Abstract
Background
Patients undergoing major vascular surgery are at high risk of postoperative delirium and postoperative cognitive dysfunction (POCD). Apolipoprotein E (APOE) is involved in central acetylcholine synthesis, and patients bearing the ε4 genotype (APOE-ε4) are at increased risk of both vascular dementia and peripheral vascular disease. The purpose of this study was to evaluate the associations among delirium, POCD, and APOE-ε4 in patients undergoing open aortic repair.
Methods
Following Research Ethics Board approval and written informed consent, we recruited a cohort of patients ≥ 60 yr of age undergoing open aortic repair. Apolipoprotein E genotyping and a battery of nine neuropsychometric (NP) tests were performed prior to surgery. Delirium was assessed on postoperative days two, four, and discharge using the Confusion Assessment Method. Neuropsychometric testing was repeated at discharge and again three months following surgery. A group of non-surgical patients was used to adjust NP scores using reliable change index methodology. Logistic regression was used to evaluate independent predictors of both delirium and POCD.
Results
Eighty-eight patients underwent surgery, 78 completed NP testing on discharge, and sixty-nine completed NP testing at three months. Delirium was noted in 36% of patients after surgery, while POCD was noted in 62% at discharge and 6% at three months. Delirium predicted POCD at discharge (odds ratio 2.86; 95% confidence intervals 0.99 to 8.27) but not at three months. Apolipoprotein E-ε4 genotype was not associated with either delirium or POCD following adjustment for covariates.
Conclusion
Both delirium and POCD are common following open aortic repair; however, the APOE genotype did not predict either condition. This trial has been registered with ClinicalTrials.gov (NCT00911677).
Résumé
Contexte
Les patients subissant une chirurgie vasculaire majeure courent un risque élevé de manifester du delirium postopératoire ainsi qu’un dysfonctionnement cognitif postopératoire (DCPO). L’apolipoprotéine E (APOE) intervient dans la synthèse centrale de l’acétylcholine, et les patients possédant le génotype ε4 (APOE-ε4) présentent un risque accru de démence vasculaire et de maladie vasculaire périphérique. L’objectif de cette étude était d’évaluer les associations entre le delirium, le DCPO et l’APOE-ε4 chez les patients subissant une chirurgie ouverte de l’aorte.
Méthode
Après avoir reçu l’approbation du Comité d’éthique de la recherche et le consentement éclairé par écrit des patients, nous avons recruté une cohorte de patients de ≥ 60 ans subissant une chirurgie ouverte de l’aorte. Le génotypage de l’apolipoprotéine E et une batterie de neuf tests neuro-psychométriques (NP) ont été réalisés avant la chirurgie. Le delirium a été évalué aux jours postopératoires deux et quatre ainsi qu’au congé à l’aide de la Méthode d’évaluation de la confusion. Les tests neuro-psychométriques ont été refaits au moment du congé puis trois mois après la chirurgie. Un groupe témoin de patients non chirurgicaux a été utilisé pour ajuster les scores NP à l’aide d’une méthodologie fiable d’indice de changement. La régression logistique a été utilisée pour évaluer les prédicteurs indépendants de delirium et de DCPO.
Résultats
Quatre-vingt-huit patients ont subi une chirurgie, soixante-dix-huit ont subi les tests NP au congé, et soixante-neuf ont subi les tests NP à trois mois. On a observé du delirium chez 36 % des patients après la chirurgie, alors que le DCPO a été observé chez 62 % au congé et 6 % à trois mois. La présence de delirium a constitué un prédicteur de DCPO au congé (rapport de cotes 2,86; intervalles de confiance 95 % 0,99 à 8,27) mais pas à trois mois. Le génotype de l’apolipoprotéine E-ε4 n’a pas été associé au delirium ou au DCPO après ajustement pour tenir compte des covariables.
