Abstract
Purpose of Review
In recent years, breast cancer-related lymphedema (BCRL), which affects one in five patients treated for breast cancer (BC), has garnered increasing interest by clinicians and researchers as BC survival rates improve and survivorship issues become increasingly imperative. This review represents an overview of the literature for BCRL risk factors, such as radiation therapy (RT), screening, and treatment.
Recent Findings
Risk factors with strong evidence include axillary surgery, regional lymph node radiation, elevated body mass index, cellulitis, and subclinical edema. Neoadjuvant and taxane-based chemotherapy, trastuzumab, breast reconstruction, RT field design, and genetic susceptibility are emerging as potentially influencing BCRL risk.
Summary
Comprehensive BCRL care necessitates a multidisciplinary team that coordinates BC treatment, educates patients, and vigilantly screens them throughout survivorship. Providers should be knowledgeable of BCRL risk factors and individualize patient education. Universal diagnostic criteria using relative change from baseline and consistently incorporating baseline measurements are imperative.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As breast cancer survival rates improve, quality of life and survivorship issues have become increasingly important. Breast cancer-related lymphedema (BCRL), a chronic and feared sequela of breast cancer (BC) treatment, has garnered research focus. It is imperative that healthcare professionals caring for patients throughout and beyond BC treatment are knowledgeable about BCRL, in order to educate, diagnose, and refer patients appropriately. This review summarizes BCRL risk factors, screening, treatment, and the role of radiation therapy (RT) in BCRL development.
Definition
Lymphedema is defined as the accumulation of protein-dense fluid in the interstitial space of the limb, breast, and/or trunk on the side of BC treatment as a result of disruption of the lymphatic vasculature and subsequent drainage impairment [1]. Such pathological buildup can generate not only physical symptoms of swelling, heaviness, tightness, pain, tingling, and impaired movement but can also cause psychological consequences such as stress, anxiety, and depression [2, 3].
Incidence
BCRL incidence is not well established, mainly due to the lack of a universally accepted definition and well-defined diagnostic criteria. Its calculated incidence reportedly ranges from 5 to 50% [4•, 5, 6]. A recent comprehensive meta-analysis determined the incidence as 21.4%, making it one of the most common and impactful chronic conditions following BC treatment [4•]. This is even more relevant given that the risk of BCRL is a lifelong threat for patients treated for BC.
Diagnostic Criteria
Unfortunately, there is no consensus on specific diagnostic criteria for BCRL. Lymphedema diagnosis should be established clinically by a certified lymphedema therapist (CLT) or healthcare provider familiar with BCRL and should include objective measurements of the affected region, subjective symptoms using a validated outcome measure, and clinical examination. There are several measurement tools available to help screen for BCRL; however, the BCRL criteria vary within tools and across institutions. Inconsistencies in quantification methods may hamper consistent and accurate calculations of BCRL incidence and prevalence, considering that the methods are not interchangeable [7,8,9].
Measurement Tools
Volumetric measurement methods include water displacement, circumferential tape measure, and perometry, and another measurement tool includes bioimpedance spectroscopy (BIS). The perometer and BIS tools are pictured in Fig. 1.
Water displacement was used historically and involves submerging the limb in a container of water, with the immersed limb’s volume equal to that of the water displaced. While reliable, valid, and accurate [7], the process is cumbersome and time-consuming as the water container requires strict hygienic emptying and sterilizing between patients. This limits the clinical utility of this practice, which has fallen out of use.
Circumferential measurements are taken with a tape measure every 4 or 10 cm along the length of the upper limb or from anatomical landmarks [10] and should be converted into arm volumes using the truncated cone formula, via commercially available software programs [11]. The tape measure is easy, inexpensive, and convenient for office use. It is reliable for quantifying arm volume change [7]; however, the measuring process is user and experience dependent, can take considerable time, and may lead to inter-rater variability in the setting of long-term BCRL screening and follow-ups [12].
The perometer is comprised of a frame containing infrared light receivers that is moved along the patient’s arm while abducted to 90 degrees (Fig. 1a). The arm’s circumference is calculated every 4.7 mm and its volume is automatically computed using the truncated cone method. Three measurements of each arm are taken, and the median limb volume is calculated. Perometry is a reliable, valid, diagnostically accurate, and efficient tool to quantify arm volumes with reproducible results [7, 13•, 14, 15]. Moreover, its high sensitivity allows for detecting subclinical edema, a known BCRL risk factor [16••, 17]. Nevertheless, the perometer is expensive and requires devoted clinical space, limiting its accessibility.
BIS calculates impedance ratios by passing an electrical current through the body and measuring resistance to flow. The resulting L-Dex score, which compares the affected extremity to the unaffected extremity, reflects the amount of extracellular fluid in the affected extremity. An L-Dex score change of ≥ 10 from preoperative baseline is typically considered diagnostic of lymphedema [7, 18], but a value of > 7.1 has been cited in the literature to discriminate between patients with and without BCRL [19•, 20]. A presurgical baseline is required, as some patients have abnormal readings preoperatively [19•, 21•]. BIS generates quick results with high reliability in detecting established BCRL [7, 19•, 20] and a newer machine (Fig. 1b) can also be used in patients who underwent bilateral breast surgeries [22]. Limitations include its costliness, size, and inability to detect later-stage, fat-dominant lymphedema [19•, 20, 23]. Moreover, its ability to identify early-stage subclinical edema is not well supported [23, 24, 25••]. Bundred et al.’s recent multi-center cohort study followed patients with preoperative baselines for a median of 36 months and compared the accuracy of BIS and volumetric measurement tools to diagnose BCRL, defined as relative arm volume increase (RAVI) of > 10% [25••]. The cohort’s 2-year lymphedema incidence using L-Dex ≥ 10 criterion was 45.2%, which is significantly higher than both the 22.4% rate detected with RAVI > 10% and 24.5% of patients that required compression sleeves. While there was a moderate correlation between BIS and RAVI at 6 months, long-term data revealed BIS overdiagnosed BCRL with a 12% false-positive rate, and RAVI correlated better with symptoms and quality of life. Conclusions drawn ascertain that BIS should not be used in isolation for BCRL screening and diagnosis [25••, 26].
Relative vs. Absolute Change
Volumetric change may be described as absolute (i.e., percent volume difference between the affected and unaffected arms) or relative (i.e., percent volume difference from preoperative baseline). Lymphedema’s definition varies widely. Several absolute thresholds have been used in the literature, including an increase of 2 cm in tape measure circumference or 200 ml in limb volume. However, they constitute flawed, unreliable BCRL definitions [16••, 17, 19•, 21•, 27, 28••, 29], as they do not account for the natural asymmetry between a patient’s arms at preoperative baseline, leading to misdiagnosis up to 50% of the time. This was demonstrated in Sun et al.’s prospective screening study. They found a natural asymmetry between a patient’s arms of ≥ 5% in 28.3% of the subjects and a difference of ≥ 10% in 2.9% of patients [28••]. To mimic cases without a baseline, the investigators substituted early postoperative measurements as pseudo-baselines in their analysis. With pseudo-baselines, BCRL was underdiagnosed and overdiagnosed in 50.0% and 54.8% of cases, respectively. Preoperative baselines are also essential in BIS measurements [19•, 21•]. Regardless of the tool used, a preoperative baseline is crucial for accurate BCRL screening and diagnosis.
