasome inhibitor lactacystin or epoxomycin can reproduce selective retrograde nigral damage in the ipsilateral SN (Fornai et al. 2003). It has been recently demonstrated that our proprietary iron-chelator drugs, M30 and VK28, produced a neurorestorative activity in the lactacystin-induced proteasomal dysfunction model of parkinsonism (Zhu et al. 2007), when given after lactacystin lesion. Administration of VK28 or M30 (5 mg/kg/day, i.p. for 21 days) after microinjection of lactacystin, both drugs managed to significantly improve behavioral performances; restore the severe reduction in DA neuron number and striatal DA level; and also attenuated proteasomal inhibition, iron accumulation, and microglial activation in the ipsilateral SN. Furthermore, M30 was capable of reversing the reduction of the anti-apoptotic Bcl-2 protein level caused by lactacystin. Although VK28 was more potent than M30 in chelating brain iron, it was not as good as M30 either in attenuating nigral neurodegeneration induced by lactacystin or in reducing proteasomal inhibition after lactacystin microinjection.
The neurorestorative potential of rasagiline and selegiline has also been studied in the lactacystin model (Zhu et al. 2008). Of these two MAO-B inhibitors, only rasagiline managed to restore the nigrostriatal degeneration. However, the results attained employing M30 and VK28 in the neurorescue paradigm were superior to those attained with rasagiline, with respect to behavioral parameters, TH-positive cell count in the SNpc, concentration of striatal DA and its metabolites, DOPAC and HVA, and restoration of proteasomal activity. Furthermore, of the two iron chelators, M30 was superior to VK28 with respect to all the aforementioned parameters, in spite of being less potent as an iron chelator, further emphasizing the role of the propargylamine moiety, absent from VK28.
In the present study we tried to elucidate the origin of the additional neurons found in the SNpc following treatment with M30. Neurogenesis in the adult brain is known to occur in three brain regions: olfactory bulbs, the forebrain rostral sub-ventricular zone (SVZ) near the striatum, the hippocampal sub-granular zone (SGZ) of the dentate gyrus (DG). The neurogenesis in these brain regions occurs following various insults (including 6-OHDA and MPTP), both spontaneously and in response to growth factors (Faiz et al. 2005; Yoshimi et al. 2005; Keilhoff et al. 2006; Van Kampen and Eckman 2006; Lagace et al. 2007; Tonchev et al. 2007), although neurogenesis in the SN is controversial (Peng et al. 2008).
Recent reports have shown neurogenesis in the SN and migration of cells into the SN, wherein they differentiate into neurons. The presence of a slow physiological turnover of neurons in the adult mouse SN, which points to a functional role for neural stem cells in the midbrain has been shown by Kay and Blum (2000), Zhao et al. (2003), and Yoshimi et al. (2005) in response to a partial nigral MPTP-induced lesion, which resulted in increased neuronal replacement, indicating that the rate of neurogenesis can be regulated. In a recent study, MPTP lesions increased the incorporation of BrdU, as well as the number of cells that co-expressed BrdU and the immature neuronal marker doublecortin (DCX), in the SGZ of the DG and the SVZ. BrdU-labeled, DCX-expressing cells were not found in the substantia nigra (SN) of MPTP-treated mice, where neuronal cell bodies are destroyed, but were present in increased numbers in the striatum, where SN neurons lost in PD normally project. Fibroblast growth factor-2 (FGF-2), which enhances neurogenesis in a mouse model of HD, also increased the number of BrdU/DCX-immunopositive cells in the SN of MPTP-treated mice (Peng et al. 2008).
Interestingly, although cell proliferation in control and MPTP-treated rats was shown to occur in the SN, most of these cells differentiated into microglia, indicative of inflammatory processes, and none into TH-expressing neurons (Yoshimi et al. 2005). In addition, following MPTP-induced unilateral lesion in the rat, polysialic acid (PSA)-positive cells (a marker for young neurons) were found in the SGZ of the DG in the hippocampus. PSA-positive cells were also found in the SN in the DA depleted hemisphere of MPTP unilaterally lesioned rats and in PD patients (Yoshimi et al. 2005). Recently we have shown that the neurorestorative activity of M30 has been linked to its ability to cause inhibition of prolyl-4-hydroxylase, resulting in activation of HIF and its related gene vascular endothelial growth factor (VGEF), enolase, erythropoietin and BDNF with the resultant cell arrest and differentiation (Kupershmidt et al. 2009).