Conclusion
Le delirium et le DCPO sont des événements fréquents après une chirurgie ouverte de l’aorte; toutefois, le génotype APOE n’a pas permis de prédire leur survenue. Cette étude a été enregistrée au ClinicalTrials.gov (NCT00911677).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Delirium is a transient fluctuating disturbance of consciousness, attention, cognition, and perception1 that frequently complicates the course of hospitalized patients. A review of 80 primary studies revealed that delirium develops in 36.8% (range 0-73.5%) of surgical patients.2 Recent estimates suggest that treatment of delirium adds US$ 2,500 to hospital stays of patients>65 yr of age, costing Medicare approximately US$ 6.9 billion annually.3 Delirium is prevalent particularly among patients undergoing major vascular surgery, affecting 29-46% of such patients.4 A prospective cohort study of delirium following non-cardiac surgery demonstrated that patients undergoing open aortic repair faced eightfold greater odds of postoperative delirium than patients undergoing all other non-cardiac surgical procedures.5 Delirium is a harbinger of poor patient outcome and is associated with increased length of hospital stay,6 greater rates of nursing home placement,7 and mortality rates approaching 30%.8 While delirium is a well-known, but under-recognized complication of the immediate postoperative period, recent research indicates that postoperative cognitive decline may be a longer-lasting consequence of major non-cardiac surgery.
Postoperative cognitive dysfunction (POCD) is a more subtle disorder of thought processes that affects different domains of cognition, such as verbal memory, visual memory, language comprehension, visuospatial abstraction, attention, and concentration.9 In a recent observational study, Monk et al. identified POCD in 138 of 333 (41%; 95% confidence intervals [CI] 36.2 to 46.7%) elderly patients one week after elective non-cardiac surgery.10 As with delirium, POCD immediately following surgery appears to have long-term health implications. Patients with POCD one week following surgery are more likely to leave employment, while those with POCD persisting three months postoperatively suffer an increased risk of mortality in the five years following surgery.11
Perioperative physicians may have difficulty distinguishing between delirium and POCD, and they may use the terms interchangeably. Both patients and physicians fear that the development of delirium in the early postoperative period leads to lasting changes in cognition following discharge.
Failure of cholinergic neurotransmission is considered to be central to the mechanism of both delirium12 and progressive dementias, such as Alzheimer’s disease and vascular dementia.13 Apolipoprotein E (APOE) is a component of plasma lipoprotein that is believed to play a central role in lipid transport and acetylcholine synthesis within the brain.14 The gene coding for APOE exists in three different allele polymorphisms, i.e., ε2, ε3, and ε4. Patients in the Canadian Study of Health and Aging who carried the APOE-ε4 allele were three times as likely to develop vascular dementia (odds ratio [OR] 3.13; 95% CI 1.76 to 5.55) and Alzheimer’s disease (OR 2.89; 95% CI 1.96 to 4.28).15 After adjustment for age and non-lipid risk factors, men in the Framingham Heart Health Study who carried APOE-ε4 were at a significantly increased risk of cardiovascular disease (OR 1.63; 95% CI 1.23 to 3.04).16 These findings suggest that patients undergoing vascular surgery may be more likely to carry the APOE-ε4 allele, and this may explain, in part, the increased incidence of cognitive impairment in this population. The relationships among APOE-ε4, cognition, and cardiovascular disease raise two research questions. If APOE-ε4 is related to decreases in brain acetylcholine and cardiovascular disease, to what extent might this gene explain the frequency with which delirium occurs following vascular surgery? If APOE-ε4 predicts dementia, could it also predict the patient at risk for POCD?
The primary objective of this study was to evaluate the relationships among delirium, POCD, and APOE-ε4 in a cohort of patients undergoing major vascular surgery. Secondary objectives were to document the association between cognitive change in the postoperative period and major postoperative morbidity and quality of life. We hypothesized that patients experiencing delirium in the immediate postoperative period would be more likely to have measurable changes in cognition in the three-month interval following elective aortic aneurysm repair. Furthermore, we anticipated that those patients with the APOE-ε4 genotype would be more likely than those of other genotypes to experience postoperative delirium and/or cognitive dysfunction.