The Lymphedema Research Program at Massachusetts General Hospital (MGH) developed the relative volume change (RVC) and the weight-adjusted volume change (WAC) formulae for patients undergoing unilateral and bilateral BC surgery, respectively [30, 31]. The RVC equation gauges volume changes of the affected arm in relation to the unaffected arm (A2 and U2, respectively) compared to their baselines (A1 and U1, respectively), whereby RVC = [(A2*U1)/(U2*A1) − 1] [30]. The WAC formula considers the two limbs independently in the setting of postoperative weight (W2) fluctuations in comparison to the weight at baseline (W1), whereby WAC = [(A2*W1)/(W2*A1) − 1] [31]. A common and accurate definition of lymphedema diagnosis is a relative increase of ≥ 10% in arm volume from baseline [9, 19•, 23, 28••, 29,30,31, 32•].
Symptoms
Quantification of arm swelling constitutes only part of lymphedema diagnosis, as it should incorporate BCRL-related symptoms reported by the patient. The role of symptoms is not clearly delineated, as studies have not shown a direct relation between symptoms’ severity and the magnitude of lymphedema [33, 34]. However, patient-reported symptoms of heaviness, current swelling, and numbness could be indicators of BCRL [33]. The presence of symptoms before lymphedema onset was associated with a higher risk of subsequent BCRL [34, 35]. Lymphedema-specific, validated questionnaires [33, 36,37,38] are available to help guide screening, diagnosis, and treatment.
Clinical Exam
To date, there has not been a reliable, valid, quantifiable method to evaluate BCRL clinically. The Cancer-Related Lymphedema of the Upper Extremity (CLUE) tool is a standardized BCRL clinical examination across three anatomical regions (digits/hand, wrist/forearm, elbow/upper arm) and four subscores (obscuration of anatomical architecture, deviation from normal anatomic contour, tissue texture, edema) [39]. It was recently developed and validated for use in research and clinical care.
BCRL Screening
Although a screening-based model is strongly supported in the literature and recommended [9, 10, 23, 28••, 40•, 41••, 42••, 43,44,45,46,47] over an impairment-based model, this is not universally applied. Prospective BCRL screening is longitudinal and incorporates objective measurements, including preoperative baseline measured via a valid, reliable, and feasible tool; a validated, patient-reported outcome measure; and multidisciplinary coordination to identify at-risk patients, ensure comprehensive patient education, and refer as needed to a CLT [41••].
The MGH Lymphedema Research Program initiated such a screening program in 2005, consisting of a multidisciplinary team of medical, surgical and radiation oncologists, CLTs, and nurses [41••]. Patients treated for BC are screened prospectively for BCRL throughout treatment and follow-ups using perometry measurements, patient-reported outcome measures, and clinical examination as indicated. Patients demonstrating elevated measurements or symptoms are routinely referred for CLT evaluation [41••].
Timing of BCRL after BC Treatment
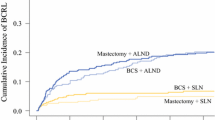
In a recent prospective study, McDuff et al. studied the time course of lymphedema in a cohort of 2171 patients treated for BC. BCRL was found to most likely occur within 12–30 months after BC surgery [42••]. However, this timeframe differed depending on axillary surgery and nodal irradiation. Patients who underwent axillary lymph node dissection (ALND) without regional lymph node radiation (RLNR) had the earliest and highest risk of developing lymphedema, which peaked in the first 6–12 months. Patients who received ALND+RLNR had later onset BCRL, with the hazard ratio (HR) highest at 18–24 months. BCRL development occurred later in those receiving sentinel lymph node biopsy (SLNB) and RLNR, peaking between 36 and 48 months. Moreover, this cohort’s estimated cumulative incidence was 7.1% at 2 years and 13.7% at 5 years. Given this data and the fact that BCRL risk never decreases to zero, BCRL screening should last beyond 2 years, for at least 3–4 years.
Risk Factors
In the literature, there are several well-established risk factors as well as other potentially emerging risk factors, which are all reviewed below.
Axillary Surgery
Axillary surgery has been established as a risk factor for BCRL [4, 6, 8, 48, 49••, 50,51,52,53, 54•, 55•]. Although both ALND and SLNB put patients at risk for lymphedema by interfering with the lymphatic system through lymph node (LN) removal, ALND carries a notably higher risk. A meta-analysis has revealed that BCRL incidence in patients undergoing ALND was 19.9% (95% CI: 13.5–28.2), almost quadruple the rate in patients who had SLNB (5.6%) [4•]. This may be explained by considerably more tissue disruption and more LNs removed in ALND [48, 49••, 50, 51]. Kilbreath et al. noted that the incidence rate of BCRL among patients who have had more than five LNs removed was almost six times that of patients with less than five LNs removed (18.2% vs. 3.3%, respectively) [49••]. Another study found that a cutoff of > 10 LNs removed in ALND significantly raised BCRL incidence from 6 to 27% compared to ALND of ≤ 10 nodes [50]. However, both studies quantified BCRL without baseline preoperative measurements [49••, 50]. It is hypothesized that increased BCRL risk with a higher number of LNs removed reflects the type/extent of axillary surgery.
Body Mass Index at Breast Cancer Diagnosis and Weight Fluctuations
Obesity at BC diagnosis, defined as body mass index (BMI) ≥ 30 kg/m2, increases BCRL risk [25••, 32•, 51, 55•, 56,57,58, 59••]. Ridner and colleagues prospectively screened patients for lymphedema and demonstrated that high BMI at BC diagnosis multiplies the patient’s risk of ensuing lymphedema by up to 3.6 times as compared to a baseline BMI ≤ 30 (odds ratio (OR) 3.59, 95% CI: 1.42–9.04) [56]. Similarly, Jammallo et al. found that a BMI ≥ 30 was an independent predictor of BCRL and that a weight gain or loss of ten pounds or more per month after surgery was correlated with greater lymphedema risk (HR 1.97, P < 0.0001) [58]. A 2019 clinical trial randomized patients to a home-based resistance exercise program, a weight loss program, a combination of the two, or to the control group. Weight loss did not affect BCRL outcome [60••, 61]. Ongoing research should be directed towards understanding the effects of weight fluctuations and developing integrative clinical interventions to achieve and/or maintain ideal body weight.
Cellulitis and Seroma
Ipsilateral cellulitis and seroma are each independent BCRL risk factors [32•, 49••, 62••, 63•, 64]. A recent review by Asdourian et al. found that current and previous ipsilateral skin infections occurring in the affected arm were significantly associated with increased arm volume [62••]. A 2017 large retrospective study demonstrated that postoperative seroma was an independent risk factor, almost doubling BCRL risk (HR 1.92; 95% CI: 1.30–2.85) [64].
Subclinical Lymphedema
Subclinical edema, which is increased arm volume from the baseline that does not qualify as clinical lymphedema (i.e., visible on clinical exam, symptoms reported), is a risk factor for BCRL [32•, 49••, 51]. Regular arm measurements are necessary to detect subclinical edema, reinforcing the need for routine BCRL screening. By prospectively screening 1173 patients using perometry, Specht et al. found that increases in arm volume within the first 3 months post-surgery, by 3 to < 5% and 5 to < 10%, respectively, were significantly correlated with amplified BCRL risk (HR 2.52, P = 0.007; HR 3.24 P < 0.0001, respectively) [32•]. Arm volume increases of 5 to < 10% occurring after 3 postoperative months was associated with a significant risk of progression to RVC ≥ 10% (HR 2.97, P < 0.0001) [32•].