In line with this, our findings show that MPTP induced cell division in the sub-granular zone (SGZ) (particularly in the granular layer) of the dentate gyrus (DG) in the hippocampus, as demonstrated by BrdU staining. However, M30 led to decreased cell division in this brain region, as shown by BrdU-marked cell nuclei, whereas very few cells were marked in control sections. This is consistent with a previous study, in which it was found that M30 has the ability to induce neuronal differentiation and negatively regulate cell cycle progression in SH-SY5Y cells (Avramovich-Tirosh et al. 2007). Similar effects were also found for HLA20 (Zheng et al. 2005a) and for the iron chelator prototype derivative VK28. All three drugs were shown to induce the characteristics of neuronal differentiation, including cell body elongation, stimulation of neurite outgrowth, arrest of the cell cycle in G0/G1, and specific upregulation of the expression of the neuronal marker growth-associated protein 43 (GAP-43) (Avramovich-Tirosh et al. 2007). Indeed, in this study, the BrdU-stained nuclei of MPTP/M30-treated mice appear more elongated, as compared to MPTP-treated mice, suggesting neuronal differentiation. However, no BrdU-positive nuclei were found in the SN or sub-ventricular zone. This may be ascribed to methodology, since BrdU has been shown to be toxic for dividing cells (Kolb et al. 1999; Zhao et al. 2003; Peng et al. 2008), yet repetitive doses of relatively high concentration are required to achieve extensive labeling as reported by Zhao et al. (2003).
All of the above may explain our findings in the present study, of increased TH-positive cell count, found in the SNpc of MPTP/M30-treated mice, as compared to MPTP-treated mice, on the one hand, and decreased cell divisions in the SGZ of the DG, on the other hand. This supposed dichotomy may be resolved by the following hypothesis: M30 induces neuronal differentiation, whereas MPTP-induced cell proliferation leads to microglial differentiation, further contributing to the inflammatory process, and in turn, to cell death. This avenue must be further pursued, in order to elucidate the mechanisms underlying these processes. The reduced number of BrdU-positive cell nuclei in MPTP/M30-treated mice compared to MPTP-treated mice is also in contrast with the enhanced cell count induced by FGF-2 following MPTP treatment (Peng et al. 2008). A possible explanation for this may be found in the different pathways M30 and FGF-2 activate: neurotrophins and basic fibroblast growth factor are ligands of tyrosine kinase receptors, though they bind to different tyrosine kinase receptor classes. Neurotrophins bind to receptor tyrosine kinase class VII, Trk receptor family, while basic fibroblast growth factor binds to receptor tyrosine kinase class IV, FGF receptor family (Munoz et al. 2009). As mentioned previously, M30 is thought to activate Trk-pathway ligands, including GDNF, BDNF, and NGF, in addition to activation of the Ras-PI3K-Akt pathway-related proteins activated by propargylamine-containing rasagiline (Sagi et al. 2007). In addition, the reduced BrdU-positive cell count of MPTP/M30-treated mice compared to MPTP-treated mice may also be explained by cell migration. It is possible that M30 induces or contributes to signal-cascades ultimately leading to cell migration from neurogenesis zones to the SN where they are required; therefore, although more cells may have been formed in MPTP/M30-treated mice, less BrdU-positive cells are found in the SGZ. Previous studies have stressed the importance of methodology issues (Kolb et al. 1999; Zhao et al. 2003; Peng et al. 2008), and it is highly likely that the dose and time frame during which BrdU was injected were insufficient.
The property of cell cycle arrest, induced by M30, is shared by other iron chelators HLA20 and VK28. In fact, a novel therapeutic strategy for neurodegenerative disease, similar to cancer drug therapy, is currently directed at interfering with mitogenic signaling and cell cycle progression to ameliorate cell death (for a comprehensive review see Amit et al. (2007), Avramovich-Tirosh et al. (2007)). This strategy relies on accumulating evidence, suggesting that neuronal death in the central nervous system (CNS) is often intimately linked to cellular processes that normally occur only during a mitotic cell cycle (Amit et al. 2007; Avramovich-Tirosh et al. 2007; Herrup and Yang 2007).