Methods
This prospective observational cohort study complies with the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) initiative17 and has been registered with ClinicalTrials.gov (NCT00911677). Following Research Ethics Board approval, patients 60 yr of age and older undergoing elective open repair of the abdominal aorta at the Ottawa Hospital, a 1,000 bed academic tertiary care centre, were assessed for study eligibility. Screening for the trial began on August 29, 2005, and the final assessment was completed on March 26, 2008. Patients meeting the following criteria were excluded: 1) refusal of informed consent; 2) planned endovascular repair; 3) emergency surgery; 4) previous diagnosis of dementia, Parkinson’s disease, or psychiatric illness; 5) active alcohol or substance abuse; and 6) physical inability to complete psychometric testing. Informed written consent was obtained from eligible consenting patients and baseline measurements were obtained. The following basic demographic information was recorded: age, sex, years of education, American Society of Anesthesiologists’ (ASA) status, revised cardiac risk score, height, and weight. Preoperative use of central nervous system (CNS)-active medications and history of alcohol use/abuse were noted. A blood sample for APOE genotyping was drawn at the preoperative visit.
Patients enrolled in this study received the usual perioperative care. Monitoring, anesthetic technique, and postoperative analgesia were at the discretion of the attending anesthesiologist. All patients were offered combined epidural and general anesthesia for intraoperative care. Epidural analgesia was planned with 0.1% bupivacaine with fentanyl 2 μg·kg−1 or hydromorphone 10 μg·kg−1. Patients requiring postoperative mechanical ventilation were sedated with propofol at the discretion of the critical care physician. The prophylactic use of anticholinergic medications (scopolamine), antipsychotic medications (haloperidol), or meperidine for postoperative analgesia was prohibited.
At the time points shown in Table 1, preoperative cognitive function was assessed by trained psychometrists under similar conditions and, whenever possible, by the same evaluator. The Mini Mental State Examination (MMSE) is a clinical tool used frequently to screen for dementia. Consenting patients scoring 23 or less on the MMSE were excluded from further testing and participation in the trial. Detailed neuropsychometric (NP) testing was performed using a battery of nine NP tests compliant with the consensus guidelines for cognitive testing following cardiac surgery18 and similar in content to the International Study of Postoperative Cognitive Dysfunction (ISPOCD) battery.9 To optimize the reliability of the NP evaluation, the psychometrists were trained and audited periodically by the same neuropsychologist (L.R.). Learning efficiency and memory consolidation were evaluated with the Rey Auditory Verbal Learning Test. Psychomotor speed and dexterity, known to be a sensitive indicator of the presence of generalized brain dysfunction, was measured by the Trails A and B, Grooved Pegboard, and Symbol Digit Modalities Tests (oral administration). Attentiveness and control were evaluated using the revised Wechsler Adult Intelligence Scale Digit Span. To further evaluate this domain, we added the Mental Control Subtest of the Wechsler Memory Scale-III, wherein the score reflects both speed and accuracy. Letter and Category Fluency was used to assess the speed and flexibility of verbal thought processes. The nine NP tests that were selected generate 12 independent measures of cognition.
Delirium was assessed in hospital at the time points indicated in Table 1 using the Confusion Assessment Method (CAM).19 An optional CAM assessment was performed on postoperative day (POD) seven for patients whose hospital lengths of stay were anticipated to be substantially longer than one week. The CAM poses nine questions to an observer regarding the mental processes of the patient being examined. The CAM then identifies four diagnostic features of delirium: 1) acute onset and fluctuating course; 2) inattention; 3) disorganized thinking; and 4) altered level of consciousness. The CAM provides a dichotomous outcome – delirium is either present or absent – based on the presence of features 1 and 2 plus either feature 3 or 4. The sensitivity and specificity of the CAM both exceed 90% and the inter-rater reliability is high (κ = 0.81-1.0).
Variables associated with delirium4 and POCD10 were recorded. Pre- and postoperative measures of mood (Geriatric Depression Scale) and anxiety (State-Trait Anxiety Inventory) were also recorded. The total battery required 60 min to administer. The Short Form Health Survey (SF-12) (QualityMetric Inc, Lincoln, RI, USA) was administered preoperatively and three months postoperatively to assess health-related quality of life.
Non-cognitive outcomes were recorded, including all-cause mortality, duration of hospital stay, duration of intensive care unit stay, duration of mechanical ventilation, unanticipated intensive care unit admission, failure to discharge home, myocardial infarction, pneumonia, and renal failure.