Regional Lymph Node Radiation
RT is a cornerstone of BC multidisciplinary treatment, and RLNR is considered an iatrogenic risk factor for BCRL [6, 49••, 51,52,53, 65, 66••, 67•, 68•, 69, 70•]. A prospective cohort study on patients with preoperative baseline showed that receiving RLNR significantly increases lymphedema risk (HR 1.70, P = 0.025), compared to only breast/chest wall radiation [51]. The cohort of patients who received no radiation or breast/chest wall radiation alone had 3.0% and 3.1% 2-year cumulative BCRL incidence, respectively. This is in contrast to a significantly higher 21.9% and 21.1% in patients treated with radiotherapy to supraclavicular (SCV) nodes with and without posterior axillary boost, respectively. However, these BCRL rates with RLNR are not stratified by type of axillary surgery. Shaitelman et al. found that RLNR addition to breast/chest wall radiation was associated with a higher BCRL incidence (OR 2.85; 95% CI 1.24–6.55). The combination ALND+RLNR was associated with an 18.2% incidence, a significantly higher rate than the 9.4% seen with ALND without RLNR. However, among patients treated with SLNB, the association of lymphedema with RLNR was not significant (95% CI 0.54–4.66) [65]. Naoum et al. prospectively evaluated 1815 patients in a BCRL screening program to evaluate the impact of axillary surgery and RLNR on local tumor control and BCRL (defined as RVC ≥ 10% increase arising ≥ 3 months postoperatively). The 5-year cumulative BCRL incidence rates were 30.1%, 24.9%, 10.7%, and 8.0% for ALND+RLNR, ALND alone, SLNB+RLNR, and SLNB alone, respectively. There was no significant local tumor control difference between SLNB+RLNR and ALND alone groups. Multivariable analysis adjusted for BMI and breast surgery type revealed there was no significant difference between SLNB alone and SLNB+RLNR groups regarding BCRL rates. Additionally, there was no significant BCRL rates difference between ALND alone and ALND+RLNR groups. However, a significant BCRL difference between SLNB+RLNR and ALND alone groups was detected. The authors concluded that while RLNR increases BCRL risk, the main contributing factor to BCRL risk is the type of axillary surgery received [67•].
In a large prospective cohort study, Chandra et al. showed that the SCV field lateral border, SCV dosage (5000 vs. 5040 cGy), beam energy (6-MV vs. 10-MV), tangent type (normal vs. wide), and fraction size (180 vs 200 cGy) do not correlate with BCRL [68•]. Conversely, Gross et al. noted that the extent of the SCV field’s lateral border significantly affected BCRL risk [69]. Furthermore, irradiating the anterior-lateral thoracic vessel juncture, with a radiation dose < 38.6 Gy, reportedly significantly decreased BCRL incidence (HR 0.13; P < .001) [53]. However, they defined BCRL as an absolute arm circumference change of 2 or 2.5 cm, failing to incorporate preoperative measurements. Further research is required to delineate the role of these findings with more accurate BCRL definitions.
Emerging BCRL Risk Factors
Chemotherapy
The association between chemotherapy and BCRL risk is not well defined. In some studies, chemotherapy has been reported to be significantly associated with lymphedema [4•, 49••, 50, 53, 59••, 70•, 71,72,73], whereas no such statistical significance was found in other studies [42••, 54•, 55•, 74]. A 2019 study of 486 patients treated for BC identified that a longer duration of neoadjuvant chemotherapy (NAC), namely ≥ 144 days, is associated with higher lymphedema incidence than in patients treated with NAC < 144 days [59••]. The type of chemotherapy regimen (i.e., anthracycline based, taxane based, or both) was not associated with lymphedema. BCRL was defined as a volume increase of ≥ 10% compared with baseline and/or the contralateral limb, limiting BCRL accuracy for those without baseline. The authors postulated that the higher BCRL rate observed could be related to the total chemotherapy dose or to delays due to toxicity.
Swaroop and colleagues prospectively screened 1121 patients treated for BC for lymphedema, defined as RVC ≥ 10% from preoperative baseline, and found that taxane-based chemotherapy was not associated with increased BCRL risk when compared to no chemotherapy and non-taxane chemotherapy (P = 0.62; P = 0.40, respectively) [54•]. However, taxane-based chemotherapy has been cited to correlate with an increased risk of fluid retention and lymphedema [49••, 53, 70•, 71, 72]. Kilbreath et al. showed that arm swelling at 6 and 12 months were both significantly associated with taxane-based chemotherapy, each representing independent risk factors for BCRL, established using BIS [49••]. This paper carried significant limitations in that baseline was not incorporated and circumference difference was used to measure swelling.
Interestingly, a 2019 study showed a tendency towards significance between trastuzumab intake and breast lymphedema (P = 0.09) [74]. In a retrospective analysis, Invernizzi et al. found that receipt vs. non-receipt of trastuzumab was significantly associated with almost triple the risk for BCRL (HR 2.7, 95% CI 1.31–5.55) [73]. BCRL was defined by circumferential difference without preoperative measurements, and the number of patients receiving trastuzumab was small (30 of n = 368, 8.15%), calling for more robust evidence.
Breast Reconstruction
The link between breast reconstruction after mastectomy and BCRL risk is emerging [55•, 75,76,77,78]. Miller et al. prospectively screened BC patients with preoperative measurements for BCRL. Their multivariate analysis revealed that immediate implant or expander-based reconstruction, but not immediate autologous reconstruction, was associated with reduced lymphedema risk compared to mastectomy alone (HR 0.432; P < 0.0001, HR 0.706; P = 0.2151, respectively) [55•]. A 2018 meta-analysis concluded that breast reconstruction was correlated with significantly lower odds of BCRL (P < 0.001), when compared to mastectomy and breast-conserving surgery. No statistically significant difference was found between an implant-based and autologous reconstruction [78]. This association may be due to tissue adhesion and fibrosis occurring without reconstruction, obstructing lymphatic flow [77]. Autologous reconstruction has been hypothesized to reduce postoperative fibrosis and subsequent obstruction [77], and implant reconstruction could possibly induce tissue ischemia stimulating angiogenesis and lymphatic regeneration [76]. These underlying mechanism theories remain nondefinitive. Furthermore, there was significant heterogeneity in the included studies’ study design and BCRL definitions [78].
Medical Procedures on the Ipsilateral Arm and Lifestyle Factors
Receiving medical procedures on the ipsilateral arm to BC as well as lifestyle factors that have been studied have not been associated with a statistically significant increase in arm volume [49••, 53, 62••, 63•, 79].
A 2019 retrospective study showed that port-sidedness, whether it was ipsilateral or contralateral to BC location and surgery, was not associated with BCRL [79]. Other medical procedures including blood draws, injections, blood pressure readings, and lifestyle factors such as air travel were not significantly associated with increased arm volume [53, 62••, 63•]. The lack of evidence for the roles of these factors in BCRL risk should be discussed with patients. Abiding to strict precautionary measures may add a significant burden on patients who have endured BC treatment [62••]. Personalization of BCRL management and risk stratification should guide BCRL risk assessment and patient education.
