Abstract
Malaria is an infectious and deadly parasitic disease, associated with fever, anaemia and other ailments. Unfortunately the upsurge of plasmodium multidrug resistant constrained researchers to look for new effective drugs. Medicinal plants seem to be an unquenchable source of bioactive principles in the treatment of various diseases. The aim of this study was to assess the antiplasmodial activity of two Ivorian medicinal plants. The in vitro activity was evaluated against clinical isolates and Plasmodium falciparum K1 multidrug resistant strain using the fluorescence based SYBR green I assay. The in vivo bioassay was carried out using the classical 4 day suppressive and curative tests on Plasmodium berghei infected mice. Results showed that the in vitro bioassay of both plant extracts were found to exhibit a promising and moderate antiparasitic effects on clinical isolates (5 µg/mL < IC50 < 15 µg/mL) and Plasmodium falciparum multidrug resistant K1 strain (15 µg/mL < IC50 < 50 µg/mL). Furthermore, the in vivo antiplasmodial screening of both extracts showed a significant decrease in parasitemia, which was dose-dependent. Body temperature in mice treated with both extracts at experimental doses increased, compared to the negative control group and was dose-dependent. As for mice body weight a significant decrease (p < 0.001) was noticed in the negative control group compared to tested groups of animals. The hydroethanolic stem bark extract of Anthocleista djalonensis A Chev and leaves extract of Ziziphus mauritiana Lam exhibited anti-malarial activities. Therefore, the bioactive compounds of both plant extracts need to be investigated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malaria is an infectious and deadly parasitic disease caused by the genus plasmodium, transmitted to human beings through a bite of an infected mosquito of the anopheles genus and this disease is associated with fever, anemia and other ailments (Chen et al. 2016).
Many countries around the world were listed malaria risk area and according to the latest estimates from the World Health Organization there were 214 million new cases of malaria with a record of 438,000 malaria deaths globally (WHO, World malaria report 2016).
Furthermore, in areas with high transmission of malaria, children under 5 years of age are particularly susceptible to infection. In 2015, malaria killed about 303,000 including 292,000 in the African region (WHO, World malaria report 2016).
Indeed, malaria remains one of the world’s most dreaded infectious parasitosis (Kaushik et al. 2013) and is still a major health problem in tropical countries (WHO, World malaria report 2015).
Artemisinin based combination therapies is the first line treatment against uncomplicated malaria on account of his highly effectiveness against Plasmodium falciparum (WHO, World malaria report 2015). Unfortunately, one of the major issue associated with malaria chemotherapy is drug resistance. Parasites are consistently been able to develop resistance to each new class of drugs, and the emergence of parasite resistant to artemisinin has been reported in Cambodia, Thailand, Myanmar, Laos and Vietnam, representing a great threat to effort to control and eventually eradicate malaria (Cui et al. 2015; WHO, Status report 2016). The problem is appalling and there is need for developing new drugs (Nondo et al. 2017).
For time immemorial medicinal plants have been a valuable source for the treatment of various diseases and an area to search for new antimalarials (Newman and Cragg 2016; Birru et al. 2017).
The objective of this study was to evaluate the antimalarial activity of the hydroethanolic stem bark extract of Anthocleista djolonensis A.Chev and leaves of Ziziphus mauritiana Lam two medicinal plants used by traditional healers.
Materials and methods
Collection and preparation of plant extract
Fresh leaves of Ziziphus mauritiana Lam and stem barks of Anthocleista djalonensis A.Chev were collected in Abidjan (Côte d’Ivoire). Both plants were authenticated at the Ivorian National Floristic Center (University of Felix Houphouet Boigny, Côte d’Ivoire). Then, plant samples were air dried in shade at room temperature and ground into powder. Then 100 g of each part of plant powder were separately macerated with 70% ethanol (1.5 L) at room temperature for 72 h and filtered through cotton sieve then on Whattman filter paper for 24 h. The filtrate was evaporated through rotary vacuum evaporator and dried in an oven at 45 °C for 48 h to obtain a dry extract which was stored at 4 °C (Zirihi et al. 2003) for further use.