In conclusion, the iron chelation properties, together with its brain selective MAO-A/B inhibitory and the propargylamine-dependent neuroprotective and neurorestorative properties, may make M30 an ideal drug for the treatment of PD and other neurodegenerative diseases, where OS and iron dysregulation have been implicated in their pathogenesis (Zecca et al. 2004). M30 may prove to be a safe and effective means of reducing the PD-induced iron load in neural tissue, thus staving off the harmful effects of oxidative damage and its sequelae. Furthermore, future studies employing this drug may help deepen our understanding of the pathogenesis of PD and pave the way for other therapeutic agents in the management of various neurodegenerative diseases.
References
Akao Y, Maruyama W, Shimizu S, Yi H, Nakagawa Y, Shamoto-Nagai M, Youdim MB, Tsujimoto Y, Naoi M (2002) Mitochondrial permeability transition mediates apoptosis induced by N-methyl(R)salsolinol, an endogenous neurotoxin, and is inhibited by Bcl-2 and rasagiline, N-propargyl-1(R)-aminoindan. J Neurochem 82:913–923
Amit T, Avramovich-Tirosh Y, Youdim MB, Mandel S (2007) Targeting multiple Alzheimer’s disease etiologies with multimodal neuroprotective and neurorestorative iron chelators. Faseb J
Avramovich-Tirosh Y, Amit T, Bar-Am O, Zheng H, Fridkin M, Youdim MB (2007) Therapeutic targets and potential of the novel brain- permeable multifunctional iron chelator-monoamine oxidase inhibitor drug, M-30, for the treatment of Alzheimer’s disease. J Neurochem 100:490–502
Bar-Am O, Yogev-Falach M, Amit T, Sagi Y, Youdim MBH (2004) Regulation of protein kinase C by the anti-Parkinson drug, MAO-B inhibitor, rasagiline and its derivatives, in vivo. J Neurochem 89:1119–1125
Bar-Am O, Weinreb O, Amit T, Youdim MB (2005) Regulation of Bcl-2 family proteins, neurotrophic factors, and APP processing in the neurorescue activity of propargylamine. Faseb J 19:1899–1901
Ben-Shachar D, Youdim MBH (1990) Selectivity of melaninized nigra-striatal dopamine neurons to degeneration in Parkinson’s disease may depend on iron-melanin interaction. J Neural Transm Suppl 29:251–258
Ben-Shachar D, Kahana N, Kampel V, Warshawsky A, Youdim MBH (2003) Neuroprotection by a novel brain permeable iron chelator, VK-28, against 6-hydroxydopamine lession in rats. Neuropharmacology
Ben-Shachar D, Kahana N, Kampel V, Warshawsky A, Youdim MB (2004) Neuroprotection by a novel brain permeable iron chelator, VK-28, against 6-hydroxydopamine lession in rats. Neuropharmacology 46:254–263
Berg D, Merz B, Reiners K, Naumann M, Becker G (2005) Five-year follow-up study of hyperechogenicity of the substantia nigra in Parkinson’s disease. Mov Disord 20:383–385
Berg D, Hochstrasser H, Schweitzer KJ, Riess O (2006) Disturbance of iron metabolism in Parkinson’s disease—ultrasonography as a biomarker. Neurotox Res 9:1–13
Braak H, Ghebremedhin E, Rub U, Bratzke H, Del Tredici K (2004) Stages in the development of Parkinson’s disease-related pathology. Cell Tissue Res 318:121–134
Carrillo MC, Minami C, Kitani K, Maruyama W, Ohashi K, Yamamoto T, Naoi M, Kanai S, Youdim MBH (2000) Enhancing effect of rasagiline on superoxide dismutase and catalase activities in the dopaminergic system in the rat. Life Sci 67:577–585
Coyle JT, Puttfarcken P (1993) Oxidative stress, glutamate, and neurodegenerative disorders. Science 262:689–695