Genetic Susceptibility
The abovementioned risk factors can only partially account for a BC patient’s BCRL risk, as some women with these risk factors do not develop secondary lymphedema whereas others do. Genetic predisposition has also been proposed to affect BCRL risk. Genetic variations, such as single-nucleic polymorphisms (SNPs), in genes involved in inflammatory pathways, can modify a patient’s physiologic reactions to trauma and therefore their vulnerability for subsequent lymphedema. A recent systemic review identified 18 possible genes variations linked to BCRL in women who had received BC treatment, with some of the genes shown to be involved in primary lymphedema pathogenesis [80]. One of the included studies concluded that certain genotypic SNPs were associated, not with limb volume increase, but rather with clusters of eight or more symptoms, highlighting the importance of symptoms inclusion in lymphedema definition [81]. While promising, these findings are nevertheless preliminary, based on studies with significant limitations such as small samples and heterogenous lymphedema definitions [80].
BCRL Management
Complete Decongestive Therapy
The standard of care for BCRL treatment is complete decongestive therapy (CDT) under the direction of a CLT. CDT is two staged and may include the following: exercise, manual lymphatic drainage (MLD), compression bandaging, and patient education [82,83,84,85,86, 87••, 88••]. The first phase is reductive CDT, wherein frequent appointments with a CLT aim to reduce limb swelling until stabilization. The second phase consists of maintenance including self-MLD, maintenance compression, skin care, and exercise. Not all components are necessarily used in every patient as the regime should be individualized.
Exercise is necessary for patients treated for BC who are at risk for or have developed BCRL. It has been established that exercise neither causes nor worsens BCRL [86, 87••, 88••, 89••, 90,91,92] and recommendations have encouraged patients to engage in exercise safely and progressively under supervision [90,91,92]. A randomized controlled trial in women with BCRL and women at risk for BCRL showed no differences in lymphedema risk and arm volumes between the controls and those assigned to a progressive weight lifting program [83, 84]. Less severe symptoms (P = 0.03) and fewer lymphedema exacerbations at 1 year were noted in the intervention group (14% vs. 29%, P = 0.04) [83]. Exercise guidelines specific to patients treated for BC are available [88••, 89••, 90,91,92] and should be followed closely to avoid injury.
Lymphatic Surgery
There are two types of surgical procedures that constitute second-line therapy for BCRL [93, 94]. Debulking surgeries entail removing edematous or fibrotic excess volume by liposuction in patients with non-pitting or fat-dominant edema [93,94,95]. Overall arm volume reduction has been reported with this approach [95, 96]; however, it requires consistent use of compression garments for maintenance [93, 96]. Physiologic procedures target the underlying pathology of BCRL by restoring lymphatic fluid flow [93, 97]. They involve harvesting LNs and connecting their vasculature to the axilla’s lymphatics (i.e., vascularized LN transplant) or constructing anastomoses between the vascular and lymphatic systems (i.e., lymphovenous anastomosis). They work best in patients with pitting edema and have led to reductions in BCRL volume [93, 97, 98]. Both surgical interventions offer effective results, and the literature continues to evolve in this area.
Lymphatic Surgery and BCRL Prevention
Recently, preventive surgical approaches have been developed to locate susceptible parts of the arm’s lymphatic system and avoid damaging them during axillary surgery.
Axillary reverse mapping (ARM) is a surgical technique wherein a tracer is injected to identify LNs draining the arm to avoid their removal. ARM has been associated with lower BCRL rates [99, 100]. A 2017 systematic review found that lymphedema incidence was lower after SLNB and ARM than after SLNB alone. The authors highlighted the varied methods and timing of lymphedema diagnosis and the need for well-designed trials to better establish the efficacy of ARM and, given the possible overlap between axillary and upper extremity LN, the necessity of assessing oncologic safety [101].
Another surgical preventive method garnering attention is the lymphatic microsurgical preventative healing approach (LYMPHA), wherein an anastomosis is created between the lymphatic and venous systems during axillary surgery. This technique has shown favorable results and an association with lower lymphedema rates [102].
Drug Therapy
There are current ongoing studies investigating the potential role of drug therapy on chronic lymphedema. Pilot data examining tissue changes has shown that patients with lymphedema receiving the anti-inflammatory drug ketoprofen demonstrated reduced skin thickness, improved histopathology, and decreased plasma granulocyte CSF (G-CSF) expression [103]. This group is currently recruiting to an observational prospective cohort study of patients with lymphedema treated with ketoprofen. This study, incorporating limb volume changes, looks to further understand treatment response to ketoprofen [104]. Drug therapy represents for the moment a developing but hopeful endeavor in BCRL treatment.
Conclusion
Lymphedema is a devastating condition with significant consequences for patients who have already endured BC treatment. Due to high BC incidence and the rising survival after treatment, BCRL represents a field of expanding research. Well-known risk factors include ALND, RLNR, high BMI at diagnosis, subclinical edema, and ipsilateral skin infection. Ongoing research is making progress in studying BCRL onset, screening, risk factors, risk prediction, and treatment. Patients treated for BC should be routinely screened and evaluated for BCRL and stratified according to their different risk factors. Screening for BCRL is evidence based and strongly recommended, but unfortunately not universally adopted. Essential components of a BCRL screening program include preoperative baseline arm volume measures, consistent arm volume measurements, and regular evaluation of patient symptoms and clinical presentation for as long as possible, but at least 3 to 4 years after BC surgery. BCRL treatment is multifaceted and may include conservative and surgical options that target the affected arm’s volume, the patient’s symptoms, and function. Surgical interventions hold promise to prevent or reduce BCRL. A multidisciplinary team approach is absolutely essential for a successful BCRL screening and treatment program.
Future Direction
Future research should aim to identify thresholds for intervention for BIS and arm volume measurements (perometry and circumferential tape measure converted to volume). Research efforts should definitively quantify the role of systemic therapy, breast reconstruction surgery, RT’s parameters and medical procedures, and precautionary lifestyle behaviors on BCRL risk.
The lack of standardization of BCRL quantification and the absence of an established consensus continue to be fundamental obstacles to comparing and generalizing studies’ results and supplementing evidence-based practices and knowledge. Collaboration to establish a comprehensive definition of BCRL incorporating patient-reported symptoms and preoperative baseline is imperative for the advancement of BCRL screening, management, and research.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hespe GE, Nitti MD, Mehrara BJ. Pathophysiology of lymphedema. In: Greene A, Slavin S, Brorson H, editors. Lymphedema presentation, diagnosis, and treatment. Cham: Springer; 2015.
Chachaj A, Malyszczak K, Pyszel K, et al. Physical and psychological impairments of women with upper limb lymphedema following breast cancer treatment. Psychooncology. 2010;19:299–305.
Fu MR, Rosedale M. Breast cancer survivors’ experiences of lymphedema-related symptoms. J Pain Symptom Manag. 2009;38:849–59.
• DiSipio T, Rye S, Newman B, et al. Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol. 2013;14:500–15. This is a review and meta-analysis of the available literature on the incidence of lymphedema. They concluded that more than one in five women treated for breast cancer will develop BCRL.
Shah C, Vicini FA. Breast cancer-related arm lymphedema: incidence rates, diagnostic techniques, optimal management and risk reduction strategies. Int J Radiat Oncol Biol Phys. 2011;81:907–14.
Tsai RJ, Dennis LK, Lynch CF, Snetselaar LG, Zamba GKD, Scott-Conner C. The risk of developing arm lymphedema among breast cancer survivors: a meta-analysis of treatment factors. Ann Surg Oncol. 2009;16:1959–72.