Phytochemical screening test
The phytochemical screening of the hydroethanolic extracts of Anthocleista djalonensis A.Chev stem bark (HAd) and Ziziphus Mauritiana Lam leaves (HZm) were carried out to determine the presence of the following phytochemicals, Tanins, Alkaloids, Flavonoids, saponins, glycosides, sterols, terpenoids, quinones using standard procedures (Békro et al. 2007; Bidie et al. 2011).
In vitro antimalarial activity
Malaria parasites
Informed consent was obtained from all patients in this study prior to clinical isolates collection. Study approval was issued from the Ivorian National Ethical Committee and Research. Four fresh clinical isolates of Plasmodium falciparum such as ANKTC023, ANKTC024, ANKTC025 and ANKTC026 were obtained from symptomatic patients, at the Community Health Center of Anoukoua-Koute in the district of Abobo (Abidjan, Côte d’Ivoire). Moreover, Plasmodium falciparum multidrug resistant K1 strain (ATCC MRA-159, MR4, ATCC®Manassas, Virginia), obtained from USA was used for this study. The parasite was cultivated and maintained continuously in a human type O positive erythrocytes according to the method described by Trager and Jensen (1976).
In vitro antiplasmodial assay
Culture medium was consisted of RPMI 1640 medium [supplemented with 12.60 mL HEPES (25 mM), 100 mL hypoxanthine, 312.5 µL gentamycin (40 mg/mL) and glucose (20 g/L, Wagtech)]. Symptomatic blood samples of patients collected in EDTA collecting tubes were centrifuged at 3000 rpm for 5 min, then blood serum and buffy coat were removed and blood pellet washed thrice in RPMI 1640 medium (Gibco USA) and diluted with uninfected human type O positive red blood cells to reach a parasitemia of 0.24% at 1.5% hematocrit. Thawing of Plasmodium falciparum K1 strain was performed according to the method described by Witkowski et al. 2010, (2013). After withdrawing the cryovial from the nitrogen liquid, it was left thawing inside the Biosafety hood Class II (STERILGUARD) and transferred in a Falcon tube (15 mL) and then centrifuged at 3000 rpm for 5 min. The supernatant was removed, an equal volume of NaCl (3.5%) was added dropwise to blood pellet and slowly stirred. The tube was left resting for 1 min, then 12 mL of RPMI 1640 washing medium preheated at 37 °C was added and centrifuged at 3000 rpm for 5 min and the supernatant was removed. Then 50 µL of the blood pellet was suspended in 8 mL of complete medium in a culture flask cells (25 mL, Nunc WVR) and a volume of 110 µL of uninfected human type O positive red blood cells were added at 2% hematocrit. Daily, the infected blood pellets were transferred into fresh complete medium to propagate the culture.
The stock solution of both crude extracts and Chloroquine were dissolved separately, 10 mg of each substance in 10 mL of distilled water to obtain a concentration of 1 mg/mL. Extract stock solutions were autoclaved at 121 °C for 15 min to sterilize them. As for Chloroquine a 0.22 µm Millipore filter was used for filtration. Aliquot of extracts and chloroquine were diluted in a complete medium and 100 µL of each aliquot was a twofold serial dilutions (100 µL) were performed in a 96 well microplate and concentrations ranged from 100 to 1.56 µg/mL for crude extracts and from 1600 to 3.125 nM for chloroquine. Plasmodium falciparum multidrug resistant K1 strain was synchronized by 10% D sorbitol (w/v) treatment at the ring stage prior to test. Then a volume of 100 µL of the inoculum (parasitized erythrocytes) was added to each well to reach a final volume of 200 µL. Infected erythrocytes non-treated with drugs were used as negative control whereas infected erythrocytes treated with chloroquine (CQ) were used as positive control. All experiments were run in duplicate. Microplates were confined in a candle jar saturated with CO2 and incubated at 37 °C in an incubator for 72 h. After 72 h of incubation, microplates were preserved at − 20 °C.