Faiz M, Acarin L, Castellano B, Gonzalez B (2005) Proliferation dynamics of germinative zone cells in the intact and excitotoxically lesioned postnatal rat brain. BMC Neurosci 6:26
Fornai F, Lenzi P, Gesi M, Ferrucci M, Lazzeri G, Busceti CL, Ruffoli R, Soldani P, Ruggieri S, Alessandri MG, Paparelli A (2003) Fine structure and biochemical mechanisms underlying nigrostriatal inclusions and cell death after proteasome inhibition. J Neurosci 23:8955–8966
Friedlich AL, Tanzi RE, Rogers JT (2007) The 5′-untranslated region of Parkinson’s disease alpha-synuclein messengerRNA contains a predicted iron responsive element. Mol Psychiatry 12:222–223
Gal S, Zheng H, Fridkin M, Youdim MB (2005) Novel multifunctional neuroprotective iron chelator-monoamine oxidase inhibitor drugs for neurodegenerative diseases. In vivo selective brain monoamine oxidase inhibition and prevention of MPTP-induced striatal dopamine depletion. J Neurochem 95:79–88
Gal S, Fridkin M, Amit T, Zheng H, Youdim MB (2006) M30, a novel multifunctional neuroprotective drug with potent iron chelating and brain selective monoamine oxidase-ab inhibitory activity for Parkinson’s disease. J Neural Transm Suppl 70:447–456
Gilgun-Sherki Y, Melamed E, Offen D (2001) Oxidative stress induced-neurodegenerative diseases: the need for antioxidants that penetrate the blood brain barrier. Neuropharmacology 40:959–975
Glinka YY, Youdim MB (1995) Inhibition of mitochondrial complexes I and IV by 6-hydroxydopamine. Eur J Pharmacol 292:329–332
Glinka Y, Tipton KF, Youdim MB (1996) Nature of inhibition of mitochondrial respiratory complex I by 6-hydroxydopamine. J Neurochem 66:2004–2010
Glinka Y, Tipton KF, Youdim MBH (1998) Mechanism of inhibition of mitochondrial respiratory complex I by 6-hydroxydopamine and its prevention by desferrioxamine. Eur J Pharmacol 351:121–129
Goto K, Mochizuki H, Imai H, Akiyama H, Mizuno Y (1996) An immuno-histochemical study of ferritin in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced hemiparkinsonian monkeys. Brain Res 724:125–128
Grunblatt E, Mandel S, Jacob-Hirsch J, Zeligson S, Amariglo N, Rechavi G, Li J, Ravid R, Roggendorf W, Riederer P, Youdim MB (2004) Gene expression profiling of parkinsonian substantia nigra pars compacta; alterations in ubiquitin-proteasome, heat shock protein, iron and oxidative stress regulated proteins, cell adhesion/cellular matrix and vesicle trafficking genes. J Neural Transm 111:1543–1573
Hall S, Rutledge JN, Schallert T (1992) MRI, brain iron and experimental Parkinson’s disease. J Neurol Sci 113:198–208
Han J, Cheng FC, Yang Z, Dryhurst G (1999) Inhibitors of mitochondrial respiration, iron (II), and hydroxyl radical evoke release and extracellular hydrolysis of glutathione in rat striatum and substantia nigra: potential implications to Parkinson’s disease. J Neurochem 73:1683–1695
Hayley S, Crocker SJ, Smith PD, Shree T, Jackson-Lewis V, Przedborski S, Mount M, Slack R, Anisman H, Park DS (2004) Regulation of dopaminergic loss by Fas in a 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine model of Parkinson’s disease. J Neurosci 24:2045–2053
Herrup K, Yang Y (2007) Cell cycle regulation in the postmitotic neuron: oxymoron or new biology? Nat Rev Neurosci 8:368–378
Huang Y, Wernyj RP, Norton DD, Precht P, Seminario MC, Wange RL (2005) Modulation of specific protein expression levels by PTEN: identification of AKAP121, DHFR, G3BP, Rap1, and RCC1 as potential targets of PTEN. Oncogene 24:3819–3829