Hidding JT, Viehoff PB, Beurskens CHG, van Laarhoven HWM, Nijhuis-van der Sanden MWG, van der Wees PJ. Measurement properties of instruments for measuring of lymphedema: systematic review. Phys Ther 2016;96(12):1965–1981.
Bernas MJ, Askew RL, Armer JM, Cormier JN. Lymphedema: how do we diagnose and reduce the risk of this dreaded complication of breast cancer treatment? Curr Breast Cancer Rep. 2010;2:53–8.
O’Toole J, Jammallo LS, Miller CL, Skolny MN, Specht MC, Taghian AG. Screening for breast cancer-related lymphedema: the need for standardization. Oncologist. 2013;18(4):350–2.
National Lymphedema Network. Screening and measurement for early detection of breast cancer related lymphedema [Internet]. 2011. Available online: https://www.lymphnet.org/resources/position-paper-screening-and-measurement-for-early-detection-breast-cancer-related-lymphedema.
Sander AP, Hajer NM, Hemenway K, Miller AC. Upper-extremity volume measurements in women with lymphedema: a comparison of measurements obtained via water displacement with geometrically determined volume. Phys Ther. 2002;82(12):1201–12.
Tidhar D, Armer JM, Deutscher D, Shyu C-R, Azuri J, Madsen R. Measurement issues in anthropometric measures of limb volume change in persons at risk for and living with lymphedema: a reliability study. J Pers Med. 2015;5(4):341–53.
• Sun F, Hall A, Tighe MP, Brunelle CL, Sayegh HE, Gillespie TC, et al. Perometry versus simulated circumferential tape measurement for the detection of breast cancer-related lymphedema. Breast Cancer Res Treat. 2018;172(1):83–91. This study compares Perometry and circumferential tape measurement, landmark-based and interval-based techniques, as volumetric tools to quantify BCRL. They found that landmark-based tape measurement is more sensitive and specific than interval-based measurement and were comparable to perometry for RVC≥10 detection and that tape measurements may lead to under or over-estimation of volumes depending on the location on the arm.
Stanton AW, Northfield JW, Holroyd B, Mortimer PS, Levick JR. Validation of an optoelectronic limb volumeter (Perometer). Lymphology. 1997;30:77–97.
Lee M-J, Boland RA, Czerniec S, Kilbreath SL. Reliability and concurrent validity of the perometer for measuring hand volume in women with and without lymphedema. Lymphat Res Biol. 2011;9(1):13–8.
•• Stout Gergich NL, Pfalzer LA, McGarvey C, Springer B, Gerber LH, Soballe P. Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer. 2008;112(12):2809–19. This paper demonstrates the importance and effectiveness of a screening program for early BCRL detection and intervention. The screening program must incorporate preoperative measurements regular postoperative follow ups.
Stout Gergich NL. Reply to preoperative assessment enables the early detection and successful treatment of lymphedema. Cancer. 2009;115(4):910–0.
Seward C, Skolny M, Brunelle C, Asdourian M, Salama L, Taghian AG. A comprehensive review of bioimpedance spectroscopy as a diagnostic tool for the detection and measurement of breast cancer-related lymphedema. J Surg Oncol. 2016;114(5):537–42.
• Ridner SH, Dietrich MS, Spotanski K, Doersam JK, Cowher MS, Taback B, et al. A prospective study of L-Dex values in breast cancer patients pretreatment and through 12 months postoperatively. Lymphat Res Biol. 2018;16(5):435–41. This paper examines BIS L-Dex values preoperatively and longitudinally for 12 months post-operatively to help identify a threshold for lymphedema diagnosis. They found that an L-Dex value of ≥7 is suggestive of clinical BCRL.
Fu MR, Cleland CM, Guth AA, Kayal M, Haber J, Cartwright F, et al. L-dex ratio in detecting breast cancer-related lymphedema: reliability, sensitivity, and specificity. Lymphology. 2013;46(2):85–96.
• Bundred NJ, Stockton C, Keeley V, Riches K, Ashcroft L, Evans A, et al. Comparison of multi-frequency bioimpedance with perometry for the early detection and intervention of lymphoedema after axillary node clearance for breast cancer. Breast Cancer Res Treat. 2015;151(1):121–9. This study compares the incidences of BCRL detected by BIS and Perometry. They concluded that there is moderate correlation between the two methods at 6 months and that arm volume measurement remains gold standard for BCRL diagnosis.
SOZO® [Internet]. Impedimed Available from: https://www.impedimed.com/products/sozo/. Accessed 2020 May 26.
Qin ES, Bowen MJ, Chen WF. Diagnostic accuracy of bioimpedance spectroscopy in patients with lymphedema: a retrospective cohort analysis. J Plast Reconstr Aesthet Surg. 2018;71(7):1041–50.
Barrio AV, Eaton A, Frazier TG. A prospective validation study of bioimpedance with volume displacement in early-stage breast cancer patients at risk for lymphedema. Ann Surg Oncol. 2015;22(Suppl 3):S370–5.
•• Bundred N, Foden P, Todd C, Morris J, Watterson D, et al. Increases in arm volume predict lymphoedema and quality of life deficits after axillary surgery: a prospective cohort study. Br J Cancer. 2020;123:17–25. This study compares the 5-year incidences of BCRL detected by BIS and Perometry. The long-term data shows that relative arm volume measurments, as compared to preopearive baselines is the most fitting tool to diagnose BCRL and that BIS alone is not adequate.
Brunelle CL, Taghian AG. Lymphoedema screening: setting the standard. Br J Cancer. 2020;123:1–2.
Ancukiewicz M, Miller CL, Skolny MN, O’Toole J, Warren LE, Jammallo LS, et al. Comparison of relative versus absolute arm size change as criteria for quantifying breast cancer-related lymphedema: the flaws in current studies and need for universal methodology. Breast Cancer Res Treat. 2012;135(1):145–52.
•• Sun F, Skolny MN, Swaroop MN, et al. The need for preoperative baseline arm measurement to accurately quantify breast cancer-related lymphedema. Breast Cancer Res Treat. 2016;157:229–40. This study illustrates how crucial a preoperative baseline is for BCRL diagnosis by demonstrating that natural asymmetries can lead to lymphedema misdiagnosis by comparing the affected arm’s volume to that of the unaffected arm.
Armer JM, Stewart BR. A comparison of four diagnostic criteria for lymphedema in a post-breast cancer population. Lymphat Res Biol. 2005;3(4):208–17.
Ancukiewicz M, Russell TA, Otoole J, Specht M, Singer M, Kelada A, et al. Standardized method for quantification of developing lymphedema in patients treated for breast cancer. Int J Radiat Oncol Biol Phys. 2011;79(5):1436–43.
Miller CL, Specht MC, Horick N, Skolny MN, Jammallo LS, O’Toole J, et al. A novel, validated method to quantify breast cancer-related lymphedema (BCRL) following bilateral breast surgery. Lymphology. 2013;46(2):64–74.
• Specht MC, Miller CL, Russell TA, et al. Defining a threshold for intervention in breast cancer-related lymphedema: what level of arm volume increase predicts progression? Breast Cancer Res Treat. 2013;140:485–94. This paper examines the role of different subclinical swelling thresholds on risk of progression to lymphedema to help define a threshold for intervention. They found that a ≥5 to <10% threshold can be used as a criterion for close surveillance or intervention.