Evaluation of parasitemia and determination of IC50
After thawing of the 96 well microplates 100 μL of each well containing a volume of 200 µL was transferred in a new 96 well microplate and 100 μL of SYBR Green I lysis buffer (5 μL of SYBR Green was mixed to 25 mL of lysis buffer) was added to each well using a multi-channel pipette and incubated in a dark room at 37 °C for 1 h. Fluorescence was measured with a spectro-fluorimeter BIOTEK microplate reader (BIOTEK, FLX 800) with excitation and emission wavelength bands centered at 485 and 530 nm, respectively. IC50 (concentration of a tested substance inhibiting 50% of parasites growth) was determined through analysis of dose–response curves using the software IVART (In vitro Analysis and Reporting Tool) of WWARN (Le Nagard et al. 2011).
In vivo antimalarial bioassay
Animal material
Swiss albino mice of both sexes with body weight ranging from 22 to 25 g used for this study were obtained from the animal husbandry of the Department of Nutrition and Pharmacology, Faculty of Biosciences, University of Felix Houphouet Boigny (Abidjan, Côte d’Ivoire). Animals were housed in plastic cages in a temperature and light controlled room with 12 h dark and 12 h light cycle. They were fed with food pellets and given water ad libitum.
All experiments in this study were conducted in accordance with the international standards of animal welfare as recommended by the European Union legislation for the protection of animals used for scientific purposes (Directive 2010/63/EU).
Parasite
The rodent malaria parasite Plasmodium berghei strain (chloroquine sensitive) ATCC-MRA-415 batch no 24,515,338 MR4 ATCC® Manassas, Virginia, was obtained from USA and stored in our Laboratory at − 196.4 °C and used for this study. Plasmodium berghei infected mice has been used because it induces a neurological syndrome in host known as experimental cerebral malaria, whose pathogenesis shares similarities with human cerebral malaria.
Parasite inoculation
Swiss mice previously infected by Plasmodium berghei with a parasitemia rate of 23% were used as donors. The donor mice were anesthesia using ethyl ether and blood was collected through the jugular vein into heparinized vacutainer tube. The neck region of the animal was shaved and the jugular vein appears blue in color and a 25G needle was inserted in the caudocephalic direction (back to front) and blood was withdrawn slowly into EDTA vacutainer tube (Parasuraman et al. 2010). Blood was then diluted with physiological saline (0.9%) in such a way that 200 µL of blood contains 1 × 107 infected red blood cells. Each mouse was intraperitoneally given 200 µL of this diluted blood containing 1 × 107 Plasmodium berghei infected red blood cells.
Suppressive test
The chemo suppressive test of the hydroethanolic crude extracts of both plants was carried out according to the method described by Peters et al. 1975. Forty mice of both sexes were divided into 8 groups of 5 mice each. Mice of each group were intraperitoneally injected 200 µL of red blood cells containing 1 × 107 Plasmodium berghei infected erythrocytes. Three hours after mice infestation, all groups of animal were treated with extracts. Group 1 negative control (200 µL of distilled water); Group 2 positive control (5 mg/Kg of chloroquine); Group 3 (200 mg/Kg of Had), Group 4 (400 mg/Kg of Had); Group 5 (600 mg/Kg of Had); Group 6 (200 mg/Kg of HZm); Group 7 (400 mg/Kg of HZm); Group 8 (600 mg/Kg of HZm). Doses were administered daily by oral route for 4 consecutive days and crude extracts were dissolved in distilled water. On the fifth day (D5), thin blood films were prepared from blood collected from mice tails and stained with 10% Giemsa (v/v).