Kaur D, Yantiri F, Rajagopalan S, Kumar J, Mo JQ, Boonplueang R, Viswanath V, Jacobs R, Yang L, Beal MF, DiMonte D, Volitaskis I, Ellerby L, Cherny RA, Bush AI, Andersen JK (2003) Genetic or pharmacological iron chelation prevents MPTP-induced neurotoxicity in vivo: a novel therapy for Parkinson’s disease. Neuron 37:899–909
Kay JN, Blum M (2000) Differential response of ventral midbrain and striatal progenitor cells to lesions of the nigrostriatal dopaminergic projection. Dev Neurosci 22:56–67
Keilhoff G, Becker A, Grecksch G, Bernstein HG, Wolf G (2006) Cell proliferation is influenced by bulbectomy and normalized by imipramine treatment in a region-specific manner. Neuropsychopharmacology 31:1165–1176
Kolb B, Pedersen B, Ballermann M, Gibb R, Whishaw IQ (1999) Embryonic and postnatal injections of bromodeoxyuridine produce age-dependent morphological and behavioral abnormalities. J Neurosci 19:2337–2346
Kupershmidt L, Weinreb O, Mandel S, Amit T, Youdim MBH (2009) Involvement of HIF and VGEF in neuroprotective and neuritogenic activities of novel multimodal iron chelating drugs in motor neuron-like NSC-34 cells and transgenic mouse model of amyotrophic lateral sclerosis. FASEB J (in press)
Lagace DC, Whitman MC, Noonan MA, Ables JL, DeCarolis NA, Arguello AA, Donovan MH, Fischer SJ, Farnbauch LA, Beech RD, DiLeone RJ, Greer CA, Mandyam CD, Eisch AJ (2007) Dynamic contribution of nestin-expressing stem cells to adult neurogenesis. J Neurosci 27:12623–12629
Lan J, Jiang DH (1997a) Desferrioxamine and vitamin E protect against iron and MPTP-induced neurodegeneration in mice. J Neural Transm 104:469–481
Lan J, Jiang DH (1997b) Excessive iron accumulation in the brain: a possible potential risk of neurodegeneration in Parkinson’s disease. J Neural Transm 104:649–660
Levites Y, Weinreb O, Maor G, Youdim MBH, Mandel S (2001) Green tea polyphenol (-)-Epigallocatechin-3-gallate prevents N-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced dopaminergic neurodegeneration. J Neurochem 78:1073–1082
Lin YL, Lin JK (1997) (-)-Epigallocatechin-3-gallate blocks the induction of nitric oxide synthase by down-regulating lipopolysaccharide-induced activity of transcription factor nuclear factor-kappaB. Mol Pharmacol 52:465–472
Lin M, Rippe RA, Niemela O, Brittenham G, Tsukamoto H (1997) Role of iron in NF-kappa B activation and cytokine gene expression by rat hepatic macrophages. Am J Physiol 272:G1355–G1364
Mandel S, Grunblatt E, Riederer P, Gerlach M, Levites Y, Youdim MB (2003) Neuroprotective strategies in Parkinson’s disease: an update on progress. CNS Drugs 17:729–762
Maruyama W, Youdim MBH, Naoi M (2001a) Antiapoptotic properties of rasagiline, N-propargylamine-1(R)-aminoindan, and its optical (S)-isomer, TV1022. Ann N Y Acad Sci 939:320–329
Maruyama W, Akao Y, Youdim MBH, Boulton AA, Davis BA, Naoi M (2001b) Transfection-enforced Bcl-2 overexpression and an anti-Parkinson drug, rasagiline, prevent nuclear accumulation of glyceraldehyde-3 phosphate dehydrogenase induced by an endogenous dopaminergic neurotoxin, N-methyl(R)salsolinol. J Neurochem 78:727–735
Maruyama W, Takahashi T, Youdim MBH, Naoi M (2002) The anti-Parkinson drug, rasagiline, prevents apoptotic DNA damage induced by peroxynitrite in human dopaminergic neuroblastoma SH-SY5Y cells. J Neural Transm 109:467–481