Armer JM, Radina ME, Porock D, Culbertson SD. Predicting breast cancer-related lymphedema using self-reported symptoms. Nurs Res. 2003;52(6):370–9.
Norman SA, Localio AR, Potashnik SL, Simoes Torpey HA, Kallan MJ, Weber AL, et al. Lymphedema in breast cancer survivors: incidence, degree, time course, treatment, and symptoms. JCO. 2009;27(3):390–7.
Armer JM, Henggeler MH, Brooks CW, Zagar EA, Homan S, Stewart BR. The health deviation of post-breast cancer lymphedema: symptom assessment and impact on self-care agency. Self Care Depend Care Nurs. 2008;16(1):14–21.
Weiss J, Daniel T. Validation of the lymphedema life impact scale (LLIS): a condition-specific measurement tool for persons with lymphedema. Lymphology. 2015;48(3):128–38.
Fu MR, Axelrod D, Guth AA, Rampertaap K, El-Shammaa N, Hiotis K, et al. mHealth self-care interventions: managing symptoms following breast cancer treatment. mHealth. 2016;2:28.
Shi S, Lu Q, Fu MR, Ouyang Q, Liu C, Lv J, et al. Psychometric properties of the breast cancer and lymphedema symptom experience index: the Chinese version. Eur J Oncol Nurs. 2016;20:10–6.
Spinelli B, Kallan MJ, Zhang X, Cheville A, Troxel A, Cohn J, et al. Intra- and interrater reliability and concurrent validity of a new tool for assessment of breast cancer-related lymphedema of the upper extremity. Arch Phys Med Rehabil. 2019;100(2):315–26.
• Shah C, Arthur DW, Wazer D, Khan A, Ridner S, Vicini F. The impact of early detection and intervention of breast cancer-related lymphedema: a systematic review. Cancer Med. 2016;5(6):1154–62. This review examines the literature for strategies to BCRL screening and diagnosis. They show that data supports an early screening program designed for early BCRL detection and treatment.
•• Brunelle C, Skolny M, Ferguson C, Swaroop M, O’Toole J, Taghian A. Establishing and sustaining a prospective screening program for breast cancer-related lymphedema at the Massachusetts General Hospital: lessons learned. JPM. 2015;5(2):153–64 This paper sets a successful example for how to establish an efficient screening program for BCRL and details the necessity of BCRL screening, the challenges encountered, the lessons learned and the steps required for other institutions to implement their own screening programs.
•• McDuff SGR, Mina AI, Brunelle CL, Salama L, Warren LEG, Abouegylah M, et al. Timing of lymphedema following treatment for breast cancer: when are patients most at risk? Int J Radiat Oncol Biol Phys. 2019;103(1):62–70. This paper studies the timeline of BCRL risk and the factors that influence it. They found that the timing of lymphedema development differs depending on the type axillary surgery and whether or not they received RLNR.
Stout NL, Pfalzer LA, Springer B, Levy E, McGarvey CL, Danoff JV, et al. Breast cancer–related lymphedema: comparing direct costs of a prospective surveillance model and a traditional model of care. Phys Ther. 2012;92(1):152–63.
National Lymphedema Network. Lymphedema Risk Reduction Practices [Internet]. 2012. Available online: https://www.lymphnet.org/resources/position-paper-lymphedema-risk-reduction-practices.
Denlinger CS, Sanft T, Baker KS, Broderick G, Demark-Wahnefried W, Friedman DL, et al. Survivorship, version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2018;16(10):1216–47.
Executive Committee. The diagnosis and treatment of peripheral lymphedema: 2016 Consensus Document of the International Society of Lymphology. Lymphology. 2016;49(4):170–84.
McLaughlin SA, Staley AC, Vicini F, Thiruchelvam P, Hutchison NA, Mendez J, et al. Considerations for clinicians in the diagnosis, prevention, and treatment of breast cancer-related lymphedema: recommendations from a multidisciplinary expert ASBrS panel: part 1: definitions, assessments, education, and future directions. Ann Surg Oncol. 2017;24(10):2818–26.
McLaughlin SA, Wright MJ, Morris KT, et al. Prevalence of lymphedema in women with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: objective measurements. J Clin Oncol. 2008;26:5213–9.
•• Kilbreath SL, Refshauge KM, Beith JM, et al. Risk factors for lymphoedema in women with breast cancer: a large prospective cohort. Breast. 2016;28:29–36. This study evaluates risk factors for lymphedema by screening at-risk women. They found that taxane-based chemotherapy, increased weight at diagnosis and arm swelling within 4 weeks post-surgery were associated with arm swelling at 6 and 12 months and that in women with ≥5 nodes removed, arm swelling at one year is a risk factor for subsequent lymphedema.
Kim M, Kim SW, Lee SU, Lee NK, Jung SY, Kim TH, et al. A model to estimate the risk of breast cancer-related lymphedema: combinations of treatment-related factors of the number of dissected axillary nodes, adjuvant chemotherapy, and radiation therapy. Int J Radiat Oncol Biol Phys. 2013;86:498–503.
Warren LEG, Miller CL, Horick N, Skolny MN, Jammallo LS, Sadek BT, et al. The impact of radiation therapy on the risk of lymphedema after treatment for breast cancer: a prospective cohort study. Int J Radiat Oncol Biol Phys. 2014;88:565–71.
Miller CL, Specht MC, Skolny MN, Horick N, Jammallo LS, O’Toole J, et al. Risk of lymphedema after mastectomy: potential benefit of applying ACOSOG Z0011 protocol to mastectomy patients. Breast Cancer Res Treat. 2014;144:71–7.
Gross JP, Lynch CM, Flores AM, Jordan SW, Helenowski IB, Gopalakrishnan M, et al. Determining the organ at risk for lymphedema after regional nodal irradiation in breast cancer. Int J Radiat Oncol Biol Phys. 2019;105(3):649–58.
• Swaroop MN, Ferguson CM, Horick NK, et al. Impact of adjuvant taxane-based chemotherapy on development of breast cancer-related lymphedema: results from a large prospective cohort. Breast Cancer Res Treat. 2015;151:393–403. In this large prospective cohort study, patients were prospectively screened for lymphedema with preoperative measurements. They found that taxane-based chemotherapy was not significantly associated with swelling when compared to no chemotherapy and non-taxane chemotherapy.
• Miller CL, Colwell AS, Horick N, et al. Immediate implant reconstruction is associated with a reduced risk of lymphedema compared to mastectomy alone: A prospective cohort study. Ann Surg. 2016;263:399–405. This paper studies the effect of immediate breast reconstruction on risk of lymphedema, as compared to mastectomy alone. They found that implant-based reconstruction, but not autologous reconstruction, does not increase the risk of lymphedema.
Ridner SH, Dietrich MS, Stewart BR, Armer JM. Body mass index and breast cancer treatment-related lymphedema. Support Care Cancer. 2011;19:853–7.
Fu MR, Axelrod D, Guth A, Fletcher J, Qiu J, Scagliola J, et al. Patterns of obesity and lymph fluid level during the first year of breast cancer treatment: a prospective study. J Pers Med. 2015;5:326–40.
Jammallo LS, Miller CL, Singer M, Horick NK, Skolny MN, Specht MC, et al. Impact of body mass index and weight fluctuation on lymphedema risk in patients treated for breast cancer. Breast Cancer Res Treat. 2013;142:59–67.