Curative test
The curative potential of the hydroethanolic crude extracts were carried out according to the method described by Riley and Peters (1970). Forty mice of both sexes were divided into 8 groups of 5 mice each. On Day (0), healthy Swiss mice were intraperitoneally inoculated with 1 × 107 infected erythrocytes. Seventy-two hours later, mice were randomly distributed into their respective groups and were administered crude extract accordingly once daily for 5 days by oral route and crude extracts were dissolved in distilled water. Group 1 negative control (200 µL of distilled water); Group 2 positive control (5 mg/Kg of chloroquine); Group 3 (200 mg/Kg of Had), Group 4 (400 mg/Kg of Had); Group 5 (600 mg/Kg of Had); Group 6 (200 mg/Kg of HZm); Group 7 (400 mg/Kg of HZm); Group 8 (600 mg/Kg of HZm). Thin blood film made daily from the tail of each mouse 3 days after mice infection up to day 8 was stained with Geimsa and examined through a microscope (LEICA) with 100× magnification to monitor parasitemia level. Mean survival time for each group was calculated from date of infection over a period of 30 days (Chandel and Bagai 2010).
Monitoring of mice body weight and temperature
Body weight and rectal temperature of each mouse was measured before infection (day 0) and from day 3 up to day 8 after infection using a sensitive digital weighing scale and a digital thermometer respectively.
Parasitemia evaluation
Parasitemia was determined by counting on 12 fields of each slide to a total of 1000 red blood cells. For low parasitemia (< 1%) 30 fields about 4000 red blood cells were determined (Fidock et al. 2004). The percentage of parasitemia was calculated according to the following formula (Kalra et al. 2006; Toma et al. 2015).
Statistical analyses
Graphics were performed using Graphpad prism 5 software (Microsoft, San Diego California, USA). All values were expressed as mean ± Standard of deviation. Data analysis were performed using one way analysis of variance (ANOVA), followed by Tukey–Kramer multiple comparisms test using Graphpad instat® software. Values were statistically significant at p < 0.05.
Ethical consideration
This study was carried out according to the guidelines of the Ivorian National reference center for malaria chemo-resistance created by the interministerial decree number 393/08/2006, and conduct research according to the Ivorian National Ethical Committee and Research. Therefore, this study was performed after receiving approval from the Ivorian National Ethical Committee and Research.
Results
Phytochemical screening
The hydroethanolic extraction of 100 g of the stem bark of Anthocleista djalonensis (HAd) or leaves of Ziziphus mauritiana Lam (HZm) gave a yield of 13.6 and 9.6% respectively. The phytochemical analysis results of both extracts showing the presence of some secondary metabolites are tabulated in Table 1. Results showed that the hydroethanolic extract of Anthocleista djalonensis contains terpenoids, steroids, cardiac glycosides, polyphenols and flavonoids. Whereas with Ziziphus mauritiana in addition to the secondary metabolites quoted above, the presence of coumarins, quinones, alkaloids and reducing sugar were noticed.
In vitro antiplasmodial activity
The hydroethanolic extracts of Anthocleista djalonensis stem bark and Ziziphus mauritiana leaves were tested on both clinical isolates and Plasmodium falciparum multidrug resistant K1 strain. The results of their antiplasmodial activity are recorded in Table 2. Both extracts showed a significant antiplasmodial activity on clinical isolates with IC50s of 9.94; 10; 9.69 and 5.36 µg/mL for HAd and 9.73; 10.18; 13.63 and 15.42 µg/mL for HZm. HAd and HZm showed an outstanding antiplasmodial activity on clinical isolates. But, tested on Plasmodium falciparum multidrug resistant K1 strain, both extracts showed a moderate activity (15 μg/mL < IC50 < 50 μg/mL).
In vivo antiplasmodial activity
Suppressive test
The hydroethanolic extracts of Anthocleista djalonensis A.Chev stem bark (HAd) and Ziziphus mauritiana Lam (HZm), reduced significantly (p < 0.001 in all cases) parasitemia in Plasmodium berghei infected Swiss mice at doses of 200; 400 and 600 mg/kg body weight, compared to negative control (Table 3), with inhibition percentage of 35.91; 47.86 and 70.55% for HAd and 58.68; 66.12 and 88.97% for HZm. The Inhibition (99.92%) obtained by chloroquine was significantly (p < 0.001) higher than both extracts notwithstanding the dose. Survival time increased and was statistically significant at doses of 400 and 600 mg/Kg body weight for both extracts (Table 3). As for the body weight, weight losses were recorded in each group of mice at day (5), Table 4.