Maruyama W, Nitta A, Shamoto-Nagai M, Hirata Y, Akao Y, Youdim MBH, Furukawa S, Nabeshima T, Naoi M (2004) N-Propargyl-1 (R)-aminoindan, rasagiline, increases glial cell line-derived neurotrophic factor (GDNF) in neuroblastoma SH-SY5Y cells through activation of NF-kappaB transcription factor. Neurochem Int 44:393–400
McNaught KS, Olanow CW (2006) Protein aggregation in the pathogenesis of familial and sporadic Parkinson’s disease. Neurobiol Aging 27:530–545
Mochizuki H, Imai H, Endo K, Yokomizo K, Murata Y, Hattori N, Mizuno Y (1994) Iron accumulation in the substantia nigra of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced hemiparkinsonian monkeys. Neurosci Lett 168:251–253
Morrish PK, Rakshi JS, Bailey DL, Sawle GV, Brooks DJ (1998) Measuring the rate of progression and estimating the preclinical period of Parkinson’s disease with [18F]dopa PET. J Neurol Neurosurg Psychiatry 64:314–319
Munoz M, Rodriguez A, Diez C, Caamano JN, Fernandez-Sanchez MT, Perez-Gomez A, De Frutos C, Facal N, Gomez E (2009) Tyrosine kinase A, C and fibroblast growth factor-2 receptors in bovine embryos cultured in vitro. Theriogenology 71(6):1005–1010
Oestreicher E, Sengstock GJ, Riederer P, Olanow CW, Dunn AJ, Arendash GW (1994) Degeneration of nigrostriatal dopaminergic neurons increases iron within the substantia nigra: a histochemical and neurochemical study. Brain Res. 660:8–18
Offen D, Beart PM, Cheung NS, Pascoe CJ, Hochman A, Gorodin S, Melamed E, Bernard R, Bernard O (1998) Transgenic mice expressing human Bcl-2 in their neurons are resistant to 6-hydroxydopamine and 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine neurotoxicity. Proc Natl Acad Sci USA 95:5789–5794
Ostrerova-Golts N, Petrucelli L, Hardy J, Lee JM, Farer M, Wolozin B (2000) The A53T alpha-synuclein mutation increases iron-dependent aggregation and toxicity. J Neurosci 20:6048–6054
Peng J, Xie L, Jin K, Greenberg DA, Andersen JK (2008) Fibroblast growth factor 2 enhances striatal and nigral neurogenesis in the acute 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine model of Parkinson’s disease. Neuroscience 153:664–670
Perier C, Bove J, Wu DC, Dehay B, Choi DK, Jackson-Lewis V, Rathke-Hartlieb S, Bouillet P, Strasser A, Schulz JB, Przedborski S, Vila M (2007) Two molecular pathways initiate mitochondria-dependent dopaminergic neurodegeneration in experimental Parkinson’s disease. Proc Natl Acad Sci USA 104:8161–8166
Ramsay RR, Kowal AT, Johnson MK, Salach JI, Singer TP (1987) The inhibition site of MPP+, the neurotoxic bioactivation product of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine is near the Q-binding site of NADH dehydrogenase. Arch Biochem Biophys 259:645–649
Sagi Y, Weinstock M, Youdim MBH (2003) Attenuation of MPTP-induced dopaminergic neurotoxicity by TV3326, a cholinesterase-monoamine oxidase inhibitor. J Neurochem 2:290–297
Sagi Y, Mandel S, Amit T, Youdim MB (2007) Activation of tyrosine kinase receptor signaling pathway by rasagiline facilitates neurorescue and restoration of nigrostriatal dopamine neurons in post-MPTP-induced parkinsonism. Neurobiol Dis 25:35–44
Sangchot P, Sharma S, Chetsawang B, Porter J, Govitrapong P, Ebadi M (2002) Deferoxamine attenuates iron-induced oxidative stress and prevents mitochondrial aggregation and alpha-synuclein translocation in SK-N-SH cells in culture. Dev Neurosci 24:143–153
Semkova I, Wolz P, Schilling M, Krieglstein J (1996) Selegiline enhances NGF synthesis and protects central nervous system neurons from excitotoxic and ischemic damage. Eur J Pharmacol 315:19–30