A reliable change index method consistent with ISPOCD methods9 was chosen to categorize the presence or absence of POCD from the NP testing battery. First, in a cohort of non-surgical volunteers (n = 45) recruited from outpatient cardiology clinics, we measured the average amount of change over time in the performance on the cognitive tests to quantify the practice effect. These non-surgical controls underwent NP testing at time points similar to those of our surgical cohort. Baseline (preoperative) scores for the surgical patients were compared with the discharge and three-month postoperative test results after first subtracting the average practice effect for those intervals measured in the non-surgical cohort. The result was divided by the standard deviation of the non-surgical cohort to obtain a standardized Z score for each individual test. The direction of change in the Z score for each test was adjusted to ensure that cognitive decline yielded a negative value. The Z scores for all tests were pooled, yielding a composite Z score reflecting an overall construct of POCD. The composite score was calculated as the sum of the Z scores for an individual patient divided by the standard deviation for the sum of Z scores in the non-surgical control group. A patient was classified as having POCD if the Z scores on either two individual tests or the combined Z score was -1.96 or more negative. This definition (from the ISPOCD group) identifies patients with either general cognitive decline or substantial deterioration in two or more isolated domains of cognition.
Individual test scores are described with mean and standard deviations at all time points, and the incidence of delirium and POCD are expressed as a percent with 95% CI. Bivariable associations between delirium and POCD were expressed as ORs and 95% CI. Likewise, bivariable associations between risk factors, including APOE genotype and outcomes, were explored using Chi square statistics, OR, and 95% CI. The effect of risk factors potentially confounding the relationship between APOE genotype and outcome was explored using logistic regression and presented as adjusted ORs with 95% CIs. We considered P values <0.05 as significant.
Delirium develops in 29-46% of patients hospitalized following major vascular surgery.4 In eastern Canada, the prevalence of patients who are homozygous or heterozygous for APOE-ε4 is estimated at 3.9% and 30.4%, respectively.20 Sample size calculations for testing the delirium-POCD association were carried out under the following assumptions: a) the incidence of delirium in our study population is 40%; b) a 32% absolute increase in POCD (from 40% to 72% in patients with delirium or an OR of 3.86) would be clinically significant; and c) there would be a 10% loss to follow-up. Under these conditions, a cohort of 90 patients would yield 82% power to detect the above stated increase in incidence of POCD using a two-sided Pearson Chi square test at the 5% level of significance.
Sample size calculations for testing the APOE-delirium association were carried out under the following assumptions: a) the prevalence of any APOE-ε4 allele in our study population is 35%; b) a 32% absolute increase in the incidence of delirium (from 30% in non-APOE-ε4 carriers to 62% in APOE-ε4 carriers, or an OR of 3.81) would be clinically significant; and c) there would be a 10% loss to follow-up. Under these conditions, a cohort of 90 patients would yield 80% power to detect the above-stated increase in incidence of delirium using a two-sided Pearson Chi square test at the 5% level of significance.
Results
Two hundred sixty-eight patients scheduled for open repair of the abdominal aorta were screened, 100 consented to NP testing, and 88 underwent open aortic repair. Patient flow through the trial is summarized in the Figure. The demographic characteristics of those with (n = 21) and without (n = 66) the APOE ε4 allele are shown in Table 2. Apolipoprotein E genotyping was unavailable for a single patient who died intraoperatively. Fifteen cases of delirium were identified on POD 2; 20 cases (13 new and seven preexisting) were noted on POD 4; six cases were noted on POD 7 (one new, five preexisting); and three patients remained delirious at the time of discharge testing (one new, two preexisting). In total, delirium was noted in 30 of 84 patients (36%, 95% CI 26 to 46) completing the CAM assessment at any time during their hospital stay.
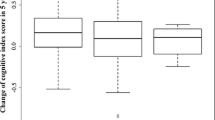
Postoperative cognitive dysfunction was noted in 48 of 78 patients (60%, 95% CI 51 to 72) completing neuropsychometric testing at discharge and four of 69 patients (6%, 95% CI 0.3 to 11) completing testing at three months. Raw scores on NP testing are shown in Table 3, and change scores corrected for learning effect are shown in Table 4. Non-cognitive outcomes for all 88 patients undergoing surgery are presented in Table 5.