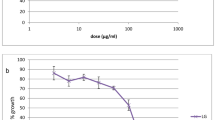
Curative test
Parasitemia in the group treated with distilled water (negative control) increased steadily to reach 56.32% on day 8. As for the group treated with chloroquine (positive control group) parasitemia decreased from 15.75% on day 3 to 0% on day 8. On the other hand, groups treated with 200; 400 and 600 mg/Kg for both extracts exhibited suppression of parasite replication, entailing a reduction of their parasitemia compared to the negative control group (Fig. 1). Survival time increased and was statistically significant at doses of 400 and 600 mg/Kg bw for both extracts (Fig. 3).
As far as mice body weight was concerned the percentage of weight loss decreased for both extracts compared to the negative control group (Table 5). Moreover, the body temperature decreased steadily in the negative control group treated with distilled water. However, body temperature progressively increased in group of mice treated with chloroquine up to day 8. Eventually, a decrease of temperature was observed in groups of mice treated with extracts on day 4 followed by a progressive increase up to day 8, (Fig. 2).
Effect of the hydroethanolic crude extract of Anthocleista djalonensis A Chev and Ziziphus mauritiana Lam on body temperature of Plasmodium berghei infected mice in rane’s test. HAd, Hydroethanolic stem bark extract of Anthocleista djalonensis A Chev; HZm, Hydroethanolic leaf extract of Ziziphus mauritiana Lam
As for mice survival time, it significantly increased according to dose of extracts, (Fig. 3).
Effect of the hydroethanolic crude extract of Anthocleista djalonensis A Chev and Ziziphus mauritiana Lam on the survival time of Plasmodium berghei infected mice in curative test. HAd, Hydroethanolic stem bark extract of Anthocleista djalonensis A Chev; HZm, Hydroethanolic leaf extract of Ziziphus mauritiana Lam
Discussion
In this study, the antiplasmodial activity of two medicinal plant extracts was assessed. The in vitro test was evaluated on 4 clinical isolates and on Plasmodium falciparum multi drug resistant K1 strain. Whereas, the in vivo tests were assessed on Plasmodium berghei infected Swiss mice. According to the natural substance classification scale established by Bero et al. 2009, the hydrothanolic extracts of Anthocleista djalonensis A. Chev and Ziziphus mauritiana Lam showed a promising and moderate anti-malarial activity on both clinical isolates and Plasmodium falciparum multidrug resistant K1 strain respectively.
Thus, the antiplasmodial activity of both plant extracts in vitro was superior to that of Ocimum sanctum leaf extracts (IC50 = 35.58 μg/mL) and Ocimum basilicum (IC50 = 43.81 μg/mL) (Inbaneson and Sundaram, 2012). However, both plant extracts showed a low antiplasmodial activity compared to the dichloromethanic fraction of Eremostachys macrophylla rhizome (IC50 = 0.797 ± 0.016 mg/mL) (Asnaashari et al. 2015).
The in vivo activity was ascertained using Plasmodium berghei infected mice required for antimalarial agents (Ang et al. 2001). The hydroethanolic stem bark extract of Anthocleista djalonensis A.Chev and leaves extracts of Ziziphus mauritiana Lam exhibited a good chemosuppression activity by reducing parasitemia to levels of 75.59 and 88.48% respectively at a dose of 600 mg/Kg in mice. The chemosuppression activity performed by HZm was not significantly different from that induced by chloroquine. As for the curative activity, HAd and HZm showed an increasing inhibitory activity at experimental doses. The phytochemical screening of both plant extracts revealed the presence of several phytocompounds such as alkaloids and terpenoids. Indeed, alkaloids are known for their antiplasmodial activity by blocking protein synthesis in Plasmodium falciparum (Atta-ur-Rahman and Choudhary, 1995; Mojarrab et al. 2014). Likewise, according to several pharmacological studies, terpenoids showed an outstanding activity against protozoans and malaria (Philipson and Wright 1991; Asase et al. 2010). Therefore, the antiplasmodial activity exhibited by both plant extracts could be due to those phytocompounds which could have acted singularly or in association to produce the observed antiplasmodial effect. Furthermore, the promising activity could be due to the inhibition of parasite growth through fatty acid biosynthesis inhibition (Adams et al. 2005; Tasdemir et al. 2007). Plasmodium uses host hemoglobin as a nutrient for growth and multiplication. It ingests more than 75% of hemoglobin during its intra-erythrocytic phase and metabolizes heme into hemozoin (Inbaneson and Sundaram 2012). Thus, these extracts could have acted by blocking the formation of hemozoin in parasites. Moreover, the antiplasmodial activity observed with both plant extracts in vivo was comparable to that obtained with the ethyl acetate fraction of Zehenria scabra (Tesfaye and Alamneh 2014). On the other hand the extracts were more active than the methanolic, ethanolic and dichloromethanolic extracts of Caesalpinia bonducella (11.36, 20.01 and 37.60%) (Nondo et al. 2016).