•• Armer JM, Ballman KV, McCall L, Ostby PL, Zagar E, Kuerer HM, et al. Factors associated with lymphedema in women with node-positive breast cancer treated with neoadjuvant chemotherapy and axillary dissection. JAMA Surg. 2019;154(9):800. This study evaluated factors associated with lymphedema in breast cancer patients who have received neoadjuvant chemotherapy and ALND. They found that a longer duration of neoadjuvant chemotherapy and obesity were significant risk factors for lymphedema.
•• Schmitz KH, Troxel AB, Dean LT, DeMichele A, Brown JC, Sturgeon K, et al. Effect of home-based exercise and weight loss programs on breast cancer–related lymphedema outcomes among overweight breast cancer survivors: the WISER Survivor Randomized Clinical Trial. JAMA Oncol. 2019;5(11):1605. This is the first randomized clinical trial to study the combination of weight loss and exercise interventions on BCRL risk. They randomized patients to a home-based resistance exercise program or a weight loss program or a combination of the two or to the control group. They found that weight loss, home-based exercise, and combined interventions did not improve BCRL outcomes.
Winkels RM, Sturgeon KM, Kallan MJ, Dean LT, Zhang Z, Evangelisti M, et al. The women in steady exercise research (WISER) survivor trial: the innovative transdisciplinary design of a randomized controlled trial of exercise and weight-loss interventions among breast cancer survivors with lymphedema. Contemp Clin Trials. 2017;61:63–72.
•• Asdourian MS, Skolny MN, Brunelle C, et al. Precautions for breast cancer-related lymphoedema: risk from air travel, ipsilateral arm blood pressure measurements, skin puncture, extreme temperatures, and cellulitis. Lancet Oncol. 2016;17:e392–405. This paper reviews the literature for the effect of medical procedures and lifestyle-associated risk factors on lymphedema risk. They conclude that the available evidence is contradictory and insufficient to support a significant association between these factors and BCRL, therefore calling for more research.
• Ferguson CM, Swaroop MN, Horick N, et al. Impact of ipsilateral blood draws, injections, blood pressure measurements, and air travel on the risk of lymphedema for patients treated for breast cancer. J Clin Oncol. 2016;34:691–8. This study assessed the influence of certain risk factors on lymphedema risk. They found that only cellulitis significantly increased BCRL risk, while air travel, ipsilateral injections, blood draws and blood pressure measurements did not.
Toyserkani NM, Jørgensen MG, Haugaard K, Sørensen JA. Seroma indicates increased risk of lymphedema following breast cancer treatment: a retrospective cohort study. Breast. 2017;32:102–4.
Shaitelman SF, Chiang YJ, Griffin KD, DeSnyder SM, Smith BD, Schaverien MV, et al. Radiation therapy targets and the risk of breast cancer-related lymphedema: a systematic review and network meta-analysis. Breast Cancer Res Treat. 2017;162:201–15.
•• Donker M, van Tienhoven G, Straver ME, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014;15:1303–10. This large multicenter randomized clinical trial evaluates regional control outcomes and side effects of axillary radiotherapy after sLNB compared to ALND in T1–2 breast cancer patients with no lymph node metastasis. They showed comparable axillary disease control with lesser morbidity with radiotherapy.
• Naoum GE, Roberts S, Brunelle CL, Shui A, Salama L, et al. Quantifying the impact of axillary surgery and regional lymph node irradiation on lymphedema risk and local tumor control in breast cancer patients: long-term results from a prospective screening trial. J Clin Oncol. 2020;38(29):3430–8. https://doi.org/10.1200/JCO.20.00459. This paper is a prospective BCRL screening trial aiming to assess the impact of axillary surgery and RLNR on BCRL rate across groups of patients treated for BC (SLNB, SLNB+RLNR, ALND, ALND+RLNR) with preoperative baseline arm measurements. They found that the ALND alone group had significantly higher BCRL risk than the SLNB+RLNR, but there was no significant difference between the ALND+RLNR and ALND alone and between the SLNB+RLNR and SLNB alone in terms of BCRL rate.
• Chandra RA, Miller CL, Skolny MN, Warren LEG, Horick N, Jammallo LS, et al. Radiation therapy risk factors for development of lymphedema in patients treated with regional lymph node irradiation for breast cancer. Int J Radiat Oncol Biol Phys. 2015;91(4):760–4. This paper assesses the effect of certain dosimetric radiation factors on lymphedema risk. They found that none of the parameters studied (ie: dose, energy, tangent type, etc…) was associated with lymphedema.
Gross JP, Sachdev S, Helenowski IB, Lipps D, Hayes JP, Donnelly ED, et al. Radiation therapy field design and lymphedema risk after regional nodal irradiation for breast cancer. Int J Radiat Oncol Biol Phys. 2018;102(1):71–8.
• Asdourian MS, Swaroop MN, Sayegh HE, et al. Association between precautionary behaviors and breast cancer-related lymphedema in patients undergoing bilateral surgery. J Clin Oncol. 2017;35:3934–41. This paper studied lifestyle and medical procedures-related factors in a cohort of prospectively screened breast cancer patients for lymphedema. They found that a high BMI at diagnosis, ALND and receipt of chemotherapy were associated with swelling while blood pressure readings, blood draws, injections, and number or duration of flights were not.
Zhu W, Li D, Li X, Ren J, Chen W, Gu H, et al. Association between adjuvant docetaxel-based chemotherapy and breast cancer-related lymphedema. Anti-Cancer Drugs. 2017;28:350–5.
Ohsumi S, Shimozuma K, Ohashi Y, Takeuchi A, Suemasu K, Kuranami M, et al. Subjective and objective assessment of edema during adjuvant chemotherapy for breast cancer using taxane-containing regimens in a randomized controlled trial: the national surgical adjuvant study of breast cancer 02. Oncology. 2012;82:131–8.
Invernizzi M, Michelotti A, Noale M, Lopez G, Runza L, Giroda M, et al. Breast cancer systemic treatments and upper limb lymphedema: a risk-assessment platform encompassing tumor-specific pathological features reveals the potential role of trastuzumab. JCM. 2019;8(2):138.
Ganju RG, Savvides G, Korentager S, Ward MJ, TenNapel M, Amin A, et al. Incidence of breast lymphedema and predictors of its development in patients receiving whole breast radiation therapy after breast-conservation surgery. Lymphology. 2019;52(3):126–33.
Crosby MA, Card A, Liu J, et al. Immediate breast reconstruction and lymphedema incidence. Plast Reconstr Surg. 2012;129:789e–95e.
Card A, Crosby M, Liu J, et al. Reduced incidence of breast cancer-related lymphedema following mastectomy and breast reconstruction versus mastectomy alone. Plast Reconstr Surg. 2012;130:1169–78.
Lee KT, Mun GH, Lim SY, Pyon JK, Oh KS, Bang SI. The impact of immediate breast reconstruction on post-mastectomy lymphedema in patients undergoing modified radical mastectomy. Breast. 2013;22:53–7.
Siotos C, Sebai ME, Wan EL, Bello RJ, Habibi M, Cooney DS, et al. Breast reconstruction and risk of arm lymphedema development: a meta-analysis. J Plast Reconstr Aesthet Surg. 2018;71(6):807–18.
Isom C, Bream P, Gallagher K, Walia S, Ahmed R, Kauffmann R. Placement of subcutaneous central venous ports in breast cancer patients: does side matter? J Surg Res. 2019;244:296–301.