Siddiq A, Ayoub IA, Chavez JC, Aminova L, Shah S, LaManna JC, Patton SM, Connor JR, Cherny RA, Volitakis I, Bush AI, Langsetmo I, Seeley T, Gunzler V, Ratan RR (2005) Hypoxia-inducible factor prolyl 4-hydroxylase inhibition. A target for neuroprotection in the central nervous system. J Biol Chem 280:41732–41743
Tatton WG, Chalmers-Redman RM, Ju WJ, Mammen M, Carlile GW, Pong AW, Tatton NA (2002) Propargylamines induce antiapoptotic new protein synthesis in serum- and nerve growth factor (NGF)-withdrawn, NGF-differentiated PC-12 cells. J Pharmacol Exp Ther 301:753–764
Temlett JA, Landsberg JP, Watt F, Grime GW (1994) Increased iron in the substantia nigra compacta of the MPTP-lesioned hemiparkinsonian African green monkey: evidence from proton microprobe elemental microanalysis. J Neurochem 62:134–146
Tonchev AB, Yamashima T, Chaldakov GN (2007) Distribution and phenotype of proliferating cells in the forebrain of adult macaque monkeys after transient global cerebral ischemia. Adv Anat Embryol Cell Biol 191:1–106
Van Kampen JM, Eckman CB (2006) Dopamine D3 receptor agonist delivery to a model of Parkinson’s disease restores the nigrostriatal pathway and improves locomotor behavior. J Neurosci 26:7272–7280
Vila M, Jackson-Lewis V, Vukosavic S, Djaldetti R, Liberatore G, Offen D, Korsmeyer SJ, Przedborski S (2001) Bax ablation prevents dopaminergic neurodegeneration in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model of Parkinson’s disease. Proc Natl Acad Sci USA 98:2837–2842
Warshawsky A, Youdim MB, Fridkin M, Zheng HL, Warshawsky R (2004) Preparation of neuroprotective iron chelators and pharmaceutical compositions comprising them. Int Publication Number WO 2004041151, A2
Weinreb O, Bar-Am O, Amit T, Chillag-Talmor O, Youdim MB (2004) Neuroprotection via pro-survival protein kinase C isoforms associated with Bcl-2 family members. Faseb J 18:1471–1473
Weinreb O, Amit T, Bar-Am O, Sagi Y, Mandel S, Youdim MB (2006) Involvement of multiple survival signal transduction pathways in the neuroprotective, neurorescue and APP processing activity of rasagiline and its propargyl moiety. J Neural Transm Suppl 70:457–465
Weinstock M, Gorodetsky E, Poltyrev T, Gross A, Sagi Y, Youdim MBH (2003) A novel cholinesterase and brain-selective monoamine oxidase inhibitor for the treatment of dementia comorbid with depression and Parkinson’s disease. Prog Neuro-Psychopharmacol Biol Psychiatry 27:555–561
Yang L, Matthews RT, Schulz JB, Klockgether T, Liao AW, Martinou JC, Penney J B Jr, Hyman BT, Beal MF (1998) 1-Methyl-4-phenyl-1,2,3,6-tetrahydropyride neurotoxicity is attenuated in mice overexpressing Bcl-2. J Neurosci 18:8145–8152
Yoshimi K, Ren YR, Seki T, Yamada M, Ooizumi H, Onodera M, Saito Y, Murayama S, Okano H, Mizuno Y, Mochizuki H (2005) Possibility for neurogenesis in substantia nigra of parkinsonian brain. Ann Neurol 58:31–40
Youdim MBH (2003) Rasagiline: an anti-Parkinson drug with neuroprotective activity. Future Drugs 3:737–749
Youdim MBH, Wadia A, Tatton NA, Weinstock M (2001) The anti-Parkinson drug rasagiline and its cholinesterase inhibitor derivatives exert neuroprotection unrelated to MAO inhibition in cell culture and in vivo. Ann N Y Acad Sci 939:450–458
Youdim MBH, Stephenson G, Ben Shachar D (2004) Ironing iron out in Parkinson’s disease and other neurodegenerative diseases with iron chelator: a lesson from 6-hydroxopaime and iron chelatos desferal and VK-28. Ann N Y Acad Sci 1012:306–325