In this study a significant weight loss was recorded in the control group treated with distilled water compared to groups of mice treated with chloroquine and crude extracts. The weight loss observed during experiment could be due to the lack of appetite causing a disturbed metabolic function and hypoglycemia (Basir et al. 2012).
In this study, the body temperature of mice decreases as parasitemia increases. The severe hypothermia observed in the negative control group treated with distilled water could be attributed to the general debilitating effect of malaria on host resulting in the loss of body heat and death (Basir et al. 2012).
But the progressive increase of body temperature in mice treated with extracts from day 5 might be due to a progressive decrease of parasitemia in treated mice and to the ability of extracts to prevent rapid falling of body temperature (Bantie et al. 2014). In this study mice treated at the dose of 600 mg/Kg with both extracts significantly lived longer than the negative control but was shorter as compared to chloroquine in the curative test. This longest survival time exhibited by both crude extracts might be due on one hand to the antiplasmodial activity of extracts and to the fast elimination phase of extracts from mice body (Muluye et al. 2015) and on the other hand to the presence of bioactive secondary metabolites in sufficient concentration at this dose (Fentahun et al. 2017).
Conclusion
The hydroethanolic stem bark extract of Anthocleista djalonensis A Chev and leaves extract of Ziziphus mauritiana Lam exhibited anti-malarial activities, therefore further studies of its bioactive compounds need to be investigated.
References
Adams Y, Smith SL, Schwartz-Albiez R, Andrews KT (2005) Carrageenans inhibit the in vitro growth of Plasmodium falciparum and cytoadhesion to CD36. Parasitol Res 97:290–294
Ang K, Holmes M, Kara U (2001). Immune-mediated parasite clearance in mice infected with Plasmodium berghei following treatment with manzamine A. Parasitol Res. 87: 715
Asase A, Akwetey GA, Achel DG (2010) Ethnopharmacological use of herbal remedies for the treatment of malaria in the Dangme West District of Ghana. J Ethno pharmacol 129:367–376
Asnaashari S, Afshar FH, Ebrahimi A, Moghadam SB, Delazar A (2015) In vitro antimalarial activity of different extracts of Eremostachys Macrophylla Montbr. & Auch. Bioimpacts 5(3):135–140
Atta-ur-Rahman M, Choudhary I (1995) Supporting the importance of and the restrictions on a carbon-centered radical for high antimalarial activity of 1, 2, 4- trioxanes like artemisinin. J Med Chem 38(13):2273–2275
Bantie L, Assefa S, Teklehaimanot T, Engidawork E (2014) In vivo antimalarial activity of the crude leaf extract and solvent fractions of Croton macrostachyus Hocsht (Euphorbiaceae) against Plasmodium berghei in mice. BMC Complement Altern Med 14:79
Basir R, Rahiman SSF, Hasballah K, Chong WC, Talib H, Yam MF, Jabbarzare M, Tie TH, Othman F, Moklas MAM, Abdullah WO, Ahmad Z (2012) Plasmodium berghei ANKA infection in ICR mice a model of cerebral malaria. Iran J Parasitol 7(4):62–74
Békro YA, Békro JA, Boua BB, Tra BF, Ehilé EE (2007) Etude ethnobotanique et screening phytochimique de caesalpinia benthamiana (baill.) (Caesalpiniaceae). Revue Science et nature 4:217–225