The association between delirium and POCD is shown in Table 6. Patients noted to have delirium while in hospital were more likely to have POCD at discharge (OR 2.86; 95% CI 0.99 to 8.27); however, 28 of 48 cases of POCD were not preceded by a positive CAM. No statistically significant association was noted between delirium in hospital and POCD three months postoperatively (OR 2.10; 95% CI 0.28 to 15.92).
Relationships between APOE ε4 genotype and cognitive outcomes are described in Table 7. The incidence of delirium in hospital was 45% among APOE-ε4 genotype carriers vs 33% among non-carriers (unadjusted OR 1.63; 95% CI 0.59 to 4.56). The incidence of POCD at discharge was 67% among carriers vs 60% among non-carriers (OR 1.33; 95% CI 0.44 to 4.04). The associations between APOE-ε4 genotype and delirium and POCD were corrected for important factors associated with outcome demonstrated in previous research and/or on bivariable analysis in this data set. Adjustment variables included age, ASA physical class, Geriatric Depression Scale, MMSE, OR time and yielded adjusted ORs for delirium (OR 1.68; 95% CI 0.60 to 4.66), and POCD at discharge (OR 1.33; 95% CI 0.44 to 4.04). These results support the absence of a statistically significant association between APOE-ε4 and early cognitive outcomes in this cohort. While the point estimate relating APOE-ε4 and POCD at three months following suggests an association (OR 3.64; 95% CI 0.47 to 28.22), the small number of events and the wide CI preclude further inference.
The mean scores on the physical and mental component scores (PCS and MCS, respectively) of the Short Form 12 completed preoperatively and three months following surgery are shown in Table 8. The Short Form 12 generates a standardized score based on population norms, with lower scores indicating decreased quality of life. Anticipated PCS and MCS scores in the general population are 50 ± 9 and 50 ± 10, respectively, while scores from those aged 65 to 74 yield PCS scores of 44 ± 11 and MCS scores 52 ± 10. Mean changes in MCS and PCS scores for all study patients and those reporting cognitive disturbances are also shown in Table 8. Despite the stresses of abdominal aortic aneurysm repair, no statistically significant changes in MCS or PCS scores were noted, even among those experiencing delirium or POCD in the perioperative period.
Discussion
The results of the present study indicate that both delirium and POCD were common sequelae of open aortic repair. The prevalence of POCD at discharge (62%, 95% CI 51 to 72) was higher than previous reports among non-cardiac surgical patients but resolved by three months in the majority of patients. It would appear that in-hospital delirium predicted fewer than half of the cases of POCD noted at hospital discharge and that the APOE-ε4 genotype was not associated with either delirium or POCD in our population.
Given the frequency of both delirium and POCD in this high-risk population, one might assume that they are part of a similar spectrum of disease. Foregoing research has identified a number of risk factors common to both delirium and POCD. Variables consistently associated with delirium included preexisting cognitive impairment, psychopathologic symptoms, psychotropic drug use, number of medical comorbidities, elevated blood urea nitrogen, nursing home residence, and functional impairment.4 Monk and the ISPOCD have identified similar lists of predictors for POCD, including increasing age, years of education, ASA physical status, perioperative complications, and previous cerebrovascular accident.10 In our study, the identification of an association between delirium and POCD at hospital discharge (OR 2.86; 95% CI 0.99 to 8.27) would seem to suggest a common mechanism; this assumption, however, cannot be confirmed by our data. It is important to note that well over half of the patients experiencing POCD did not have a preceding episode of delirium, and a variety of confounding risk factors might drive the association identified. Future research evaluating both the clinical predictors and biology of cognitive impairment is required if the mechanisms of delirium and POCD are to be understood.