Youdim MB, Bar Am O, Yogev-Falach M, Weinreb O, Maruyama W, Naoi M, Amit T (2005) Rasagiline: neurodegeneration, neuroprotection, and mitochondrial permeability transition. J Neurosci Res 79:172–179
Youdim MB, Amit T, Bar-Am O, Weinreb O, Yogev-Falach M (2006) Implications of co-morbidity for etiology and treatment of neurodegenerative diseases with multifunctional neuroprotective-neurorescue drugs; ladostigil. Neurotox Res 10:181–192
Youdim MB, Grunblatt E, Mandel S (2007) The copper chelator, D-penicillamine, does not attenuate MPTP induced dopamine depletion in mice. J Neural Transm 114:205–209
Zaman K, Ryu H, Hall D, O’Donovan K, Lin KI, Miller MP, Marquis JC, Baraban JM, Semenza GL, Ratan RR (1999) Protection from oxidative stress-induced apoptosis in cortical neuronal cultures by iron chelators is associated with enhanced DNA binding of hypoxia-inducible factor-1 and ATF-1/CREB and increased expression of glycolytic enzymes, p21(waf1/cip1), and erythropoietin. J Neurosci 19:9821–9830
Zecca L, Youdim MB, Riederer P, Connor JR, Crichton RR (2004) Iron, brain ageing and neurodegenerative disorders. Nat Rev Neurosci 5:863–873
Zecca L, Berg D, Arzberger T, Ruprecht P, Rausch WD, Musicco M, Tampellini D, Riederer P, Gerlach M, Becker G (2005) In vivo detection of iron and neuromelanin by transcranial sonography: a new approach for early detection of substantia nigra damage. Mov Disord 20:1278–1285
Zhao M, Momma S, Delfani K, Carlen M, Cassidy RM, Johansson CB, Brismar H, Shupliakov O, Frisen J, Janson AM (2003) Evidence for neurogenesis in the adult mammalian substantia nigra. Proc Natl Acad Sci USA 100:7925–7930
Zheng H, Gal S, Weiner LM, Bar-Am O, Warshawsky A, Fridkin M, Youdim MB (2005a) Novel multifunctional neuroprotective iron chelator-monoamine oxidase inhibitor drugs for neurodegenerative diseases: in vitro studies on antioxidant activity, prevention of lipid peroxide formation and monoamine oxidase inhibition. J Neurochem 95:68–78
Zheng H, Weiner LM, Bar-Am O, Epsztejn S, Cabantchik ZI, Warshawsky A, Youdim MBH, Fridkin M (2005b) Design, synthesis, and evaluation of novel bifunctional iron-chelators as potential agents for neuroprotection in Alzheimer’s, Parkinson’s, and other neurodegenerative diseases. Bioorg Med Chem 13:773–783
Zhu W, Xie W, Pan T, Xu P, Fridkin M, Zheng H, Jankovic J, Youdim MB, Le W (2007) Prevention and restoration of lactacystin-induced nigrostriatal dopamine neuron degeneration by novel brain-permeable iron chelators. Faseb J 21:3835–3844
Zhu W, Xie W, Pan T, Jankovic J, Li J, Youdim MB, Le W (2008) Comparison of neuroprotective and neurorestorative capabilities of rasagiline and selegiline against lactacystin-induced nigrostriatal dopaminergic degeneration. J Neurochem 105:1970–1978
Acknowledgments
We wish to thank Technion-Research and Development (Haifa), Alzheimer Drug Discovery Foundation (New York), World Class University Program (R33-10014), Seoul University for their generous support. The generous supply of M30 from Varinel Inc (USA) is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gal, S., Zheng, H., Fridkin, M. et al. Restoration of Nigrostriatal Dopamine Neurons in Post-MPTP Treatment by the Novel Multifunctional Brain-Permeable Iron Chelator-Monoamine Oxidase Inhibitor Drug, M30. Neurotox Res 17, 15–27 (2010). https://doi.org/10.1007/s12640-009-9070-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-009-9070-9