Bero J, Frederich M, Quetin-Leclercq J (2009) Antimalarial compounds isolated from plants used in traditional medicine. J Pharm Pharmacol 61:1401–1433
Bidie P, Banga B, Yapo AF, N’guessan JD, Djaman AJ (2011) Activités antioxydantes de dix plantes médicinales de la pharmacopée ivoirienne. Revue science et nature 8(1):1–11
Birru EM, Geta M, Gurmu AE (2017) Antiplasmodial activity of Indigofera spicata root extract against plasmodium berghei in mice. Malar J 16:198
Chandel S, Bagai U (2010) Antiplasmodial activity of Ajuga bracteosa against Plasmodium berghei infected BALB/C mice. Indian J Med Res 131:440–444
Chen I, Clarke SE, Gosling R, Hamainza B, Killeen G, Magill A, O’Meara W, Price RN, Riley EM (2016) Asymptomatic malaria: a chronic and debilitating infection that should be treated. PLoS Med 13(1):e1001942
Cui L, Mharakurwa S, Ndiaye D, Rathod PK, Rosenthal PJ (2015) Antimalarial drug resistance literature review and activities and finding of the ICEMR network. Am J Trop Med Hyg 93(3 suppl):57–68
Fentahun S, Mekonnen E, Tesfaye A, Giday M (2017) In vivo antimalarial activity of crude extracts and solvent fractions of leaves extract of Strychnos mitis in Plasmodium berghei infected mice. BMC Complement Altern Med 17:13
Fidock DA, Rosenthal PJ, Croft SL, Brun R, Solomon N (2004) Antimalarial drug discovery: efficacy models for compound screening. Nat Rev Drug Discov 3:509–520
Inbaneson SJ, Sundaram R (2012) In vitro antiplasmodial effect of ethanolic extracts of traditional medicinal plant Ocimum species against Plasmodium falciparum. Asian Pac J Trop Med 5(2):103–106
Kalra BS, Chawla S, Gupta P, Valecha N (2006) Screening of antimalarial drugs. Indian J Pharmacol 38:5–12
Kaushik NK, Bagavan A, Rahuman AA, Mohanakrishnan D, Kamaraj C, Elango G et al (2013) Antiplasmodial potential of selected medicinal plants from eastern Ghats of South India. Exp Parasitol 134:26–32
Le Nagard H, Vincent C, Mentre F, Le Bras J (2011) Online analysis of in vitro resistance to antimalarial drugs through nonlinear regression. Comput Methods Programs Biomed 104:10–18
Mojarrab M, Shiravand A, Delazar A, Heshmati Afshar F (2014) Evaluation of in vitro antimalarial activity of different extracts of Artemisia aucheri Boiss. and A. armeniaca L and fractions of the most potent extracts. Sci World J 2014:1–6
Muluye AB, Melese EandAdinew E, Adinew GM (2015) Antimalarial activity of 80% methanolic extract of Brassica nigra (L.) Koch. (Brassicaceae) seeds against Plasmodium berghei infection in mice. BMC Complementary Altern Med 15:367
Newman DJ, Cragg GM (2016) Natural products as sources of new drug over the 30 years from 1981 to 2010. J Nat Prod 75(3):311–315
Nondo RS, Erasto P, Moshi MJ, Zacharia A, Masimba PJ, Kidukuli AW (2016) In vivo antimalarial activity of extracts of Tanzanian medicinal plants used for the treatment of malaria. J Adv Pharm Technol Res 7:59–63
Nondo RSO, Moshi MJ, Erasto P, Masimba PJ, Machumi F, Aw K, Heydreich M, Zofou D (2017) Antiplasmodial activity of norcaesalpin D and extracts of four medicinal plants used traditionally for treatment of malaria. BMC Complement Altern Med 17:167
Parasuraman S, Raveendran R, Kesavan R (2010) Blood sample collection in small laboratory animals. Pharmacol Pharmacother 1(2):87–93