The APOE-ε4 genotype has been associated consistently with a threefold or greater increase in the risk of Alzheimer’s dementia,21 suggesting a potential biological role in perioperative cognitive disorders. Early studies indicated that the APOE-ε4 genotype was associated with both the incidence and severity of cognitive impairment26 and declines in MMSE scores22 in patients undergoing cardiac surgery. Subsequent studies in cardiac23,24 and non-cardiac25,26 surgery failed to confirm an association between APOE-ε4 and POCD. Similarly, APOE-ε4 has also been associated with the incidence and duration of delirium in non-cardiac surgery27 and critical care patients,28 while these relationships could not be identified following cardiac surgery29 and hip surgery.30 Our results suggest that the APOE-ε4 genotype was not a dominant predictor of either delirium or POCD; we cannot, however, rule out a facilitating role of APOE-ε4-mediated changes in cholinergic neurotransmission in the pathogenesis of these cognitive disorders. Trends noted in the associations between APOE-ε4 and both short- and long-term POCD suggest that large carefully controlled trials should be considered to fully explore the role of this genotype in perioperative cognitive outcome. It should be noted, however, that a trial with 80% power to detect a doubling of the rate of long-term POCD from 5-10% would require a cohort of nearly 1,100 patients, assuming a 25% prevalence of APOE-ε4 in the population. In the absence of a clear biological mechanism predicting delirium or POCD, the clinician must rely on predictors of clinical risk. Once patients at risk have been identified, what steps should clinicians take to prevent these cognitive complications after surgery?
To date, few interventions have been successful at preventing either delirium or POCD. Multidisciplinary care focusing on the unique concerns of the elderly31 and low-dose haloperidol32 have been shown to decrease the incidence and severity of delirium, respectively. Intravenous lidocaine33 and donepezil34 have proven unsuccessful at reducing POCD. Randomized trials comparing regional and general anesthesia did not identify a benefit of regional anesthesia on either delirium or POCD.35 Cohort studies have identified associations between interleukins and an increased risk of delirium and statin use with its reduction.36 Further research evaluating the relationship between inflammation and cognitive outcome is required.
The present study has a number of limitations. First, we had powered our study to detect effects of a similar magnitude (OR of 3 or more) as those seen between APOE-ε4 and dementia15 as well as those seen for clinical predictors, postoperative cognitive changes (e.g., advanced age),5 and previous cerebrovascular accident.10 While similar to other trials, our selection of this large effect in the sample estimation may have been too conservative and may have effectively decreased power to detect a smaller association. Our observed rates of delirium (36%) and effect size (OR 2.6) were less than the 40% rate we had anticipated,2 presenting another potential type II error. Similarly, our control event rate was derived from vascular surgery trials in which the APOE genotype was an unknown mix of both APOE-ε4 and other genotypes. These blended populations may have artificially increased the event rate assumed in our estimate, subsequently decreasing power to detect an APOE-ε4 effect. Our population also reported a lower rate of APOE-ε4 carriers (24%) than existing health data of the population from our region (35%) would indicate. This lower prevalence of the genotype in question in our study could represent a simple sampling error, for instance, an under representation of women and our exclusion of patients with dementia, both of whom are more frequent carriers of APOE-ε4. Second, while a statistically significant association between delirium and POCD was found in this study, a slightly larger trial designed with a total of 138 patients would have been required to yield 80% power to detect the smaller increase in POCD observed in those with preceding delirium. Consideration was given to increasing enrollment, but a move to endovascular aortic repair at The Ottawa Hospital severely limited recruitment in the latter stages of the trial and precluded the practical expansion of our sample. Third, our study was powered to assess only the primary relationships between delirium and POCD, and we had an insufficient number of events for accurate multivariable modelling of multiple risk factors.37 Fourth, our study did not rigidly control anesthetic techniques and drugs in the perioperative period, permitting significant discretion in perioperative care. It is reassuring that we found no significant relationship between opioid consumption, use of psychoactive drugs, or other elements of perioperative care in either of our cognitive outcomes. Lastly, despite the significant physical stresses of open aortic repair and a 60% incidence of POCD at discharge, we noted no significant impact of either surgery or cognitive dysfunction on physical or mental quality of life. Confidence intervals for quality of life measures at discharge included mean preoperative scores for the study population. In those patients with and without cognitive problems in the perioperative period, mental component scores on the SF-12 were comparable with age-matched persons in the general population. These findings contrast with those of Newman and Monk who identified significant associations between POCD and quality of life. It is possible that patients more significantly impaired by their surgery may have chosen not to return for further testing. Furthermore, the use of the SF12, rather than a more detailed instrument like the SF36 or the EuroQoL, might account, in part, for our failure to corroborate these earlier findings.