Visser J, van Geel M, Cornelissen AJM, van der Hulst RRWJ, Qiu SS. Breast cancer-related lymphedema and genetic predisposition: a systematic review of the literature. Lymphat Res Biol. 2019;17(3):288–93.
Fu MR, Conley YP, Axelrod D, Guth AA, Yu G, Fletcher J, et al. Precision assessment of heterogeneity of lymphedema phenotype, genotypes and risk prediction. Breast. 2016;29:231–40.
Koul R, Dufan T, Russell C, Guenther W, Nugent Z, Sun X, et al. Efficacy of complete decongestive therapy and manual lymphatic drainage on treatment-related lymphedema in breast cancer. Int J Radiat Oncol Biol Phys. 2007;67(3):841–6.
Rogan S, Taeymans J, Luginbuehl H, Aebi M, Mahnig S, Gebruers N. Therapy modalities to reduce lymphoedema in female breast cancer patients: a systematic review and meta-analysis. Breast Cancer Res Treat. 2016;159(1):1–14.
Jeffs E, Ream E, Taylor C, Bick D. Clinical effectiveness of decongestive treatments on excess arm volume and patient-centered outcomes in women with early breast cancer-related arm lymphedema: a systematic review. JBI Database System Rev Implement Rep. 2018;16(2):453–506.
Ezzo J, Manheimer E, McNeely ML, et al. Manual lymphatic drainage for lymphedema following breast cancer treatment. Cochrane Database Syst Rev. 2015;5:CD003475.
Panchik D, Masco S, Zinnikas P, Hillriegel B, Lauder T, Suttmann E, et al. Effect of exercise on breast cancer-related lymphedema: what the lymphatic surgeon needs to know. J Reconstr Microsurg. 2019;35(1):37–45.
•• Schmitz KH, Troxel AB, Cheville A, Grant LL, Bryan CJ, Gross CR, et al. Physical activity and lymphedema (the PAL trial): assessing the safety of progressive strength training in breast cancer survivors. Contemp Clin Trials. 2009;30(3):233–45. This paper describes a randomized clinical trial that aims to compare lymphedema incidence rates among at-risk women and lymphedema exacerbations among women with established lymphedema. Women are randomly assigned to a twice weekly progressive exercise regimen for 12 months or to a group of non-exercising controls.
•• Schmitz KH, Ahmed RL, Troxel A, Cheville A, Smith R, Lewis-Grant L, et al. Weight lifting in women with breast-cancer-related lymphedema. N Engl J Med. 2009;361(7):664–73. This is a randomized controlled trial studying the effect of weight lifting exercises in breast cancer patient with lymphedema. Patients were randomly assigned to either to a progressive weight-lifting program or to the control group. They found that weight lifting did not affect swelling and that it was associated lesser exacerbations and symptoms.
•• Schmitz KH, Ahmed RL, Troxel AB, Cheville A, Lewis-Grant L, Smith R, et al. Weight lifting for women at risk for breast cancer-related lymphedema: a randomized trial. JAMA. 2010;304(24):2699–705. This is a randomized controlled trial studying the effect of weight lifting exercises on lymphedema risk in at-risk breast cancer patient. Patients were randomly assigned to either a weight-lifting intervention or to the control group. They found that weight lifting did not increase risk of lymphedema.
McLaughlin SA, DeSnyder SM, Klimberg S, Alatriste M, Boccardo F, Smith ML, et al. Considerations for clinicians in the diagnosis, prevention, and treatment of breast cancer-related lymphedema, recommendations from an expert panel: part 2: preventive and therapeutic options. Ann Surg Oncol. 2017;24(10):2827–35.
Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvão DA, Pinto BM, et al. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010;42(7):1409–26.
Irwin M. ACSM’s guide to exercise and cancer survivorship. Champagne: Human Kinetics; 2012.
Granzow JW, Soderberg JM, Kaji AH, Dauphine C. Review of current surgical treatments for lymphedema. Ann Surg Oncol. 2014;21(4):1195–201.
Allen RJ, Cheng M-H. Lymphedema surgery: patient selection and an overview of surgical techniques: lymphedema surgery. J Surg Oncol. 2016;113(8):923–31.
Brorson H. Liposuction in lymphedema treatment. J Reconstr Microsurg. 2015;32(01):056–65.
Greene AK, Maclellan RA. Operative treatment of lymphedema using suction-assisted lipectomy. Ann Plast Surg. 2016;77:337–40.
Baumeister RG, Mayo W, Notohamiprodjo M, Wallmichrath J, Springer S, Frick A. Microsurgical lymphatic vessel transplantation. J Reconstr Microsurg. 2016;32:34–41.
Poumellec MA, Foissac R, Cegarra-Escolano M, Barranger E, Ihrai T. Surgical treatment of secondary lymphedema of the upper limb by stepped microsurgical lymphaticovenous anastomoses. Breast Cancer Res Treat. 2017;162:219–24.
Tummel E, Ochoa D, Korourian S, Betzold R, Adkins L, McCarthy M, et al. Does axillary reverse mapping prevent lymphedema after lymphadenectomy? Ann Surg. 2017;265:987–92.
Jørgensen MG, Toyserkani NM, Sørensen JA. The effect of prophylactic lymphovenous anastomosis and shunts for preventing cancer-related lymphedema: a systematic review and meta-analysis. Microsurgery. 2018;38(5):576–85.
Parks RM, Cheung KL. Axillary reverse mapping in N0 patients requiring sentinel lymph node biopsy - a systematic review of the literature and necessity of a randomised study. Breast. 2017;33:57–70.
Feldman S, Bansil H, Ascherman J, Grant R, Borden B, Henderson P, et al. Single institution experience with lymphatic microsurgical preventive healing approach (LYMPHA) for the primary prevention of lymphedema. Ann Surg Oncol. 2015;22:3296–301.
Rockson SG, Tian W, Jiang X, Kuznetsova T, Haddad F, Zampell J, et al. Pilot studies demonstrate the potential benefits of antiinflammatory therapy in human lymphedema. JCI Insight. 2018;18:3(20).
ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). 2000 Feb 29. Identifier NCT03783715, Characterization of Treatment Responses in Lymphedema; 2018 Dec 21 [cited 2020 Sept 30]. Available from: https://clinicaltrials.gov/ct2/show/NCT03783715.
Funding
The project was supported by Award Number R01CA139118 (AG Taghian) and Award Number P50CA08393 (AG Taghian) from the National Cancer Institute. This program is supported by the Adele McKinnon Research Fund for Breast Cancer-Related Lymphedema, the Heinz Family Foundation and the Olayan-Xefos Family Fund for Breast Cancer Research.
Author information
Authors and Affiliations
Contributions
All authors were involved in manuscript writing and final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Alphonse Taghian is on the Scientific Advisory Board of Puretech Health and a previous consultant in VisionRT. AGT has been loaned equipment from ImpediMed for use in investigator-initiated clinical trials. Cheryl Brunelle is on the Scientific Advisory Board of Puretech Health. The remaining authors have nothing to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Radiation Oncology
Rights and permissions
About this article
Cite this article
Nassif, T.M., Brunelle, C.L., Gillespie, T.C. et al. Breast Cancer-Related Lymphedema: a Review of Risk Factors, Radiation Therapy Contribution, and Management Strategies. Curr Breast Cancer Rep 12, 305–316 (2020). https://doi.org/10.1007/s12609-020-00387-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-020-00387-8