Peters W, Portus JH, Robinson BL (1975) The chemotherapy of rodent malaria XXII. The value of drug-resistant strains of Plasmodium berghei in screening for blood schizonticidal activity. Ann Trop Med Parasitol 69:155–171
Philipson JD, Wright CW (1991) Antiprotozoal compounds from plants sources. Planta Med 57:553–559
Riley JF, Peters W (1970) The antimalarial activity of some quinolone esters. Ann Trop Med Parasitol 84:209–222
Tasdemir D, Topaloglu B, Perozzo R, Brun R, O’Neill R, Carballeira NM et al (2007) Marine natural products from the Turkish sponge Agelas oroides that inhibit the enoyl reductases from Plasmodium falciparum, Mycobacterium tuberculosis and Escherichia coli. Bioorganic Med Chem 15:6834–6845
Tesfaye W, Alamneh EA (2014) In vivo antimalarial activity of the crude extract and solvent of the leaves of Zehenria scabra (Cucurbitaceae) against Plasmodium berghei in mice. J Med Plant Res 8(42):1230–1236
Toma A, Deyno S, Fikru A, Eyado A, Beale A (2015) In vivo antimalarial and toxicological effect of crude ethanol extract of Echinops kebericho traditionnally used in treatment of malaria in Ethiopia. Malar J 14:196
Trager W, Jensen JB (1976) Human malaria parasites in continuous culture. Science 193:673–675
Witkowski B, Lelievre J, Barragan MJ, Laurent V, Su XZ, Berry A, Benoit-Vical F (2010) Increased tolerance to artemisinin in Plasmodium falciparum is mediated by a quiescence mechanism. Antimicrob Agents Chemother 54:1872–1877
Witkowski B, Khim N, Chim P, Kim S, Ke S, Kloeung N, Chy S, Duong S, Leang R, Ringwald P, Dondorp AM, Tripura R, Benoit Vical F, Berry A, Gorgette O, Ariey F, Barale JC, Mercereau-Puijalon O, Menard D (2013) Reduced artemisinin susceptibility of Plasmodium falciparum ring stages in Western Cambodia. Antimicrob Agents Chemother 57:914–923
World Health Organization. Status report (2016): Artemisinin and artemisinin-based combination therapy resistance. Geneva: The Organization; [cited 2016 Aug 16]. http://apps.who.int/iris/ handle/10665/208820
WHO. World malaria report (2015). Geneva
WHO. World malaria report (2016). Geneva
Zirihi G, Kra AKM, Guede-guina F (2003) Evaluation de l’activité antifongique de Microglossa pyrifolia (Lamarck) O. Kantze (Astéracée) « PYMI » sur la croissance in vitro de Candida albicans. Revue de Médecine et pharmacopée Africaines 17(3):11–18
Acknowledgements
The authors are grateful to Institut Pasteur of Côte d’Ivoire for providing us with Plasmodium falciparum multidrug resistant K1 strain and to the Laboratory of Nutrition and Pharmacology of the University of Felix Houphouet Boigny, Côte d’Ivoire.
Author information
Authors and Affiliations
Contributions
Study concept and design: KS and DAJ; Study supervision: KS, DAJ and TOA; Statistical analysis: ADSD and BS; Material support: TOA and KA; Laboratory bioassay: ADSD, BS, TK and GAA; Analysis and interpretation of data: ADSD, TK and GA; Drafting of the manuscript: ADSD and BS; Revision of final manuscript: ADSD, BS, TK, GAA, KA, TOA, KS and DAJ
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Attemene, S.D.D., Beourou, S., Tuo, K. et al. Antiplasmodial activity of two medicinal plants against clinical isolates of Plasmodium falciparum and Plasmodium berghei infected mice. J Parasit Dis 42, 68–76 (2018). https://doi.org/10.1007/s12639-017-0966-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12639-017-0966-7