In conclusion, the results of this study indicate that both delirium and POCD frequently complicated the postoperative course of patients undergoing open aortic surgery. Fortunately, these “in-hospital” events bore little direct impact on health and mental quality of life, and few patients experienced cognitive changes lasting three months beyond discharge. A summary of the available evidence would suggest that older less educated patients with poor functional capacity who have dementia, depression, or previous cerebrovascular accidents should be considered at high risk for cognitive complications. This study lacks the power to confirm the presence or absence of an association between early postoperative changes and the APOE genotype. Future research is required to identify means to prevent and treat these common postoperative complications.
References
American Psychitric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM IV, 4th ed, text revision. Washington, DC: American Psychiatric Association; 2000.
Dyer CB, Ashton CM, Teasdale TA. Postoperative delirium. A review of 80 primary data-collection studies. Arch Intern Med 1995; 155: 461-5.
Inouye SK. Delirium in older persons. N Engl J Med 2006; 354: 1157-65.
Dasgupta M, Dumbrell AC. Preoperative risk assessment for delirium after noncardiac surgery: a systematic review. J Am Geriatr Soc 2006; 54: 1578-89.
Marcantonio ER, Goldman L, Mangione CM, et al. A clinical prediction rule for delirium after elective noncardiac surgery. JAMA 1994; 271: 134-9.
McCusker J, Cole MG, Dendukuri N, Belzile E. Does delirium increase hospital stay? J Am Geriatr Soc 2003; 51: 1539-46.
Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med 1998; 13: 234-42.
McCusker J, Cole M, Abrahamowicz M, Primeau F, Belzile E. Delirium predicts 12-month mortality. Arch Intern Med 2002; 162: 457-63.
Rasmussen LS, Larsen K, Houx P, Skovgaard LT, Hanning CD, Moller JT; ISPOCD group. The International Study of Postoperative Cognitive Dysfunction. The assessment of postoperative cognitive function. Acta Anaesthesiol Scand 2001; 45: 275-89.
Monk TG, Weldon BC, Garvan CW, et al. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology 2008; 108: 18-30.
Steinmetz J, Christensen KB, Lund T, Lohse N, Rasmussen LS; ISPOCD Group. Long-term consequences of postoperative cognitive dysfunction. Anesthesiology 2009; 110: 548-55.
Trzepacz PT. Is there a final common neural pathway in delirium? Focus on acetylcholine and dopamine. Semin Clin Neuropsychiatry 2000; 5: 132-48.
Grantham C, Geerts H. The rationale behind cholinergic drug treatment for dementia related to cerebrovascular disease. J Neurol Sci 2002; 203-204: 131-6.
Poirier J. Apolipoprotein E and cholesterol metabolism in the pathogenesis and treatment of Alzheimer’s disease. Trends Mol Med 2003; 9: 94-101.
Hsiung GY, Sadovnick AD, Feldman H. Apolipoprotein E epsilon4 genotype as a risk factor for cognitive decline and dementia: data from the Canadian Study of Health and Aging. CMAJ 2004; 171: 863-7.
Lahoz C, Schaefer EJ, Cupples LA, et al. Apolipoprotein E genotype and cardiovascular disease in the Framingham Heart Study. Atherosclerosis 2001; 154: 529-37.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453-7.
Murkin JM, Newman SP, Stump DA, Blumenthal JA. Statement of consensus on assessment of neurobehavioral outcomes after cardiac surgery. Ann Thorac Surg 1995; 59: 1289-95.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990; 113: 941-8.
Poirier J. Apolipoprotein E in animal models of CNS injury and in Alzheimer’s disease. Trends Neurosci 1994; 17: 525-30.
Bertram L, Tanzi RE. Thirty years of Alzheimer’s disease genetics: the implications of systematic meta-analyses. Nat Rev Neurosci 2008; 9: 768-78.
Lelis RG, Krieger JE, Pereira AC, et al. Apolipoprotein E4 genotype increases the risk of postoperative cognitive dysfunction in patients undergoing coronary artery bypass graft surgery. J Cardiovasc Surg (Torino) 2006; 47: 451-6.
Silbert BS, Evered LA, Scott DA, Cowie TF. The apolipoprotein E epsilon4 allele is not associated with cognitive dysfunction in cardiac surgery. Ann Thorac Surg 2008; 86: 841-7.
Steed L, Kong R, Stygall J, Acharya J, Bolla M, Harrison MJ, et al. The role of apolipoprotein E in cognitive decline after cardiac operation. Ann Thorac Surg 2001; 71: 823-6.
Abildstrom H, Rasmussen LS, Rentowl P, et al. Cognitive dysfunction 1-2 years after non-cardiac surgery in the elderly. ISPOCD group. International Study of Post-Operative Cognitive Dysfunction. Acta Anaesthesiol Scand 2000; 44: 1246-51.
Abildstrom H, Christiansen M, Siersma VD, Rasmussen LS; ISPOCD2 Investigators. Apolipoprotein E genotype and cognitive dysfunction after noncardiac surgery. Anesthesiology 2004; 101: 855-61.
Leung JM, Sands LP, Wang Y, et al. Apolipoprotein E e4 allele increases the risk of early postoperative delirium in older patients undergoing noncardiac surgery. Anesthesiology 2007; 107: 406-11.
Ely EW, Girard TD, Shintani AK, et al. Apolipoprotein E4 polymorphism as a genetic predisposition to delirium in critically ill patients. Crit Care Med 2007; 35: 112-7.
Tagarakis GI, Tsolaki-Tagaraki F, Tsolaki M, Diegeler A, Tsilimingas NB, Papassotiropoulos A. The role of apolipoprotein E in cognitive decline and delirium after bypass heart operations. Am J Alzheimers Dis Other Demen 2007; 22: 223-8.
van Munster BC, Korevaar JC, de Rooij SE, Levi M, Zwinderman AH. The association between delirium and the apolipoprotein E epsilon4 allele in the elderly. Psychiatr Genet 2007; 17: 261-6.
Siddiqi N, Stockdale R, Britton AM, Holmes J. Interventions for preventing delirium in hospitalised patients. Cochrane Database Syst Rev 2007; (2): CD005563.
Kalisvaart KJ, de Jonghe JF, Bogaards MJ, et al. Haloperidol prophylaxis for elderly hip-surgery patients at risk for delirium: a randomized placebo-controlled study. J Am Geriatr Soc 2005; 53: 1658-66.
Mathew JP, Mackensen GB, Phillips-Bute B, et al. Randomized, double-blinded, placebo controlled study of neuroprotection with lidocaine in cardiac surgery. Stroke 2009; 40: 880-7.
Doraiswamy PM, Babyak MA, Hennig T, et al. Donepezil for cognitive decline following coronary artery bypass surgery: a pilot randomized controlled trial. Psychopharmacol Bull 2007; 40: 54-62.
Wu CL, Hsu W, Richman JM, Raja SN. Postoperative cognitive function as an outcome of regional anesthesia and analgesia. Reg Anesth Pain Med 2004; 29: 257-68.
Katznelson R, Djaiani GN, Borger MA, Friedman Z, Abbey SE, Fedorko L, et al. Preoperative use of statins is associated with reduced early delirium rates after cardiac surgery. Anesthesiology 2009; 110: 67-73.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996; 49: 1373-9.
Funding
This work was funded by the Canadian Anesthesiologists’ Society’s Dr. R.A. Gordon Clinical Research Award (2005) and the University of Ottawa, Department of Anesthesiology’s Chair’s Research Fund. Dr. Bryson was supported by the Ottawa Hospital Anesthesia Alternate Funds Association.
Conflicts of interests
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is accompanied by an editorial. Please see Can J Anesth 2011; 58(3).
Rights and permissions
About this article
Cite this article
Bryson, G.L., Wyand, A., Wozny, D. et al. A prospective cohort study evaluating associations among delirium, postoperative cognitive dysfunction, and apolipoprotein E genotype following open aortic repair. Can J Anesth/J Can Anesth 58, 246–255 (2011). https://doi.org/10.1007/s12630-010-9446-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-010-9446-6